Pelvic fracture
Pelvic fracture is a break in one or more bones of the pelvis. Pelvic fracture is uncommon accounting for only about 3% of all adult fractures. Most pelvic fractures are caused by some type of traumatic, high-energy event, such as a car collision. In some cases, a lower-impact event—such as a minor fall—may be enough to cause a pelvic fracture in an older person who has weaker bones.
Pelvic fractures range widely in severity. A mild fracture (for example, one that occurs only at the part of the pelvis called the pubic rami) may heal in several weeks without surgery. However, a serious pelvic fracture, such as ones sustained in car and motorbike accidents, can be a life-threatening event as it often also involves damage to nearby internal organs requiring emergency medical care, surgery and long period of recovery. Because the pelvis is in proximity to major blood vessels and organs, pelvic fractures may cause extensive bleeding and other injuries that require urgent treatment.
Treatment for a pelvic fracture varies depending on the severity of the injury. While lower-energy fractures can often be managed with conservative care, treatment for high-energy pelvic fractures usually involves surgery to reconstruct the pelvis and restore stability so that patients can resume their daily activities.
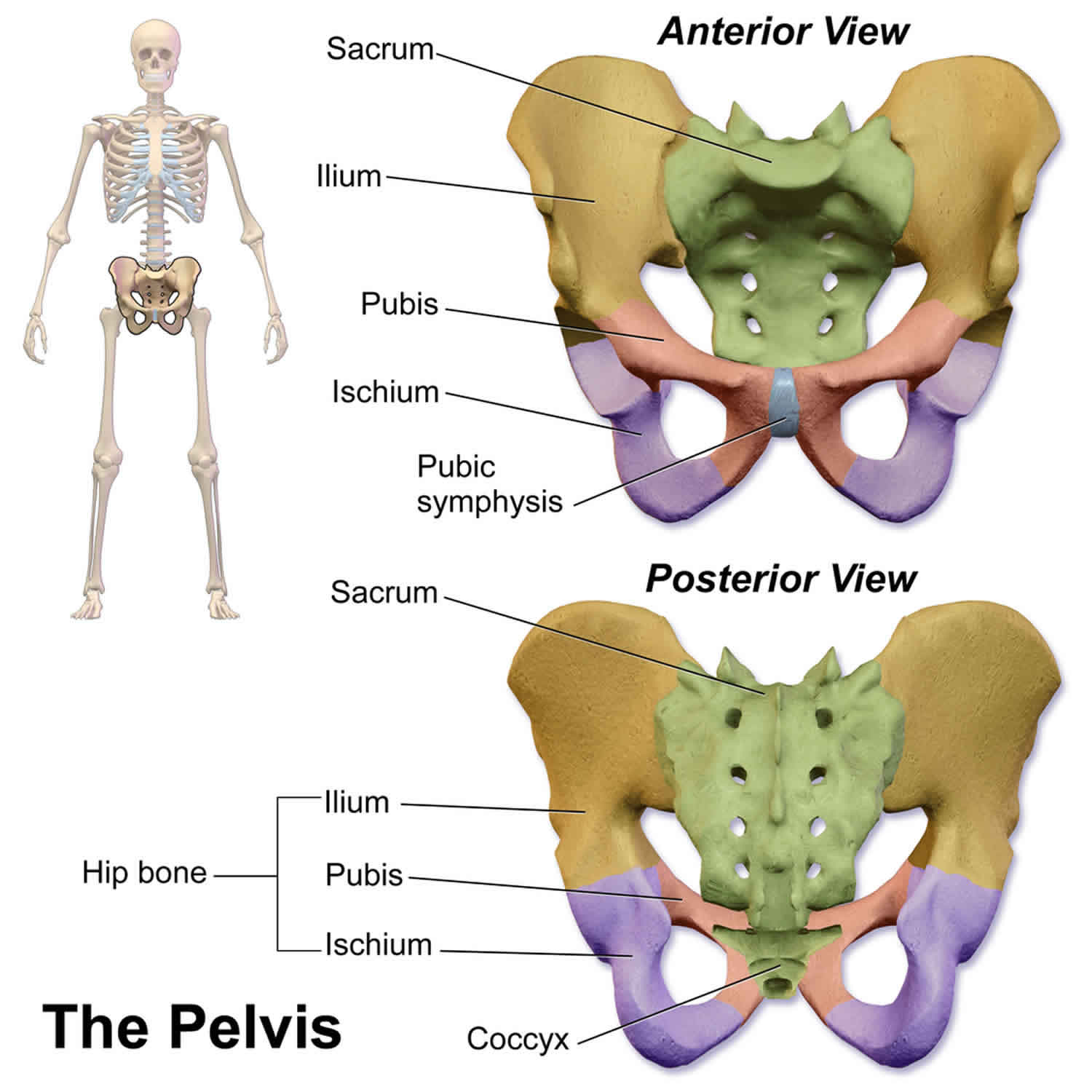
Pelvis anatomy
The pelvis is a butterfly-shaped ring of bones located at the base of the spine—between the spine and the legs. The pelvis is made up of three bones:
- Sacrum (the large triangular bone at the base of the spine). The sacrum is a central triangular shaped bone which forms the base of the spine and at its tip joins on to the coccyx
- Coccyx (tailbone).
- Hip bones. Hip bones are the large bones either side of the sacrum. The hip socket (or acetabulum) is a part of the hip bones. The thigh bone or femur fits into the socket forming the hip joint.
Each hip bone contains three bones—the ilium, ischium, and pubis—that are separate during childhood but fuse together as you grow older. These three bones meet to form the acetabulum—the hollow cup that serves as the socket for the ball-and-socket hip joint.
