Nonalcoholic steatohepatitis
Nonalcoholic steatohepatitis also called NASH or metabolic dysfunction associated steatohepatitis (MASH) is a fatty liver disease characterized by fatty changes with lobular hepatitis in people who drink little or no history of excessive alcohol consumption 1, 2, 3, 4, 5, 6. Jurgen Ludwig and colleagues in July 1980, at Mayo Clinic in Rochester, Minnesota, published the first article to identify non-alcoholic steatohepatitis (NASH) 1. At the time, steatohepatitis, which is a term to describe an inflammation of the liver that is accompanied by the abnormal accumulation of fat, was thought to be caused by excessive alcohol consumption. But the Mayo study described 20 people with fatty and inflamed livers — none of whom was a heavy alcohol drinker 1. Most had some liver scarring, also known as fibrosis 1. Three of the patients had cirrhosis, liver damage that results from such scarring. The study also noted that “most patients were moderately obese, and many had obesity-associated diseases” 1. Obesity and type 2 diabetes, two conditions associated with insulin resistance, are major risk factors for the development of NASH. Accumulating evidence suggests that the hyperinsulinemia associated with insulin resistance may be important in the pathogenesis of NASH.
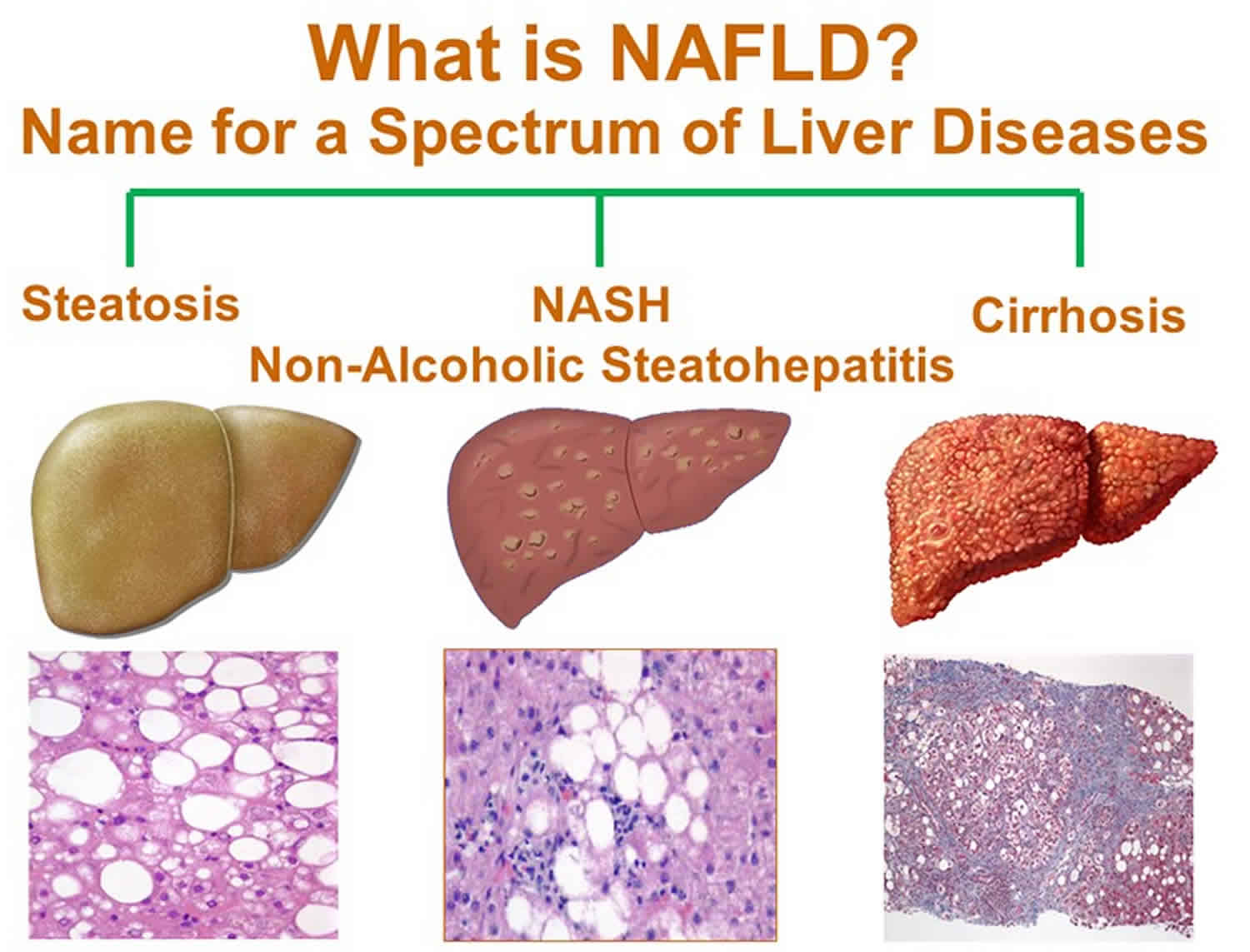
Nonalcoholic steatohepatitis (NASH) is a severe form of nonalcoholic fatty liver disease (NAFLD) now called metabolic dysfunction-associated steatotic liver disease (MASLD) a term applied to a liver disease involving the presence of too much fat in the liver cells with or without inflammation and cellular injury that is not caused by alcohol 7, 8. Nonalcoholic steatohepatitis (NASH) is the form of NAFLD in which you have inflammation of the liver and liver damage, in addition to fat in your liver. The inflammation and liver damage of NASH may lead to serious liver scarring, called cirrhosis. NASH may progress to cirrhosis, in which the liver is scarred and permanently damaged. Cirrhosis can lead to liver cancer.
