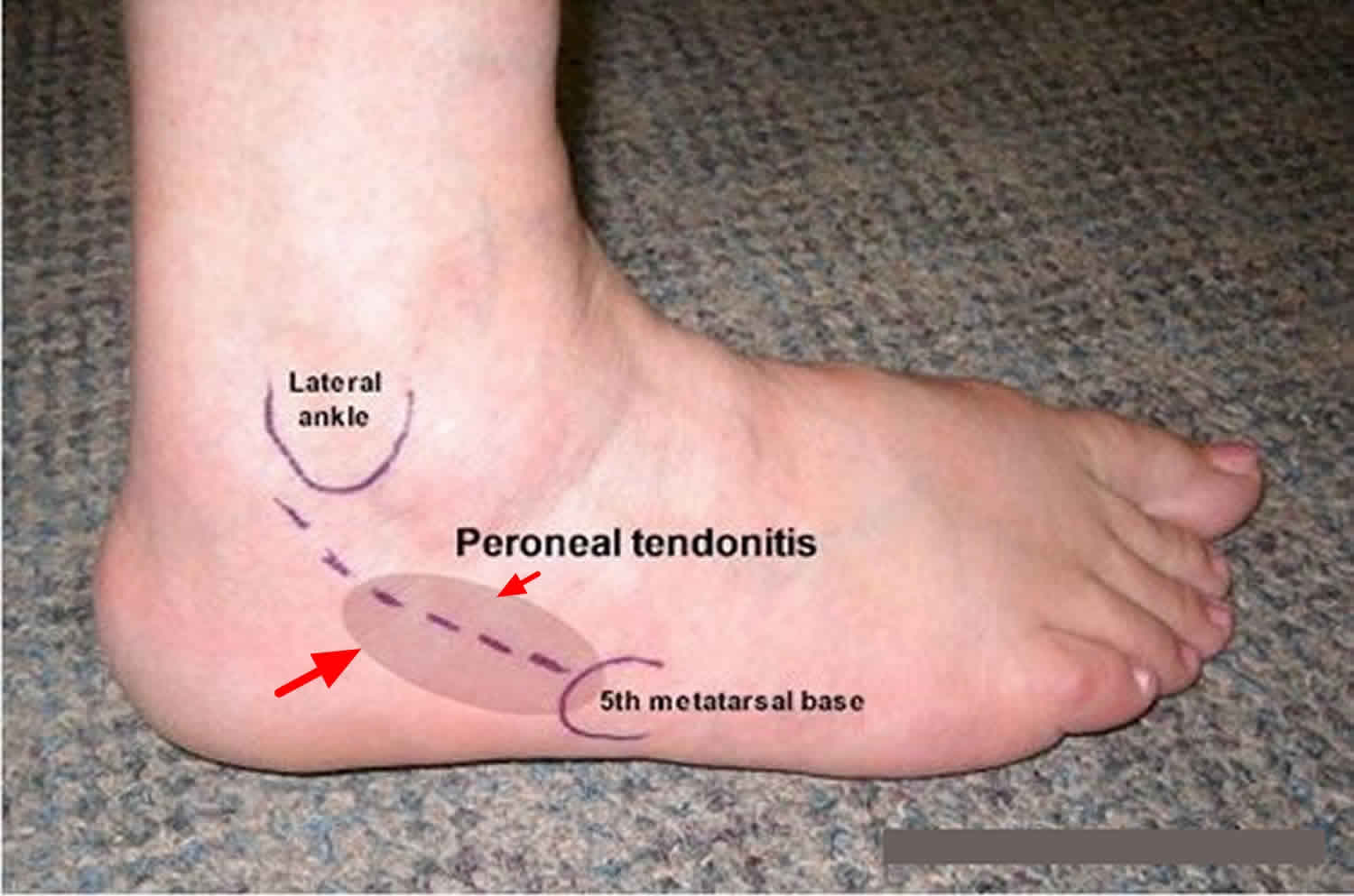
Peroneal tendonitis
Peroneal tendonitis is an inflammation and degeneration of the two peroneal tendons (peroneus brevis and peroneus longus tendons) on the outer side of your foot. Peroneal tendonitis usually occurs when the tendons are overused or placed under too much tension, such as a repetitive activity that irritates the tendon over long periods of time. Micro-trauma from overuse or repetitive tension on the peroneal tendons, or an ankle injury such as a sprain, damages the peroneal tendons which can lead to peroneal tendonitis 1.
People with peroneal tendonitis typically have either tried a new exercise or have markedly increased their activities. Characteristic activities include marathon running or others that require repetitive use of the ankle. Patients usually have pain around the back and outside of the ankle. There usually is no history of a specific injury.
