Nasopharyngeal cancer
Nasopharyngeal cancer is a rare cancer arising from the epithelium of the nasopharynx, which is located behind your nose and above the back of your throat. Most nasopharyngeal cancers are nasopharyngeal carcinoma. It is by far the most common cancer in the nasopharynx. Carcinoma is another word for cancer. Carcinoma is cancer that starts in the cells that line the internal and external surfaces of the body called epithelial cells. Nasopharyngeal cancer accounts for approximately 1% of all childhood malignancies. Whereas almost all adult nasopharyngeal cancers are carcinomas, only 35-50% of nasopharyngeal malignancies are carcinomas in children. In the pediatric population, additional nasopharyngeal malignancies include rhabdomyosarcomas or lymphomas.
Nasopharyngeal cancer (nasopharyngeal carcinoma) is quite rare. In most parts of the world (including the United States), there’s less than one case for every 100,000 people each year.
Nasopharyngeal cancer is much more common in certain parts of South Asia, the Middle East, and North Africa. In some parts of China there are as many as 21 cases per 100,000 people. It’s also more common among Inuits of Alaska and Canada.
The risk of nasopharyngeal carcinoma increases slowly throughout life, but it can occur in people of any age, including children. About half of the people with nasopharyngeal carcinoma in the United States are younger than 55 years old.
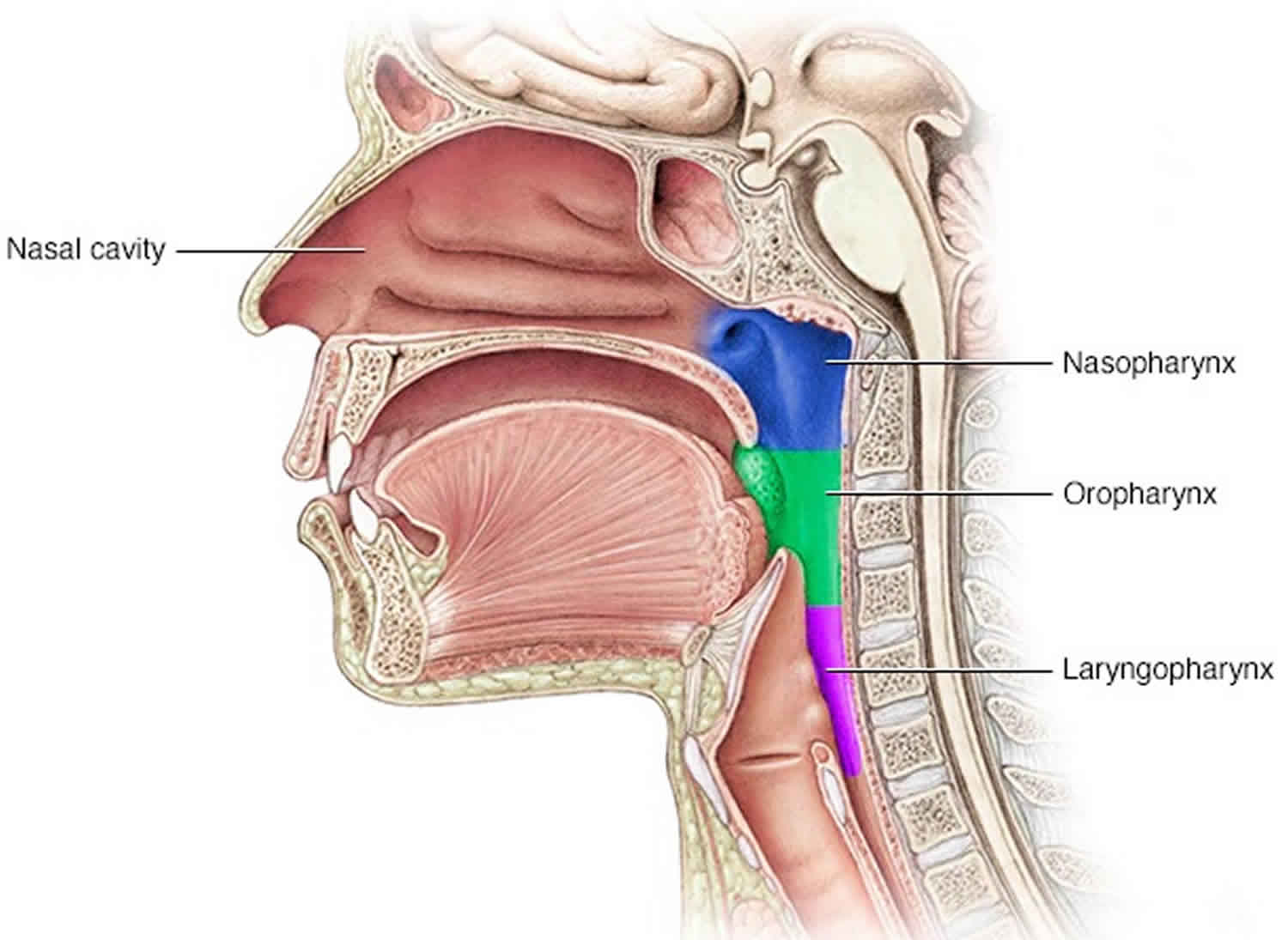
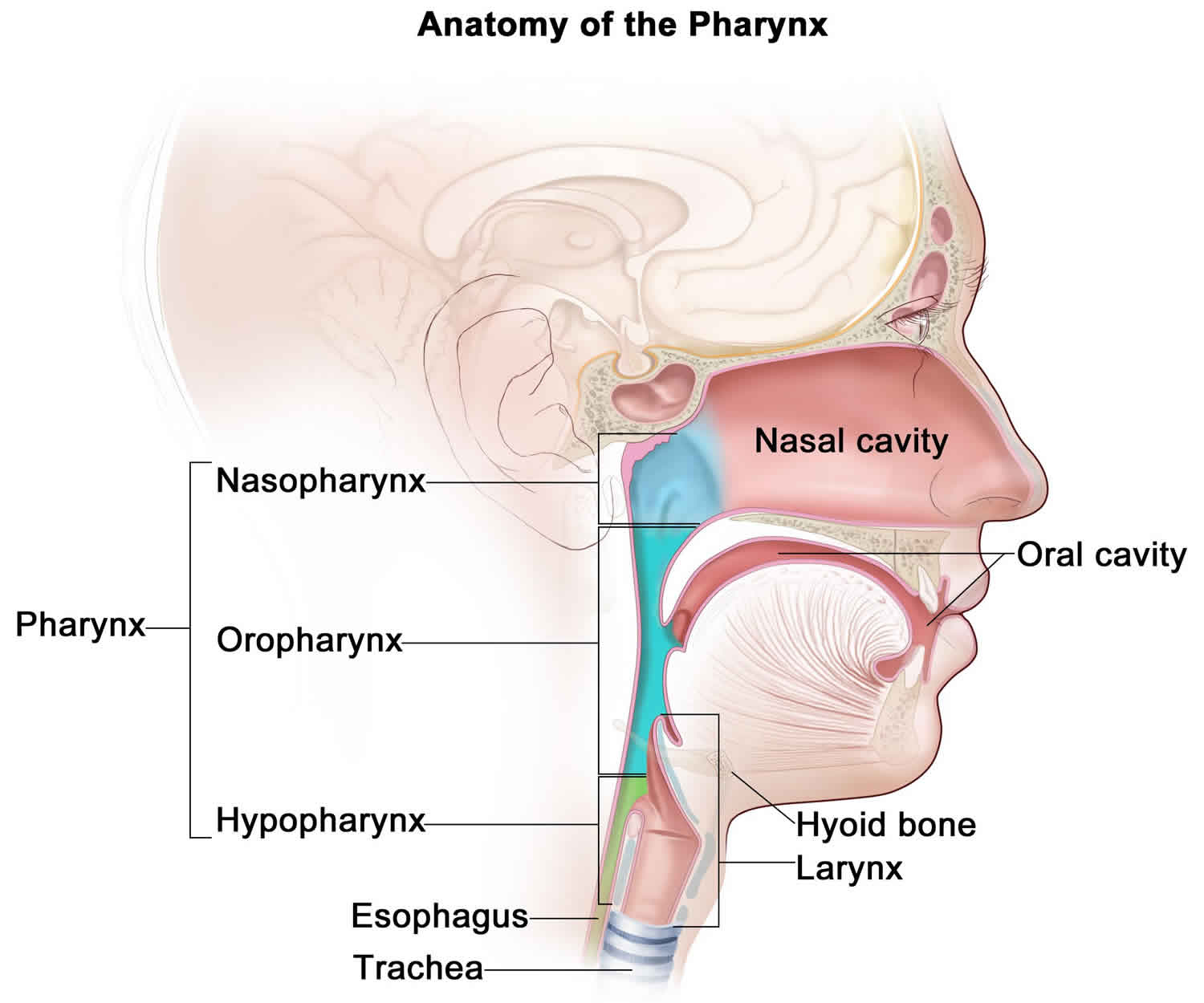
Nasopharynx anatomy
You can’t see your own nasopharynx directly. It lies above the soft area at the back of the roof of your mouth (your soft palate) and the dangly bit (uvula) at the back of your mouth. You can see these if you look inside your mouth using a mirror.
The other 2 parts of the pharynx are:
- the oropharynx – the part of the throat at the back of the mouth
- the hypopharynx – this sits behind and on either side of the larynx (voice box)
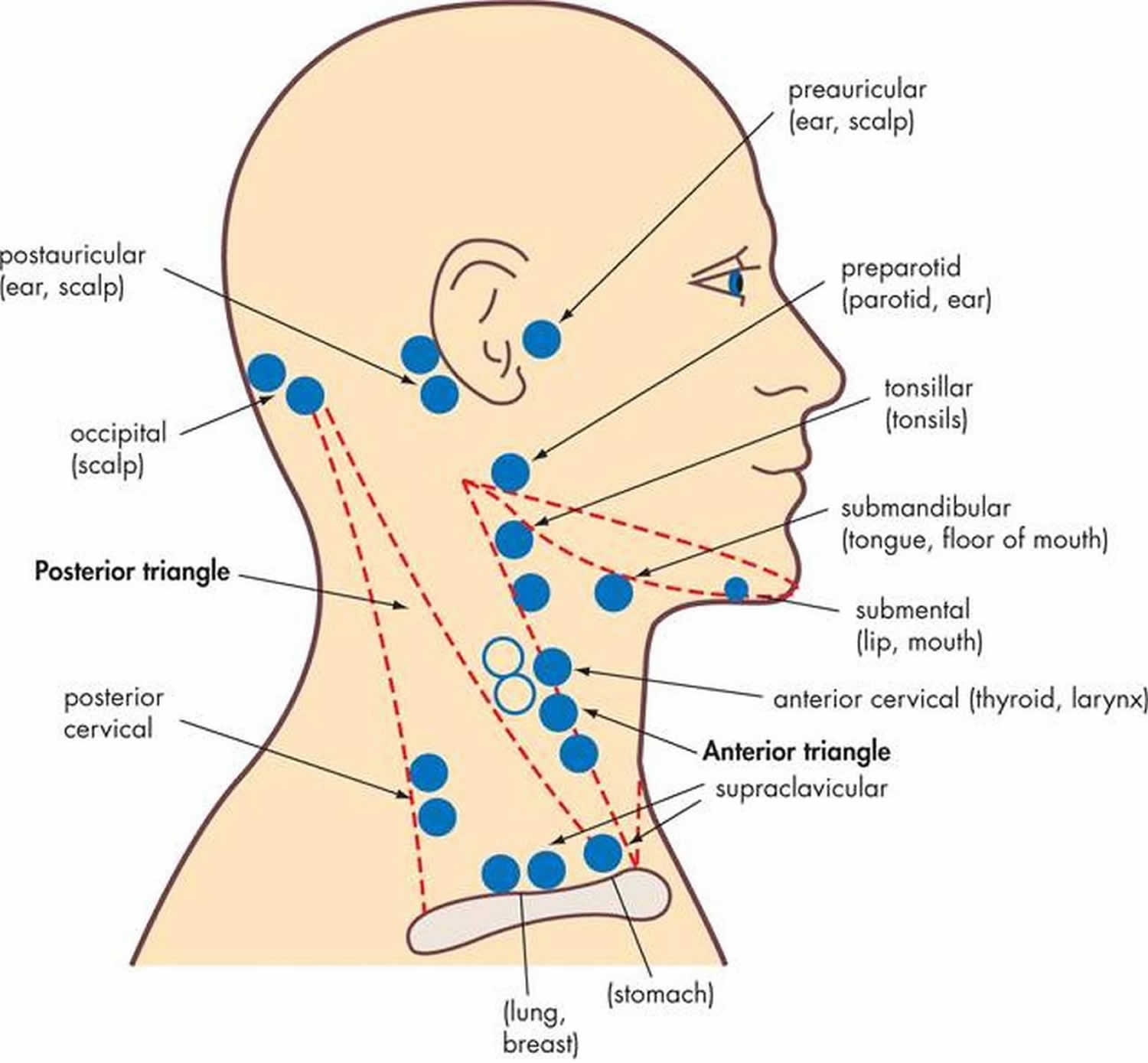
Like other parts of your body, the neck contains lymph nodes. They are also called lymph glands. These small, bean shaped glands are part of the lymphatic system, which is part of your immune system. Lymph nodes are often the first place cancer cells spread to when they break away from a tumor. There are groups of lymph nodes in your neck. If you have nasopharyngeal cancer, it might spread to these lymph nodes.
