What is a PET scan
PET scan stands for Positron Emission Tomography scan, is a modern non-invasive imaging technique that uses small amounts of radioactive materials called radiotracers, a special camera and a computer to help evaluate your organ, tissue functions and to produce detailed 3-dimensional images of the inside of your body 1. A PET scan measures important body functions, such as blood flow, oxygen use, and sugar (glucose) metabolism, to help doctors evaluate how well organs and tissues are functioning as well as what they look like. By identifying body changes at the cellular level, PET may detect the early onset of disease before it is evident on other imaging tests.
Different types of positron-emitting (radioactive) substances (radiotracers) can be used in PET scan. Depending on the substance used, different kinds of chemical or functional changes can be imaged. A radiotracer is essentially a biological compound of interest labelled with a positron emitting isotope, such as 11C, 18F, and 15O. These isotopes are used because they have relatively short half-lives (minutes to less than two hours), allowing the tracers to reach equilibrium in the body, but without exposing the subjects to prolonged periods of radiation. The most common type of PET procedure uses an imaging agent called FDG (2-deoxy-2-(18F)fluoro-D-glucose, a radioactive form of the sugar glucose), which shows the metabolic activity of tissues. Because cancerous tumors are usually more metabolically active than normal tissues, they appear different from other tissues on a PET scan. Other PET imaging agents can provide information about the level of oxygen in a particular tissue, the formation of new blood vessels, the presence of bone growth, or whether tumor cells are actively dividing and growing.
PET scan involves the intravenous injection of a positron-emitting radiopharmaceutical also called radiotracer [e.g., fluorodeoxyglucose (FDG)] and waiting to allow for systemic distribution, and then scanning to detect and quantify the patterns of radiotracer [e.g. fluorodeoxyglucose (FDG)] accumulation in your body. Body cells take in different amounts of the sugar (glucose), depending on how fast they are growing. Cancer cells, which grow quickly, are more likely to take up larger amounts of the sugar (glucose) than normal cells.
Tumor cells have a high metabolic rate, and hence the fluorodeoxyglucose (FDG) compound is also metabolized by tumor cells. Fluorodeoxyglucose (FDG) is metabolized to FDG-6-phosphate which cannot be further metabolized by tumor cells, and hence it accumulates and concentrates in tumor cells. This accumulation is detected and quantified by the PET scan.
Radionuclides decay in your body with the release of a positron (anti-particle of the electron, with electric charge of +1 e, a spin of 1/2 same as electron, sometimes referred to as a β+ particle). The positron travels a short distance and annihilates with an electron. The annihilation reaction results in the formation of two high energy photons which travel in diametrically opposite directions.
Each photon has an energy of 511 keV. Two detectors at opposite ends facing each other detect these two photons traveling in opposite directions, and the radioactivity is localized somewhere along a line between the two detectors. This is referred to as the line of response.
PET scan images can clearly show the part of your body being investigated, including any abnormal areas, and can highlight how well certain functions of the body are working.
Although the physiologic information afforded by PET scan imaging is invaluable, the quality of obtained data is poor/noisy and limits imaging spatial resolution. For this reason, PET scans are often combined with CT imaging to produce even more detailed images, allowing correlation between functional and anatomical imaging (“hybrid imaging”). This is known as a PET-CT scan. Combining CT and PET may provide a more complete picture of a tumor’s location and growth or spread than either test alone. PET/CT scanners give information on any areas of increased cell activity (from the PET), as well as show more detail in these areas (from the CAT scan). This helps doctors pinpoint tumors. The combined procedure may improve the ability to diagnose cancer, to determine how far a tumor has spread, to plan treatment, and to monitor response to treatment. Combined PET/CT may also reduce the number of additional imaging tests and other procedures a patient needs. But they also expose the patient to more radiation. Today, almost all PET scans are performed on instruments that are combined PET and CT scanners. The combined PET/CT scans provide images that pinpoint the anatomic location of abnormal metabolic activity within the body. The combined scans have been shown to provide more accurate diagnoses than the two scans performed separately.
PET scans may also occasionally be combined with an MRI scan also known as a PET-MRI scan.
