What is myxedema coma
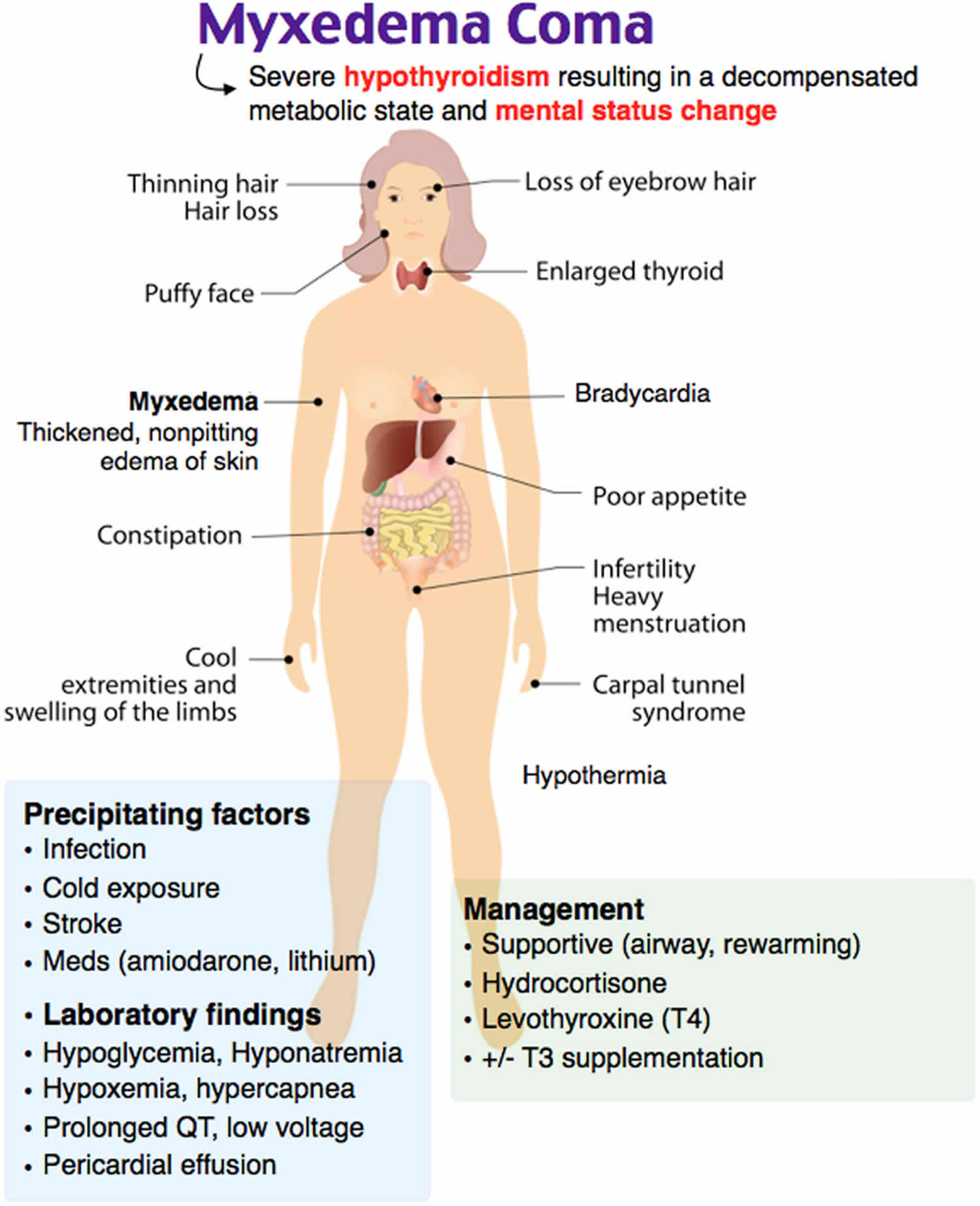
Myxedema coma occasionally called myxedema crisis, is a rare life-threatening clinical condition in patients with longstanding severe untreated hypothyroidism that represents severe hypothyroidism with physiological decompensation 1. The condition usually occurs in patients with long-standing, undiagnosed hypothyroidism and is usually precipitated by infection, cerebrovascular disease, heart failure, trauma, or drug therapy 2. Patients with myxedema coma are generally severely-ill with significant hypothermia and depressed mental status. Most patients, however, are not comatose, and the entity rather represents a form of very severe, decompensated hypothyroidism.