Experts guess that about 10% to 24% of Americans have nonalcoholic fatty liver disease (NAFLD) and about 1.5% to 6.5% have nonalcoholic steatohepatitis (NASH) 9, 10.
A diagnosis of nonalcoholic steatohepatitis (NASH) is established by the presence of morphologic changes on liver biopsy similar to those seen in alcoholic hepatitis, including hepatocellular fat accumulation, evidence of lobular inflammation and cell injury, and in some cases, progressive fibrosis, but are found in the absence of alcohol abuse. Nonalcoholic steatohepatitis (NASH) is typically identified during the evaluation of elevated ALT (alanine aminotransferase) or AST (aspartate aminotransferase) levels after exclusion of viral, metabolic, and other causes of liver disease.
Nonalcoholic steatohepatitis (NASH) is increasingly recognized as a relatively common disorder occurring in 3% of adults that may progress to hepatic fibrosis, a precursor to cirrhosis in 15% to 40% of nonalcoholic steatohepatitis (NASH) patients 5. Cirrhosis is a condition in which your liver is scarred and permanently damaged. Scar tissue replaces healthy liver tissue and prevents your liver from working normally. Scar tissue also partly blocks the flow of blood through your liver. As cirrhosis gets worse, your liver begins to fail. Exactly how many patients with nonalcoholic steatohepatitis (NASH) progress to cirrhosis is unknown, but 1% to 2% of liver transplants are now performed because of a pretransplant diagnosis of nonalcoholic steatohepatitis (NASH).
If you have nonalcoholic steatohepatitis (NASH), you may have symptoms that could take years for them to develop. If liver damage from nonalcoholic steatohepatitis (NASH) leads to permanent scarring and hardening of your liver, this is called cirrhosis.
Symptoms from nonalcoholic steatohepatitis (NASH) may include:
- Severe tiredness
- Weakness
- Weight loss
- Yellowing of the skin or eyes (jaundice)
- Spiderlike blood vessels on your skin
- Long-lasting itchy skin.
Nonalcoholic steatohepatitis (NASH) that turns into cirrhosis could cause symptoms like fluid retention, abdominal swelling (ascites), shortness of breath, swelling of the legs, enlarged spleen, red palms, internal bleeding, muscle wasting, and confusion. People with cirrhosis over time may develop liver failure and need a liver transplant.
If you have nonalcoholic steatohepatitis (NASH), no medication is available to reverse the fat buildup in your liver. In some cases, the liver damage stops or even reverses itself. But in others, nonalcoholic steatohepatitis (NASH) continues to progress. If you have nonalcoholic steatohepatitis (NASH), it’s important to control any conditions that may contribute to fatty liver disease.
Nonalcoholic steatohepatitis (NASH) treatments and lifestyle changes may include:
- Losing weight
- Medication to reduce cholesterol or triglycerides
- Medication to reduce blood pressure
- Medication to control diabetes
- Limiting over-the-counter (OTC) drugs
- Avoiding alcohol
- Seeing a liver specialist
Some medications are being studied as possible treatments for nonalcoholic steatohepatitis (NASH). These include antioxidants like vitamin E. Scientists are also studying some new diabetes medications for nonalcoholic steatohepatitis (NASH) that may be given even if you don’t have diabetes. However, you should only take these medicines after consulting with a liver specialist.
Figure 1. Nonalcoholic steatohepatitis (NASH)
Liver anatomy
Your liver is essential to your life. You cannot live without your liver. Your liver is the largest internal organ in your body. Your liver is about the size of a football and weighs about 3 to 3.5 pounds (1.36–1.59kg). Your liver lies under your right ribs just beneath your right lung. Your liver has two lobes (sections). Your liver is made up mainly of liver cells called hepatocytes. It also has other types of cells, including cells that line its blood vessels and cells that line small tubes in the liver called bile ducts. The bile ducts carry bile from the liver to the gallbladder or directly to the intestines.
Your liver has many important functions:
- It breaks down and stores many of the nutrients absorbed from the intestine that your body needs to function. Some nutrients must be changed (metabolized) in the liver before they can be used for energy or to build and repair body tissues.
- It makes most of the clotting factors that keep you from bleeding too much when you are cut or injured.
- It delivers bile into the intestines to help absorb nutrients (especially fats).
- It breaks down alcohol, drugs, and toxic wastes in the blood, which then pass from the body through urine and stool.
Figure 2. Liver anatomy
What is nonalcoholic fatty liver disease (NAFLD)?
Nonalcoholic fatty liver disease (NAFLD) now called metabolic dysfunction-associated steatotic liver disease (MASLD) is a liver disease in which too much fat builds up in your liver. This buildup of fat is not caused by heavy alcohol use. Non-alcoholic fatty liver disease (NAFLD) is the most common form of liver disease in the world. When heavy alcohol use causes fat to build up in your liver, this condition is called alcohol-associated liver disease.
Non-alcoholic fatty liver disease (NAFLD) is seen most often in people who are overweight or obese. NAFLD is becoming more common, especially in Middle Eastern and Western nations as the number of people with obesity rises.
Non-alcoholic fatty liver disease (NAFLD) ranges in severity from nonalcoholic fatty liver (NAFL) to a more severe form of the disease called nonalcoholic steatohepatitis (NASH).
- Nonalcoholic fatty liver (NAFL). Nonalcoholic fatty liver (NAFL) is a form of NAFLD in which you have fat in your liver but little or no inflammation or liver damage. Nonalcoholic fatty liver (NAFL) typically does not progress to cause liver damage or complications. However, nonalcoholic fatty liver (NAFL) can cause pain from enlargement of the liver and have a higher risk for other health problems 9.