Figure 1. Nasopharynx anatomy
Nasopharyngeal tumor types
Several types of tumors can develop in the nasopharynx. Some of these tumors are benign (not cancer), but others are malignant (cancer). It’s important to talk with your doctor about what type of tumor you might have.
Nasopharyngeal carcinoma
Most nasopharyngeal cancers are nasopharyngeal carcinoma. It is by far the most common cancer in the nasopharynx. Carcinoma is cancer that starts in the cells that line the internal and external surfaces of the body (called epithelial cells).
There are 3 main types of nasopharyngeal cancer. They all start from epithelial sells that line the nasopharynx, but the cells of each type look different under a microscope:
- Non-keratinizing undifferentiated carcinoma (this is the most common type of nasopharyngeal carcinoma in the US.)
- Non-keratinizing differentiated carcinoma
- Keratinizing squamous cell carcinoma (basaloid squamous cell cancer)
Squamous cells are the flat skin-like cells that line the inside of your mouth, nose, larynx and throat. A keratinizing cancer has keratin in the cancer cells. Keratin is the protein that forms your hair and nails.
Non keratinizing cancer is the most common type of nasopharyngeal cancer. Basaloid squamous cell cancer is very rare.
All these types of nasopharyngeal cancer are treated in the same way. The non-keratinizing types tend to respond better to treatment, but the stage of the cancer – how far it has grown and spread – is often more important than the type in predicting a person’s outlook (prognosis).
Many nasopharyngeal carcinomas also contain lots of immune system cells, especially white blood cells called lymphocytes. The term lymphoepithelioma is sometimes used to describe an undifferentiated nasopharyngeal carcinoma with many lymphocytes among the cancer cells. The presence of these cells does not usually affect the choice of treatment options. But they may help researchers develop new treatments, because they may be a clue to how the body attempts to fight the tumor.
Other cancers in the nasopharynx
Other types of cancers can also be found in the nasopharynx:
