Peak inspiratory pressure
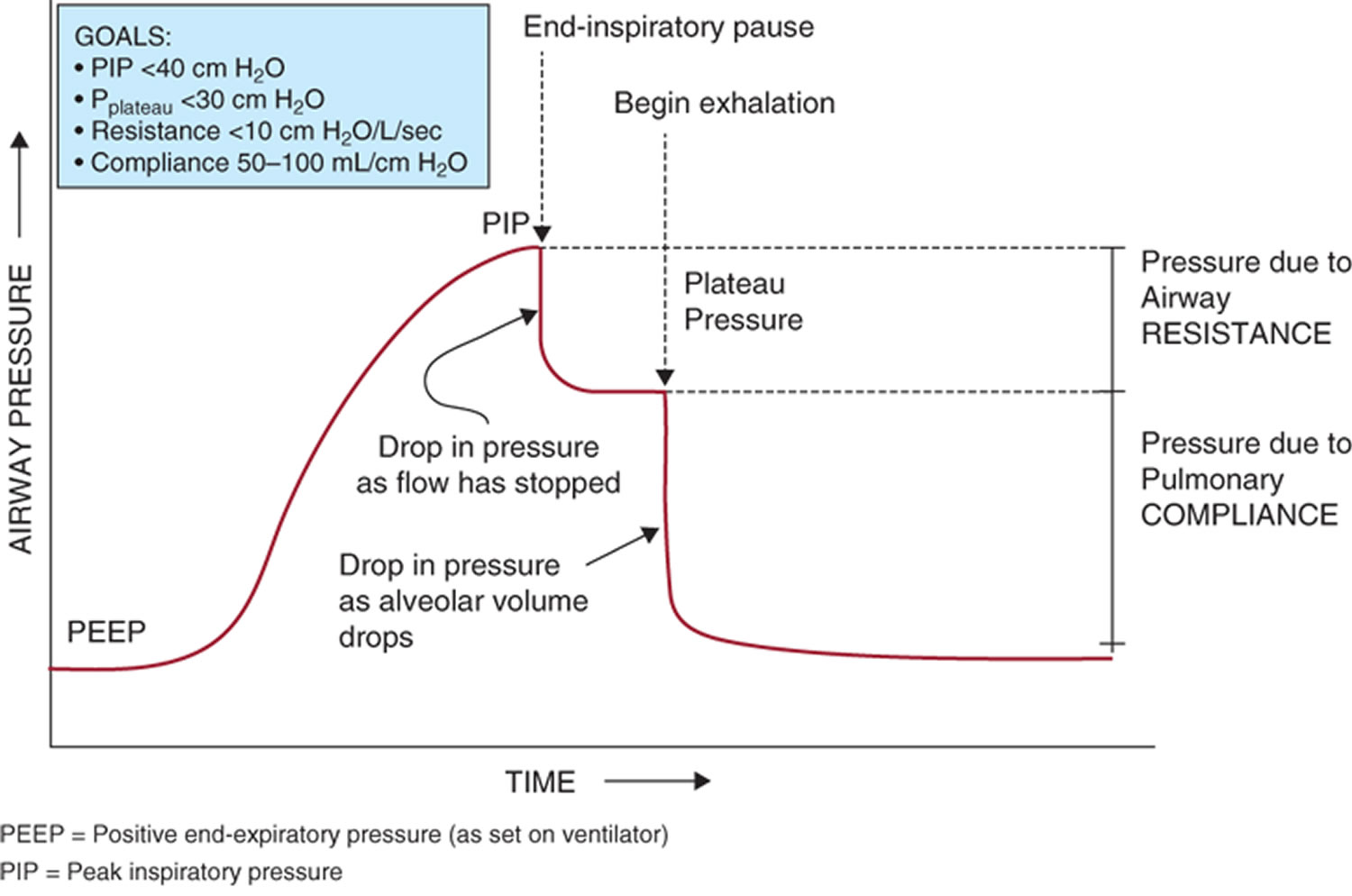
Peak inspiratory pressure (PIP) is the highest level of pressure applied to the lungs during inhalation 1. The peak inspiratory pressure (PIP) is the sum of the plateau pressure (Pplat) (pressure used to keep air in the lungs) and pressure used to overcome airway resistance (P resistance) to get the air into the lungs (elastic recoil of the lungs and chest wall, friction, etc.). In other words: Peak inspiratory pressure (PIP) = Pplat + P resistance. Consequently, Pplat can never be more than peak inspiratory pressure (PIP), because there’s always going to be intrinsic resistance which must be overcome by P resistance. In mechanical ventilation the number reflects a positive pressure in centimeters of water pressure (cm H2O). Normal peak inspiratory pressure (PIP) is 25-30 cm H2O. Peak inspiratory pressure (PIP) should be kept below 20 to 25 cm H2O whenever positive-pressure ventilation is required, especially if pneumothoraces, or fresh bronchial or pulmonary suture lines, are present. The risk for barotrauma increases whenever the peak pressures and plateau pressures become elevated to the same degree 2. Peak inspiratory pressure (PIP) increases with any airway resistance. Things that may increase Peak inspiratory pressure (PIP) could be increased secretions, bronchospasm, biting down on ventilation tubing, and decreased lung compliance.
Plateau pressure (Pplat) (pressure used to keep air in the lungs) is determined by an inspiratory hold maneuver in which the patient is given a fixed volume of air. Peak inspiratory pressure (PIP) is determined at the end of that inspiration. The drop-off that occurs between peak inspiratory pressure (PIP) and plateau pressure (Pplat) is airway resistance which was overcome during the inspiratory phase by pressure used to overcome airway resistance (P resistance). The pressure that remains during the hold maneuver is the plateau pressure (Pplat) and is a product of the lung tissue itself. Decreased pulmonary compliance, pulmonary edema, and interstitial lung disease can all affect this.