- Nonalcoholic steatohepatitis (NASH). Nonalcoholic steatohepatitis (NASH) is the form of NAFLD in which you have inflammation of the liver and liver damage, in addition to fat in your liver. The inflammation and liver damage of NASH can cause fibrosis, or scarring, of the liver. NASH may lead to cirrhosis, in which the liver is scarred and permanently damaged. Cirrhosis can lead to liver cancer. Furthermore, people with NASH have an increased chance of dying from liver-related causes 11. It is hard to tell apart NAFLD from NASH without a clinical evaluation and testing.
Scientists are not sure why some people with NAFLD have NASH while others have nonalcoholic fatty liver (NAFL) 12. People typically develop one type of NAFLD or the other, although sometimes people with one form are later diagnosed with the other form of NAFLD. The majority of people with NAFLD have nonalcoholic fatty liver (NAFL). Only a small number of people with NAFLD have NASH. Experts guess that about 10% to 24% of Americans have nonalcoholic fatty liver disease (NAFLD) and about 1.5% to 6.5% have nonalcoholic steatohepatitis (NASH) 9, 10.
Non-alcoholic fatty liver disease (NAFLD) is more common in people who have certain diseases and conditions, including obesity, and conditions that may be related to obesity, such as type 2 diabetes 12. Studies suggest that one-third to two-thirds of people with type 2 diabetes have NAFLD 9. Research also suggests that NAFLD is present in up to 75% of people who are overweight and in more than 90% of people who have severe obesity 13, 14.
NAFLD can affect people of any age, including children. Research suggests that close to 10% of U.S. children ages 2 to 19 have NAFLD 15. However, people are more likely to develop NAFLD as they age.
While NAFLD occurs in people of all races and ethnicities, it is most common among Hispanic individuals, followed by non-Hispanic whites and Asian Americans, including those of East Asian and South Asian descent 11, 16. NAFLD is less common among non-Hispanic Blacks 11. On average, Asian Americans with NAFLD have a lower body mass index (BMI) than non-Hispanic whites with NAFLD 16. Experts think that genes may help explain some of the racial and ethnic differences in NAFLD 12.
Non-alcoholic fatty liver disease (NAFLD) usually is a silent disease with few or no symptoms. When it does, they may include:
- Fatigue.
- Not feeling well, or malaise.
- Pain or discomfort in the upper right belly area.
People with non-alcoholic fatty liver disease (NAFLD) have a higher risk for certain health problems, including:
- Cardiovascular disease, which is the most common cause of death in people who have NAFLD 11
- Type 2 diabetes
- Metabolic syndrome
- Conditions that may be part of metabolic syndrome, such as high blood pressure and abnormal levels of fats—cholesterol and triglycerides—in the blood.
Early-stage NAFLD does not usually cause any harm, but it can lead to serious liver damage, including cirrhosis, if it gets worse.
Having high levels of fat in your liver is also associated with an increased risk of serious health problems, such as diabetes, high blood pressure and kidney disease.
If you already have diabetes, NAFLD increases your chance of developing heart problems.
If detected and managed at an early stage, it’s possible to stop NAFLD getting worse and reduce the amount of fat in your liver.
Nonalcoholic steatohepatitis causes
Scientists don’t know exactly why fat builds up in some livers and not others. They also don’t fully understand why some fatty livers turn into nonalcoholic steatohepatitis (NASH).
Non-alcoholic fatty liver disease (NAFLD) and nonalcoholic steatohepatitis (NASH) are both linked to the following 17, 18, 19, 20, 21:
- Genetics. Researchers have found that certain genes may make you more likely to develop NAFLD. These genes may help explain why NAFLD is more common in certain racial and ethnic groups. Studies have identified many genetic changes that may be associated with the development of NAFLD and NASH. Among these is a particular variation in the PNPLA3 gene 22. The PNPLA3 gene provides instructions for making a protein called adiponutrin, which is found in fat cells (adipocytes) and liver cells (hepatocytes). The function of this protein is not well understood, but it is thought to help regulate the production and breakdown of fats (lipogenesis and lipolysis) and the development of adipocytes. Studies indicate that the activity (expression) of the PNPLA3 gene decreases during periods without food (fasting) and increases after eating, suggesting that the amount of adiponutrin protein produced is regulated as needed to help process and store fats in the diet. The PNPLA3 gene variation associated with NAFLD is thought to lead to increased production and decreased breakdown of fats in the liver. Research is ongoing to determine how this and other genetic changes contribute to the development of NAFLD and its complications.
- Overweight or obesity.
- Insulin resistance, which happens when your cells don’t take up sugar in response to the hormone insulin.
- Type 2 diabetes, sometimes called high blood sugar or hyperglycemia.
- High levels of fats (abnormal levels of cholesterol—high total cholesterol, high LDL cholesterol, or low HDL cholesterol), especially triglycerides, in the blood.
These combined health problems may contribute to a fatty liver. However, some people get NAFLD even if they do not have any risk factors.
Risk factors for developing nonalcoholic steatohepatitis
Many diseases and health problems can increase your risk of non-alcoholic fatty liver disease (NAFLD), including:
- Family history of fatty liver disease or obesity.
- Growth hormone deficiency, which means the body doesn’t make enough hormones to grow.
- High cholesterol.
- High levels of triglycerides in the blood.
- Insulin resistance.
- Metabolic syndrome. Metabolic syndrome is a group of traits and medical conditions linked to overweight and obesity. Doctors define metabolic syndrome as the presence of any three of the following:
- large waist size
- high levels of triglycerides in your blood
- low levels of HDL cholesterol in your blood
- high blood pressure
- higher than normal blood glucose levels or a diagnosis of type 2 diabetes
- Obesity, especially when fat is centered in the waist.