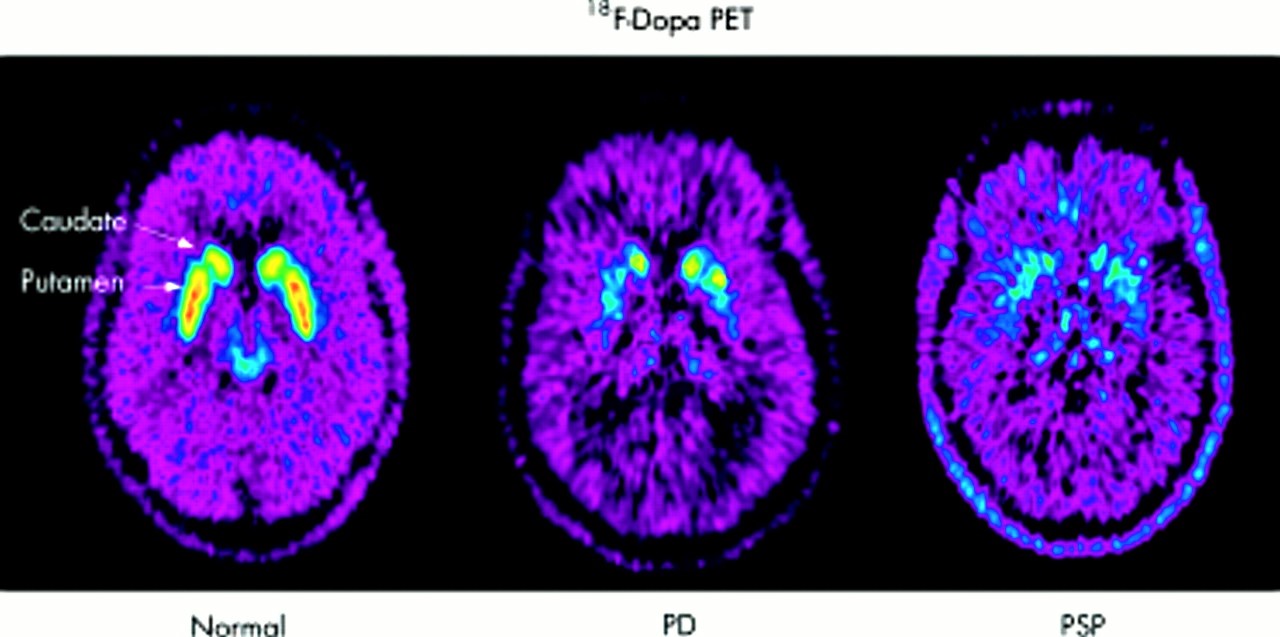
Figure 1. PET scan brain
Footnote: 18F-Dopa PET in a healthy volunteer (normal); in a subject with Parkinson’s disease (PD) showing asymmetrical loss of putaminal 18F-dopa Ki, with relative preservation of the caudate Ki earlier on in the disease; and in a subject with progressive supranuclear palsy (PSP) showing diffuse and symmetrical decrease in striatal Ki.
[Source 2 ]How long does a pet scan take?
The actual PET scan usually takes 30 to 60 minutes, plus the waiting time (about 1 hour) after the radiotracer material is given. However, the whole procedure may take up to 2 hours to complete especially if you’re having a combined PET-CT scan or PET-MRI scan.
How PET scans work
PET scanners work by detecting the radiation given off by a substance injected into your arm called a radiotracer as it collects in different parts of your body.
In most PET scans a radiotracer called fluorodeoxyglucose (FDG) is used, which is similar to naturally occurring glucose (a type of sugar) so your body treats it in a similar way.
By analyzing the areas where the radiotracer does and doesn’t build up, it’s possible to work out how well certain body functions are working and identify any abnormalities.
For example, a concentration of fluorodeoxyglucose (FDG) in the body’s tissues can help identify cancerous cells because cancer cells use glucose at a much faster rate than normal cells.
PET scan vs CAT scan
Computerized axial tomography (CAT) or better known as computerized tomography (CT), is an imaging procedure that uses special x-ray equipment and in some cases a contrast material, to create detailed pictures, or scans, of areas inside the body. These images can then be interpreted by a radiologist on a computer monitor. CT imaging provides excellent anatomic information.
The term tomography comes from the Greek words tomos (a cut, a slice, or a section) and graphein (to write or record). Each picture created during a CT procedure shows the organs, bones, and other tissues in a thin “slice” of the body. The entire series of pictures produced in CT is like a loaf of sliced bread—you can look at each slice individually (2-dimensional pictures), or you can look at the whole loaf (a 3-dimensional picture). Computer programs are used to create both types of pictures.
Most modern CT machines take continuous pictures in a helical (or spiral) fashion rather than taking a series of pictures of individual slices of the body, as the original CT machines did. Helical CT has several advantages over older CT techniques: it is faster, produces better 3-D pictures of areas inside the body, and may detect small abnormalities better. The newest CT scanners, called multislice CT or multidetector CT scanners, allow more slices to be imaged in a shorter period of time.