Now how does this translate to a real world example? Let’s say you walk into the room and see a peak inspiratory pressure (PIP) of 60 cm H2O (normal is 25-30 cm H2O). Let’s say you do an inspiratory hold maneuver, and plateau pressure (Pplat) is only 20 cm H2O. That means there’s a huge pressure overcoming airway resistance (ie, a very high P resistance). Now you’ll be thinking more about things which are decreasing the radius of the airway pipe. For example, the patient was biting his endotracheal tube and there’s a huge kink in the tubing coming off the ventilator.
What if the peak inspiratory pressure (PIP) was 50 cm H2O and the plateau pressure (Pplat) was 45 cm H2O? The high plateau pressure (Pplat) points towards a lung issue affecting the alveoli or small airways. Did the patient develop a pneumothorax? Is his pneumonia evolving?
Also, it’s important to consider that once the underlying pulmonary issue begins to resolve, pressures will change. Compliance will change. Pressure/volume curves will change. Peak and plateau pressures are a crude way to assess clinical improvement (all other factors being equal).
Figure 1. Peak inspiratory pressure
Footnote: Airway pressure and flow waveforms during constant flow volume control ventilation, illustrating the effect of an end-inspiratory breath-hold (end-inspiratory pause). With a period of no flow, the pressure equilibrates to the plateau pressure (Pplat). Plateau pressure (Pplat) represents the peak alveolar pressure. The difference between pressure at zero flow (Pz) and plateau pressure (Pplat) is due to time constant inhomogeneity within the lungs. The difference between the peak inspiratory pressure (PIP) and plateau pressure (Pplat) is determined by resistance and flow. The difference between plateau pressure (Pplat) and positive end-expiratory pressure (PEEP) is determined by tidal volume and respiratory system compliance. Pz = pressure at zero flow.