- Lymphomas (non-Hodgkin lymphoma or Hodgkin lymphoma) can sometimes start in the nasopharynx. They are cancers of immune system cells called lymphocytes, which are found throughout the body, including in the nasopharynx. Lymphoma is a cancer that begins in the lymph nodes, rather than spreading to them.
- Adenocarcinoma and adenoid cystic carcinoma are cancers that can start in the minor salivary glands in the nasopharynx. But these cancers are more commonly found in the nose (nasal cavity) or mouth (oral cavity).
Nasopharyngeal cancer causes
The exact cause of most cases of nasopharyngeal cancer (nasopharyngeal carcinoma) is not known. But scientists have found that it’s linked with certain diets, infections, and inherited characteristics.
In recent years, scientists have studied how the Epstein-Barr virus (EBV) may cause cells in the nasopharynx to become cancer, but there’s still a lot to learn. In developed countries, most people infected with Epstein-Barr virus (EBV) have infectious mononucleosis (mono), and their immune system is able to recognize and destroy the virus. These people recover without any long-term problems. But in some cases, pieces of EBV DNA mix with the DNA of cells in the nasopharynx.
DNA is the chemical in each of our cells that makes up our genes, the instructions for how our cells work. For instance, we often look like our parents because they’re the source of our DNA. But DNA affects more than how we look. Some genes contain instructions that control when cells grow and divide into new cells. Viruses like Epstein-Barr virus (EBV) also contain DNA. When a cell is infected with the virus, the viral DNA may mix with the normal human DNA. Then the EBV DNA may instruct the cells of the nasopharynx to divide and grow in an abnormal way. Still, Epstein-Barr virus (EBV) infection rarely leads to nasopharyngeal carcinoma, so other factors probably play a role in whether or not it causes cancer.
For instance, eating a diet high in salt-cured fish and meat seems to increase the ability of EBV to cause nasopharyngeal carcinoma. Studies show that foods preserved in this way may produce chemicals that can damage DNA. The damaged DNA then alters a cell’s ability to control its growth and replication.
