Nail dystrophy
Nail dystrophy also called onychodystrophy, is a general term that describes malformed fingernails and toenails; in this condition, the nails are often deformed, ridged, pitted or discolored. Nail dystrophy involves partial or complete disruption of the various keratinous layers of the nail plate. Nail dystrophy may result from any traumatic or inflammatory process that involves the nail matrix, nail bed, or surrounding tissues.
Nail dystrophy causes
Nail dystrophy can be caused by congenital nail diseases, systemic disorders, dermatophyte fungal nail infection (onychomycosis) and nonfungal infections, various noninfectious inflammatory dermatologic diseases of the nail unit such as psoriasis (Figure 3), atopic dermatitis (Figure 4), and lichen planus (Figure 5), lichen nitidus, pityriasis rubra pilaris, alopecia areata, and Darier’s disease and tumors 1, 2. Nail dystrophy can also occur secondarily to systemic drug use like chemotherapeutic agents are associated with nail dystrophy because they act on rapidly proliferating organs. Systemic diseases such as anemia, Raynaud’s disease, hepatic failure, chronic heart failure, renal failure, thyroiditis, inflammatory bowel disease, and chronic bronchitis also affect nail growth 3.
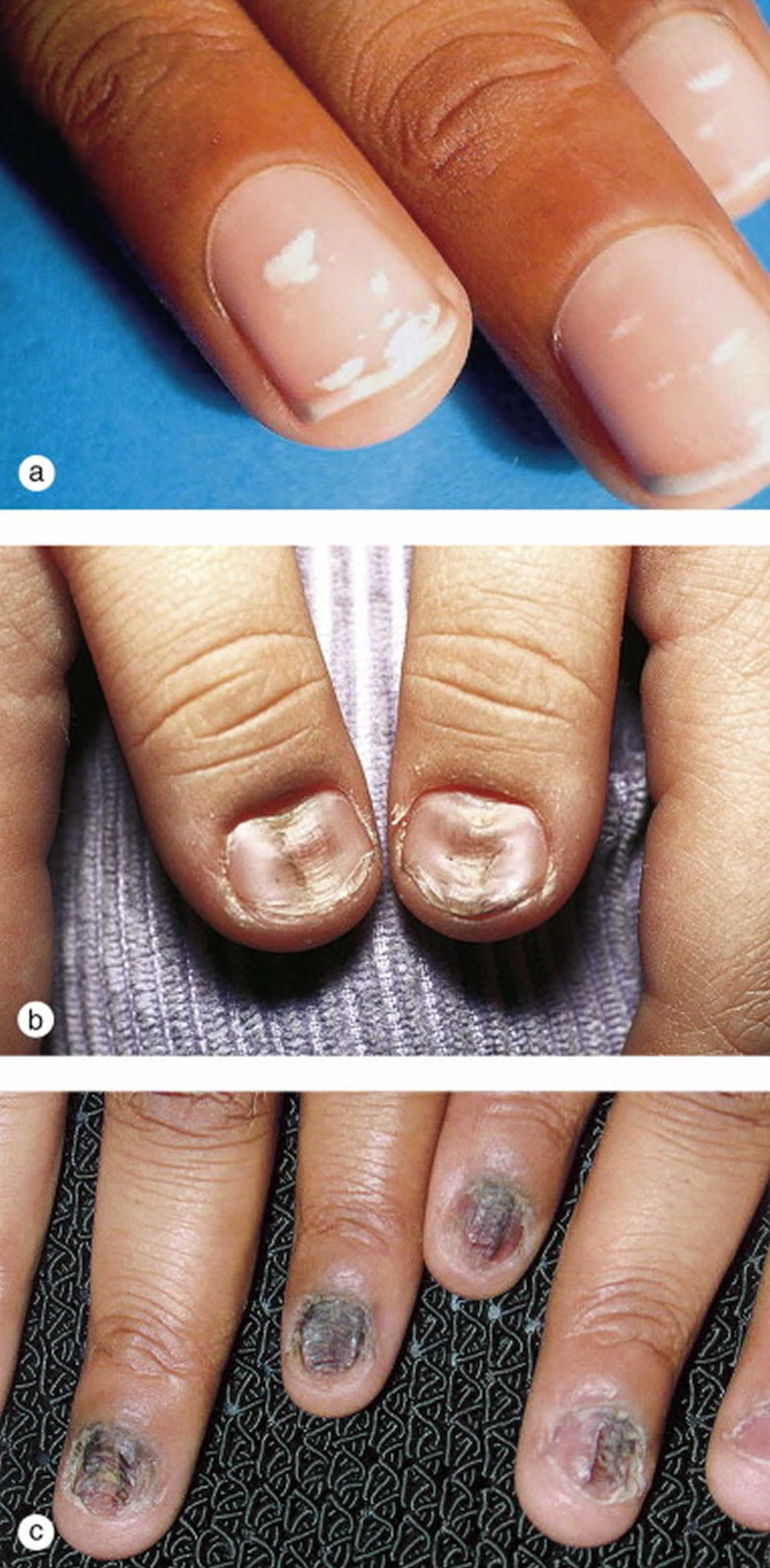
Nail biting, grooming, and chronic manipulation of any sort may also result in nail dystrophy. Repeated trauma to the cuticle may produce leukonychia (transverse white lines) and median nail dystrophy (central longitudinal ridging) see Figure 7.
Onychomycosis is the most common cause of nail dystrophy in adults, it is unusual in children before puberty (Figure 1). Dystrophic nails occur frequently as a complication of trauma (Figure 2).
Figure 1. Nail dystrophy due to onychomycosis (fungal nail infection)
Footnote: Onychomycosis. Dystrophic toenails which grew Trichophyton rubrum on fungal culture. His father had chronic athlete’s foot.
Figure 2. Traumatic nail dystrophy