Bands of strong connective tissues called ligaments join the pelvis to the sacrum, creating a bowl-like cavity below the rib cage.
Major nerves, blood vessels, and portions of the bowel, bladder, and reproductive organs all pass through the pelvic ring. The pelvis protects these important structures from injury. It also serves as an anchor for the muscles of the hip, thigh, and abdomen.
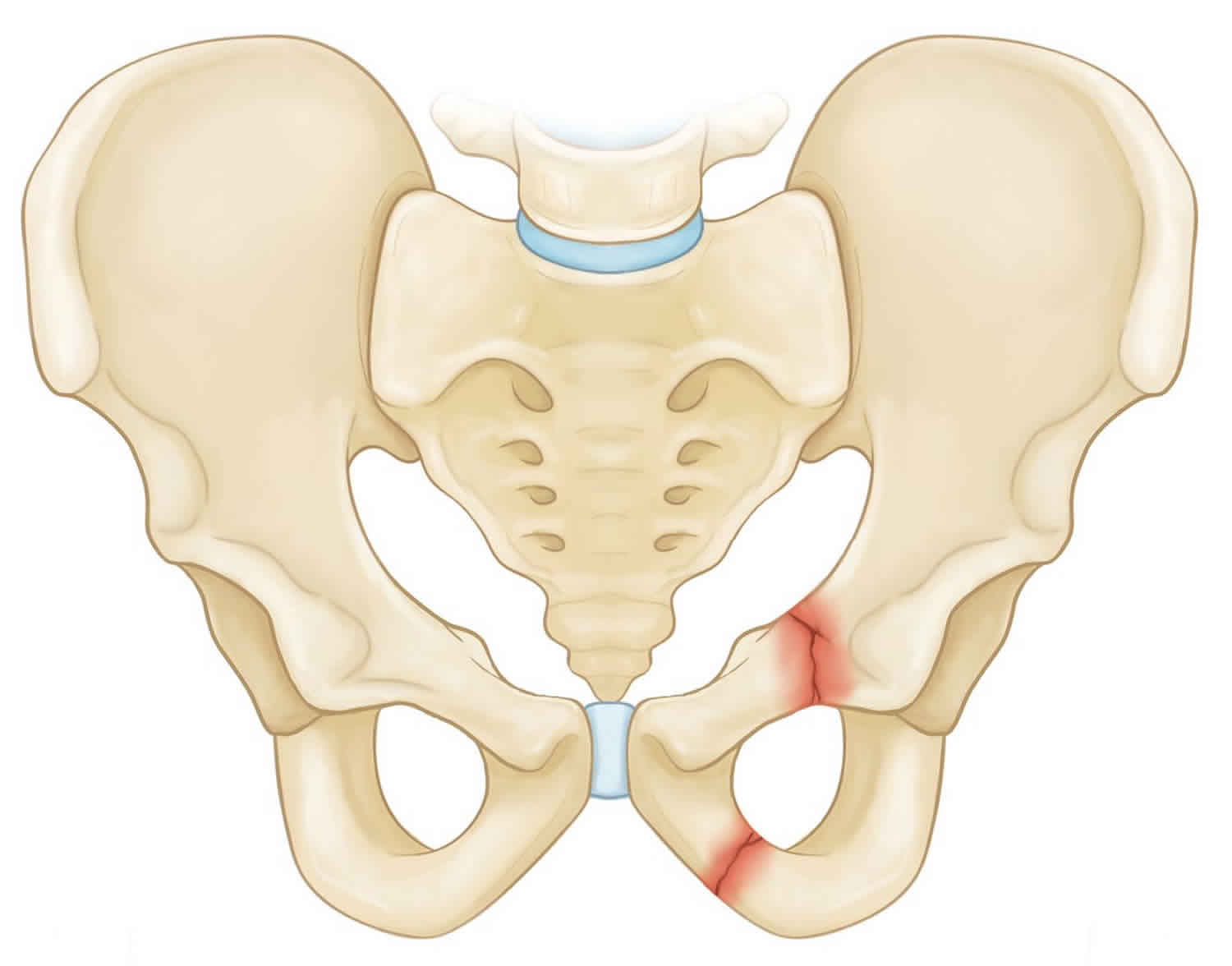
Figure 2. Pelvic fracture
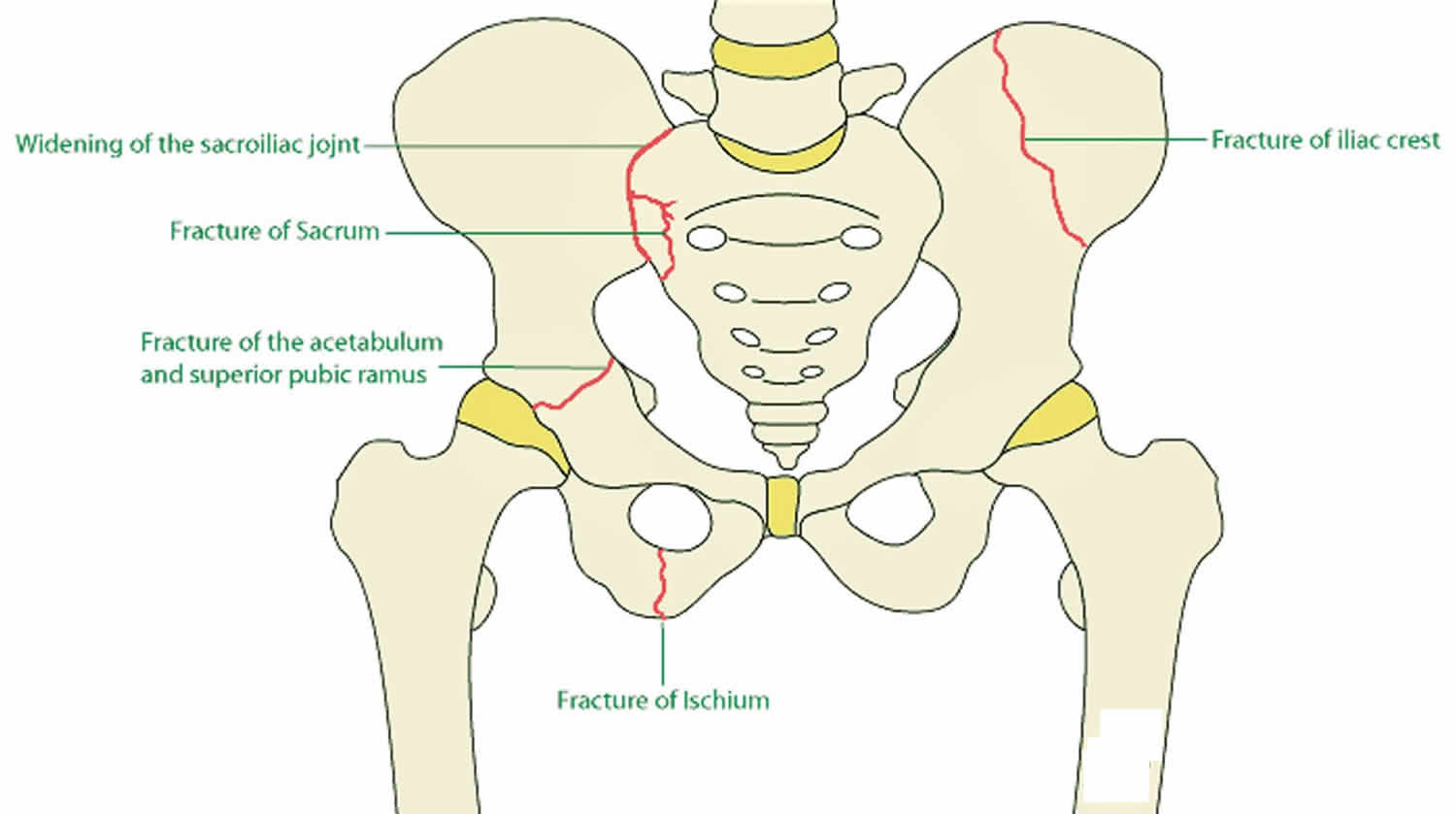
Pelvic fracture types
The pelvis is a ring-like structure, a fracture in one part of the structure is often accompanied by a fracture or damage to ligaments at another point in the structure. Doctors have identified several common pelvic fracture patterns. The specific pattern of the fracture depends upon the direction in which it was broken and the amount of force that caused the injury.