In addition to its use in cancer, CT is widely used to help diagnose circulatory (blood) system diseases and conditions, such as coronary artery disease (atherosclerosis), blood vessel aneurysms, and blood clots; spinal conditions; kidney and bladder stones; abscesses; inflammatory diseases, such as ulcerative colitis and sinusitis; and injuries to the head, skeletal system, and internal organs. CT can be a life-saving tool for diagnosing illness and injury in both children and adults.
During a CT procedure, the person lies very still on a table, and the table passes slowly through the center of a large x-ray machine. With some types of CT scanners, the table stays still and the machine moves around the person. The person might hear whirring sounds during the procedure. At times during a CT procedure, the person may be asked to hold their breath to prevent blurring of the images.
Sometimes, CT involves the use of a contrast (imaging) agent, or “dye.” The dye may be given by mouth, injected into a vein, given by enema, or given in all three ways before the procedure. The contrast dye highlights specific areas inside the body, resulting in clearer pictures. Iodine and barium are two dyes commonly used in CT.
In very rare cases, the contrast agents used in CT can cause allergic reactions. Some people experience mild itching or hives (small bumps on the skin). Symptoms of a more serious allergic reaction include shortness of breath and swelling of the throat or other parts of the body. People should tell the technologist immediately if they experience any of these symptoms, so they can be treated promptly. Very rarely, the contrast agents used in CT can also cause kidney problems in certain patients. These kidney problems usually do not have any symptoms, but they can be detected by running a simple test on a blood sample.
CT does not cause any pain. However, lying in one position during the procedure may be slightly uncomfortable. The length of a CT procedure depends on the size of the area being scanned, but it usually lasts only a few minutes to half an hour. For most people, the CT is performed on an outpatient basis at a hospital or a radiology center, without an overnight hospital stay.
Some people are concerned about experiencing claustrophobia during a CT procedure. However, most CT scanners surround only portions of the body, not the whole body. Therefore, people are not enclosed in a machine and are unlikely to feel claustrophobic.
Women should let their health care provider and the technologist know if there is any possibility that they are pregnant, because radiation from CT can harm a growing fetus.
PET scan vs MRI scan
Magnetic resonance imaging (MRI) uses a powerful magnetic field, radio waves and a computer to produce detailed pictures of the body’s internal structures that are clearer, more detailed and more likely in some instances to identify and accurately characterize disease than other imaging methods. It is used to evaluate the body for a variety of conditions, including tumors and diseases of the liver, heart, and bowel.
MRI does not use radiation (no X-rays) so they are safer for pregnant women and young children, but because the imaging is created with magnets, anyone who had metal implants should not get an MRI. There’s no evidence to suggest MRI scans pose a risk during pregnancy. However, as a precaution, MRI scans aren’t usually recommended during pregnancy, particularly in the first three months.
An MRI scan can be used to examine almost any part of the body, including the:
- brain and spinal cord
- bones and joints
- breasts
- heart and blood vessels
- internal organs, such as the liver, womb or prostate gland
The results of an MRI scan can be used to help diagnose conditions, plan treatments and assess how effective previous treatment has been.
Who can have MRI
Magnetic resonance imaging (MRI) is very safe and most people can have the procedure, including pregnant women and babies.
However, there are some instances where an MRI scan may not be recommended, because the strong magnets used during the scan can affect any metal implants or fragments in your body.
Before having an MRI scan, you should tell medical staff if:
- you think you have any metal in your body
- you’re pregnant or breastfeeding
There’s no evidence to suggest MRI scans pose a risk during pregnancy. However, as a precaution, MRI scans aren’t usually recommended during pregnancy, particularly in the first three months.
Metal implants or fragments
Having something metallic in your body doesn’t necessarily mean you can’t have an MRI scan, but it’s important for medical staff carrying out the scan to be aware of it.
They can decide on a case-by-case basis if there are any risks, or if further measures need to be taken to ensure the scan is as safe as possible. For example, it may be possible to make a pacemaker or defibrillator MRI-safe, or to monitor your heart rhythm during the procedure.
If you’re unsure about any metal fragments in your body, you may need an X-ray.