[Source 3 ]Some animal studies have looked at the association between alveolar overdistention and lung injury. Tsuno et al. 4 looked at histopathologic changes in the lungs of baby pigs. The settings on the ventilator produced a peak inspiratory pressure (PIP) of 40 cm H2O for up to 32 hours as well as the tidal volume of 15 mL/kg. Pathological findings on the subject’s studies included interstitial lymphocyte proliferation, alveolar hemorrhage, and hyaline membrane formation; all of which are similar to the histopathology observed in patients with acute respiratory distress syndrome (ARDS) 4. Other studies in human subjects have also demonstrated an association between high volume ventilation and increased levels of TNF-alpha and MIP-2; both are inflammatory cytokines researchers believe are implicated in the multi-organ dysfunction associated with ARDS 5.
Pulmonary barotrauma results from positive pressure mechanical ventilation. Positive pressure ventilation may lead to elevation of the trans-alveolar pressure or the difference in pressure between the alveolar pressure and the pressure in the interstitial space. Elevation in the trans-alveolar pressure may lead to alveolar rupture, which results in leakage of air into the extra-alveolar tissue.
Every patient on positive pressure ventilation is at risk of developing pulmonary barotrauma. However, certain ventilator settings, as well as specific disease processes, may increase the risk of barotrauma significantly. When managing a ventilator, physicians and other health care professionals must be aware of these risks to avoid barotrauma.
Specific disease processes, including chronic obstructive pulmonary disease (COPD), asthma, interstitial lung disease, pneumocystis jiroveci pneumonia, and acute respiratory distress syndrome (ARDS), may predispose individuals to pulmonary barotrauma. These diseases are associated with either dynamic hyperinflation or poor lung compliance, both of which predispose patients to increased alveolar pressure and ultimately barotrauma 6.
Patients with obstructive lung disease, COPD, and asthma are at risk of dynamic hyperinflation. These patients have a prolonged expiratory phase, and therefore have difficulty exhaling the full volume before the ventilator delivers the next breath. As a result, there is an increase in the intrinsic positive end-expiratory pressure (PEEP), also known as auto-PEEP. The hyperinflation is progressive and worsens with each tidal volume delivered. It leads to overdistention of the alveoli and increases the risk for barotrauma. Dynamic hyperinflation can be managed by decreasing the respiratory rate, decreasing the tidal volume, prolonging the expiratory time, and in some cases by increasing the external PEEP on the ventilator 7. The static auto-peep is easily measurable on a ventilator by performing an expiratory pause; by using this method you would obtain the total PEEP, the external PEEP subtracted from the total PEEP will equal the intrinsic PEEP or auto-PEEP. In many cases, auto-PEEP results in ventilator asynchrony, which may result in an increased risk of barotrauma. For a patient to be able to trigger a breath on the ventilator and for the flow to begin, the inspiratory muscles must overcome the recoil pressure. When intrinsic PEEP is present, it imposes an additional force that the inspiratory muscles have to overcome to trigger a breath. In many instances, auto-PEEP may lead to ventilator asynchrony, increased alveoli distention, and ultimately barotrauma 8.
Elevated plateau pressure (Pplat) is perhaps one of the most critical measurements of which to be aware. Plateau pressure (Pplat) is the pressure applied to the alveoli and other small airways during ventilation. Elevated plateau pressures, particularly pressures higher than 35 cm H2O, have been associated with an elevated risk for barotrauma 9. Plateau pressures are easily measurable on a ventilator by performing an inspiratory hold. Based on current data, as well as the increased mortality associated with barotrauma, the ARDSnet protocol suggests keeping plateau pressures below 30 cmH2O in patients on mechanical ventilation for ARDS management 10.
Elevated positive end-expiratory pressure (PEEP) may theoretically lead to overdistention of healthy alveoli in regions not affected by disease and ultimately barotrauma. However, clinical data has not associated increased PEEP with increased risk of barotrauma when used in conjunction with lung protective strategies, such as low tidal volume and target plateau pressure under 30 cm H2O. If higher PEEP is necessary for oxygenation, it should be titrated up slowly with close monitoring of the peak inspiratory and plateau pressures 11.