Footnote: Traumatic nail dystrophy. (a) Onychoschizia (transverse splitting of the nail at the distal free edge) occurred in both great toenails as a result of recurrent trauma from basketball in this high-school athlete. (b) Green nail syndrome or chloronychia, is caused by Pseudomonas aeruginosa infection in a dystrophic great toenail that leads to a greenish discoloration of nails.
Figure 3. Nail psoriasis
Footnote: Nail psoriasis. (a) This 26-year-old male presented with pits on the fingernail surface, onycholysis, and mild subungual hyperkeratosis as well as generalized psoriatic plaques and (b) yellow, friable, flaking nails in another child with severe psoriatic arthritis.
Figure 4. Atopic nails
Footnote: Clinical pictures of nail abnormalities in patients with atopic dermatitis. (A) Transverse groove (male/12 years of age), (B) nail pitting (female/9), (C) koilonychia and trachyonychia (male/11), (D) leukonychia (male/10), (E) brachyonychia (female/15), (F) melanonychia (female/15), (G) onychomadesis (male/14), (H) onychoschizia (male/17), (I) onycholysis (male/11).
Figure 5. Lichen planus
Footnote: Characteristic nail changes in lichen planus, which include onychorrhexis (longitudinal splitting) and pterygium formation (forward growth of the skin at the proximal nail fold, which results from scarring).
Figure 6. Lichen striatus
Footnote: Lichen striatus. This healthy 7-year-old boy developed an asymmetric nail dystrophy as a linear lichenoid eruption extended down his left arm to the lateral aspect of his thumb. A biopsy of the skin showed changes typical of lichen striatus.
Figure 7. Traumatic nail changes
Footnote: Traumatic nail changes. (a) Leukonychia consists of punctate lesions or transverse white lines that grow out along the nail plate and frequently result from trauma to the nail at the cuticle. (b) Median nail dystrophy developed in this teenage boy, who admitted to chronically picking at his nails. (c) This adolescent was an obsessive nail picker. In addition to median nail dystrophy he developed crusting and hemorrhage of multiple finger and toenails.