- Polycystic ovary syndrome (PCOS).
- Obstructive sleep apnea.
- Type 2 diabetes.
- Underactive thyroid, also called hypothyroidism.
- Underactive pituitary gland, or hypopituitarism.
If you have risks for NAFLD and also drink alcohol excessively, you could have both NAFLD and alcohol-associated liver disease at the same time. No tests can easily tell how much each plays a role.
Nonalcoholic steatohepatitis (NASH) is more likely in these groups:
- People older than 50.
- People with certain genetic risk factors.
- People with obesity.
- People with diabetes or high blood sugar.
- People with symptoms of metabolic syndrome, such as high blood pressure, high triglycerides and a large waist size.
Having more of these health conditions increases your chances of developing NASH. Losing weight may cause nonalcoholic steatohepatitis (NASH) to switch to nonalcoholic fatty liver (NAFL) and regaining weight may cause nonalcoholic fatty liver (NAFL) to switch to nonalcoholic steatohepatitis (NASH).
Nonalcoholic steatohepatitis prevention
You may be able to prevent non-alcoholic fatty liver disease (NAFLD) and nonalcoholic steatohepatitis (NASH) by being physically active regularly, eating a healthy diet, limiting your portion sizes, and maintaining a healthy weight.
To reduce your risk of non-alcoholic fatty liver disease (NAFLD) and nonalcoholic steatohepatitis (NASH):
- Eat a healthy diet. Eat a healthy diet that’s rich in fruits, vegetables, whole grains and healthy fats.
- Limit alcohol, simple sugars and portion sizes. Avoid sugary drinks like soda, sports drinks, juices and sweet tea. Drinking alcohol can damage your liver and should be avoided or minimized.
- Keep a healthy weight. If you are overweight or obese, work with your health care team to gradually lose weight. If you are a healthy weight, work to keep it by eating a healthy diet and exercising.
- Exercise. Be active most days of the week. Get an OK from your health care team first if you haven’t been exercising regularly.
Nonalcoholic steatohepatitis symptoms
If you have nonalcoholic steatohepatitis (NASH), you may have symptoms that could take years for them to develop. If liver damage from nonalcoholic steatohepatitis (NASH) leads to permanent scarring and hardening of your liver, this is called cirrhosis. You may not have symptoms even if you develop cirrhosis due to NASH.
Symptoms from nonalcoholic steatohepatitis (NASH) may include:
- Severe tiredness
- Weakness
- Weight loss
- Yellowing of the skin or eyes (jaundice)
- Spiderlike blood vessels on your skin
- Long-lasting itchy skin.
Nonalcoholic steatohepatitis (NASH) that turns into cirrhosis could cause symptoms like fluid retention, abdominal swelling (ascites), shortness of breath, swelling of the legs, enlarged spleen, red palms, internal bleeding, muscle wasting, and confusion. People with cirrhosis over time may develop liver failure and need a liver transplant.
If nothing is done to stop the scarring, cirrhosis can lead to:
- Fluid buildup in the stomach area, called ascites.
- Swollen veins in your esophagus, or esophageal varices, which can rupture and bleed.
- Confusion, sleepiness and slurred speech, also called hepatic encephalopathy.
- Overactive spleen, or hypersplenism, which can cause too few blood platelets.
- Liver cancer.
- End-stage liver failure, which means the liver has stopped working.
Nonalcoholic steatohepatitis complications
The main complication of nonalcoholic steatohepatitis (NASH) is the progression of NASH to cirrhosis. Cirrhosis means permanent scarring and hardening of the liver. Cirrhosis is a condition in which your liver is scarred and permanently damaged. Your liver performs many vital functions, including filtering toxins from your blood, managing blood clotting, making bile to digest fat, storing sugar for energy, turning extra glucose into glycogen, making protein for blood plasma, and helping with digestion. Scar tissue replaces healthy liver tissue and prevents your liver from working normally. Scar tissue also partly blocks the flow of blood through your liver. As cirrhosis gets worse, your liver begins to fail and you’ll need a liver transplant. Exactly how many patients with nonalcoholic steatohepatitis (NASH) progress to cirrhosis is unknown, but 1% to 2% of liver transplants are now performed because of a pretransplant diagnosis of nonalcoholic steatohepatitis (NASH). Moreover, people with NASH have an increased chance of dying from liver-related causes 11.
Liver fibrosis and cirrhosis
The inflammation and liver cell damage that happen with nonalcoholic steatohepatitis (NASH) can cause serious health problems. The inflamed liver will start to scar, a process called fibrosis (scar tissue is a kind of fibrous tissue). If left untreated, scar tissue will continue to replace healthy liver tissue leading to cirrhosis, which is advanced, late-stage scarring. About 20% of people with NASH will progress to cirrhosis over several years typically decades. Once you’ve been diagnosed with cirrhosis, treatment will focus on keeping your condition from getting worse. It may be possible to stop or slow the liver damage. Doctors can treat the health problems caused by cirrhosis with medications, operations, and other medical procedures. It’s important to protect the healthy liver tissue you have left.
Liver failure
If cirrhosis is not treated, the liver will not be able to work well or work at all. Liver failure means that your liver is losing or has lost all of its function. When liver failure occurs as a result of cirrhosis, it usually means that your liver has been failing gradually for some time, possibly for years. If cirrhosis leads to liver failure, you may need a liver transplant.
Liver cancer
One of the complications of cirrhosis is liver cancer. Liver cancer is the growth and spread of unhealthy cells in the liver. Cancer that starts in the liver is called primary liver cancer or hepatocellular carcinoma (HCC). Hepatocellular carcinoma (HCC) is the most common type of primary liver cancer. NAFLD is now considered the third-most common cause of hepatocellular carcinoma (HCC) in the United States behind hepatitis C and alcohol induced liver disease although it is increasing more rapidly than from other conditions.