In addition to being described by the specific fracture pattern, pelvic fractures are often described as “stable” or “unstable,” based on how much damage has occurred to the structural integrity of the pelvic ring. Both stable and unstable pelvic fractures can also be divided into “open” fractures, in which the bone fragments stick out through the skin, or “closed” fractures, in which the skin is not broken. Open fractures are particularly serious because, once the skin is broken, infection in both the wound and the bone can occur. Immediate treatment is required to prevent infection.
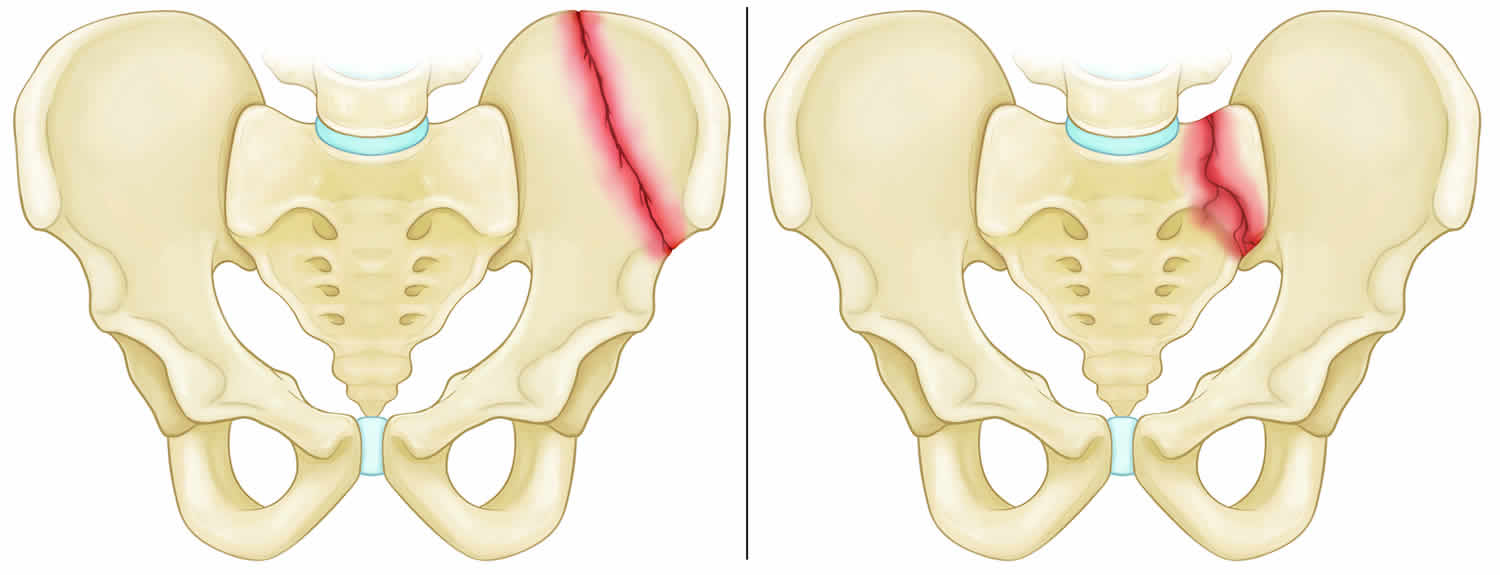
Stable pelvic fracture
In stable pelvic fracture type, there is often only one break in the pelvic ring and the broken ends of the bones line up adequately. Low-energy fractures are often stable fractures. Stable pelvic fracture patterns include:
