Omphalitis
Omphalitis is an bacterial infection of the umbilical cord stump, the umbilicus and/or surrounding tissues, occurring primarily in the neonatal period 1. Omphalitis typically presents as a superficial cellulitis that can spread to involve the entire abdominal wall and may progress to necrotizing fasciitis, myonecrosis, or systemic disease 2. Omphalitis is a true medical emergency that can rapidly progress to systemic infection and death, with an estimated mortality rate between 7% and 15% 3. Early recognition and treatment are essential to prevent the morbidity and mortality associated with omphalitis.
The umbilical cord is the lifeline between the baby and mother during pregnancy and is cut after birth. The umbilical cord stump then gradually dries and typically falls off within 5 to 15 days. Both skin and enteric bacteria may colonize the devitalized tissue of the stump and lead to infection. Omphalitis is, therefore, a polymicrobial infection and the most common pathogens are Staphylococcus aureus, Streptococcus pyogenes, and gram-negative bacteria such as Escherichia coli, Klebsiella pneumoniae, and Proteus mirabilis 4. If maternal infection with chorioamnionitis is suspected, anaerobic bacteria such as Bacteroides fragilis, Clostridium perfringens, and Clostridium tetani can also contribute to infection 5.
Omphalitis is uncommon outside of the neonatal period. Symptoms typically begin at an average age of 3 days. Omphalitis is a rare disease in developed countries, with an incidence of 0.7%. However, in developing countries, the incidence of neonates delivered at hospitals can approach 8%, and if born at home, the incidence can be as high as 22% 6. Risk factors for the development of omphalitis include the following: low birth weight, prolonged rupture of membranes, maternal infection, umbilical catheterization, nonsterile delivery, maternal infection, prolonged labor, home birth, and improper cord care. Cultural application of cow dung is also associated with higher rates of omphalitis. In addition, immune system abnormalities such as defects in leukocyte adhesion, neutrophil or natural killer lymphocyte function, and interferon production have been associated with an increased risk of omphalitis 7.
Omphalitis in newborn staging
Staging of neonatal omphalitis is as follows 8:
- Grade 1: Funisitis with purulent umbilical discharge that may be malodorous
- Grade 2: Funisitis with purulent umbilical discharge that may be malodorous with periumbilical abdominal wall cellulitis
- Grade 3: Funisitis with purulent umbilical discharge that may be malodorous, the presence of periumbilical abdominal wall cellulitis, and systemic involvement, including sepsis, shock, disseminated intravascular coagulation, multiple organ dysfunction
- Grade 4: Funisitis with purulent umbilical discharge that may be malodorous; the presence of periumbilical abdominal wall cellulitis, ecchymosis, crepitus, bullae; with evidence of involvement of superficial and deep fascia and associated muscle; and with systemic involvement, including sepsis, shock, disseminated intravascular coagulation, multiple organ dysfunction
Omphalitis causes
Immediately after birth, the umbilicus becomes colonized with many different types of bacteria. Gram-positive cocci are present within hours, followed shortly by the presence of many enteric microorganisms. The devitalized tissues of the umbilical stump promote rapid growth of these bacteria, and the thrombosed blood vessels allow entry into the bloodstream, potentially leading to systemic infection.
Associated risk factors for omphalitis of newborn include the following:
- Low birth weight (< 2500 g)
- Prior umbilical catheterization
- Septic delivery (as suggested by premature rupture of membranes, nonsterile delivery, or maternal infection)
- Prolonged rupture of membranes
Omphalitis occasionally manifests from an underlying immunologic disorder. Leukocyte adhesion deficiency is most prominent among the immunodeficiency syndromes 9. Numerous infants with acute or chronic omphalitis have been diagnosed with leukocyte adhesion deficiency, a rare immunologic disorder with an autosomal recessive pattern of inheritance. These infants typically present with the following:
- Leukocytosis
- Delayed separation of the umbilical cord, with or without omphalitis
- Recurrent infections
Omphalitis may also be the initial manifestation of neutrophil disorders in the neonate, including neonatal alloimmune neutropenia and congenital neutropenia 10. Affected infants may present with other cutaneous infections, pneumonia, sepsis, and meningitis.
Neonatal alloimmune neutropenia is a disease analogous to Rh-hemolytic disease and results from maternal sensitization to fetal neutrophils bearing antigens that differ from the mother’s 11. Maternal immunoglobulin G antibodies cross the placenta and result in an immune-mediated neutropenia that can be severe and last for several weeks to 6 months 12.
The congenital neutropenias are a disease group of heterogeneous disorders that range from intermittent to persistent manifestations of varying severity 13.
Because omphalitis complicated by sepsis can also be associated with neutropenia, the underlying immune-mediated neutrophil destruction may not be immediately appreciated in affected newborns.
Rarely, an anatomic abnormality such as a patent urachus, a patent omphalomesenteric duct, or a urachal cyst may be present 14.