Figure 8. Onycholysis
Footnote: This young woman developed whitening of the distal nail plate with distal separation of the nail plate from the nail bed. It can be seen in inflammatory skin disorders such as psoriasis and secondary to chemical irritants, trauma, and medications. Onycholysis resulting from sunlight exposure is called photo-onycholysis and may occur in individuals taking oral doxycycline.
Twenty nail dystrophy
Twenty-nail dystrophy also called trachyonychia, which translates to “rough nail condition” in Latin, is a condition is which the texture of the nails change. Twenty-nail dystrophy or trachyonychia is a disorder of otherwise healthy children of school age and is characterized by yellowing, loss of lustre, longitudinal ridging (alternating elevation and depression), pitting, increased friability and other dystrophic changes that progresses over 6–18 months to involve most or all of the nails giving them a roughened texture similar to sandpaper (Figure 9). Although the course is variable, in many cases the dystrophy resolves without scarring over a period of several years. 20 nail dystrophy probably includes a number of conditions that cannot be differentiated unless other cutaneous findings appear.
Figure 9. Twenty nail dystrophy
Footnote: Trachyonychia. This otherwise-healthy 9-year-old boy developed an asymptomatic nail dystrophy which progressed to involve all 20 nails. Note the increased ridging, opalescence, and sandpaper-like roughness of all his nails. These nail changes can occur in association with lichen planus, psoriasis, atopic dermatitis, and alopecia areata.
Trachyonychia causes
The cause of twenty-nail dystrophy is unknown but in some cases it appears to be associated with other skin conditions such as lichen planus, eczema, psoriasis and alopecia areata. In some cases an autosomal dominant pattern of inheritance has been found; in one report twenty-nail dystrophy occurred in 4 males in 3 successive generations. Other cases of twenty-nail dystrophy are of unknown origin and begin gradually in early childhood. These cases tend to be self-limiting and may resolve slowly with age.
Trachyonychia signs and symptoms
Twenty-nail dystrophy most commonly occurs in childhood. In one study the condition was most evident in young males in the 10-20 year old age group (52%). Slight nail abnormalities may be evident at birth with the condition slowly progressing over the years to cause changes in the texture of fingernails and toenails. Typical signs and symptoms include:
- Nails become grubby, rough and brittle
- Some nails may become distorted
- Nail examination shows longitudinal ridging, pitting, roughening and splitting
- Nails lose their lustre and may change to a muddy, greyish-white color (sand-blasted appearance)
Trachyonychia treatment
There is no specific treatment for twenty-nail dystrophy. It is a very difficult condition to treat and often results are unsatisfactory. Some treatments that have been tried include:
- Griseofulvin and other oral antifungal agents
- Systemic, topical and intralesional corticosteroids
- Topical PUVA
Treatment of any underlying cause/association should help resolve the defect of the nail. Twenty-nail dystrophy is a self-limiting condition that may clear spontaneously over several months to several years without leaving any residual scarring. Patients should be counseled and reassured that abstinence of therapy is an acceptable and safe option. If there is no associated dermatologic disease, then treatment is often unsatisfactory. Some treatments which may be tried include topical or oral steroids, topical PUVA, biotin, and topical retinoids. Cosmetically, buffing and filing of the nail plate can improve the appearance.
Follow up is necessary as twenty-nail dystrophy can precede alopecia areata, psoriasis, and lichen planus.
Median nail dystrophy
Median nail dystrophy also called median canaliform nail dystrophy, dystrophia unguium mediana canaliformis or median canaliform dystrophy of Heller 4, is a rare nail condition characterized by a midline or a paramedian ridge or split and canal formation in nail plate of one or both the thumb nails, but can affect other fingers or toes 5. It is accompanied by small lateral cracks or fissures that project from the central canal toward the nail edge. These findings give the typical fir-tree pattern appearance 6.