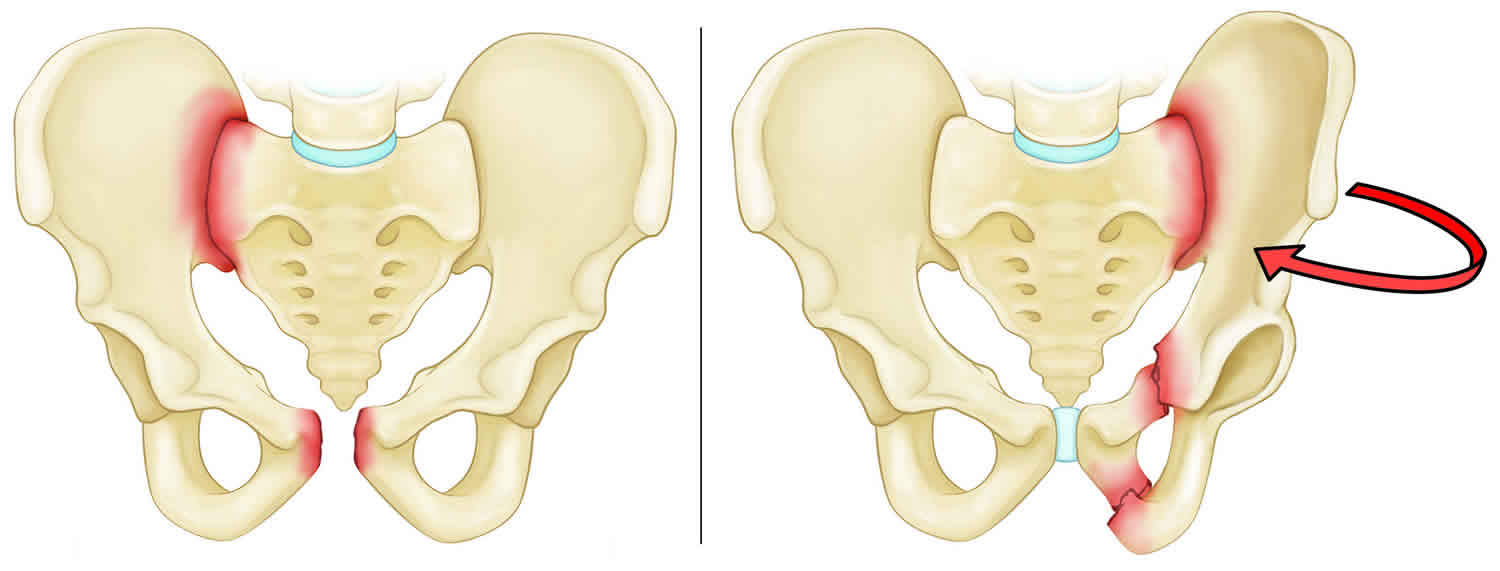
Figure 3. Stable pelvic fractures
Footnote: Types of stable pelvic fractures: (Left) Iliac wing fracture. (Right) Sacrum fracture.
Figure 4. Stable pelvic fracture (superior and inferior pubic ramus fracture)
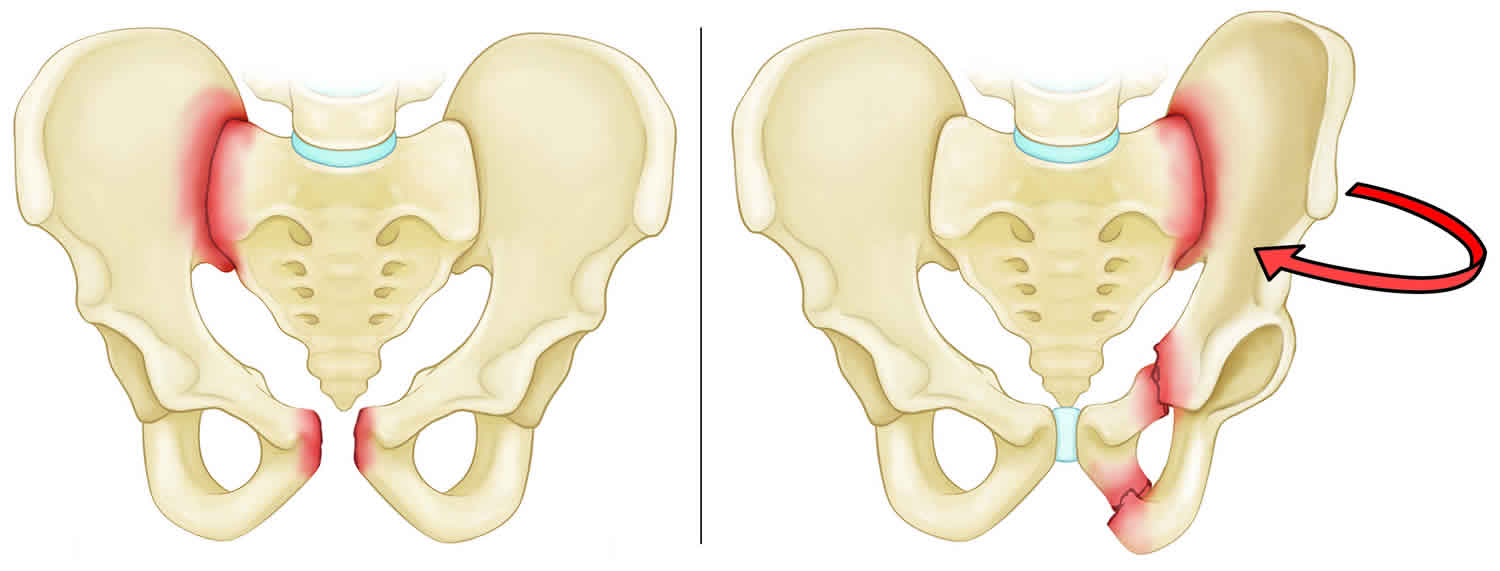
Unstable pelvic fractures
In unstable pelvic fracture type, there are usually two or more breaks in the pelvic ring and the ends of the broken bones do not line up correctly (displacement). This type of fracture is more likely to occur due to a high-energy event. Unstable pelvic fracture patterns include:
Figure 5. Unstable pelvic fractures
Footnote: Types of unstable pelvic fractures: (Left) Anterior-posterior compression fracture. (Right) Lateral compression fracture. In this fracture, the pelvis is pushed inward.