Omphalitis prevention
Prevention of omphalitis requires both aseptic techniques during delivery services and proper cord care. The umbilical cord should be cut with a sterile blade or scissors. In the hospital setting where aseptic care is routine, and the risk of omphalitis is low, dry cord care is recommended. In developing countries with a higher risk of omphalitis, chlorhexidine as a topical agent has been shown to reduce the risk of omphalitis inexpensively. In a meta-analysis of studies conducted in community settings of developing countries, the use of chlorhexidine reduced all-cause mortality and the risk of omphalitis when compared to dry cord care 15. Inappropriate cord care has also been shown to increase the risk of umbilical infection. Cultural application of cow dung or bentonite clay to the umbilical stump has resulted in neonatal tetanus 16.
Omphalitis symptoms
Omphalitis is primarily a disease of the neonate and is characterized by tenderness, erythema, and induration of the umbilicus and surrounding tissues. Early on, patients may only have superficial cellulitis but, if untreated, this can progress to involve the entire abdominal wall. Patients may also have purulent drainage or be bleeding from the umbilical cord stump. Foul-smelling drainage should raise the suspicion of anaerobic infection. Systemic symptoms such as lethargy, poor feeding, fever, and irritability suggest sepsis and portend a worse prognosis. If there is a rapid progression of abdominal wall erythema or gas in the surrounding tissues, necrotizing fasciitis should be considered, and acute surgical consultation is needed 17.
Local disease
Physical signs of omphalitis vary with the extent of the disease. Signs of localized infection include the following:
- Purulent or malodorous discharge from the umbilical stump
- Periumbilical erythema (Recently, algorithms that attempt to standardize the clinical diagnosis of omphalitis have been developed, emphasizing extent of periumbilical erythema and absence or presence of pus.)
- Edema
- Tenderness
Extensive local disease with extension
The following signs indicate more extensive local disease, such as necrotizing fasciitis or myonecrosis, which are typically found in a periumbilical location but may spread across the abdominal wall, onto the flanks and back, and into the scrotum. These signs may also suggest infection by both aerobic and anaerobic organisms and include the following:
- Ecchymoses, violaceous discoloration
- Bullae
- Peau d’orange appearance
- Crepitus
- Petechiae
- Progression of cellulitis despite antimicrobial therapy
Systemic disease
Signs of sepsis or other systemic disease are nonspecific and include disturbances of thermoregulation or evidence of dysfunction of multiple organ systems. Examples include the following:
- Disturbances of thermoregulation: Fever (temperature > 100.4 °F [>38°C]), hypothermia (temperature < 96.8 °F [< 36°C]), or temperature instability
- Cardiovascular disturbances: Tachycardia (pulse >180 beats per minute [bpm]), hypotension (systolic blood pressure < 60 mm Hg in full-term infants), or delayed capillary refill (< 2-3 seconds)
- Respiratory disturbances: Apnea, tachypnea (respirations >60/min), grunting, flaring of the alae nasi, intercostal or subcostal retractions, or hypoxemia
- Gastrointestinal tract disturbances: Rigid or distended abdomen or absent bowel sounds
- Cutaneous abnormalities: Jaundice, petechiae, or cyanosis
- Neurologic abnormalities: Irritability, lethargy, weak sucking, hypotonia, or hypertonia.
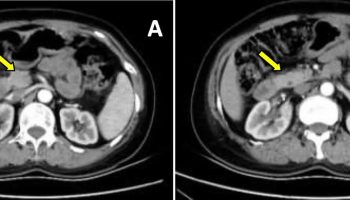
Omphalitis complications
Early recognition and treatment of omphalitis are essential to prevent the serious complications of omphalitis. Sepsis is the most common complication and can progress to septic shock and death. Other rare complications include peritonitis, intestinal gangrene, small bowel evisceration, liver abscess, septic umbilical arteritis, and portal vein thrombosis. Although uncommon, necrotizing fasciitis can occur and should be suspected if there is a rapid progression of infection and signs of systemic toxicity. It should also be suspected if there is no clinical improvement with intravenous antibiotics in 24 to 48 hours. Mortality rates as high as 60% to 85% have been reported in patients with omphalitis complicated by necrotizing fasciitis 18. If suspected, in addition to broad-spectrum antibiotics, prompt surgical consultation for debridement of the umbilical structures and the involved abdominal wall is essential.
Omphalitis diagnosis
Laboratory evaluation with complete blood count and culture should be obtained for all patients with suspected omphalitis. In addition, cultures of any purulent material from the umbilical stump should be sent prior to initiation of antibiotics if possible. If the patient has systemic symptoms, a full neonatal septic workup including chest radiograph, urinalysis, urine culture, and cerebrospinal fluid culture should be obtained.