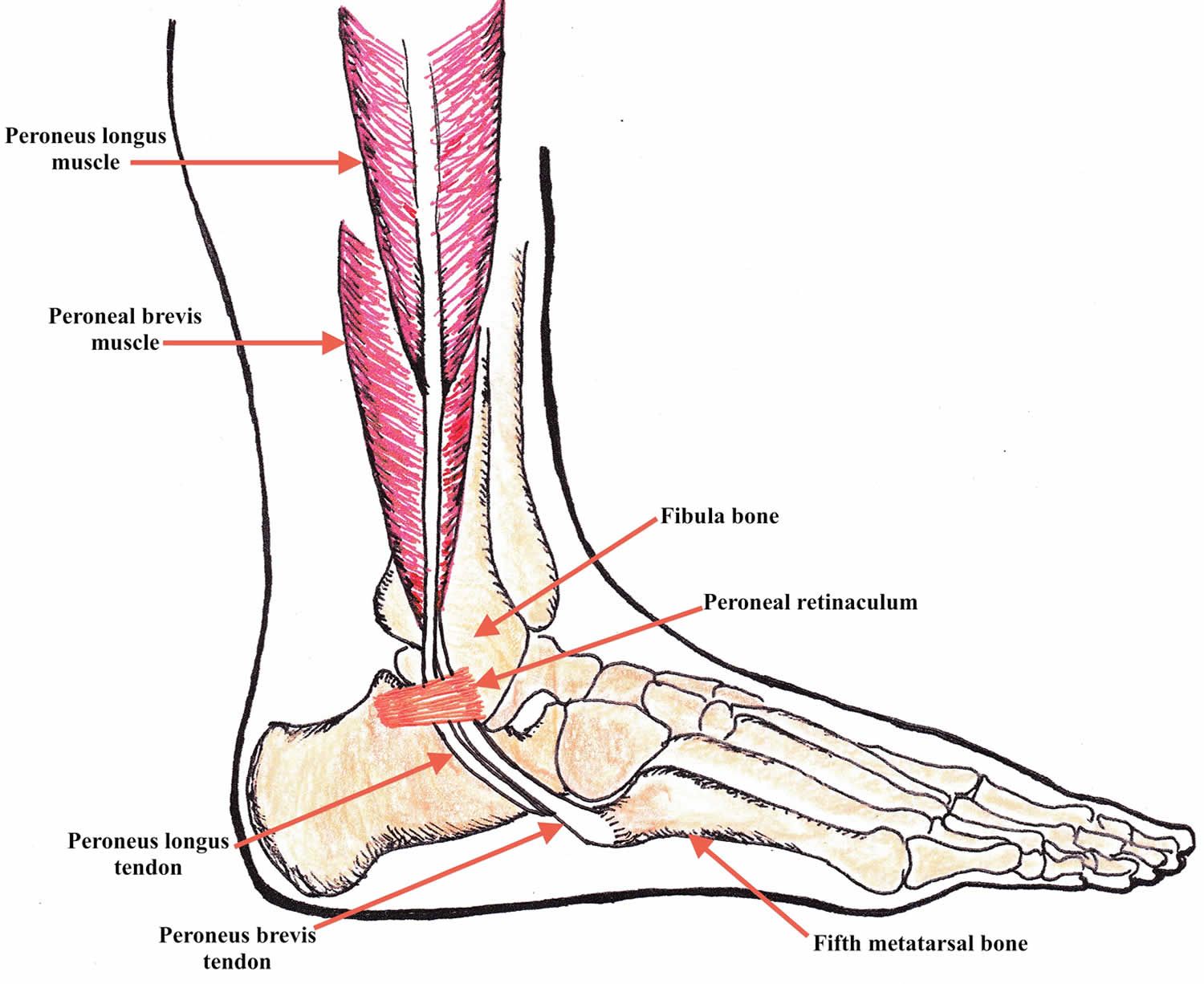
Tendons are strong, cord-like structures that link muscles to bones. In order to move, our muscles contract, which pulls on the appropriate tendon which in turn pulls on the appropriate bone.
There are two peroneal tendons that run along the back of the fibula. The first is called the peroneus brevis. The term “brevis” implies short. It is called this because it has a shorter muscle and starts lower in the leg. It then runs down around the back of the bone called the fibula on the outside of the leg and connects to the fifth metatarsal on the side of the foot.
The peroneus longus takes its name because it has a longer course. It starts higher on the leg and runs all the way underneath the foot to connect to the first metatarsal on the other side. Both tendons share the major job of turning the ankle to the outside. The tendons are held in a groove behind the back of the fibula and are covered by a ligament-type tissue called a retinaculum.
The two peroneal tendons work to pull your foot and toes downwards, known as “plantarflexion” and to turn your foot outwards, known as “eversion”.