Some studies suggest that inheriting certain tissue types may contribute to a person’s risk of developing nasopharyngeal carcinoma. Because the tissue type plays a role in the function of the immune system, some scientists suspect that an abnormal immune reaction to EBV infection may be involved. The details of how certain tissue types might increase nasopharyngeal carcinoma risk are still being worked out.
Risk factors for nasopharyngeal cancer
A risk factor is anything that raises a person’s chance of getting a disease such as cancer. Different cancers have different risk factors. Some risk factors, like smoking or diet, can be changed. Others, like a person’s age or family history, can’t be changed.
But risk factors don’t tell us everything. Having a risk factor, or even many risk factors, does not mean that you will get the disease. And many people who get the disease may have few or no known risk factors.
Scientists have found risk factors that make a person more likely to develop nasopharyngeal cancer. These include:
- Gender
- Ethnicity and where you live
- Diet
- Infection with the Epstein-Barr virus
- Family history
Smoking, alcohol, and some workplace exposures may also increase the risk of this cancer.
Gender
Nasopharyngeal cancer is found about twice as often in males as it is in females.
Race/ethnicity and where you live
Nasopharyngeal cancer is most common in southern China (including Hong Kong), Singapore, Vietnam, Malaysia, and the Philippines. It’s also fairly common in Northwest Canada and Greenland.
People of south China have a lower risk of nasopharyngeal cancer if they move to another area that has lower rates of nasopharyngeal cancer (like the US or Japan), but their risk is still higher than for people who are native to areas with lower risk. Over time, their risk seems to go down. The risk also goes down in new generations. Although whites born in the United States have a low risk of nasopharyngeal cancer, whites born in China have a higher risk.
In the United States, nasopharyngeal cancer is most common in Asian and Pacific Islanders (particularly Chinese Americans), followed by American Indian and Alaskan natives, African Americans, whites, and Hispanics/Latinos.
Diet
People who live in parts of Asia, northern Africa, and the Arctic region where nasopharyngeal cancer is common, typically eat diets very high in salt-cured fish and meat. Indeed, the rate of this cancer is dropping in southeast China as people begin eating a more Westernized diet. In contrast, some studies have suggested that diets high in nuts, legumes, fruits, and vegetables and low in dairy products and meat may help lower the risk of nasopharyngeal cancer.
Epstein-Barr virus infection
Almost all nasopharyngeal cancer cells contain parts of the Epstein-Barr virus (EBV), and most people with nasopharyngeal cancer have evidence of EBV infection in their blood. Infection with EBV is very common throughout the world, often occurring in childhood. In the United States, where infection with this virus tends to occur in teens, it’s commonly known as mononucleosis (“mono”).
The link between EBV infection and nasopharyngeal cancer is complex and not yet completely understood. EBV infection alone is not enough to cause nasopharyngeal cancer, since infection with this virus is very common and this cancer is very rare. Other factors, such as a person’s genes, may affect how the body deals with EBV, which in turn may affect how EBV contributes to the development of nasopharyngeal cancer.
Family history
Family members of people with nasopharyngeal cancer are more likely to get this cancer. It’s not known if this is because of inherited genes , shared environmental factors (such as the same diet or living quarters), or some combination of these.
Just as people have different blood types, they also have different tissue types. Studies have found that people with certain inherited tissue types have an increased risk of developing nasopharyngeal cancer. Tissue types affect immune responses, so this may be related to how a person’s body reacts to EBV infection.
Other possible risk factors
- Tobacco and alcohol use: Most (but not all) studies have found that smoking may contribute to the development of nasopharyngeal cancer, especially the keratinizing type. Some studies have also linked heavy drinking to this type of cancer.
- Workplace exposures: Some studies have suggested that workplace exposure to formaldehyde increases the risk of nasopharyngeal cancer. Still, not all studies have shown this and this link isn’t clear.
Nasopharyngeal cancer prevention
Most people in the United States who develop nasopharyngeal cancer (nasopharyngeal carcinoma) have no risk factors that can be controlled, so their cancers could not have been prevented. The possible links with tobacco and heavy alcohol use are not yet clear, so we don’t know if avoiding these can lower a person’s risk of nasopharyngeal cancer. Still, both tobacco and alcohol use have clearly been linked to many other cancers, as well as other health problems, so avoiding them can have many health benefits.
Infection with Epstein-Barr virus (EBV) has been linked to nasopharyngeal cancer. Scientists are trying to create an EBV vaccine, but at this time there’s no known way to prevent this infection.
Because certain types of foods have been linked with nasopharyngeal cancer risk, reducing or not eating some types of food may lower the number of cases. This is especially true in parts of the world where nasopharyngeal cancer is common, such as southern China, northern Africa, and the Arctic region. Descendants of Southeast Asians who immigrated to the United States and eat a typical American diet, for example, have a lower risk of developing nasopharyngeal cancer. But these dietary factors are not thought to account for all cases of nasopharyngeal cancer in most other parts of the world. Other factors, such as genetics, are likely to play a part as well.
Nasopharyngeal cancer symptoms
Some people with nasopharyngeal cancer have no symptoms at all. However, most people with nasopharyngeal cancer (nasopharyngeal carcinoma) notice a lump or mass in the neck that leads them to see a doctor. There may be lumps on both sides of the neck towards the back. The lumps are usually not tender or painful. They’re caused by the cancer spreading to lymph nodes in the neck, causing them to swell. Lymph nodes are glands or organs that contain collections of immune system cells. They’re found throughout the body. Normally, they’re smaller than the size of a pea.