Median nail dystrophy is an acquired condition resulting from a temporary defect in the matrix that interferes with nail formation. Habitual picking of the nail base may be responsible for some cases. There is no sex predilection. Mean age of occurrence is 25.72 years. Typically, patients will have had the problem for a long time and have no explanation as to why the issue is present. It is thought that the condition may be related to repetitive trauma such as picking or pushing of the cuticle. Habit-tic deformity is another nail condition with a similar presentation to median nail dystrophy and is also thought to be caused by repetitive unnoticed external trauma to the nail 7. It is very difficult to distinguish the two, but if there is an inverted fir-tree pattern, this is more suggestive of median nail dystrophy. However, it is sometimes thought that the two are variants of the same disease process 7.
Median canaliform nail dystrophy diagnosis is confirmed solely on clinical findings 8.
The pathophysiology of median nail dystrophy is unclear and speculative, and there are no definitive diagnostic tests. Histopathology classically shows parakeratosis, accumulation of melanin within and between the nail bed keratinocytes. All of these factors make the management of patients with median nail dystrophy difficult.
There is also no standard therapy for treatment. Treatment of median nail dystrophy may include injectable triamcinalone acetonide, topical 0.1% tacrolimus, and tazarotene 0.05%, which is many a times challenging for a dermatologist. Psychiatric opinion should be taken when associated with the depressive, obsessive-compulsive, or impulse-control disorder 5. Spontaneous remission is often seen after a period of months to years, but the condition can be recurrent. Avoidance of repetitive nail trauma can be achieved through behavioral counseling.
Figure 10. Median canaliform dystrophy
Footnote: Median canaliform dystrophy results in a longitudinal groove in a nail plate.
Median nail dystrophy causes
The causes of median nail dystrophy is unknown. However it is theorized that median nail dystrophy is the result of a temporary defect in the nail matrix following dyskeratinization or focal infection, or due to self-inflicted trauma to the nail or nail bed, hindering normal nail formation. Median nail dystrophy has been shown to be associated with self-inflicted or job-related trauma to the nail 9. Familial cases have been reported as well 10. Median nail dystrophy development has also been reported in patients treated for acne with isotretinoin 11.
Presumably, the condition results from a temporary defect in the matrix that interferes with nail formation 12. Trauma has been implicated as a causative factor 13. Habitual picking of the nail base may be responsible for some cases. A few cases have been attributed to oral retinoid use also 14. Intentional trauma in the form of pushing back of cuticle and proximal nail fold (habitual tic) is hypothesized in its pathogenesis 15. However, subungual skin tumors such as glomus tumors 16, myxoid tumors, have also been described to cause longitudinal grooving, lifting of the nail plate from the bed resulting in a tube-like structure (solenos) distal to it. The absence of keratinocytic adhesions within nail matrix with dyskeratosis is responsible for the formation of longitudinal grove with splitting of nail plate due to weaker tensile strength 12. Histopathology classically shows parakeratosis, accumulation of melanin within and between the nail bed keratinocytes, which was not done in our case.
The main condition from which median nail dystrophy needs to be differentiated is habit tic deformity. Habit tic deformity, digital mucous cyst (synovial cyst), lichen striatus, nail-patella syndrome, pterygium, Raynaud disease, and trachyonychia are other conditions in which a longitudinal nail defect have been described 15. Habit tic deformity is usually present in one or both thumbnails and results in the alteration of normal nail growth. It is caused by the constant or habitual rubbing of the thumb’s proximal nail fold by the tip of the second digit. The subsequent damage to the nail matrix produces transverse ridges along the central nail plate depression instead of a longitudinal groove with lateral projections as in median canaliform nail dystrophy. The depth of the central nail plate canal depends on the intensity of the inflicted trauma by the index finger to the matrix of the thumb nail.