The three key features of myxedema coma are 1:
- Altered mental status. Usually somnolence and lethargy have been present for months. Lethargy may develop via stupor into a comatose state. There may have been transient episodes of reduced consciousness before a more complete variety develops.
- Defective thermoregulation: hypothermia.The lower the temperature, the worse the prognosis. Please check the ability of the thermometer to accurately measure decreased temperatures (automatic thermometers may not register frank hypothermia). Fever may be absent despite infectious disease. With cold weather the body temperature may drop sharply. Myxedema coma mostly develops during winter months.
- Precipitating event. Look for cold exposure, infection, drugs (diuretics, tranquillizers, sedatives, analgesics), trauma, stroke, heart failure, gastrointestinal bleeding.The typical patient is an older woman with altered consciousness, presenting in wintertime. There is often a history of hypothyroidism, neck surgery or radioactive iodine treatment.
Physical examination may reveal hypothermia, hypoventilation, hypotension, bradycardia, dry coarse skin, macroglossia, and delayed deep-tendon reflexes. Absence of mild diastolic hypertension in severely hypothyroid patients is a warning sign of impending myxedema coma.
Laboratory examination may reveal anemia, hyponatremia, hypoglycemia, hypercholesterolemia, and high serum creatine kinase concentrations. Most patients have low serum FT4 and high serum TSH. However, serum TSH can be low or normal, due to the presence of central hypothyroidism or the nonthyroidal illness syndrome.
A medical emergency, myxedema coma requires immediate medical attention. If myxedema coma is suspected, immediate management is necessary before confirming the diagnosis due to the high associated mortality rate 2. Patients with myxedema coma should be treated in an intensive care unit (ICU) with continuous cardiac monitoring. Initial steps in therapy include airway management, thyroid hormone replacement, glucocorticoid therapy, and supportive measures.
Myxedema coma causes
Myxedema is a term generally used to denote severe hypothyroidism. Myxedema is also used to describe the dermatologic changes that occur in hypothyroidism and occasionally hyperthyroidism. In this setting, myxedema refers to deposition of mucopolysaccharides in the dermis, which results in swelling of the affected area. When skin changes occur in hyperthyroidism, mostly Graves disease, it’s called pretibial myxedema.
Myxedema coma occurs as a result of long-standing, undiagnosed, or undertreated hypothyroidism and is usually precipitated by a systemic illness. Myxedema coma can result from any of the causes of hypothyroidism, most commonly chronic autoimmune thyroiditis. Myxedema coma can also occur in patients who had thyroidectomy or underwent radioactive iodine therapy for hyperthyroidism. Rare causes may include secondary hypothyroidism and medications such as lithium and amiodarone 3.
Most patients with myxedema coma have a history of hypothyroidism. Some patients may have developed hypothyroidism after thyroidectomy or iodine therapy for hyperthyroidism. However, some patients will have undiagnosed hypothyroidism and myxedema coma will be the initial presentation.
Symptoms of hypothyroidism, including fatigue, weight gain, cold intolerance, constipation, and dry skin, may be elicited.
Patients have depressed mental state with lethargy, delirium, or coma.
Symptoms of the precipitating illness can be seen such as infection (commonly pneumonia), stroke, myocardial infarction, trauma, or heart failure.