Other possible symptoms of nasopharyngeal cancer include:
- Hearing loss, ringing in the ear, pain, or feeling of fullness in the ear (especially on one side only)
- Ear infections that keep coming back
- Nasal blockage or stuffiness
- Nosebleeds
- Headaches
- Facial pain or numbness
- Trouble opening the mouth
- Blurred or double vision
- Trouble breathing or talking
Ear infections are common in children, but are less common in adults. If you develop an infection in one ear and you haven’t had ear infections in the past, it’s important to have a specialist examine your nasopharynx. This is especially true if you don’t have an upper respiratory tract infection (like a “cold”) along with the ear infection.
Many of the symptoms and signs of nasopharyngeal cancer are more often caused by other, less serious diseases. Still, if you have any of these problems, it’s important to see a doctor right away so the cause can be found and treated, if needed. The earlier a cancer is picked up, the easier it is to treat. And the more likely it is that the treatment will be successful.
Nasopharyngeal cancer diagnosis
Nasopharyngeal cancer is most often diagnosed when a person goes to a doctor because of symptoms such as a lump in the neck or stuffy nose, but no signs of a cold. The doctor will take a history and do an exam. The patient may then be sent to see an ear, nose and throat (ENT) specialist. The nasopharynx is hard to examine. Most other kinds of doctors do not have the specialized training or equipment to do a thorough exam of this part of the body.
Medical history and physical exam
If you have signs or symptoms that suggest you might have nasopharyngeal cancer, the doctor will want to get your complete medical history. You will be asked about the changes you’ve noticed, possible risk factors, and your family history.
A physical exam will be done to look for signs of nasopharyngeal cancer or other health problems. A more thorough exam of your nasopharynx will be done. During the exam, the doctor will pay special attention to your head and neck, including your nose, mouth, and throat; your facial muscles; and the lymph nodes in your neck. A hearing test may also be done.
Exams of the nasopharynx
The nasopharynx is deep inside the head and isn’t easily seen, so special techniques are needed to examine this area. There are 2 main types of exams used to look inside the nasopharynx for abnormal growths, bleeding, or other signs of disease. Both types are usually done in the doctor’s office.
- For indirect nasopharyngoscopy, the doctor uses special small mirrors and bright lights to look at the nasopharynx and nearby areas.
- For direct nasopharyngoscopy, a fiber-optic scope known as a nasopharyngoscope to look directly at the lining of the nasopharynx. The scope is a thin, flexible, lighted tube that’s put in through your nose. Numbing medicine is sprayed into your nose before the exam to make it easier. This is the method most often used to carefully examine the nasopharynx.
If a tumor starts under the lining of the nasopharynx (in the tissue called the submucosa), the doctor may not be able to see it. Because of this, imaging tests, like CT or MRI scans, may be needed.
Biopsy
Symptoms and the results of exams can suggest that a person might have nasopharyngeal cancer, but the only way to be sure is by taking out cells from the abnormal area and looking at them under a microscope. This is called a biopsy. Different kinds of biopsies may be done, depending on where the abnormal area is.
Endoscopic biopsy
If a suspicious growth is seen in the nasopharynx, the doctor may take out a tiny piece of it with small instruments and the aid of a fiber-optic scope. Often, biopsies of the nasopharynx are done in the operating room as an outpatient procedure. The tissue sample is then sent to a lab, where a pathologist (a doctor who specializes in diagnosing and classifying diseases in the lab) looks at it under a microscope. If the biopsy sample contains cancer cells, the pathologist sends back a report describing the type of the cancer.
Nasopharyngeal cancer cannot always be seen during an exam. If a person has symptoms suggesting nasopharyngeal cancer but nothing looks abnormal on exam, the doctor may biopsy normal-looking tissue, which may be found to contain cancer cells when looked at under the microscope.
Fine needle aspiration (FNA) biopsy
An fine needle aspiration (FNA) biopsy may be used if you have a suspicious lump in or near your neck. To do this, the doctor puts a thin, hollow needle into the lump. The needle is attached to a syringe which is used to aspirate (withdraw) a few drops of fluid containing cells and tiny bits of tissue. The skin where the needle will be inserted might be numbed with a local anesthetic, but sometimes this isn’t needed.
The cells are then looked at under a microscope to see if they’re cancer cells.
An FNA biopsy can show if an enlarged lymph node in the neck is caused by a response to an infection, the spread of cancer from somewhere else (such as the nasopharynx), or a cancer that starts in lymph nodes – which is called a lymphoma. If the cancer started somewhere else, the FNA biopsy alone might not be able to tell where it started. But if a patient already known to have nasopharyngeal cancer has enlarged neck lymph nodes, FNA can help find out if the spread of nasopharyngeal cancer caused the swelling.
Imaging tests
Imaging tests use x-rays, magnetic fields, sound waves, or radioactive particles to make pictures of the inside of your body. Imaging tests may be done for a number of reasons, including to help find a suspicious area that might be cancer, to learn how far cancer may have spread, and to help see if treatment is working.
Chest x-ray
If you’ve been diagnosed with nasopharyngeal cancer, a plain x-ray of your chest may be done to see if the cancer has spread to your lungs. This is very unlikely unless your cancer is far advanced. If the results are normal, you probably don’t have cancer in your lungs.
Computed tomography (CT) scan
The CT scan is an x-ray test that produces detailed cross-sectional images of your body.
A CT scan of the head and neck can provide information about the size, shape, and position of a tumor and can help find enlarged lymph nodes that might contain cancer. CT scans or MRIs are important in looking for cancer that may have grown into the bones at the base of the skull. This is a common place for nasopharyngeal cancer to grow. CT scans can also be used to look for tumors in other parts of the body.
Magnetic resonance imaging (MRI) scan
Like CT scans, MRI scans make detailed images of soft tissues inside the body. But MRI scans use radio waves and strong magnets instead of x-rays. A contrast material called gadolinium is often injected into a vein before the scan to better see details.