Some examples of metal implants or fragments include:
- a pacemaker – an electrical device used to control an irregular heartbeat
- an implantable cardioverter-defibrillator (ICD) – a similar device to a pacemaker that uses electrical shocks to regulate heartbeats
- metal plates, wires, screws or rods – used during surgery for bone fractures
- a nerve stimulator – an electrical implant used to treat long-term nerve pain
- a cochlear implant – a device similar to a hearing aid that’s surgically implanted inside the ear
- a drug pump implant – used to treat long-term pain by delivering painkilling medication directly to an area of the body, such as the lower back
- brain aneurysm clips – small metal clips used to seal blood vessels in the brain that would otherwise be at risk of rupturing (bursting)
- metallic fragments in or near your eyes or blood vessels (common in people who do welding or metalwork for a living)
- prosthetic (artificial) metal heart valves
- penile implants – used to treat erectile dysfunction (impotence)
- eye implants – such as small metal clips used to hold the retina in place
- an intrauterine device (IUD) – a contraceptive device made of plastic and copper that fits inside the womb
- artificial joints – such as those used for a hip replacement or knee replacement
- dental fillings and bridges
- tubal ligation clips – used in female sterilisation
- surgical clips or staples – used to close wounds after an operation
Tattoos
Some tattoo ink contains traces of metal, but most tattoos are safe in an MRI scanner. Tell the radiographer immediately if you feel any discomfort or heat in your tattoo during the scan.
MRI scan prep
On the day of your MRI scan, you should be able to eat, drink and take any medication as usual, unless advised otherwise.
In some cases, you may be asked not to eat or drink anything for up to four hours before the MRI scan, and sometimes you may be asked to drink a fairly large amount of water beforehand. This depends on the area being scanned.
When you arrive at the MRI center, you’ll usually be asked to fill in a questionnaire about your health and medical history. This helps the medical staff to ensure you have the scan safely.
Once you’ve completed the questionnaire, you’ll usually be asked to give your signed consent for the scan to go ahead.
As the MRI scanner produces strong magnetic fields, it’s important to remove any metal objects from your body, including:
- watches
- jewellery, such as earrings and necklaces
- piercings, such as ear, nipple and nose rings
- dentures (false teeth)
- hearing aids
- wigs (some wigs contain traces of metal)
Any valuables can usually be stored in a secure locker.
Depending on which part of your body is being scanned, you may need to wear a hospital gown during the procedure. If you do not need to wear a gown, you should wear clothes without metal zips, fasteners, buttons, underwire (bras), belts or buckles.
Contrast dye
Some MRI scans involve having an injection of contrast dye. This makes certain tissues and blood vessels show up more clearly and in greater detail.
It’s possible for contrast dye to cause tissue and organ damage in people with severe kidney disease. If you have a history of kidney disease, you may be given a blood test to determine how well your kidneys are functioning and whether it’s safe to proceed with the scan.
You should also let the staff know if you have a history of allergic reactions or any blood clotting problems before having the injection.
Anesthesia and sedatives
An MRI scan is a painless procedure, so anesthesia (painkilling medication) isn’t usually required. If you’re claustrophobic, you can ask for a mild sedative to help you relax – you should ask your doctor or consultant well in advance of having the scan.
If you decide to have a sedative during the MRI scan, you’ll need to arrange for a friend or family member to drive you home afterwards, as you won’t be able to drive for 24 hours.
General anaesthetic is often used when young children and babies have an MRI scan. This is because it’s very important to stay still during the scan, which young children and babies are often unable to do when they’re awake.
The MRI scanner will make loud tapping noises at certain times during the procedure. This is the electric current in the scanner coils being turned on and off. You’ll be given earplugs or headphones to wear.
You’re usually able to listen to music through headphones during the scan if you want to, and in some cases you can bring your own CD.
You’ll be moved out of the scanner when your scan is over.
MRI contraindications
There are few contraindications to MRI. Most contraindications to MRI can be divided into the following groups:
- Implanted devices and other metallic devices
- Pacemakers and other implanted electronic devices
- Aneurysm clips and other magnetizable materials
- Cochlear implants
- Some artificial heart valves
- Intraocular metallic foreign bodies
- Screening CT of the orbits if history suggests possible metallic foreign body in the eye
- Unstable patients (most resuscitation equipment cannot be brought into the scanning room)
- Pregnancy (relative contraindication due to unknown effects on the fetus)
- Other – severe agitation, or claustrophobia (may require anesthesia assistance)
MRI Advantages
The advantages of MRI include:
- Images may be acquired in multiple planes (axial, sagittal, coronal, or oblique) without repositioning the patient.