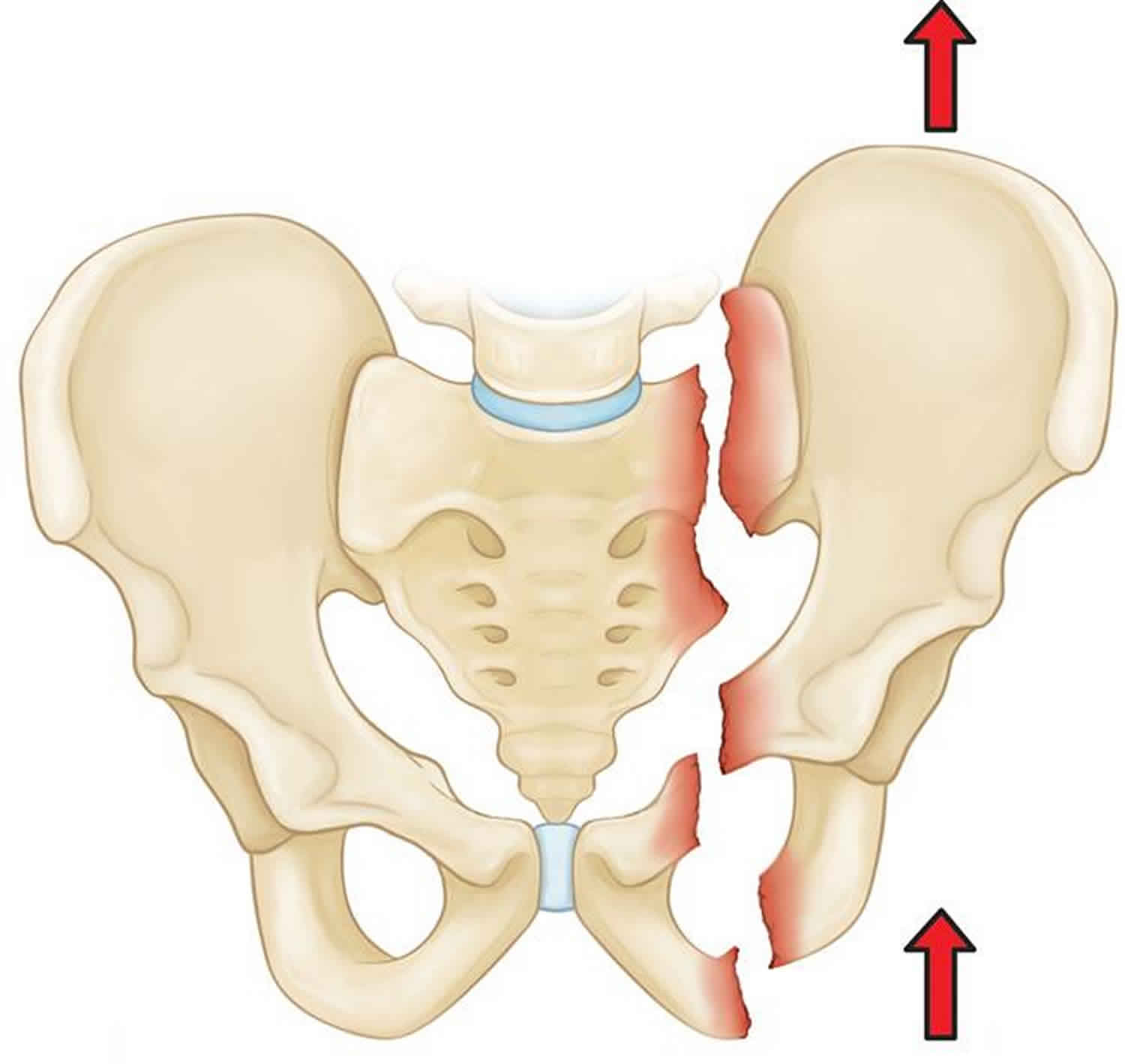
Figure 6. Unstable pelvic fracture
Footnote: Vertical shear fracture. In this fracture, one half of the pelvis shifts upward.