MRIs can be used to try to find out if the cancer has grown into structures near the nasopharynx. MRIs are a little better than CT scans at showing the soft tissues in the nose and throat, but they’re not quite as good for looking at the bones at the base of the skull, a common place for nasopharyngeal cancer to grow.
Positron emission tomography (PET) scan
PET scans use a form of radioactive sugar that’s put into the blood. Because cancer cells in the body are growing rapidly, they absorb large amounts of the sugar. After about an hour, you lie on the table for about 30 minutes while a special camera creates a picture of areas of radioactivity in the body. The picture is not finely detailed like a CT or MRI scan, but it provides helpful information about your whole body. Some machines are able to do both a PET and CT scan at the same time (PET/CT scan). This lets the doctor compare areas of higher radioactivity on the PET with the more detailed appearance of that area on the CT.
Your doctor may use this test to see if the cancer has spread to your lymph nodes. It can also help give the doctor a better idea of whether an abnormal area on a chest x-ray may be cancer. A PET scan can also be useful if your doctor thinks the cancer may have spread but doesn’t know where.
Blood tests
Blood tests are not used to diagnose nasopharyngeal cancer, but they may be done for other reasons, such as to help find out if the cancer has spread to other parts of the body.
Routine blood counts and blood chemistry tests
Routine blood tests can help determine a patient’s overall health. These tests can help diagnose nutrition problems, anemia (low red blood counts), liver disease, and kidney disease. And they may suggest the possibility of spread of the cancer to the liver or bone, which may lead to more testing.
Epstein-Barr virus (EBV) DNA levels
Tests to measure the blood level of EBV DNA may be done before and after treatment to help show how well treatment is working.
Nasopharyngeal cancer stages
After someone is diagnosed with nasopharyngeal cancer (nasopharyngeal carcinoma), doctors will try to figure out if it has spread, and if so, how far. This process is called staging. The stage of a cancer describes how much cancer is in the body. It’s used help know how serious the cancer is and how best to treat it. Doctors also use a cancer’s stage when talking about survival statistics.
The earliest stage of nasopharyngeal cancer is stage 0, also known as carcinoma in situ (CIS). The other stages range from I (1) through IV (4). Some stages are split further, using capital letters (A, B, etc.). As a rule, the lower the number, the less the cancer has spread. A higher number, such as stage IV, means cancer has spread more. And within a stage, an earlier letter means a lower stage. Although each person’s cancer experience is unique, cancers with similar stages tend to have a similar outlook and are often treated in much the same way.
The staging system most often used for nasopharyngeal cancer is the American Joint Committee on Cancer (AJCC) TNM system, which is based on 3 key pieces of information:
- The extent of the main tumor (T): How far has the tumor grown into nearby structures?
- The spread to nearby lymph nodes (N): Has the cancer spread to nearby lymph nodes in the neck? If so, how large are they?
- The spread (metastasis) to distant sites (M): Has the cancer spread to distant parts of the body? (The most common sites of spread are the lungs, liver, bones, or lymph nodes in distant parts of the body.)
These categories are mainly based on the results of any exams, biopsies, and imaging tests that have been done (described in How Is Nasopharyngeal Cancer Diagnosed?). Numbers or letters after T, N, and M provide more details about each of these factors.
Once the T, N, and M categories of the cancer have been determined, this information is combined in a process called stage grouping to assign an overall stage.
The system described below is the most recent American Joint Committee on Cancer (AJCC) system for nasopharyngeal cancer, effective January 2018.
Nasopharyngeal cancer staging can be complex. If you have questions about your cancer’s stage and what it might mean for you, ask your doctor to explain it to you in a way you understand.
Table 1. Nasopharyngeal cancer stages
| AJCC stage | Stage grouping | Stage description* |
| 0 | Tis N0 M0 | The tumor is only in the top layer of cells lining the inside of the nasopharynx, and has not grown any deeper (Tis). The cancer has not spread to nearby lymph nodes (N0) or to distant parts of the body (M0). |
| I | T1 N0 M0 | The tumor is in the nasopharynx. It might also have grown into the oropharynx (the part of the throat in the back of the mouth) and/or nasal cavity but no farther (T1). The cancer has not spread to nearby lymph nodes (N0) or to distant parts of the body (M0). |
|
II | T1 (or T0) N1 M0 | The tumor is in the nasopharynx. It might also have grown into the oropharynx (the part of the throat behind the mouth) and/or nasal cavity but no farther (T1). OR, no tumor is seen in the nasopharynx, but cancer is found in lymph nodes in the neck and is Epstein-Barr virus (EBV) positive, which makes it very likely to be NPC (T0). The cancer has spread to 1 or more lymph nodes on one side of the neck, or it has spread to lymph nodes behind the throat. In either case, no lymph node is larger than 6 cm (centimeters) across (N1). The cancer has not spread to distant parts of the body (M0). |
| OR | ||
| T2 N0 or N1 M0 | The tumor has grown into the tissues of the left or right sides of the upper part of the throat, but not into bone (T2). The cancer has not spread to nearby lymph nodes (N0). OR, it has spread to 1 or more lymph nodes on one side of the neck, or it has spread to lymph nodes behind the throat. In either case, no lymph node is larger than 6 cm across (N1). The cancer has not spread to distant parts of the body (M0). | |
|
III | T1 (or T0) N2 M0 | The tumor is in the nasopharynx. It might also have grown into the oropharynx (the part of the throat behind the mouth) and/or nasal cavity but no farther (T1). OR, no tumor is seen in the nasopharynx, but cancer is found in lymph nodes in the neck and is Epstein-Barr virus (EBV) positive, which makes it very likely to be NPC (T0). The cancer has spread to lymph nodes on both sides of the neck, none of which is larger than 6 cm across (N2). The cancer has not spread to distant parts of the body (M0). |
| OR | ||
| T2 N2 M0 | The tumor has grown into the tissues of the left or right sides of the upper part of the throat, but not into bone (T2). The cancer has spread to lymph nodes on both sides of the neck, none of which is larger than 6 cm across (N2). The cancer has not spread to distant parts of the body (M0). | |
| OR | ||
| T3 N0 to N2 M0 | The tumor has grown into the sinuses and/or the bones nearby (T3). The cancer might or might not have spread to nearby lymph nodes in the neck or behind the throat, but none are larger than 6 cm across (N0 to N2). The cancer has not spread to distant parts of the body (M0). | |
|
IVA | T4 N0 to N2 M0 | The tumor has grown into the skull and/or cranial nerves, the hypopharynx (lower part of the throat), the main salivary gland, or the eye or its nearby tissues (T4). The cancer might or might not have spread to nearby lymph nodes in the neck or behind the throat, but none are larger than 6 cm across (N0 to N2). The cancer has not spread to distant parts of the body (M0). |
| OR | ||
| Any T N3 M0 | The tumor might or might not have grown into structures outside the nasopharynx (any T). The cancer has spread to lymph nodes that are either larger than 6 cm across, or located in the shoulder area just above the collarbone (N3). The cancer has not spread to distant parts of the body (M0). | |
| IVB | Any T Any N M1 | The tumor might or might not have grown into structures outside the nasopharynx (any T). The cancer might or might not have spread to nearby lymph nodes (any N). The cancer has spread to distant parts of the body (M1). |
Footnote: * The following additional categories are not listed in the table above
TX: Main tumor cannot be assessed due to lack of information.