- MRI images demonstrate superior soft tissue contrast than CT scans and plain films making it the ideal examination of the brain, spine, joints and other soft tissue body parts
- Some angiographic (blood vessels) images can be obtained without the use of contrast material, unlike CT or conventional angiography
- Advanced techniques such as diffusion, spectroscopy and perfusion allow for precise tissue characterization rather than merely ‘macroscopic’ imaging
- Functional MRI (fMRI) allows visualization of both active parts of the brain during certain activities and understanding of the underlying networks. fMRI is technically challenging to perform as the techniques used to visualize cortical (brain) activity.
- Functional MRI (fMRI) detects subtle alteration in blood flow in response to stimuli or actions. It is used in two broad ways:
- Clinical practice
- typically in pre-surgical patients aimed at localizing eloquent areas (e.g. speech, motor function)
- Research
- often cohort of patients (often normals)
- aimed at elucidating novel neural networks
- Clinical practice
- Functional MRI (fMRI) detects subtle alteration in blood flow in response to stimuli or actions. It is used in two broad ways:
Disadvantages of MRI
There are many disadvantages and challenges to implementing MRI scanning.
MRI scans are more expensive than CT scans and take longer to acquire the images, so patient comfort is sometimes an issue. Additionally, images are subject to unique artefacts that must be recognized and abated.
MRI scans vary from ten minutes to an hour and even longer if an in-depth scan of a particular area is needed. Extremely sensitive, the MRI scanner produces high quality images of specific areas. However, this means that patients must lie completely still during the procedure. Often, patients are given a sedative to relax.
During an MRI, the patient lies still inside a tube-like scanner. The closed space can trigger claustrophobia in some patients. There are larger machines that accommodate more space.
MRI scanning is not safe for patients with some metal implants and foreign bodies. Careful attention to safety measures is necessary to avoid serious injury to patients and staff, and this requires special MRI compatible equipment and stringent adherence to safety protocols.
MRI safety
MRI scanners, although free from potentially cancer-inducing ionizing radiation (x-rays) found in plain radiography and CT scanners, have a host of safety issues which must be taken very seriously.
MRI safety can be divided into:
- main magnetic field
- varying magnetic (gradient) fields
- radiofrequency
Main magnetic field
The main magnetic field of a 1.5 Tesla magnet is about 30,000 times the strength of the earth’s magnetic field. It is strong enough to pull fork-lift tines off of machinery, pull heavy-duty floor buffers and mop buckets into the bore of the magnet, pull stretchers across the room and turn oxygen bottles into flying projectiles. Deaths have occurred from trauma as a result of these effects. Smaller objects such as pagers, bobby pins and pens have been known to be pulled off the person carrying them.
The strong field also affects common devices such as pacemakers and watches. The magnetic reed switch in modern pacemakers is disturbed by strong magnetic fields resulting in possible deleterious effects to the patient with one implanted. Mechanic watches will “freeze up” in a strong field, sometimes permanently.
Many intracranial aneurysm clips are ferromagnetic and as a result experience a torque or twisting in a magnetic field. Not everyone with an aneurysm clip experiences a fatal hemorrhage when placed in a magnet, but several cases have been reported.
Some types of heart valves (e.g. Starr-Edwards) are torqued in a magnetic field: however, this torque is less than the stresses that occur normally as a result of blood flow. Therefore heart valves are now considered not to be an absolute contraindication for MRI.
More of an annoyance than a safety problem is the ability of the magnetic field of a MRI machine to erase the information contained on the magnetic strip on ATM and credit cards. This may occur a short distance inside of the scanner room of a MRI machine.
Some metallic objects that are usually safe near an MRI machine are gold jewellery, shirt cuff-links and eyeglass frames.
Varying magnetic (gradient) fields
Varying magnetic fields are necessary in order to obtain images from MRI scanners. Changing magnetic field induce electrical currents in conductors (this is how an electrical generator works). In patients with metal in their body, the potential exists for electrical currents being induced in the metal with subsequent heating. This may occur with metal foreign bodies or some surgical implants. It does not universally occur and some patients with hip prostheses, for example, may be scanned without harm.
Very rapidly changing magnetic fields as may be achieved with echo planar imaging can cause nerve stimulation. This stimulation can affect motor nerves with resulting muscle contraction as well as the retina with resulting flickering lights called magnetophosphenes.
Radiofrequency
The radiofrequency (RF) power that is capable of being produced matches that of many small radio stations (15-20 kW). As a result there is the presence of heating effects from the radiofrequency (RF). In most pulse sequences, the heating is insignificant and does not exceed U.S. Food and Drug Administration (FDA) guidelines. New pulse sequences such as for echo planar imaging (EPI) and some spectroscopy localization techniques are capable of exceeding the FDA guidelines. Monitoring of the power deposition in patients is a requirement for FDA approval of clinical MRI scanners.