Cardiovascular disease and type 2 diabetes
The association between NAFLD and NASH with both cardiovascular disease and type 2 diabetes is bidirectional. This means that people with cardiovascular disease and/or type 2 diabetes are more likely to have NAFLD and NASH. And conversely, people with NAFLD or NASH are more likely to have cardiovascular disease and/or type 2 diabetes. In fact, cardiovascular disease is the most common cause of death in people who have either form of NAFLD.
Nonalcoholic steatohepatitis diagnosis
Doctors use your medical history, a physical exam, and tests to diagnose nonalcoholic fatty liver disease (NAFLD) including nonalcoholic fatty liver (NAFL) and nonalcoholic steatohepatitis (NASH). Because nonalcoholic fatty liver disease (NAFLD) typically causes no symptoms, it is often found when tests done for other reasons point to a liver problem. For example, your blood work may show high levels of liver enzymes, or an ultrasound of your abdomen might reveal that your liver looks enlarged, which can lead to more testing. Doctors use blood tests, imaging tests, and sometimes liver biopsy to diagnose NAFLD and to tell the difference between NAFL and NASH.
Medical history
Your doctor will ask if you have a history of health conditions or diseases that make you more likely to develop NAFLD, such as:
- overweight or obesity
- insulin resistance or type 2 diabetes
- high levels of triglycerides or abnormal levels of cholesterol in your blood
- metabolic syndrome
Your doctor will ask about your diet and lifestyle factors that may make you more likely to develop liver disease or fat in your liver.
- What medicines you take to determine whether a medicine might be causing your fatty liver.
- Your doctor will ask about your alcohol intake to find out whether fat in your liver is a sign of alcohol-associated liver disease or NAFLD. Medical tests cannot show whether alcohol is the cause of fat in the liver, so it’s important to be honest with your doctor.
- What your diet is like (eating a diet high in sugar, or drinking sugary beverages), your level of physical activity, and other lifestyle factors that can contribute to the likelihood of developing NAFLD.
Physical exam
During a physical exam, a doctor usually examines your body and checks your weight and height to calculate your body mass index (BMI). Your BMI estimates how much you should weigh based on your height. Most experts say that a BMI greater than 30 (obesity) is unhealthy. If you want to figure out your BMI on your own, there are many websites that calculate it for you when you enter your height and weight. If you have more or less muscle than is normal, your BMI may not be a perfect measure of how much body fat you have. Your doctor may also take your waist circumference and waist-to-hip ratio into consideration.
Your doctor will look for signs of nonalcoholic fatty liver (NAFL) or nonalcoholic steatohepatitis (NASH), such as:
- an enlarged liver
- signs of insulin resistance, such as darkened skin patches over your knuckles, elbows, and knees
- signs of cirrhosis, such as an enlarged spleen, ascites, spiderlike blood vessels on your skin, yellowing of your skin and whites of your eyes (jaundice) and muscle loss
Blood tests
Your doctor may take a blood sample from you and send the sample to a lab.
Your blood tests may include:
- Complete blood count.
- Iron studies, which show how much iron is in your blood and other cells.
- Liver enzyme and liver function tests.
- Tests for chronic viral hepatitis (hepatitis A, hepatitis C and others).
- Celiac disease screening test.
- Fasting blood sugar.
- Hemoglobin A1C, which shows how stable your blood sugar is.
- Lipid profile, which measures blood fats, such as cholesterol and triglycerides.
Your doctor may suspect you have NAFLD if your blood test shows increased levels of the liver enzymes alanine aminotransferase (ALT) and aspartate aminotransferase (AST). The cells in your liver contain proteins called enzymes, which are chemicals that help the liver do its work. When liver cells are damaged or destroyed, the enzymes in the cells leak out into the blood where they can be measured by blood tests. Liver enzyme testing usually checks the blood for two main enzymes:
- ALT (alanine aminotransferase)
- AST (aspartate aminotransferase)
If your liver is damaged due to inflammation, the level of these enzymes may be higher than normal. However, ALT and AST levels do not tell you how much scarring (fibrosis) may be present in your liver or predict how much liver damage will develop. In some people with NAFLD these liver enzymes may be normal as well.
Fibrosis assessment tests
These blood tests result in a score that estimates your level of liver scarring or fibrosis. They include:
- AST-to-Platelet Ratio Index (APRI) score
- Fibrosis-4 (Fib-4) score
These scores can help doctors identify or rule out advanced liver fibrosis, or scarring.
Your doctor may perform additional blood tests to find out if you have other health conditions that may increase your liver enzyme levels.
Imaging tests
Your doctor may order tests that take images, or pictures, of your liver to help make the diagnosis of liver disease. Different types of images can be obtained by using various types of equipment. However, these tests can’t show inflammation or fibrosis, so your doctor can’t use these tests to find out whether you have nonalcoholic fatty liver (NAFL) or nonalcoholic steatohepatitis (NASH). If you have cirrhosis, routine imaging tests may show nodules, or lumps, in your liver.
Your doctor may use the following imaging tests to help diagnose NAFLD:
- Abdominal ultrasound, which uses a device called a transducer that bounces safe, painless sound waves off your organs to create an image of their structure. Abdominal ultrasoundis often the first test used when liver disease is suspected.
- Computed tomography (CT) scan, which uses a combination of x-rays and computer technology to create images of your liver.
- Magnetic resonance imaging (MRI), which uses radio waves and magnets to produce detailed images of organs and soft tissues without using x-rays.