Myxedema coma is a physiologic decompensation of untreated hypothyroidism that is usually caused by a precipitating factor such as the following:
- Infection
- Exposure to cold temperatures
- Trauma
- Burns
- Cerebrovascular accident
- Myocardial infarction
- Congestive heart failure
- Respiratory acidosis
- Medications such as the following:
- Tranquilizers
- Sedatives
- Anesthetics
- Narcotics
- Amiodarone
- Rifampin
- Beta blockers
- Lithium
- Phenytoin
- Gastrointestinal hemorrhage
- Metabolic disturbances such as hypoglycemia, hyponatremia, acidosis, and hypercapnia
- Ingestion of raw bok choy
Myxedema coma signs and symptoms
Given the importance of thyroid hormones in cell metabolism, long-standing hypothyroidism is associated with reduced metabolic rate and decreased oxygen consumption, which affects all body systems 4. This results in hypothermia, which is a strong predictor of mortality. Another consequence is decreased drug metabolism leading to overdosing of medications particularly sedatives, hypnotics, and anesthetic agents; this can precipitate myxedema coma.
Cardiovascular
Cardiac contractility is impaired, leading to reduced stroke volume, low cardiac output, bradycardia and sometimes hypotension 5. Reduced stroke volume in severe cases may also be due to pericardial effusions caused by the accumulation of fluid rich in mucopolysaccharides within the pericardial sac. Congestive heart failure is rarely seen in the absence of preexisting cardiac disease.
Electrocardiographic findings may include bradycardia, varying degrees of block, low voltage, nonspecific ST-segment changes, flattened or inverted T waves, prolonged Q-T interval, and ventricular or atrial arrhythmias 6.
The reduction of the effect of beta-adrenergic receptors leads to prevalence of the effect of alpha-adrenergic receptors, increased catecholamines, and increased systemic vascular resistance, causing some patients to have diastolic hypertension and a narrowed pulse pressure.
Plasma volume is decreased, and capillary permeability is increased, leading to fluid accumulation in tissue and spaces and pericardial effusions 7.
Neurologic
Despite the term myxedema coma, many patients do not present in coma, but manifest variable degrees of altered consciousness 8. Brain function is affected by reduction in oxygen delivery and subsequent consumption, decreased glucose utilization and reduced cerebral blood flow. Hyponatremia can also contribute to altered mental function.
Pulmonary
The main pulmonary effect of myxedema coma is hypoventilation, which results from central depression of ventilatory drive with decreased responsiveness to hypoxia and hypercapnia 9. Other contributing factors to hypoventilation include respiratory muscle weakness, mechanical obstruction by a large tongue, and obesity-hypoventilation syndrome. Fluid accumulation may cause pleural effusions and decreased diffusing capacity.
Renal
Kidney function may be compromised with reduced glomerular filtration rate because of low cardiac output and peripheral vasoconstriction or because of rhabdomyolysis 10. Hyponatremia is common in patients with myxedema coma and is caused by increased serum antidiuretic hormone and impaired water excretion 11.
Gastrointestinal
The gastrointestinal tract in myxedema coma can be marked by mucopolysaccharide infiltration and edema. In addition, neuropathic changes can cause malabsorption, gastric atony, impaired peristalsis, paralytic ileus, and megacolon 12. Ascites may occur due to increased capillary permeability, heart failure, or other mechanisms 13. Gastrointestinal bleeding secondary to an associated coagulopathy may occur 14.
Hematologic
Myxedema coma is associated with a higher risk of bleeding caused by coagulopathy related to an acquired von Willebrand syndrome (type 1) and decreases in factors V, VII, VIII, IX, and X 15. Patients may also have microcytic anemia secondary to hemorrhage, or macrocytic anemia caused by vitamin B12 deficiency, or normocytic normochromic anemia, which may be secondary to decreased oxygen requirement and reduced erythropoietin 7.
Myxedema coma complications
Complications may include the following:
- Respiratory failure
- Coma
- Heart failure
- Myocardial infarction
- Sepsis
- Gastrointestinal bleeding
Myxedema coma diagnosis
Physical Examination
Physical findings may include the following:
- Hypothermia, which may not be recognized initially because many automatic thermometers do not register low body temperatures (It may be necessary to use special thermometers.)