Potential for electrical shock exists with radiofrequency (RF) coils so proper grounding and insulation of coils is necessary. Any damage to coils or their cables needs prompt attention. Also looping of the cable to a coil can result in burns to patients that come into contact with them. It is best to avoid all contact with the radiofrequency (RF) coil cables.
Physics of MRI scan
MRI is based on the magnetization properties of atomic nuclei. A powerful, uniform, external magnetic field is employed to align the protons that are normally randomly oriented within the water nuclei of the tissue being examined. This alignment (or magnetization) is next perturbed or disrupted by introduction of an external Radio Frequency (RF) energy. The nuclei return to their resting alignment through various relaxation processes and in so doing emit RF energy. After a certain period following the initial RF, the emitted signals are measured. Fourier transformation is used to convert the frequency information contained in the signal from each location in the imaged plane to corresponding intensity levels, which are then displayed as shades of gray in a matrix arrangement of pixels. By varying the sequence of Radio Frequency (RF) pulses applied and collected, different types of images are created. Repetition Time (TR) is the amount of time between successive pulse sequences applied to the same slice. Time to Echo (TE) is the time between the delivery of the Radio Frequency (RF) pulse and the receipt of the echo signal.
Tissue can be characterized by two different relaxation times – T1 and T2. T1 (longitudinal relaxation time) is the time constant which determines the rate at which excited protons return to equilibrium. It is a measure of the time taken for spinning protons to realign with the external magnetic field. T2 (transverse relaxation time) is the time constant which determines the rate at which excited protons reach equilibrium or go out of phase with each other. It is a measure of the time taken for spinning protons to lose phase coherence among the nuclei spinning perpendicular to the main field.
MRI imaging sequences
The two basic types of MRI images are are T1-weighted and T2-weighted images, often referred to as T1 and T2 images. In general, T1- and T2-weighted images can be easily differentiated by looking at the cerebrospinal fluid (CSF). CSF is dark on T1-weighted imaging and bright on T2-weighted imaging.
A third commonly used sequence is the Fluid Attenuated Inversion Recovery (Flair). The Flair sequence is similar to a T2-weighted image except that the Time to Echo (TE) and Repetition Time (TR) times are very long. By doing so, abnormalities remain bright but normal CSF fluid is attenuated and made dark. This sequence is very sensitive to pathology and makes the differentiation between CSF and an abnormality much easier.
Diffusion weighted imaging (DWI) is designed to detect the random movements of water protons. Water molecules diffuse relatively freely in the extracellular space; their movement is significantly restricted in the intracellular space. Spontaneous movements, referred to as diffusion, rapidly become restricted in ischemic brain tissue. During ischemia, the sodium – potassium pump shuts down and sodium accumulates intracellularly. Water then shifts from the extracellular to the intracellular space due to the osmotic gradient. As water movement becomes restricted intracellularly, this results in an extremely bright signal on DWI. Thus, DWI is an extremely sensitive method for detecting acute stroke.
Table 1. Most common MRI Sequences and their Approximate TR and TE times
| TR (msec) | TE (msec) | |
| T1-Weighted (short TR and TE) | 500 | 14 |
| T2-Weighted (long TR and TE) | 4000 | 90 |
| Flair (very long TR and TE) | 9000 | 114 |
Abbreviations: TE = Time to Echo; TR = Repetition Time
The timing of radiofrequency (RF) pulse sequences used to make T1 images results in images which highlight FAT tissue within the body.
- T1-weighted images are produced by using short Time to Echo (TE) and Repetition Time (TR) times. The contrast and brightness of the image are predominately determined by T1 properties of tissue.
- T1 images can be thought of as a map of proton energy within fatty tissues of the body
- Fatty tissues include subcutaneous fat and bone marrow of the vertebral bodies
- Cerebrospinal fluid (CSF) contains no fat – so it appears black on T1-weighted images
- T1-weighted imaging can also be performed while infusing Gadolinium (Gad). Gadolinium is a non-toxic paramagnetic contrast enhancement agent. When injected during the scan, Gadolinium changes signal intensities by shortening T1. Thus, Gadolinium is very bright on T1-weighted images. Gadolinium enhanced images are especially useful in looking at vascular structures and breakdown in the blood-brain barrier [e.g., tumors, abscesses, inflammation (herpes simplex encephalitis, multiple sclerosis, etc.)].
The timing of radiofrequency pulse sequences used to make T2 images results in images which highlight FAT and WATER within the body.