- Transient elastography, a newer type of ultrasound that measures the stiffness of your liver to determine if you have advanced liver fibrosis. Liver stiffness is a sign of fibrosis or scarring. Commonly used types of elastography are:
- Vibration-controlled transient elastography, a special type of ultrasound
- Sheer wave elastography, another type of ultrasound to detect increased liver stiffness
- Magnetic resonance elastography (MRE), is a newer, noninvasive test that combines features of ultrasound and MRI imaging to create a visual map showing gradients of stiffness throughout the liver. MRE has been shown to be a more reliable measure of liver stiffness in severely obese patients.
Liver biopsy
If other tests show signs of more-advanced liver disease or NASH, or if your test results are unclear, your doctor may suggest a liver biopsy. Liver biopsy is a procedure to remove a small piece of tissue from your liver. It is usually done using a needle through the abdominal wall. The tissue sample is looked at in a lab for signs of inflammation and scarring. Liver biopsy is the only test that can prove a diagnosis of NASH and clearly shows the amount of liver damage.
Liver biopsy can show fibrosis at earlier stages than elastography can. However, doctors don’t recommend liver biopsy for everyone with suspected NAFLD. Your doctor may recommend a liver biopsy if you are more likely to have NASH with advanced fibrosis or if your other tests show signs of advanced liver disease or cirrhosis. In some cases, doctors may recommend a liver biopsy to rule out other liver diseases.
During a liver biopsy, a doctor using a needle that is passed through the abdominal wall and into the liver will take small pieces of tissue from your liver. A pathologist will examine the tissue under a microscope to look for signs of damage or disease.
A liver biopsy can be uncomfortable, and it does have risks that your doctor will go over with you in detail.
Nonalcoholic steatohepatitis treatment
Doctors recommend weight loss, done through a combination of calorie reduction, exercise, and healthy eating, to treat nonalcoholic fatty liver disease (NAFLD), either nonalcoholic fatty liver (NAFL) or nonalcoholic steatohepatitis (NASH). Weight loss can reduce fat, inflammation, and fibrosis or scarring in your liver.
If you are overweight or have obesity, losing weight by making healthy food choices, limiting portion sizes, and being physically active can improve NAFLD either nonalcoholic fatty liver (NAFL) or nonalcoholic steatohepatitis (NASH). Losing at least 3% to 5% of your body weight can reduce fat in the liver 11. You may need to lose up to 7% to 10% of your body weight to reduce liver inflammation and fibrosis 11. Physical activity alone, even without weight loss, is also beneficial.
The best way to lose weight is done by:
- Reducing the number of calories you eat. Keeping track of the calories you consume every day and employing portion control can help.
- Eating a healthy diet that’s rich in fruits and vegetables, whole grains and low in saturated fats. Limit animal-based foods, like red meat which is high in saturated fats, and eat more plant-based foods like beans, legumes, and nuts. Use good fats like olive oil. This is the basis for the Mediterranean diet – which isn’t a diet in the traditional sense, but a healthy way of eating inspired by the eating habits of people living in the Mediterranean area and is often recommended by doctors as a way to reduce some of the risk factors associated with fatty liver disease.
- Limiting the amount of salt and sugar in your diet, particularly sugar-sweetened beverages, like soda, juices, sports drinks, and sweetened tea. High consumption of fructose, one of the main sweeteners in these beverages, increases your odds of developing obesity, type 2 diabetes, metabolic syndrome, and NAFLD.
- Limit your intake of saturated fats, which are found in meat, poultry skin, butter, shortening, milk and dairy products (except fat-free versions). Replace them with monounsaturated fats (olive, canola, and peanut oils) and polyunsaturated fats (corn, safflower, soybean oils, and many types of nuts). Particularly helpful in reducing heart disease are omega-3 fatty acids, a type of polyunsaturated fat found in oily fish such as salmon, flaxseed oil, and walnuts. Healthy eating combined with exercise – and taking cholesterol-lowering medications if prescribed by your doctor – will help keep your cholesterol and triglyceride levels where they need to be.
- Exercise and be more active – exercise is important for many reasons; it can help with weight control, boost your immune system, and alleviate stress and depression. Aim for at least 150 minutes of exercise a week. Depending on how much weight you’re trying to lose, you may need to up that amount. Getting exercise doesn’t mean you have to go to a gym – walking, gardening, and even housework counts. However, if you don’t already exercise, get your doctor’s okay first and build slowly. The goal is to participate in exercise of a moderate intensity (examples include light jogging, biking, swimming or playing a sport that boosts your heart rate and results in sweating).
Doctors recommend gradually losing weight to improve NAFLD. Rapid weight loss and malnutrition can make liver disease worse.
If you’ve tried to lose weight in the past without success, talk to your dietitian about getting help. You may also be a candidate for a medically-supervised weight loss program that employs medication along with diet and exercise. Alternatively, there are weight-loss (bariatric) surgical procedures and endoscopic therapies that work by either physically limiting the amount of food your stomach can hold, or reducing the amount of nutrients and calories your body absorbs. Talk to your doctor about which option may be best for you.
Nonalcoholic steatohepatitis diet
If you have NAFLD, your doctor may suggest changes to your diet such as:
- Limiting your intake of fats, which are high in calories and increase your chance of developing obesity.
- Replacing saturated fats and trans fats in your diet with unsaturated fats, especially omega-3 fatty acids, which may reduce your chance of heart disease if you have NAFLD.
- Eating more low-glycemic (low GI) index foods such as most fruits, vegetables, and whole grains. These foods affect your blood glucose less than high-glycemic index foods, such as white bread, white rice, and potatoes.
- Avoiding foods and drinks that contain large amounts of simple sugars, especially fructose. Fructose is found in sweetened soft drinks, sports drinks, sweetened tea, and juices. Table sugar, called sucrose, is rapidly changed to glucose and fructose during digestion and is therefore a major source of fructose.