Median nail dystrophy treatment
Median nail dystrophy has no standard treatment because no therapy has consistently worked and because it often will resolve on its own without intervention 4. Stressful condition leading to depression can be the cause of median canaliform dystrophy 5. An opinion of a psychiatrist should be sought, if the patient has the depressive, obsessive–compulsive, or impulse-control disorder. Injecting triamcinolone acetonide into the dystrophic nail is one option but is difficult to tolerate and has numerous adverse effects. Recently reported treatment is the topical application of 0.1% tacrolimus ointment once daily without occlusion as also seen in our case 12. Calcineurin inhibitors are an effective treatment due to their interference with the inflammatory component. Topical tazarotene 0.05% ointment known to normalize the process of keratinization has been used by Madke et al 17. Keeping the nail length short and buffing the surface of the nail can prevent the edge of the nail plate from catching on clothing and other objects. Covering the nail plate with tape or a nail wrap also can aid in it.
- Zhang JA, Yu JB, Li XH, Zhao L. Oral and cutaneous lichenoid eruption with nail changes due to imatinib treatment in a Chinese patient with chronic myeloid leukemia. Ann Dermatol 2015;27:228-229.[↩]
- Kim IS, Lee JW, Park KY, Li K, Seo SJ, Hong CK. Nail change after chemotherapy: simultaneous development of Beau’s lines and Mees’ lines. Ann Dermatol 2012;24:238- 239.[↩]
- Fawcett RS, Linford S, Stulberg DL. Nail abnormalities: clues to systemic disease. Am Fam Physician 2004;69: 1417-1424.[↩]
- Scher R, Daniel III C. Nails: Diagnosis, Therapy, Surgery. 3rd ed. Philadelphia: Saunders; 2005. p. 252-253.[↩][↩]
- Kota R, Pilani A, Nair PA. Median Nail Dystrophy Involving the Thumb Nail. Indian J Dermatol. 2016;61(1):120. doi:10.4103/0019-5154.174092 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4763640[↩][↩][↩]
- Tosti A, Piraccini BM. Nail disorders. In: Bolognia JL, Jorizzo JL, Rapini RP, editors. Dermatology. 2nd edition. St. Louis, Mo, USA: Mosby Elsevier; 2008. p. 1031.[↩]
- Griego RD, Orengo IF, Scher RK. Median nail dystrophy and habit tic deformity: are they different forms of the same disorder? Int J Dermatol. 1995;34:799-800.[↩][↩]
- Sweeney SA, Cohen PR, Schulze KE, Nelson BR. Familial median canaliform nail dystrophy. Cutis. 2005;75:161–5.[↩]
- Kim BY, Jin SP, Won CH, Cho S. Treatment of median canaliform nail dystrophy with topical 0.1% tacrolimus ointment. J Dermatol. 2010;37(6):573-4.[↩]
- Sweeney SA, Cohen PR, Schulze KE, Nelson BR. Familial median canaliform nail dystrophy. Cutis. 2005;75(3):161-5.[↩]
- Bottomley WW, Cunliffe WJ. Median nail dystrophy associated with isotretinoin therapy. Brit J Dermatol. 1992;127(4):447-8.[↩]
- Kim BY, Jin SP, Won CH, Cho S. Treatment of median canaliform nail dystrophy with topical 0.1% tacrolimus ointment. J Dermatol. 2010;37:573–4.[↩][↩][↩]
- Olszewska M, Wu JZ, Slowinska M, Rudnicka L. The ‘PDA nail’: Traumatic nail dystrophy in habitual users of personal digital assistants. Am J Clin Dermatol. 2009;10:193–6.[↩]
- Dharmagunawardena B, Charles-Holmes R. Median canaliform dystrophy following isotretinoin therapy. Br J Dermatol. 1997;137:658–9.[↩]
- Griego RD, Orengo IF, Scher RK. Median nail dystrophy and habit tic deformity: Are they different forms of the same disorder? Int J Dermatol. 1995;34:799–800.[↩][↩]
- Verma SB. Glomus tumor-induced longitudinal splitting of nail mimicking median canaliform dystrophy. Indian J Dermatol Venereol Leprol. 2008;74:257–9.[↩]
- Madke B, Gadkari R, Nayak C. Median canaliform dystrophy of Heller. Indian Dermatol Online J. 2012;3:224–5.[↩]