- Hypotension
- Bradycardia
- Decreased pulse pressure, normal systolic pressure, elevated diastolic pressure
- Decreased respiratory rate
- Periorbital puffiness
- Macroglossia
- Coarse or thinning hair
- Thyroid is commonly small (Look for scar suggesting previous thyroidectomy.)
- Slow respiratory rate
- Signs of pleural effusion
- Soft or distant heart sounds, diminished apical impulse, pericardial effusion
- Abdominal distension due to ascites
- Diminished or absent bowel sounds due to ileus
- Bladder distension
- Cold extremities, nonpitting edema of the upper and lower extremities
- Cool, pale, dry, scaly, and thickened skin
- Dry, brittle nails
- Ecchymoses, purpura
- Confusion, stupor, slow speech, delayed reflexes, seizures, coma
Laboratory studies
Laboratory studies are important to confirm the diagnosis of myxedema coma. However, if the condition is suspected, treatment should be started immediately without waiting for the results.
- Thyroid function tests
- TSH is elevated in most patients indicating a primary thyroid disorder
- Free T4 and free T3 levels are low
- A low or normal TSH level with low levels of free T4 and free T3 may indicate that the disorder is due to pituitary or hypothalamic dysfunction
- Assessment of adrenal function should be performed. A random serum cortisol can be obtained; however, the test is only helpful if it’s very low (< 3 mcg/dL) or high (>20 mcg/dL). Since most patients will have serum cortisol levels in between these values, an ACTH stimulation test is usually needed to assess the adrenal function. This test should not delay starting treatment. In contrast to hydrocortisone, which interferes with the cortisol assay, leading to falsely normal serum cortisol, dexamethasone does not interfere with the testing and can be administered immediately and continued until the results of the test become available.
- Hyponatremia with low serum osmolality
- Because of decreased renal perfusion, serum creatinine levels are usually elevated
- Hypoglycemia is common and may also be caused by reduced nutrition, sepsis, or the associated adrenal insufficiency.
- Complete blood count: leukocytosis may not be seen because of hypothermia. A white blood cell differential may be one of the few clues to the presence of infection.
A diagnostic scoring system for the diagnosis of myxedema coma has been proposed 16. The scoring system gives points for the following indicators: hypothermia; lethargy, obtundation, stupor, or coma; anorexia, reduced intestinal mobility, or paralytic ileus; bradycardia, electrocardiogram changes, pericardial or pleural effusions, cardiomegaly or hypertension; hyponatremia, hypoglycemia, hypoxemia, hypercapnia or reduced glomerular filtration rate, and the presence of a precipitating cause. This scoring system was based on data derived from a small sample of 21 patients, which may limit its generalizability.
Another diagnostic tool, developed by Chiong et al 17, uses six variables to screen for myxedema coma, including heart rate, temperature, Glasgow coma scale score, TSH levels, free T4 levels, and precipitating factors. The investigators, whose work utilized 10 study patients and 13 controls, reported the tool’s sensitivity and specificity to be about 80%.
Imaging Studies
Chest X-ray may show signs of cardiomegaly, pericardial effusion, congestive heart failure, or pleural effusion.
Other Tests
Electrocardiogram may reveal sinus bradycardia, low-amplitude QRS complexes, a prolonged QT interval, flattened or inverted T waves, or arrhythmias.
Myxedema coma treatment
Myxedema coma is a medical emergency. Early diagnosis, rapid administration of thyroid hormones and adequate supportive measures (Table) are essential for a successful outcome. The prognosis, however, remains poor with a reported mortality between 20% and 50%. In-hospital mortality was 29.5% among 149 patients with myxedema coma identified between 2010-2013 through a national inpatient database in Japan 18.