- T2-weighted images are produced by using longer Time to Echo (TE) and Repetition Time (TR) times. In these images, the contrast and brightness are predominately determined by the T2 properties of tissue.
- T2 images are a map of proton energy within fatty AND water-based tissues of the body
- Fatty tissue is distinguished from water-based tissue by comparing with the T1 images – anything that is bright on the T2 images but dark on the T1 images is fluid-based tissue
- For example, the CSF is white on this T2 image and dark on the T1 image above because it is free fluid and contains no fat
- Note that the bone cortex is black – it gives off no signal on either T1 or T2 images because it contains no free protons
So, to makes things easy to remember:
- T1 images – 1 tissue type is bright – FAT
- T2 images – 2 tissue types are bright – FAT and WATER
What is a PET scan used for?
A PET scan can show how well certain parts of your body are working, rather than simply showing what they look like.
PET scans are particularly helpful for investigating confirmed cases of cancer to determine how far the cancer has spread and how well it’s responding to treatment.
A PET scan for cancer can help to:
- show up a cancer
- find out the stage of a cancer, so doctors know how big it is and whether it has spread
- show whether a lump is cancer or not
- show whether a cancer has spread to other parts of the body
- decide the best treatment for your cancer
PET scans can also show how well a cancer drug is working.
After you have had treatment for cancer, a CT scan may show that there are still some signs of the cancer left. But this may not be active disease. It could be scar tissue left over from cancer killed off by your treatment. A PET scan can show whether this tissue is active cancer or not.
PET scans are sometimes used to look for cancer in the lymph nodes in the center of the chest.
PET scans are sometimes used to help plan operations, such as a coronary artery bypass graft or brain surgery for epilepsy.
They can also help diagnose some conditions that affect the normal workings of the brain, such as dementia.
Uses of PET scan:
- Cancer
- detection, staging, response to treatment
- differentiation between radiation necrosis and recurrence
- Neurology
- early diagnosis of Alzheimer’s disease
- localization of seizure focus in interictal phase
- localizing eloquent areas (e.g. speech, motor function)
- Heart
- identification of hibernating myocardium
PET scan for heart
A heart positron emission tomography (PET) scan is an imaging test that uses a radioactive substance called a tracer to look for disease or poor blood flow in the heart. A heart PET scan takes about 90 minutes.
Unlike magnetic resonance imaging (MRI) and computed tomography (CT), which reveal the structure of and blood flow to and from organs, a PET scan gives more information about how organs and tissues are working.
A heart PET scan can detect whether areas of your heart muscle are receiving enough blood, if there is heart damage or scar tissue in the heart, or if there is a buildup of abnormal substances in the heart muscle.
Heart PET scan uses
- A heart PET scan can reveal the size, shape, position, and some function of the heart.
- It is most often used when other tests, such as echocardiogram (ECG) and cardiac stress tests do not provide enough information.
- A heart PET scan can be used to diagnose heart problems and show areas in which there is poor blood flow to the heart.
- Several PET scans may be taken over time to determine how well you are responding to treatment for heart disease.
Abnormal results may be due to:
- Coronary artery disease
- Heart failure or cardiomyopathy
How the heart PET scan is performed
A PET scan requires a small amount of radioactive material (tracer).
- This tracer is given through a vein (IV), most often on the inside of your elbow.
- It travels through your blood and collects in organs and tissues, including your heart.
- The tracer helps the radiologist see certain areas or diseases more clearly.
You will need to wait nearby as the tracer is absorbed by your body. This takes about 1 hour in most cases.
Then, you will lie on a narrow table, which slides into a large tunnel-shaped scanner.
- Electrodes for an electrocardiogram (ECG) will be placed on your chest. The PET scanner detects signals from the tracer.
- A computer changes the results into 3-D pictures.
- The images are displayed on a monitor for the radiologist to read.
You must lie still during the PET scan so that the machine can produce clear images of your heart.
Sometimes, the test is done in conjunction with stress testing (exercise or pharmacologic stress).
How to prepare for the heart PET scan
You may be asked not to eat anything for 4 to 6 hours before the scan. You will be able to drink water. Sometimes you may be given a special diet before the test.
Tell your health care provider if:
- You are afraid of close spaces (have claustrophobia). You may be given a medicine to help you feel sleepy and less anxious.
- You are pregnant or think you might be pregnant.
- You have any allergies to injected dye (contrast).
- You take insulin for diabetes. You will need special preparation.
Always tell your provider about the medicines you are taking, including those bought without a prescription. Sometimes, medicines may interfere with the test results.