If you have NAFLD, you should minimize alcohol use, which can further damage your liver.
Nonalcoholic steatohepatitis medicine
A new medicine called Resmetirom (Rezdiffra) can help reduce the amount of fat that collects in the liver is available to treat people who have NASH with moderate to severe liver scarring. In March 2024, the US Food and Drug Administration (FDA) approved the use of resmetirom (Rezdiffra) for people with NASH and stage 2 or 3 fibrosis (but not cirrhosis) along with eating a healthy diet and participating in regular exercise. This is the first drug approved for NASH in the United States and the approval was based on resolution of NASH and improvement in fibrosis in about a quarter of the patients treated in a large international trial 23. Resmetirom (Rezdiffra) is not recommended for people with cirrhosis. For those who have cirrhosis due to NASH, a liver transplant may be needed.
Resmetirom (Rezdiffra) drug works by revving up the thyroid hormone pathway in the liver to increase the metabolism of liver fat. The most common side effects of treatment are nausea and diarrhea. Gallstones and gallbladder inflammation also developed in some patients in the trials. It can also interact with other medications such as statins, gemfibrozil (Lopid) and clopidogrel (Plavix), so be sure that your doctor has a full list of your medications before prescribing resmetirom (Rezdiffra). A liver biopsy is not essential to start resmetirom (Rezdiffra) because other tests that can show the accumulation of liver fibrosis such as Fibroscan or other measures of liver stiffness can provide the necessary information. Resmetirom (Rezdiffra) is not for people who do not have evidence of significant liver fibrosis.
Protect your liver
Don’t do things that put extra stress on your liver:
- Avoid drinking alcohol.
- Take medications and over-the-counter drugs only as instructed by your doctor.
- Be cautious about taking dietary supplements. Certain vitamins and minerals – like vitamins A, iron, and niacin – can be harmful to your liver in higher doses than necessary or prescribed.
Check with your doctor before trying any herbal remedies. Just because a product is called “natural,” does not mean it’s safe. - Get vaccinated for hepatitis A and hepatitis B. If you get hepatitis A or B, along with fatty liver, it’s more likely to lead to liver failure.
- Manage your diabetes. Follow your doctor’s advice to manage your diabetes. Take your medicines as told by your care team and watch your blood sugar closely.
- Lower your cholesterol and blood pressure. Improve your cholesterol levels and blood pressure if they are high. A healthy diet, exercise and medicines can help keep your cholesterol, triglycerides and blood pressure at healthy levels.
Vitamin E, which is an antioxidant, in theory could help protect the liver by reducing or canceling out the damage caused by inflammation. But more research is needed. Some evidence suggests vitamin E supplements may be helpful for people with liver damage due to NAFLD and NASH who don’t have type 2 diabetes. Researchers in one study found that a daily dose of the natural form of vitamin E – the kind that comes from food sources and isn’t made in a laboratory – improved NASH in study participants overall by reducing fat and inflammation although not scarring. This medication is not for everyone and may have potential side effects as well. Vitamin E has been linked with a slightly increased risk of heart disease and prostate cancer. Discuss the potential benefits and side effects of vitamin E with your doctor.
Some studies suggest that coffee may benefit the liver by reducing the risk of liver diseases like NAFLD and lowering the chance of scarring. It’s not yet clear how coffee may prevent liver damage. But certain compounds in coffee are thought to lower inflammation and slow scar tissue growth. If you already drink coffee, these results may make you feel better about your morning cup. But if you don’t already drink coffee, this probably isn’t a good reason to start. Discuss the possible benefits of coffee with your health care team.
Nonalcoholic steatohepatitis prognosis
Patients with non-alcoholic fatty liver disease (NAFLD) exhibit increased mortality rates when compared to the general population. These patients have a high risk of mortality from cardiovascular causes as these patients have metabolic derangements. Cardiovascular causes of mortality are higher in these patients than liver causes 24. NAFLD is a slowly progressive disease; simple steatosis is reversible and non-progressive, whereas nonalcoholic steatohepatitis (NASH) can progress to cirrhosis. It is unclear why some people develop NASH. Exactly how many patients with nonalcoholic steatohepatitis (NASH) progress to cirrhosis is unknown, but 1% to 2% of liver transplants are now performed because of a pretransplant diagnosis of nonalcoholic steatohepatitis (NASH). Over a 13 year follow-up, the progression of cirrhosis presented in 41% in a study by Ekstedt et al 25. A meta-analysis done by White et al 26 showed that in cohorts of NAFLD or NASH with few or no cases of cirrhosis, the risk of developing hepatocellular carcinoma (HCC) was minimal at 0 to 3% over 20 years, and in cohorts with NASH with cirrhosis, the risk was high at 2.4 % over seven years. Losing weight and managing diabetes can slow or sometimes reverse the deposit of fat in your liver.