Table 1. Myxedema coma management
| MANAGEMENT OF MYXEDEMA COMA | |
|---|---|
| 1.Hypothyroidism | large initial iv dose of 300-500 μg T4, if no response add T3; |
| 1a | Alternative- initial iv dose of 200-300 μg T4 plus 10-25 μg T3 |
| 2.Hypocortisolemia | iv hydrocortisone 200-400 mg daily |
| 3. Hypoventilation | don’t delay intubation and mechanical ventilation too long |
| 4. Hypothermia | blankets, no active rewarming |
| 5. Hyponatremia | mild fluid restriction |
| 6. Hypotension | cautious volume expansion with crystalloid or whole blood |
| 7. Hypoglycemia | glucose administration |
| 8. Precipitating event | identification and elimination by specific treatment, liberal use of antibiotics |
Note 1. Administration of thyroid hormone is essential, but opinions differ about the dose and the preparation (T4 or T3). A high dose carries the risk of precipitating fatal tachycardia or myocardial infarction, but a low dose may be unable to reverse a downhill course. Treatment with T4 may be less effective due to impaired conversion of T4 into T3 (associated with severe illness and inadequate caloric intake), but treatment with T3 may expose tissues to relatively high levels of thyroid hormone. In the absence of randomized clinical trials, the available case series suggest higher mortality with initial T4 doses larger than 500 μg and with T3 doses larger than 75 μg daily. Treatment should be started intravenously because gastrointestinal absorption may be impaired. Typically, a large initial intravenous loading dose of 300-500 μg T4 may be given, followed by daily doses of 1.6 μg/kg (initially intravenously, and orally when feasible). If there is no response within 24 hours, addition of T3 is recommended. An alternative scheme is an initial intravenous dose of 200-300 μg T4 plus 10-25 μg T3, followed by 2.5-10 μg T3 every 8 hours depending on the patient’s age and presence of cardiovascular risk factors. Upon clinical improvement, T3 is discontinued and a daily oral T4 replacement dose is maintained.
Note 2. Pituitary-adrenal function is impaired in severe hypothyroidism. Restoration of a normal metabolic rate with exogenous thyroid hormones may precipitate adrenal insufficiency. It is therefore prudent to administer glucocorticoids in stress doses (e.g. hydrocortisone 100 mg intravenously every 8 hours).
Note 3. Mechanical ventilation may be needed, particularly when obesity and myxedema coexist.
Note 4. The cutaneous blood flow is markedly reduced in severe hypothyroidism in order to conserve body heat. Warming blankets will defeat this mechanism. Thus, central warming may be attempted, but peripheral warming should not, since it may lead to vasodilatation and shock.
Note 5. Fluid restriction and the use of isotonic sodium chloride will usually restore normal serum sodium. Normal saline should not be administered in patients with suspicious hyponatremic encephalopathy. In cases with severe symptomatic hyponatremia, 100 ml of 3% NaCl should be administered (Liamis et al. 2017). The new vasopressin antagonist conivaptan might be potentially useful in hyponatremia as high vasopressin levels have been observed in myxedema coma; however, no cases of myxedema coma have been reported in which this drug was administered.
Note 6. Volume expansion is usually required in case of hypotension since patients are maximally vasoconstricted. Dopamine should be added if fluid therapy does not restore efficient circulation.
Note 7. Serum glucose should be monitored. Supplemental glucose may be necessary, especially if adrenal insufficiency is present.
Note 8. A vigorous search for precipitating events is mandatory. Signs of infection (like fever, tachycardia, leukocytosis) may be absent. Prophylactic antibiotics are indicated until infection can be ruled out.
Follow up
In case treatment was initiated with intravenous T4 but after 24 hours the patient is still comatose or vital functions have not improved, iv administration of T3 should be considered. T3 should be discontinued and replaced by T4 once circulation and respiration have been stabilized. Intravenous administration of thyroid hormones is replaced by oral administration when the patient is fully awake.
Myxedema coma treatment guidelines
Recommendation 21 of the American Thyroid Association Guidelines for the treatment of myxedema coma 19 deals with the management of myxedema coma. It favors an initial loading dose of levothyroxine (200-400 μg intravenously) and intravenous glucocorticoid administration (strong recommendation, low-quality evidence). Additional administration of intravenous liothyronine (LT3) in a loading dose of 5-20 μg can be considered (weak recommendation, low-quality of evidence).
American Thyroid Association 2014 Guidelines for the treatment of Myxedema coma 19
21a. In patients with myxedema coma beingtreated with levothyroxine, what route of administration should be used?