NX: Nearby lymph nodes cannot be assessed due to lack of information.
Nasopharyngeal cancer treatment
A team of doctors and other professionals discuss the best treatment and care for you. They are called a multidisciplinary team (MDT).
The treatment you have depends on:
- where your cancer is
- how far it has grown or spread (the stage)
- the type of cancer
- your general health and level of fitness
Your doctor will talk to you about your treatment, its benefits and the possible side effects.
Different types of treatment are available for patients with nasopharyngeal cancer. Some treatments are standard (the currently used treatment), and some are being tested in clinical trials. A treatment clinical trial is a research study meant to help improve current treatments or obtain information on new treatments for patients with cancer. When clinical trials show that a new treatment is better than the standard treatment, the new treatment may become the standard treatment. Patients may want to think about taking part in a clinical trial. Some clinical trials are open only to patients who have not started treatment.
Radiation therapy (radiotherapy) is the main treatment for nasopharyngeal cancer. You might have radiotherapy alone, or with chemotherapy (this is called chemoradiotherapy).
Surgery is not often used to treat nasopharyngeal cancer.
Three types of standard treatment are used:
Radiation therapy
Radiation therapy is a cancer treatment that uses high-energy x-rays or other types of radiation to kill cancer cells or keep them from growing. There are two types of radiation therapy:
External radiation therapy uses a machine outside the body to send radiation toward the cancer.
Certain ways of giving radiation therapy can help keep radiation from damaging nearby healthy tissue. These types of radiation therapy include the following:
- Intensity-modulated radiation therapy (IMRT): IMRT is a type of 3-dimensional (3-D) radiation therapy that uses a computer to make pictures of the size and shape of the tumor. Thin beams of radiation of different intensities (strengths) are aimed at the tumor from many angles. Compared to standard radiation therapy, intensity-modulated radiation therapy may be less likely to cause dry mouth.
- Stereotactic radiation therapy: A rigid head frame is attached to the skull to keep the head still during the radiation treatment. A machine aims radiation directly at the tumor. The total dose of radiation is divided into several smaller doses given over several days. This procedure is also called stereotactic external-beam radiation therapy and stereotaxic radiation therapy.
Internal radiation therapy uses a radioactive substance sealed in needles, seeds, wires, or catheters that are placed directly into or near the cancer.
The way the radiation therapy is given depends on the type and stage of the cancer being treated. External and internal radiation therapy are used to treat nasopharyngeal cancer.
External radiation therapy to the thyroid or the pituitary gland may change the way the thyroid gland works. A blood test to check the thyroid hormone level in the blood is done before and after therapy to make sure the thyroid gland is working properly. It is also important that a dentist check the patient’s teeth, gums, and mouth, and fix any existing problems before radiation therapy begins.
Chemotherapy
Chemotherapy is a cancer treatment that uses drugs to stop the growth of cancer cells, either by killing the cells or by stopping them from dividing. When chemotherapy is taken by mouth or injected into a vein or muscle, the drugs enter the bloodstream and can reach cancer cells throughout the body (systemic chemotherapy). When chemotherapy is placed directly into the cerebrospinal fluid, an organ, or a body cavity such as the abdomen, the drugs mainly affect cancer cells in those areas (regional chemotherapy). The way the chemotherapy is given depends on the type and stage of the cancer being treated.
Chemotherapy may be given after radiation therapy to kill any cancer cells that are left. Treatment given after radiation therapy, to lower the risk that the cancer will come back, is called adjuvant therapy.
Chemoradiotherapy
Having chemotherapy and radiotherapy at the same time is called chemoradiotherapy. The chemotherapy makes the cancer cells more sensitive to the radiotherapy.
You might have this treatment if your cancer has grown into the tissue around the nasopharynx, or into the nearby lymph nodes.
Chemoradiotherapy can be quite a tough treatment to have. The side effects can be more severe than the side effects of radiotherapy or chemotherapy on their own. So you have tests to see if you’re fit enough to have it.
Surgery
Surgery is a procedure to find out whether cancer is present, to remove cancer from the body, or to repair a body part. Also called an operation. Surgery is sometimes used for nasopharyngeal cancer that does not respond to radiation therapy. If cancer has spread to the lymph nodes, the doctor may remove lymph nodes and other tissues in the neck.
Clinical trial
For some patients, taking part in a clinical trial may be the best treatment choice. Clinical trials are part of the cancer research process. Clinical trials are done to find out if new cancer treatments are safe and effective or better than the standard treatment.