There is no single strategy to prevent pulmonary barotrauma on patients on mechanical ventilation 12. The most efficient mechanism that has been described to prevent the risk of developing barotrauma on mechanical ventilation involves maintaining the plateau pressure (Pplat) and peak inspiratory pressure (PIP) low 12. The goal plateau pressure (Pplat) should be below 35 cm H2O, and ideally below 30 cm H2O, on most patients on mechanical ventilation as recommended by the ARDS Network group. Various techniques may be employed to aid in maintaining the plateau pressure (Pplat) at goal. Various ventilator modes are available. The two modes most commonly used in intensive care units are volume assist control (volume AC), a volume cycled mode, and pressure assist control (pressure AC), a pressure cycled mode 12. Lung protective ventilator strategies should be used in every ARDS and most other patients, regardless of the mode of mechanical ventilation. Lung protective ventilator strategies derive for the most part from a study published in the year 2000 by the ARDS Network group. The study involved ARDS patients and compared outcomes in ARDS patients using higher tidal volume ventilation (about 12 mL/kg of ideal body weight) and patients using lower tidal volume ventilation (about 6 mL/kg of ideal body weight). Although tidal volume was the variable in this study, the goal with the low volume ventilation group was to keep the plateau pressure below 30 cm H2O. The low tidal volume ventilatory strategy correlated with a lower mortality rate (31% vs. 40%) 13. The incidence of barotrauma in this study was not lower when using lung-protective ventilator strategies; however, other studies have demonstrated a higher incidence of barotrauma when the plateau pressure rises above 35 cm H2O 14. Low tidal volume ventilation is especially important in patients at higher risk for barotrauma, such as patients with ARDS, COPD, asthma, Pneumocystis jiroveci pneumonia and chronic interstitial lung disease 6.
The driving pressure is another concept with which physicians managing patients at risk of barotrauma must be familiar. The driving pressure is measurable in patients not making an inspiratory effort; one can obtain the calculated pressure by subtracting the positive end-expiratory pressure (PEEP) from the plateau pressure (Pplat). Driving pressure became a hot topic of discussion after the ARDS trial proposed that high plateau pressures increase mortality in patients with ARDS but that high PEEP pressure is associated with improved outcomes. Amato et al. 15, in 2015, proposed that the driving pressure was a better ventilation variable to stratify risk 15. In the trial, published in the NEJM in 2015, they concluded that an increment of 1 standard deviation in driving pressure was associated with increased mortality even in patients receiving protective plateau pressure and tidal volumes. Individual changes in tidal volume and PEEP were only associated with improved survival if these changes led to a reduction in driving pressure.[17] Based on the data available, clinicians should maintain the optimal driving pressure between 13 and 15 cm H2O 15.
Patients with obstructive lung disease are at risk of dynamic hyperinflation due to a prolonged expiratory phase, and difficulty exhaling the full volume before the ventilator delivers the next breath. Physicians must be aware of intrinsic PEEP or auto-PEEP, particularly in patients at high risk, such as those with obstructive lung disease. An expiratory pause maneuver on the ventilator will provide the static intrinsic pressure. If intrinsic PEEP is present, then the physician may increase the external PEEP to help with ventilator synchronization by allowing the patient to trigger the ventilator and initiate a breath more effectively. The goal is to increase the external PEEP by 75 to 85% of the intrinsic PEEP 8. Other methods that the physician may employ to decrease the intrinsic PEEP include decreasing the respiratory rate, decreasing the tidal volume, and prolonging the expiratory time 7.
High positive end-expiratory pressure (PEEP) may theoretically lead to overdistention of healthy alveoli in regions not affected by disease and ultimately lead to barotrauma. Many conditions, such as moderate to severe ARDS, require the use of high PEEP pressures to improved oxygenation by recruiting as many alveoli units as possible. When used in conjunction with lung protective strategies, as described above, the risk of barotrauma due to high PEEP is minimal 11. Several methods exist to aid physicians in determining the adequate level of PEEP to treat individual patients based on lung compliance. A system pressure-volume curve may be used to determine the lower inflection point and the higher inflection point. The lower inflection point in the curve determines the minimal level of PEEP required to start alveolar recruitment. The upper inflection point in the curve determines the pressure level at which the risk of barotrauma and lung injury occurs 16.