RECOMMENDATION
Initial thyroid hormone replacement for myxedema comashould be levothyroxine given intravenously. A loadingdose of 200–400lg of levothyroxine may be given, withlower doses given for smaller or older patients and thosewith a history of coronary disease or arrhythmia. A dailyreplacement dose of 1.6lg/kg body weight, reduced to75% as long as it is being intravenously administered, canbe given thereafter. Oral therapy or other enteral therapy ifthe oral route cannot be employed may be instituted afterthe patient improves clinically.
21b. In patients with myxedema coma beingtreated with levothyroxine, should empiricglucocorticoid coverage be provided?
RECOMMENDATION
Empiric glucocorticoid coverage should be employed as partof the initial therapy for myxedema coma, with intravenous glucocorticoid administration, at doses appropriate for thestressed state, preceding levothyroxine administration.
21c. In patients with myxedema coma beingtreated with levothyroxine, should liothyroninetherapy also be initiated?
RECOMMENDATION
Given the possibility that thyroxine conversion to triio-dothyronine may be decreased in patients with myxedemacoma, intravenous liothyronine may be given in addition tolevothyroxine. High doses should be avoided given theassociation of high serum triiodothyronine during treat-ment with mortality. A loading dose of 5–20 μg can be given, followed by a maintenance dose of 2.5–10 μg every 8 hours, with lower doses chosen for smaller or older pa-tients and those with a history of coronary artery disease orarrhythmia. Therapy can continue until the patient isclearly recovering (e.g., until the patient regains con-sciousness and clinical parameters have improved).
21d. In patients with myxedema coma beingtreated with levothyroxine, what therapeuticendpoints should be targeted?
RECOMMENDATION
Intravenous levothyroxine treatment in severely hypothy-roid patients may lead to improvement in cardiovascular,renal, pulmonary, and metabolic parameters within a week. Serum thyroxine and triiodothyronine concentrations mayimprove or normalize with a similar time frame, with moregradual improvement in serum TSH. Thus, the therapeuticendpoints in myxedema coma should be improved mentalstatus, improved cardiac function, and improved pulmonaryfunction. Measurement of thyroid hormones every 1–2 days is reasonable to ensure a favorable trajectory in the bio-chemical parameters. While optimal levels for serum TSH and thyroid hormones are not well defined in this circum-stance, failure of TSH to trend down or for thyroid hormonelevels to improve could be considered indications to increaselevothyroxine therapy and/or add liothyronine therapy,whereas high serum triiodothyronine could be considered anindication to decrease therapy given safety concerns.
Myxedema coma prognosis
Myxedema coma is a medical emergency. If the condition is not promptly diagnosed and treated, the mortality rate can be more than 50%. Even with immediate recognition and timely medical intervention, mortality rates are as high as 25% 7.
The most common causes of death are respiratory failure, sepsis, and gastrointestinal bleeding.
Myxedema coma carries a high mortality and morbidity rate. Therefore, timely recognition and proper management is critical. Factors suggesting a poor prognosis are older age, persistent hypothermia, or bradycardia, lower degree of consciousness by Glasgow Coma Scale, multiorgan impairment indicated by high APACHE (Acute Physiology and Chronic Health Evaluation) II score 20. The aforementioned study by Ono et al reported that, as revealed through multivariable logistic regression, a higher inhospital mortality rate was associated with older age and catecholamine use (with or without steroids) 21.