Pelvic fracture causes
Pelvic fractures are often classified into two groups depending on their cause:
- Pelvic fractures due to high-energy trauma
- Pelvic fractures due to low-energy trauma
Pelvic fractures due to high-energy trauma
High energy trauma means any accident that involves a large amount of force. The most common type of these injuries includes:
- Car or motorcycle collision
- Crush accident
- Fall from a significant height (such as a ladder)
Depending on the direction and magnitude of the force, these injuries can be life-threatening and require surgical treatment.
There are a variety of different pelvic fractures that can occur depending on the direction of the force and the amount of force. The doctor assessing you will want to know as much information about the accident as possible as this will help to narrow down the possible type of pelvic fracture.
Pelvic fractures due to low energy trauma
In these fractures, the force that causes the fracture is not very high and is something that may occur in every day life. There are two main types of pelvic fractures that occur at low energy
- Avulsion fractures: this is where a small piece of bone is pulled off at the site where a muscle attaches. This is most common in young athletes who are still growing and often occurs during sporting activities. This is a relatively minor form of pelvic fracture. An avulsion fracture does not usually make the pelvis unstable or injure internal organs.
- Pathological fracture: This means that the fracture occurred due to some kind of disease process (or pathology) affecting the bone. Most commonly this is due to osteoporosis which weakens the bones and makes them more vulnerable to fracture. This type of fracture is seen most commonly in the elderly whose bones have become weakened by osteoporosis. In these patients, a fracture may occur even during a fall from standing or a routine activity such as getting out of the bathtub or descending stairs. These injuries are typically stable fractures that do not damage the structural integrity of the pelvic ring, but may fracture an individual bone.
Risk factors for pelvic fracture
For high energy pelvic fractures or those involving a large force the risk factors include:
- car accidents/ motor cycle accidents
- falls from a height
- crush fractures
- high speed sporting accidents such as alpine skiing, down hill mountain-biking, motor cross etc.
For low energy pelvic fractures or those involving minimal force, the risk factors include:
- osteoporosis
- destructive bone lesion such as cancer
- age: the elderly are more susceptible to low energy pelvic fractures.
Pelvic fracture prevention
In a person susceptible to low energy trauma fractures, which means an accident that does not require a lot of force, the following measures may be taken to prevent fractures:
- Prevent falls by using a stool or stepladder to reach high places. Add handrails along stairways and place nonslip mats in your bathroom, shower, and under carpets.
- Maintain your muscle strength which will help to prevent falls.
- Maintain bone density through weight bearing exercise and appropriate medical treatment as guided by your doctor.
For high energy trauma fractures, the following measures may be taken:
- Lower your chance of injuries due to car and motorcycle accidents by always wearing your seatbelt.
- Always use safety precautions to avoid falls during high-risk sports, such as rock climbing and mountaineering.
Pelvic fracture symptoms
A fractured pelvis is almost always painful. This pain is aggravated by moving the hip or attempting to walk. Often, the patient will try to keep his or her hip or knee bent in a specific position to avoid aggravating the pain. Some patients may experience swelling or bruising in the hip area.
The symptoms of a fractured pelvis include:
- Pain: pelvic fractures can be very painful. Depending on where the fracture is, the pain may be felt in different areas. Common areas of pain include groin, buttock and lower back.
- Deformity: Due to the break in the pelvis, one leg may appear shorter than the other or one side of the pelvis may appear larger than the other.
- Swelling and bruising: there will often be a lot of swelling and bruising around the site of the injury. Sometimes bruising or bleeding can occur within the pelvis and not be obvious from the outside.
- Wounds: If the pelvic fracture is severe or was caused by a high impact injury, the broken bone may break through the skin.
- Organ damage: the pelvis is a ring of bone that protects internal organs, especially the bladder, uterus and intestine. A fractured pelvis can cause damage to these organs. This can lead to blood in the urine or stools.
- Nerve damage: nerves that run from the spinal cord to supply the legs can be damaged by pelvic fractures. This may be felt as pain or numbness in the legs. It may also cause weakness in the muscles of the legs.
- Pain in other areas of the body: Pelvic fractures are often caused by high impact injuries. These injuries will often affect multiple areas of the body and as such, pain in other areas of the body may indicate additional fractures, strains or bruising.
Pelvic fracture complications
The complications of pelvic fractures include:
- Bleeding: This may occur if a broken bone punctures the skin in which case it is easily observable. Bleeding can also occur internally due to a pelvic fracture and lead to large amounts of blood loss without being obvious.
- Organ damage: The bladder and lower bowel may be injured due to a pelvic fracture.
- Infection: An infection may occur at the site of a wound caused by a broken bone, however infections can also occur within the pelvis in the form of an abscess
- Nerve damage: Damage to nerves may occur as a result of broken bones impinging on nerves or as a complication of surgery which may be necessary to stabilise the pelvis. This can lead to numbness or weakness in the legs. It can also lead to sexual dysfunction due to nerve damage affecting the genitals.
- Blood clots (vein thrombosis): Blood clots can develop within the veins of the pelvis which can lead to the further complication of these clots travelling to the lungs.
- Delayed healing of fracture: This may occur if there is incomplete fixation of the broken bones following surgery.
Pelvic fracture diagnosis
Patients with high-energy fractures will almost always go or be brought to an urgent care center or emergency room for initial treatment due to the severity of their symptoms.
These patients may also have additional injuries to the head, chest, abdomen, or legs. If their injuries cause significant blood loss, it could lead to shock—a life-threatening condition that can result in organ failure.