The stress index is another method that may be used by physicians to determine the adequate amount of PEEP for individual patients. For the stress index to be an accurate measurement, the patient must be well sedated, and the flow must be constant. The physician may look at the pressure waveform on the ventilator to determine the stress index. A pressure wave that is concave down indicates a stress index less than 1. A stress index of less than 1 indicates that the patient may benefit from increased PEEP to help with alveoli recruitment. A pressure wave that is concave up indicates a stress index higher than 1. A stress index higher than one should alert the physician that the patient’s alveoli unit is at risk of distention and barotrauma. A straight diagonal line in the pressure wave is ideal because it correlates with a stress index between 0.9 and 1.1, which is the ideal range for proper alveoli recruitment with a low risk of distention and rupture 17.
Different ventilator modes also exist, which may be better tolerated by some patients and decrease the risk of barotrauma. There is no evidence to suggest that one ventilator mode is better than the other. However, in patients who are difficult to manage, physicians may try different modes to synchronize the patient with the ventilator better.
Volume AC mode is a volume cycled mode. It will deliver a set volume on every ventilator assisted breath, which will lead to significant variations in peak inspiratory pressures as well as plateau pressures depending on the compliance of the lung parenchyma. The peak inspiratory and plateau pressures may be kept at goal using this mode of ventilation by using low tidal volume ventilation (between 6 to 8 mL/kg based on the ideal body weight). The respiratory rate and inspiratory time may be adjusted as well to prevent intrinsic PEEP. In some cases, sedation, and even neuromuscular blocking agents may be to be used to improve ventilator synchrony and maintain inspiratory peak and plateau pressures at goal 18.
Pressure AC mode is a pressure cycled mode. It allows medical personnel to set an inspiratory pressure level as well as the applied PEEP. The advantage of using a pressure cycled mode is that the peak inspiratory pressure will remain constant and will be equal to the inspiratory pressure in addition to the PEEP. The plateau pressure will also be lower or equal to the peak inspiratory pressure; therefore, this mode of ventilation correlates with a lower rate of barotrauma. The disadvantage, however, is that the tidal volume delivered will vary depending on lung compliance. Patients with poor lung compliance may not receive an adequate tidal volume using this ventilator mode 18.
- Clinical application of ventilator modes: Ventilatory strategies for lung protection. Aust Crit Care. 2010 May;23(2):71-80. doi: 10.1016/j.aucc.2010.03.003. Epub 2010 Apr 7. https://doi.org/10.1016/j.aucc.2010.03.003[↩]
- Tuxen DV, Lane S. The effects of ventilatory pattern on hyperinflation, airway pressures, and circulation in mechanical ventilation of patients with severe air-flow obstruction. Am. Rev. Respir. Dis. 1987 Oct;136(4):872-9.[↩]
- Respiratory Mechanics in Mechanically Ventilated Patients. Respiratory Care November 2014, 59 (11) 1773-1794; DOI: https://doi.org/10.4187/respcare.03410 [↩]
- Tsuno K, Prato P, Kolobow T. Acute lung injury from mechanical ventilation at moderately high airway pressures. J. Appl. Physiol. 1990 Sep;69(3):956-61.[↩][↩]