Peroneal tendons anatomy
A tendon is a band of tissue that connects a muscle to a bone and allow them to exert their force across the joints that separate bones. The two peroneal tendons in the foot run side by side behind the outer ankle bone called the fibula. Peroneus brevis tendon attaches to the outer part of the midfoot (into the lateral base of the fifth metatarsal), while the peroneus longus tendon runs under the foot and attaches near the inside of the arch into the plantar surfaces of the first metatarsal base and the medial cuneiform bone. The main function of the peroneal tendons is to stabilize the foot and ankle and protect them from sprains.
The peroneus brevis muscle originates medial to the peroneus longus muscle, from the lateral surface of the fibula and the intermuscular septa in the distal two-thirds of the lower leg. The peroneus longus muscle arises from the proximal fibula, the lateral tibial condyle and the adjacent intermuscular septae and fasciae 2. At the level of the ankle, both tendons share a common synovial sheath that is held in place by a fibro-osseous tunnel. This tunnel is bordered anteriorly by a sulcus in the dorsal fibula, called the retromalleolar groove, and posterolaterally by a fibrous band, the superior peroneal retinaculum. The superior peroneal retinaculum originates from the lateral margin of the distal fibula and the retromalleolar groove and inserts most typically onto the aponeurosis of the Achilles tendon or the lateral calcaneus. The superior peroneal retinaculum may include a small, fibrocartilaginous ridge at the fibular insertion, thus deepening the retromalleolar groove. The calcaneofibular ligament acts as an additional stabiliser on the medial side of the tunnel 3. In the fibular groove, the peroneus brevis tendon is typically situated adjacent to the bone, anteromedially to the peroneus longus tendon (peroneus longus tendon). Its profile on transverse sections is flat or mildly crescentic, whereas the peroneus longus tendon shows rounded contours 2. The inferior peroneal retinaculum is a less important stabiliser of the peroneal tendon distal to the fibular tip. It originates from the posterior lateral rim of the sinus tarsi in continuation with the inferior extensor retinaculum and inserts into the retrotrochlear eminence of the calcaneus 3. At the hindfoot, the peroneus longus tendon normally undercrosses the peroneus brevis tendon and runs plantar and deep (medial) to it. The peroneus brevis tendon inserts into the lateral base of the fifth metatarsal. The peroneus longus tendon is inflected medially to the plantar region at the cuboid notch and inserts into the plantar surfaces of the first metatarsal base and the medial cuneiform bone.
Figure 1. Peroneal tendons anatomy
Peroneal tendonitis causes
Peroneal tendonitis is caused by activities involving repetitive use of the peroneal tendon, overuse of the peroneal tendon or trauma (such as an ankle sprain).
There are a number of different causes of tendonitis in the peroneal muscles:
- Overuse: This the most common cause of peroneal tendonitis. Sudden increases in training levels, inappropriate footwear or poor training techniques tend to be to blame. Sports such as basketball, football and gymnastics, or anything requiring quick pivoting movements are also commonly associated with the disease
- Running: Runners who frequently run along slopes e.g. cambered roads or uneven surfaces, which cause the foot to excessively roll out into eversion, are more prone to peroneal tendonitis
- Injury: You may also be prone to peroneal problems if you have injured your ankle or suffered from recurrent ankle sprains. Repeatedly damaging the ligaments that support the foot and ankle leads to weakness and instability which can put more strain on the peroneal tendons
- Abnormal foot position: Typically if the heel is turned inwards slightly, known as “hindfoot varus” or you have high arches, you are at increased risk of peroneal tendonitis as these makes the peroneal muscles and therefore tendons work harder
- Muscle imbalance: Tightness in the calf muscles and weakness in the calf and peroneal muscles can lead to tendonitis.
Improper training or rapid increases in training and poor shoe wear can lead to peroneal tendonitis. Also, patients who have a high arch may be more susceptible because their heel is slightly turned inwards which requires that the peroneal tendons work harder. Their main job is to evert or turn the ankle to the outside, which fights against the inwards (varus) heel position. The harder the tendons work, the more likely patients are to develop tendonitis.
Peroneal tendonitis symptoms
People suffering from peroneal tendonitis tend to complain of pain and tenderness around the back and outside of their foot and ankle.
The pain from peroneal tendonitis tends to come on gradually over a few weeks or months, gets worse with activity and eases with rest.
Symptoms often tends to be worse first thing in the morning, easing once you are up and about. It may also hurt to turn your foot inwards, known as inversion, as this movement stretches the tendons.
Peroneal tendonitis complications
If the tendonitis is not addressed, the tendon can tear. Also, weakness of the tendons can lead to an ankle sprain. In the case of surgery, infection can develop. Nerve damage can occur if the sural nerve, which runs along the side of the foot and provides sensation to the foot, is cut or stretched. Instability itself can lead to many sprains which can damage the cartilage on the inside of the ankle.