- Wiersinga WM. Myxedema and Coma (Severe Hypothyroidism) [Updated 2018 Apr 25]. In: Feingold KR, Anawalt B, Boyce A, et al., editors. Endotext [Internet]. South Dartmouth (MA): MDText.com, Inc.; 2000-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK279007[↩][↩]
- Myxedema Coma or Crisis. https://emedicine.medscape.com/article/123577-overview[↩][↩]
- Waldman SA, Park D. Myxedema coma associated with lithium therapy. Am J Med. 1989 Sep. 87 (3):355-6.[↩]
- Nicoloff JT, LoPresti JS. Myxedema coma. A form of decompensated hypothyroidism. Endocrinol Metab Clin North Am. 1993 Jun. 22(2):279-90[↩]
- Klein I. Thyroid hormone and the cardiovascular system. Am J Med. 1990 Jun. 88 (6):631-7[↩]
- Schenck JB, Rizvi AA, Lin T. Severe primary hypothyroidism manifesting with torsades de pointes. Am J Med Sci. 2006 Mar. 331 (3):154-6[↩]
- Mathew V, Misgar RA, Ghosh S, Mukhopadhyay P, Roychowdhury P, Pandit K, et al. Myxedema coma: a new look into an old crisis. J Thyroid Res. 2011. 2011:493462[↩][↩][↩]
- Kwaku MP, Burman KD. Myxedema coma. J Intensive Care Med. 2007 Jul-Aug. 22(4):224-31[↩]
- Ladenson PW, Goldenheim PD, Ridgway EC. Prediction and reversal of blunted ventilatory responsiveness in patients with hypothyroidism. Am J Med. 1988 May. 84 (5):877-83[↩]
- Ardalan MR, Ghabili K, Mirnour R, Shoja MM. Hypothyroidism-induced rhabdomyolysis and renal failure. Ren Fail. 2011. 33 (5):553-4[↩]
- Skowsky WR, Kikuchi TA. The role of vasopressin in the impaired water excretion of myxedema. Am J Med. 1978 Apr. 64 (4):613-21[↩]
- Bergeron E, Mitchell A, Heyen F, Dube S. Acute colonic surgery and unrecognized hypothyroidism: a warning. Report of six cases. Dis Colon Rectum. 1997 Jul. 40 (7):859-61[↩]
- Ji JS, Chae HS, Cho YS, Kim HK, Kim SS, et al. Myxedema ascites: case report and literature review. J Korean Med Sci. 2006 Aug. 21 (4):761-4[↩]
- Fukunaga K. Refractory gastrointestinal bleeding treated with thyroid hormone replacement. J Clin Gastroenterol. 2001 Aug. 33 (2):145-7[↩]
- Manfredi E, van Zaane B, Gerdes VE, Brandjes DP, Squizzato A. Hypothyroidism and acquired von Willebrand’s syndrome: a systematic review. Haemophilia. 2008 May. 14 (3):423-33[↩]
- Popoveniuc G, Chandra T, Sud A, Sharma M, Blackman MR, Burman KD, et al. A diagnostic scoring system for myxedema coma. Endocr Pract. 2014 Aug 1. 20(8):808-17[↩]
- Chiong YV, Bammerlin E, Mariash CN. Development of an objective tool for the diagnosis of myxedema coma. Transl Res. 2015 Sep. 166 (3):233-43[↩]
- Clinical characteristics and outcomes of myxedema coma: Analysis of a national inpatient database in Japan. Journal of Epidemiology 27 (2017) 117-122. https://www.jstage.jst.go.jp/article/jea/27/3/27_27_117/_pdf[↩]
- Guidelines for the Treatment of Hypothyroidism: Prepared by the American Thyroid Association Task Force on Thyroid Hormone Replacement. Jacqueline Jonklaas, Antonio C. Bianco, Andrew J. Bauer, Kenneth D. Burman, Anne R. Cappola, Francesco S. Celi, David S. Cooper, Brian W. Kim, Robin P. Peeters, M. Sara Rosenthal, and Anna M. Sawka. Thyroid 2014 24:12, 1670-1751 https://www.liebertpub.com/doi/full/10.1089/thy.2014.0028[↩][↩]
- Dutta P, Bhansali A, Masoodi SR, et al. Predictors of outcome in myxoedema coma: a study from a tertiary care centre. Crit Care. 2008. 12(1):R1.[↩]
- Ono Y, Ono S, Yasunaga H, Matsui H, Fushimi K, Tanaka Y. Clinical characteristics and outcomes of myxedema coma: Analysis of a national inpatient database in Japan. J Epidemiol. 2017 Mar. 27 (3):117-122[↩]