- Chiumello D, Pristine G, Slutsky AS. Mechanical ventilation affects local and systemic cytokines in an animal model of acute respiratory distress syndrome. Am. J. Respir. Crit. Care Med. 1999 Jul;160(1):109-16.[↩]
- Anzueto A, Frutos-Vivar F, Esteban A, Alía I, Brochard L, Stewart T, Benito S, Tobin MJ, Elizalde J, Palizas F, David CM, Pimentel J, González M, Soto L, D’Empaire G, Pelosi P. Incidence, risk factors and outcome of barotrauma in mechanically ventilated patients. Intensive Care Med. 2004 Apr;30(4):612-9.[↩][↩]
- Thorevska NY, Manthous CA. Determinants of dynamic hyperinflation in a bench model. Respir Care. 2004 Nov;49(11):1326-34.[↩][↩]
- Mughal MM, Culver DA, Minai OA, Arroliga AC. Auto-positive end-expiratory pressure: mechanisms and treatment. Cleve Clin J Med. 2005 Sep;72(9):801-9.[↩][↩]
- Esteban A, Anzueto A, Frutos F, Alía I, Brochard L, Stewart TE, Benito S, Epstein SK, Apezteguía C, Nightingale P, Arroliga AC, Tobin MJ., Mechanical Ventilation International Study Group. Characteristics and outcomes in adult patients receiving mechanical ventilation: a 28-day international study. JAMA. 2002 Jan 16;287(3):345-55.[↩]
- International consensus conferences in intensive care medicine: Ventilator-associated Lung Injury in ARDS. This official conference report was cosponsored by the American Thoracic Society, The European Society of Intensive Care Medicine, and The Societé de Réanimation de Langue Française, and was approved by the ATS Board of Directors, July 1999. Am. J. Respir. Crit. Care Med. 1999 Dec;160(6):2118-24.[↩]
- Brower RG, Lanken PN, MacIntyre N, Matthay MA, Morris A, Ancukiewicz M, Schoenfeld D, Thompson BT., National Heart, Lung, and Blood Institute ARDS Clinical Trials Network. Higher versus lower positive end-expiratory pressures in patients with the acute respiratory distress syndrome. N. Engl. J. Med. 2004 Jul 22;351(4):327-36.[↩][↩]
- Diaz R, Heller D. Barotrauma And Mechanical Ventilation. [Updated 2019 Oct 1]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK545226[↩][↩][↩]
- Acute Respiratory Distress Syndrome Network. Brower RG, Matthay MA, Morris A, Schoenfeld D, Thompson BT, Wheeler A. Ventilation with lower tidal volumes as compared with traditional tidal volumes for acute lung injury and the acute respiratory distress syndrome. N. Engl. J. Med. 2000 May 04;342(18):1301-8.[↩]
- Boussarsar M, Thierry G, Jaber S, Roudot-Thoraval F, Lemaire F, Brochard L. Relationship between ventilatory settings and barotrauma in the acute respiratory distress syndrome. Intensive Care Med. 2002 Apr;28(4):406-13.[↩]
- Amato MB, Meade MO, Slutsky AS, Brochard L, Costa EL, Schoenfeld DA, Stewart TE, Briel M, Talmor D, Mercat A, Richard JC, Carvalho CR, Brower RG. Driving pressure and survival in the acute respiratory distress syndrome. N. Engl. J. Med. 2015 Feb 19;372(8):747-55.[↩][↩][↩]
- Lu Q, Rouby JJ. Measurement of pressure-volume curves in patients on mechanical ventilation: methods and significance. Crit Care. 2000;4(2):91-100.[↩]
- Sun XM, Chen GQ, Chen K, Wang YM, He X, Huang HW, Luo XY, Wang CM, Shi ZH, Xu M, Chen L, Fan E, Zhou JX. Stress Index Can Be Accurately and Reliably Assessed by Visually Inspecting Ventilator Waveforms. Respir Care. 2018 Sep;63(9):1094-1101.[↩]
- Ioannidis G, Lazaridis G, Baka S, Mpoukovinas I, Karavasilis V, Lampaki S, Kioumis I, Pitsiou G, Papaiwannou A, Karavergou A, Katsikogiannis N, Sarika E, Tsakiridis K, Korantzis I, Zarogoulidis K, Zarogoulidis P. Barotrauma and pneumothorax. J Thorac Dis. 2015 Feb;7(Suppl 1):S38-43.[↩][↩]