- Ludwig J, Viggiano TR, McGill DB, Oh BJ. Nonalcoholic steatohepatitis: Mayo Clinic experiences with a hitherto unnamed disease. Mayo Clin Proc. 1980 Jul;55(7):434-8.[↩][↩][↩][↩][↩]
- Anderson, M.L. (2006), Treating NASH. Journal of Gastroenterology and Hepatology, 21: 14-14. https://doi.org/10.1111/j.1440-1746.2005.04216.x[↩]
- CINAR, K., COBAN, S., IDILMAN, R., TUZUN, A., SARIOGLU, M., BEKTAS, M., ERDEN, E., BOZKAYA, H. and OZDEN, A. (2006), Long-term prognosis of nonalcoholic fatty liver disease: Is pharmacological therapy actually necessary?. Journal of Gastroenterology and Hepatology, 21: 169-173. https://doi.org/10.1111/j.1440-1746.2005.04221.x[↩]
- Neuschwander-Tetri BA. Fatty liver and nonalcoholic steatohepatitis. Clin Cornerstone. 2001;3(6):47-57. doi: 10.1016/s1098-3597(01)90078-x[↩]
- Neuschwander-Tetri BA. Evolving pathophysiologic concepts in nonalcoholic steatohepatitis. Curr Gastroenterol Rep. 2002 Feb;4(1):31-6. doi: 10.1007/s11894-002-0035-x[↩][↩]
- Drew L. Fatty liver disease: turning the tide. Nature. 2017 Oct 11;550(7675):S101. https://doi.org/10.1038/550S101a[↩]
- Nonalcoholic Fatty Liver Disease (NAFLD). https://liverfoundation.org/liver-diseases/fatty-liver-disease/nonalcoholic-fatty-liver-disease-nafld[↩]
- Nonalcoholic Steatohepatitis (NASH). https://liverfoundation.org/liver-diseases/fatty-liver-disease/nonalcoholic-steatohepatitis-nash[↩]
- Younossi ZM, Koenig AB, Abdelatif D, Fazel Y, Henry L, Wymer M. Global epidemiology of nonalcoholic fatty liver disease—meta-analytic assessment of prevalence, incidence, and outcomes. Hepatology. 2016;64(1):73–84. doi:10.1002/hep.28431[↩][↩][↩][↩]
- Nonalcoholic fatty liver disease. https://www.mayoclinic.org/diseases-conditions/nonalcoholic-fatty-liver-disease/symptoms-causes/syc-20354567[↩][↩]
- Chalasani N, Younossi Z, Lavine JE, et al. The diagnosis and management of nonalcoholic fatty liver disease: practice guidance from the American Association for the Study of Liver Diseases. Hepatology. 2018;67(1):328–357. doi:10.1002/hep.29367[↩][↩][↩][↩][↩][↩][↩]
- Nonalcoholic Fatty Liver Disease (NAFLD) & NASH. https://www.niddk.nih.gov/health-information/liver-disease/nafld-nash[↩][↩][↩]
- Cotter TG, Rinella M. Nonalcoholic fatty liver disease 2020: the state of the disease. Gastroenterology. 2020;158(7):1851–1864. doi:10.1053/j.gastro.2020.01.052[↩]
- Machado M, Marques-Vidal P, Cortez-Pinto H. Hepatic histology in obese patients undergoing bariatric surgery. Journal of Hepatology. 2006;45(4):600–606. doi: 10.1016/j.jhep.2006.06.013[↩]
- Schwimmer JB, Deutsch R, Kahen T, Lavine JE, Stanley C, Behling C. Prevalence of fatty liver in children and adolescents. Pediatrics. 2006;118(4):1388–1393. doi: 10.1542/peds.2006-1212[↩]
- Golabi P, Paik J, Hwang JP, Wang S, Lee HM, Younossi ZM. Prevalence and outcomes of non-alcoholic fatty liver disease (NAFLD) among Asian American adults in the United States. Liver International. 2019;39(4):748–757. doi:10.1111/liv.14038[↩][↩]
- Kudaravalli P, John S. Nonalcoholic Fatty Liver. [Updated 2023 Apr 7]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK541033[↩]
- Kim CH, Younossi ZM. Nonalcoholic fatty liver disease: a manifestation of the metabolic syndrome. Cleve Clin J Med. 2008 Oct;75(10):721-8. doi: 10.3949/ccjm.75.10.721[↩]
- Rector RS, Thyfault JP, Wei Y, Ibdah JA. Non-alcoholic fatty liver disease and the metabolic syndrome: an update. World J Gastroenterol. 2008 Jan 14;14(2):185-92. doi: 10.3748/wjg.14.185[↩]
- Brennan PN, Elsharkawy AM, Kendall TJ, Loomba R, Mann DA, Fallowfield JA. Antifibrotic therapy in nonalcoholic steatohepatitis: time for a human-centric approach. Nat Rev Gastroenterol Hepatol. 2023 Oct;20(10):679-688. doi: 10.1038/s41575-023-00796-x[↩]
- Kim K, Kim KH. Targeting of Secretory Proteins as a Therapeutic Strategy for Treatment of Nonalcoholic Steatohepatitis (NASH). Int J Mol Sci. 2020 Mar 26;21(7):2296. doi: 10.3390/ijms21072296[↩]
- PNPLA3 gene. https://medlineplus.gov/genetics/gene/pnpla3[↩]
- Harrison SA, Bedossa P, Guy CD, et al. MAESTRO-NASH Investigators. A Phase 3, Randomized, Controlled Trial of Resmetirom in NASH with Liver Fibrosis. N Engl J Med. 2024 Feb 8;390(6):497-509. doi: 10.1056/NEJMoa2309000[↩]
- Machado MV, Cortez-Pinto H. Non-alcoholic fatty liver disease: what the clinician needs to know. World J Gastroenterol. 2014 Sep 28;20(36):12956-80. doi: 10.3748/wjg.v20.i36.12956[↩]
- Ekstedt M, Franzén LE, Mathiesen UL, Thorelius L, Holmqvist M, Bodemar G, Kechagias S. Long-term follow-up of patients with NAFLD and elevated liver enzymes. Hepatology. 2006 Oct;44(4):865-73. doi: 10.1002/hep.21327[↩]
- White DL, Kanwal F, El-Serag HB. Association between nonalcoholic fatty liver disease and risk for hepatocellular cancer, based on systematic review. Clin Gastroenterol Hepatol. 2012 Dec;10(12):1342-1359.e2. doi: 10.1016/j.cgh.2012.10.001[↩]