Many of today’s standard treatments for cancer are based on earlier clinical trials. Patients who take part in a clinical trial may receive the standard treatment or be among the first to receive a new treatment.
Patients who take part in clinical trials also help improve the way cancer will be treated in the future. Even when clinical trials do not lead to effective new treatments, they often answer important questions and help move research forward.
Patients can enter clinical trials before, during, or after starting their cancer treatment.
Some clinical trials only include patients who have not yet received treatment. Other trials test treatments for patients whose cancer has not gotten better. There are also clinical trials that test new ways to stop cancer from recurring (coming back) or reduce the side effects of cancer treatment.
Clinical trials are taking place in many parts of the country. Information about clinical trials can be found on the ClinicalTrials.gov website (https://clinicaltrials.gov/).
Treatment options by stage
Stage 1 nasopharyngeal cancer
Treatment of stage 1 nasopharyngeal cancer is usually radiation therapy to the tumor and lymph nodes in the neck.
Stage 2 nasopharyngeal cancer
Treatment of stage 2 nasopharyngeal cancer may include the following:
- Chemotherapy given with radiation therapy, followed by more chemotherapy.
- Radiation therapy to the tumor and lymph nodes in the neck.
Stage 3 nasopharyngeal cancer
Treatment of stage 3 nasopharyngeal cancer may include the following:
- Chemotherapy given with radiation therapy, which may be followed by more chemotherapy.
- Radiation therapy.
- Radiation therapy followed by surgery to remove cancer-containing lymph nodes in the neck that remain or come back after radiation therapy.
- A clinical trial of chemotherapy given before, with, or after radiation therapy.
Stage 4 nasopharyngeal cancer
Treatment of stage 4 nasopharyngeal cancer may include the following:
- Chemotherapy given with radiation therapy, followed by more chemotherapy.
- Radiation therapy.
- Radiation therapy followed by surgery to remove cancer-containing lymph nodes in the neck that remain or come back after radiation therapy.
- Chemotherapy for cancer that has metastasized (spread) to other parts of the body.
- A clinical trial of chemotherapy given before, with, or after radiation therapy.
Nasopharyngeal cancer prognosis
The results of clinical trials that include both radiation therapy and chemotherapy generally report long-term survival rates of 50-80% overall 2.
In a study by Serin et al 3, the 5-year overall survival rate was 42% with radiotherapy alone and 58% with chemoradiation (radiotherapy with chemotherapy).
Rodriguez-Galindo et al 4 reported a 4-year event-free and overall survival rate of 77% and 75%, respectively, in a Phase II Pediatric Oncology Group clinical trial using radiation alone for patients with T1-T2N0M0 disease and radiation with neoadjuvant chemotherapy for all others. Most were treated with 4 cycles of chemotherapy consisting of methotrexate, cisplatin, 5-fluorouracil, and leucovorin prior to radiotherapy.
Nasopharyngeal cancer survival rate
Survival rates can give you an idea of what percentage of people with the same type and stage of cancer are still alive a certain amount of time (usually 5 years) after they were diagnosed. They can’t tell you how long you will live, but they may help give you a better understanding of how likely it is that your treatment will be successful.
Keep in mind that survival rates are estimates and are often based on previous outcomes of large numbers of people who had a specific cancer, but they can’t predict what will happen in any particular person’s case. These statistics can be confusing and may lead you to have more questions. Talk with your doctor about how these numbers may apply to you, as he or she is familiar with your situation.
A relative survival rate compares people with the same type and stage of cancer to people in the overall population. For example, if the 5-year relative survival rate for a specific stage of nasopharyngeal cancer is 80%, it means that people who have that cancer are, on average, about 80% as likely as people who don’t have that cancer to live for at least 5 years after being diagnosed.
Table 2. 5-year relative survival rates for nasopharyngeal cancer (Based on people diagnosed with cancers of the nasopharynx between 2008 and 2014)
| SEER stage | 5-year relative survival rate |
| Localized | 82% |
| Regional | 70% |
| Distant | 51% |
| All SEER stages combined | 62% |
Footnote:
- These numbers apply only to the stage of the cancer when it is first diagnosed. They do not apply later on if the cancer grows, spreads, or comes back after treatment.
- These numbers don’t take everything into account. Survival rates are grouped based on how far the cancer has spread. But other factors, such as your age and overall health, and how well the cancer responds to treatment, can also affect your outlook.
- People now being diagnosed with nasopharyngeal cancer may have a better outlook than these numbers show. Treatments improve over time, and these numbers are based on people who were diagnosed and treated at least five years earlier.
- Localized: There is no sign that the cancer has spread outside of the nasopharynx.
- Regional: The cancer has spread outside the nasopharynx to nearby structures or lymph nodes.
- Distant: The cancer has spread to distant parts of the body, such as the lungs or liver.
Abbreviation: SEER = Surveillance, Epidemiology, and End Results.
- Nasopharyngeal Cancer Stages. https://www.cancer.org/cancer/nasopharyngeal-cancer/detection-diagnosis-staging/staging.html[↩]
- Teo PM, Chan AT, Lee WY, Leung TW, Johnson PJ. Enhancement of local control in locally advanced node-positive nasopharyngeal carcinoma by adjunctive chemotherapy. Int J Radiat Oncol Biol Phys. 1999 Jan 15. 43(2):261-71.[↩]
- Serin M, Erkal HS, Elhan AH, Cakmak A. Nasopharyngeal carcinoma in childhood and adolescence. Med Pediatr Oncol. 1998 Dec. 31(6):498-505.[↩]
- Rodriguez-Galindo C, Wofford M, Castleberry RP, et al. Preradiation chemotherapy with methotrexate, cisplatin, 5-fluorouracil, and leucovorin for pediatric nasopharyngeal carcinoma. Cancer. 2005 Feb 15. 103(4):850-7.[↩]