Peroneal tendonitis diagnosis
Because peroneal tendon injuries are sometimes misdiagnosed and may worsen without proper treatment, prompt evaluation by a foot and ankle surgeon is advised.
Your orthopedic surgeon will take your history and perform an exam to make the diagnosis. Most patients with peroneal tendonitis will report overuse of activity, rapid increase in recent activity, or other training errors, along with pain in the back and outside of the ankle. During the exam, there often is pain when the surgeon touches the peroneal tendons.
It is important to distinguish this from pain over the fibula, which might indicate a different problem (e.g., stress reaction of the bone). Pain on the fibula occurs directly over the bone. Pain in the peroneals occurs slightly further behind. There also is pain when you turn the foot inside towards the middle of your body (inversion). You may also have weakness in trying to bring the foot to the outside (eversion). The surgeon also will look for the varus posturing of the heel, which means that the heel is turned inwards. This can predispose a patient to the problem. X-rays for peroneal tendonitis usually are normal. Ultrasound is a very effective and way to assess the tendons and can show an abnormal appearance or tear. An MRI also may be used to show a tear.
Peroneal tendonitis treatment
It can take a number of months for the symptoms of peroneal tendonitis to fully settle down so effective treatment is vital. The vast majority of peroneal tendonitis cases will heal without surgery. Non-operative treatment should be for 4 to 6 months to allow resolution of inflammation. This is because it is an overuse injury and can heal with rest. It is essential to avoid any activity which aggravates your symptoms, to allow the peroneal tendon to heal properly. Failure to do so will result in longer healing time. If there is significant pain, wearing a CAM walker boot for several weeks is a good idea. If there is no tenderness with walking, an ankle brace might be the next best step. Talk to your doctor about taking non-steroidal anti-inflammatories (NSAIDs) such as ibuprofen to reduce the pain and swelling.
You should limit how much you are walking or are on your feet until the pain improves. This usually takes several weeks. After this period you can resume training, but very slowly and based on pain. For patients with hindfoot varus, an orthotic that tilts the ankle to the opposite side may help relieve pressure on the peroneal tendons. It is important to talk to your doctor about changing your training. This includes using new shoes for running or cross-training instead. Physical therapy also is very important to strengthen the peroneal tendons.
There is some interest in using platelet-rich plasma 4 or amniotic tissue to help stimulate healing growth. Currently, there are no studies showing that this works for the peroneal tendons. Steroids probably are best avoided as they can actually damage tendons.
Surgical treatment is indicated if the pain does not get better with rest. Non-surgical treatment could last up to a year before considering surgery.
Peroneal tendonitis surgical treatment include:
- Open Debridement and synovectomy
- Arthroscopic peroneal tendoscopy
If there is a tear, meaning a split that runs along the length of the tendons, one could consider cleaning it out and repairing the tendon. Sometimes, making the groove in the back of the bone of the fibula deeper allows the tendons more space and can help as well. Finally, if the tendon is very bad, a surgeon may need to resect the tendon and connect both the longus and brevis together. Only the specific tendon involved should be addressed. Occasionally, both may be involved.
Peroneal tendonitis recovery
Patients usually recover fully but this can take considerable time. You must be patient and allow the tendon to heal before going back to activity. If you need surgery, your recovery time may be substantial. You may be instructed not to bear weight for about six weeks. Your doctor likely will order physical therapy once you’re ready.
The outcome usually is good. However, sometimes it takes time for people to get back to their activity. When a tear develops and there is chronic thickening of the tendon, the outcomes are not as good.
- Schepsis AA, Busconi BD. Sports medicine. Philadelphia, Pa: Lippincott Williams & Wilkins; 2006.[↩]
- Normal variants and diseases of the peroneal tendons and superior peroneal retinaculum: MR imaging features. Wang XT, Rosenberg ZS, Mechlin MB, Schweitzer ME. Radiographics. 2005 May-Jun; 25(3):587-602.[↩][↩]
- MRI features of chronic injuries of the superior peroneal retinaculum. Rosenberg ZS, Bencardino J, Astion D, Schweitzer ME, Rokito A, Sheskier S. AJR Am J Roentgenol. 2003 Dec; 181(6):1551-7.[↩][↩]
- Dallaudière B, Pesquer L, Meyer P, Silvestre A, Perozziello A, Peuchant A, Durieux MH, Loriaut P, Hummel V, Boyer P, Schouman-Claeys E, Serfaty JM. Intratendinous injection of platelet-rich plasma under US guidance to treat tendinopathy: a long-term pilot study. J Vasc Interv Radiol. 2014 May;25(5):717-23.[↩]