Omphalitis treatment
Broad spectrum parenteral antibiotics are required to treat omphalitis. Antibiotic coverage should be directed against both gram-positive and gram-negative organisms. Initial empiric treatment with antistaphylococcal penicillin and aminoglycoside is recommended. If there is a high prevalence of methicillin-resistant Staphylococcus aureus, vancomycin should be administered while awaiting culture results. If there is suspicion for maternal chorioamnionitis or the patient has foul-smelling discharge from the stump, clindamycin or metronidazole is indicated to cover for anaerobes 5. The duration of antibiotic therapy depends on the patient’s clinical response and any complications that may develop during hospital admission. For uncomplicated cases of omphalitis, the recommended course of parenteral therapy is ten days, followed by a switch to oral therapy depending on culture results.
Omphalitis prognosis
The prognosis for infants with omphalitis varies.
Outcome is usually favorable in infants with uncomplicated omphalitis associated with cellulitis of the anterior abdominal wall. In a study by Sawin and colleagues, no deaths occurred among 32 infants with omphalitis in the absence of necrotizing fasciitis and myonecrosis 19. The mortality rate among all infants with omphalitis, including those who develop complications, is estimated at 7%-15%. The mortality rate is significantly higher (38%-87%) after the development of necrotizing fasciitis or myonecrosis. Suggested risk factors for poor prognosis include male sex, prematurity or being small for gestational age, and septic delivery (including unplanned home delivery); however, data are limited and conclusions cannot be drawn regarding the role of these factors in the mortality rate.
References- Painter K, Feldman J. Omphalitis. [Updated 2019 Jun 4]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK513338
- Omphalitis. https://emedicine.medscape.com/article/975422-overview
- Güvenç H, Aygün AD, Yaşar F, Soylu F, Güvenç M, Kocabay K. Omphalitis in term and preterm appropriate for gestational age and small for gestational age infants. J. Trop. Pediatr. 1997 Dec;43(6):368-72.
- Faridi MM, Rattan A, Ahmad SH. Omphalitis neonatorum. J Indian Med Assoc. 1993 Nov;91(11):283-5.
- Brook I. Cutaneous and subcutaneous infections in newborns due to anaerobic bacteria. J Perinat Med. 2002;30(3):197-208.
- Mir F, Tikmani SS, Shakoor S, Warraich HJ, Sultana S, Ali SA, Zaidi AK. Incidence and etiology of omphalitis in Pakistan: a community-based cohort study. J Infect Dev Ctries. 2011 Dec 13;5(12):828-33.
- Davies EG, Isaacs D, Levinsky RJ. Defective immune interferon production and natural killer activity associated with poor neutrophil mobility and delayed umbilical cord separation. Clin. Exp. Immunol. 1982 Nov;50(2):454-60.
- Bradley JS, Nizet V. Staphylococcal infections. In: Wilson CB, Nizet V, Maldonado YA, Remington JS, Klein JO, eds. Remington and Klein’s Infectious Diseases of the Fetus and Newborn Infant. 8th ed. Philadelphia, PA: Elsevier Saunders; 2016. 487.
- Deshpande P, Kathirvel K, Alex AA, et al. Leukocyte adhesion deficiency-I: clinical and molecular characterization in an Indian population. Indian J Pediatr. 2016 Aug. 83(8):799-804.
- Shim YJ, Kim HJ, Suh JS, Lee KS. Novel ELANE gene mutation in a Korean girl with severe congenital neutropenia. J Korean Med Sci. 2011 Dec. 26(12):1646-9.
- van den Tooren-de Groot R, Ottink M, Huiskes E, et al. Management and outcome of 35 cases with foetal/neonatal alloimmune neutropenia. Acta Paediatr. 2014 Nov. 103(11):e467-74.
- Porcelijn L, de Haas M. Neonatal alloimmune neutropenia. Transfus Med Hemother. 2018 Oct. 45(5):311-6.
- Skokowa J, Dale DC, Touw IP, Zeidler C, Welte K. Severe congenital neutropenias. Nat Rev Dis Primers. 2017 Jun 8. 3:17032.
- Razvi S, Murphy R, Shlasko E, Cunningham-Rundles C. Delayed separation of the umbilical cord attributable to urachal anomalies. Pediatrics. 2001 Aug. 108(2):493-4.
- Sinha A, Sazawal S, Pradhan A, Ramji S, Opiyo N. Chlorhexidine skin or cord care for prevention of mortality and infections in neonates. Cochrane Database Syst Rev. 2015 Mar 05;(3):CD007835
- Centers for Disease Control and Prevention (CDC). Neonatal tetanus–Montana, 1998. MMWR Morb. Mortal. Wkly. Rep. 1998 Nov 06;47(43):928-30.
- Ameh EA, Nmadu PT. Major complications of omphalitis in neonates and infants. Pediatr. Surg. Int. 2002 Sep;18(5-6):413-6.
- Hsieh WS, Yang PH, Chao HC, Lai JY. Neonatal necrotizing fasciitis: a report of three cases and review of the literature. Pediatrics. 1999 Apr;103(4):e53.
- Sawin RS, Schaller RT, Tapper D, et al. Early recognition of neonatal abdominal wall necrotizing fasciitis. Am J Surg. 1994 May. 167(5):481-4.