The care of patients with high-energy pelvic fractures requires a multidisciplinary approach with input from a number of medical specialists. In some cases, doctors must address airway, breathing, and circulatory problems before treating the fracture and other injuries.
Clinical assessment
Your doctor will carefully examine your pelvis, hips, and legs. He or she will also check for nerve injury by assessing whether you can move your ankles and toes and feel sensation on the bottom of your feet.
Your doctor will also carefully examine the rest of your body to determine if you have sustained any other injuries.
- The first step of investigating any medical problem is a clinical assessment with both a thorough history and examination.
- The history is particularly important for pelvic fractures as the way the injury happened may guide the doctor to make a diagnosis of the type of pelvic fracture.
- The examination will include assessment of any wounds, bruising, deformity or altered leg position, nerves of the leg, as well as an examination of pelvic organs.
Imaging studies
- X-ray: All pelvic fractures require x-rays—usually from a number of different angles—to help the doctor determine how displaced place the bones are. This is the first step in diagnosis of pelvic fractures and will help to confirm or rule out the presence of a fracture
- CT scan: Will give a more accurate picture of the extent of pelvic fractures and is often used following an X-ray. Because of the complexity of this type of injury, a CT scan is commonly ordered for pelvic fractures. A CT scan will provide a more detailed, cross-sectional image of the pelvis. Your doctor will use this information to better determine the specific pattern and extent of your injury, look for associated injuries, and aid in preoperative planning.
- Magnetic resonance imaging (MRI) scans: In rare cases, your doctor may order an MRI scan to discover a fracture that cannot be seen on x-ray or CT scan.
Diagnosis of instability
The pelvis is a ring of bone which if broken can lead to instability. This means that there is abnormal movement of the pelvic bones during normal activities such as walking. This can be diagnosed by clinical examination if the pelvic fracture is severe but may require imaging to pick up the presence of certain criteria which may indicate pelvic instability.
Pelvic fracture treatment
Depending on the severity of the pelvic fracture, the treatment for pelvic fractures varies from simple rest or medical aids to surgical intervention.
Treatment is based on a number of factors, including:
- The specific pattern of the fracture
- How much the bones are displaced
- Your overall condition and associated injuries
Nonsurgical Treatment
Your doctor may recommend nonsurgical treatment for stable fractures in which the bones are nondisplaced or minimally displaced. This approach is appropriate for when the fracture is ‘stable’. This means that with normal activities, the two parts of the broken bone do not move and will heal without surgical intervention. It may be necessary to use crutches or a walking frame and avoid any high impact activities. It will usually take up to 3 months for a full recovery during which time care needs to be taken to avoid aggravating the injury. This approach is often taken with avulsion fractures (where a piece of bone is pulled off by a tendon where it attaches to the bone) or other minor fractures.
Nonsurgical treatments may include:
- Walking aids. To avoid bearing weight on your leg, your doctor may recommend that you use crutches or a walker for up to three months—or until your bones are fully healed. If you have injuries above both legs, you may need to use a wheelchair for a period of time so that you can avoid bearing weight on either leg.
- Medications. Your doctor may prescribe medication to relieve pain, as well as an anti-coagulant, or blood thinner, to reduce the risk of blood clots forming in the veins of your legs and pelvis.
Pelvic fracture surgery
Patients with unstable pelvic fractures may require one or more surgical procedures. An unstable fracture is present when the two parts of the broken bone will move when performing normal movement. In this case, the bones will not heal unless they are fixed in place by a surgical procedure. The type of surgical technique used depends on the location and the extent of the fracture. Sometimes, as well as fixing the broken bones in place, damage to organs may also need to be repaired.
External fixation
Your doctor may use external fixation to stabilize your pelvic area. In this operation, metal pins or screws are inserted into the bones through small incisions into the skin and muscle. The pins and screws project out of the skin on both sides of the pelvis where they are attached to carbon fiber bars outside the skin. The external fixator acts as a stabilizing frame to hold the broken bones in proper position.
In some cases, an external fixator is used to stabilize the bones until healing is complete. In patients who are unable to tolerate a lengthy, more complicated procedure, an external fixator may be used as a temporary treatment until another procedure can be performed.
Skeletal traction
Skeletal traction is a pulley system of weights and counterweights that helps realign the pieces of bone. Skeletal traction is often used immediately after an injury and removed after surgery. Occasionally, acetabular fractures can be treated with skeletal traction alone. This is rare, however, and will be a decision made jointly with input from your doctor.
During skeletal traction, metal pins are implanted in the thighbone or shinbone to help position the leg. Weights attached to the pins gently pull on the leg, keeping the broken bone fragments in as normal a position as possible. For many patients, skeletal traction also provides some pain relief.
Open reduction and internal fixation
During this operation, the displaced bone fragments are first repositioned (reduced) into their normal alignment. They are then held together with screws or metal plates attached to the outer surface of the bone.
Pelvic fracture surgery risks
There are risks associated with any surgical procedure. Before your surgery, your doctor will discuss each of these risks with you and will take specific measures to help avoid potential complications.
Possible complications include:
- Wound healing problems, including infection
- Damage to nerves or blood vessels
- Blood clots
- Pulmonary embolism—a blood clot in the lungs
Pelvic fracture healing time
After surgery, you will feel some pain. This is a natural part of the healing process. Your doctor and nurses will work to reduce your pain, which can help you recover from surgery faster.
Medications are often prescribed for short-term pain relief after surgery. Many types of medicines are available to help manage pain, including opioids, non-steroidal anti-inflammatory drugs (NSAIDs), and local anesthetics. Your doctor may use a combination of these medications to improve pain relief, as well as minimize the need for opioids.