PET scan procedure
PET scans are usually carried out on an outpatient basis. This means you won’t need to stay in hospital overnight.
It’s important to arrive on time for your PET scan because the radiotracer used has a short shelf-life and your PET scan may be cancelled if you’re late.
Your appointment letter will mention anything you need to do to prepare for your scan. You’ll usually be advised not to eat anything for 4 to 6 hours beforehand.
- fasting for 4-6 hours
- blood glucose level <150 mg/dl
- avoid strenuous activity 24 hours prior to imaging
- avoid speech 20 minutes prior to imaging
- the scan is carried out 60 minutes post-injection of fluorodeoxyglucose (FDG)
Drinking is allowed, but you should ideally just drink water. You should also avoid strenuous exercise for 24 hours before your appointment.
It’s a good idea to wear loose, comfortable clothes. It may be possible to wear these during the scan, although sometimes you may be asked to change into a hospital gown.
Avoid wearing jewellery and clothes that have metal parts, such as zips, because these will need to be removed.
If you’re claustrophobic, ask the hospital staff before the day of the scan about the possibility of having a mild sedative to help you relax.
In cases of fusion imaging such as PET-CT, the whole body CT scan is conducted first, followed by the whole-body PET scan and subsequently the two sets of images are co-registered.
A standard uptake value (SUV) is calculated at the end of the study i.e. ratio of activity per unit mass tissue to injected dose per unit body mass.
What happens during PET scan
Radiotracer injection
Before the PET scan, the radiotracer (FDG) is injected into a vein in your arm or hand. You’ll need to wait quietly for about an hour to give it time to be absorbed by the cells in your body.
It’s important to relax, keep as still as possible, and avoid talking while you wait because moving and speaking can affect where the radiotracer goes in your body.
You’ll be able to go to the toilet if you need to before having the scan.
The scan
Your radiographer takes you into the scanning room. The PET machine is large and shaped like a doughnut.
During the PET scan, you lie on a flat bed that’s moved into the center of the large, cylindrical scanner.
Stay still and don’t talk while the scanner takes pictures of your body.
PET scan usually takes up to 30 minutes. Having the scan is completely painless, but you may feel uncomfortable lying still for this long.
If you feel unwell at any point, there’s a buzzer you can press to alert the medical team. They’ll be able to see you throughout the scan.
After the scan
You shouldn’t experience any side effects after having a PET scan and can usually go home soon afterwards.
You can then eat and drink normally.
You’ll need someone to take you home if you’ve had medicine to help you relax. You won’t be able to drive for the rest of the day, as you might be drowsy.
If you are traveling abroad within a few days of your scan, it may be a good idea to take your appointment letter with you to show that you have had a scan. Most airports have sensitive radiation monitors which may pick up the trace of radiation following your test.
The results of your scan won’t usually be available on the same day. They’ll be sent to your specialist to be discussed at your next appointment.
PET scan side effects
A PET scan is a safe test for most people. But like all medical tests it has some risks. Your doctor and radiographer make sure the benefits of having the test outweigh these risks.
Pregnant women should only have the scan in an emergency. There’s a risk that the radiation could harm the baby. Contact the department as soon as you can before the scan if you are, or think you might be, pregnant.
Contact the department if you are breastfeeding. They will let you know if you need to stop breastfeeding for a length of time after the radioactive injection. You might need to store enough milk for one feed.
The radiation in the radioactive tracer is very small. Drinking plenty of fluids after your scan helps to flush the drug out of your system.
Any exposure to radiation carries a very small risk of potential tissue damage that could lead to cancer at a later date.
But the amount of radiation you’re exposed to in a standard PET scan is small – about the same as the amount you get from natural sources, such as the sun, over 3 years.
The radiotracer becomes quickly less radioactive over time and will usually be passed out of your body naturally within a few hours. Drinking plenty of fluid after the scan can help flush it from your body.
As a precaution, you may be advised to avoid prolonged close contact with pregnant women, babies or young children for a few hours after having a PET scan because you’ll be slightly radioactive during this time.
The CT component of a PET-CT scan also involves exposure to a small amount of additional radiation, but the risk of this causing any problems in the future is still very small.
- Positron Emission Tomography – Computed Tomography (PET/CT). https://www.radiologyinfo.org/en/info.cfm?pg=pet[↩]
- Tai YF, Piccini P. Applications of positron emission tomography (PET) in neurology. Journal of Neurology, Neurosurgery & Psychiatry 2004;75:669-676. https://jnnp.bmj.com/content/75/5/669[↩]