Be aware that although opioids help relieve pain after surgery, they are a narcotic and can be addictive. Opioid dependency and overdose has become a critical public health issue in the U.S. It is important to use opioids only as directed by your doctor. As soon as your pain begins to improve, stop taking opioids. Talk to your doctor if your pain has not begun to improve within a few days of your surgery.
Early Movement
In most cases, your doctor will encourage early movement. Most patients begin walking—with weight-bearing restrictions—and performing foot and leg exercises as soon as possible after surgery.
Weight Bearing
Your doctor may recommend that you use crutches or a walker for a period of time. Full weight bearing is usually allowed by 3 months—or when your bones are fully healed. You may require the use of a cane or walking aid for a longer period of time.
Physical Therapy
Specific exercises will help you regain flexibility and restore range of motion in your hip. Other exercises will help you build strength and endurance so that you are better able to perform your daily activities.
Blood Clot Prevention
Although early movement is encouraged, your mobility after surgery will still be somewhat limited. For this reason, your doctor may prescribe an anticoagulant, or blood thinner, to help prevent blood clots from forming in the deep veins of your pelvis and legs.
Pelvic fracture long term complications
Stable pelvic fractures tend to heal well. Unstable pelvic fractures sustained during high-energy incidents, such as car accidents, may result in significant complications, including severe bleeding, internal organ damage, and infection. If these injuries are addressed successfully, the fracture usually heals well.
You may walk with a limp for several months if damage has occurred to the muscles around your pelvis. These muscles may take up to one year to become strong again.
Subsequent problems, such as pain, impaired mobility, and sexual dysfunction, may result from damage to nerves and organs that is associated with the pelvic fracture.
Pelvic fracture prognosis
Early stabilization of pelvic ring injuries has demonstrated improved outcomes in patients with pelvic fractures. Stabilization of pelvic fractures immobilizes bleeding cancellous surfaces, thereby decreasing overall blood loss 1. Goldstein et al 2 noted decreased operative time, blood transfusions, and hospital stays for patients who were treated within 24 hours of hospital admission. Similarly, Latenser et al 3 noted decreased complications, blood loss, hospital stays, long-term disability, and better survival for patients treated within 8 hours of hospital admission.
Injury pattern and reduction of fracture-related displacements have been correlated with outcome results. Injuries involving the SI joint are associated with poorer results when compared with patients with either sacral fractures or iliac wing fractures 4. Posterior pelvic displacement of 5 mm has been identified as leading to poorer patient outcomes 5. Another study noted that patients with pelvic displacements greater than 1 cm in any plane had increased levels of pain when compared with patients with displacements less than 1 cm. Limb length discrepancy greater than 2.5 cm also has been implicated in poor results 6.
Permanent neurologic injury contributes to poorer patient outcomes after pelvic ring injury, and is present in approximately 20% of patients with unstable pelvic ring injuries 4. Tile noted that permanent nerve damage led to unsatisfactory results in 12 of 248 patients 4. Templeman et al 7 also noted that neurologic injury was associated with compromised outcome in patients with sacral fractures. Most neurologic injuries after pelvic ring injuries involve the L5 and S1 nerve roots, though injury may occur along any portion of the lumbosacral trunk. Management of neurologic injuries is expectant, as neurologic recovery has been documented as long as 4 years after injury 8.
A study by Sharma et al 9 focused on risk assessment for mortality in 566 patients with pelvic fracture. High risk was defined (on the basis of blood pressure, examination, radiographs, and computed tomography [CT]) as open fractures, open-book injuries, abbreviated injury score of 4 or higher, and hypotension (systolic blood pressure ≤89 mm Hg). Mortality was 24% for high-risk pelvic fracture and 3% for low-risk pelvic fracture. The investigators concluded that assessment of mortality risk in patients with pelvic fracture can be aided by trauma mechanism, initial blood pressure measurement, radiography, and CT 9.
- Huittinen VM, Slätis P. Postmortem angiography and dissection of the hypogastric artery in pelvic fractures. Surgery. 1973 Mar. 73(3):454-62.[↩]
- Goldstein A, Phillips T, Sclafani SJ, et al. Early open reduction and internal fixation of the disrupted pelvic ring. J Trauma. 1986 Apr. 26(4):325-33[↩]
- Latenser BA, Gentilello LM, Tarver AA, et al. Improved outcome with early fixation of skeletally unstable pelvic fractures. J Trauma. 1991 Jan. 31(1):28-31[↩]
- Tile M, Kellam JF. Anatomy of the pelvic ring. Tile M, Helfet DL, Kellam JF, Vrahas M, eds. Fractures of the Pelvis and Acetabulum: Principles and Methods of Management. 4th ed. New York: Thieme/AO; 2015. Vol 1[↩][↩][↩]
- Pohlemann T, Bosch U, Gansslen A, Tscherne H. The Hannover experience in management of pelvic fractures. Clin Orthop. 1994 Aug. (305):69-80[↩]
- Tile M. Pelvic ring fractures: should they be fixed?. J Bone Joint Surg Br. 1988 Jan. 70(1):1-12.[↩]
- Templeman D, Goulet J, Duwelius PJ, et al. Internal fixation of displaced fractures of the sacrum. Clin Orthop. 1996 Aug. (329):180-5.[↩]
- Reilly MC, Zinar DM, Matta JM. Neurologic injuries in pelvic ring fractures. Clin Orthop. 1996 Aug. (329):28-36.[↩]
- Sharma OP, Oswanski MF, Rabbi J, Georgiadis GM, Lauer SK, Stombaugh HA. Pelvic fracture risk assessment on admission. Am Surg. 2008 Aug. 74(8):761-6.[↩][↩]