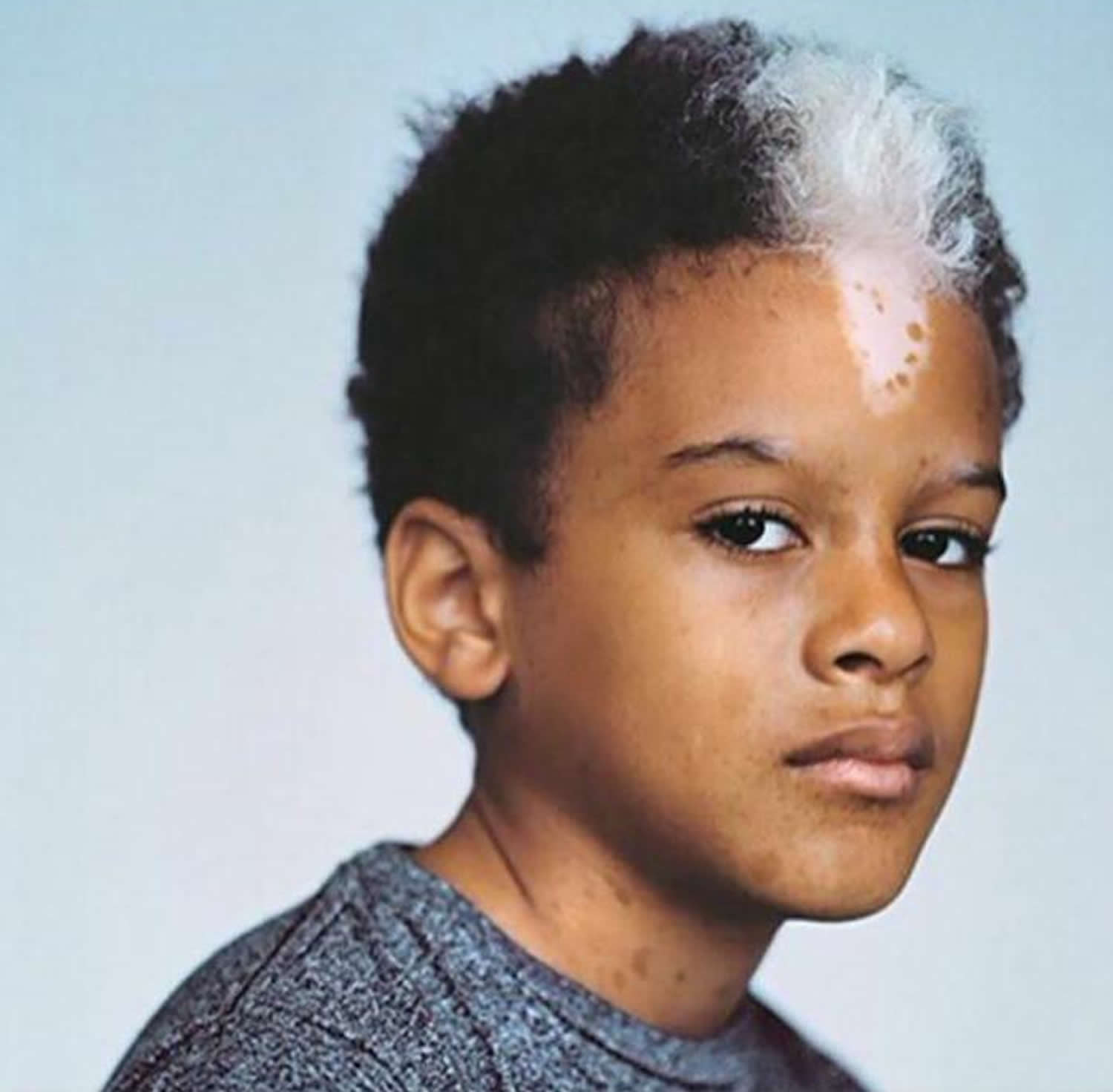
What is piebaldism
Piebaldism is a rare inherited condition characterized by the absence of cells called melanocytes in certain areas of the skin and hair, resulting in a white forelock (a patch of white hair directly above the forehead). The name piebaldism is derived from the words “pie” from magpie, which is a black and white plumage bird and “bald” from the bald eagle, the US national bird that has a white feathered head 1. Hence the major characteristic of piebaldism is a white forelock, a patch of white hair directly above the forehead. Other features include a white patch on the central portion of the forehead; white eyebrow and eyelash hair; and white patches of skin on the face (particularly the chin), trunk and extremities (hands and feet are not usually affected).
Piebaldism is a rare inherited disorder with an estimated incidence of less than 1 in 20,000 individuals 2. Both males and females are affected equally. There is no known racial predilection.
Melanocytes produce the pigment melanin, which contributes to hair, eye, and skin color. The absence of melanocytes leads to patches of skin and hair that are lighter than normal. Approximately 90 percent of affected individuals have a white section of hair near their front hairline (a white forelock). The eyelashes, the eyebrows, and the skin under the forelock may also be unpigmented.
Piebaldism is characterised by:
- White forelock in 80-90% of those affected (poliosis)
- White patch (due to absence of pigmentation) of the central portion of the forehead
- Eyebrow and eyelash hair may also be affected, either continuously or discontinuously with the forelock
- White patches of skin may also be seen on the face (particularly the chin), trunk and extremities (hands and feet are not usually affected)
- Often a narrow border of hyperpigmented skin surrounds the white unpigmented patches
- Sometimes islands of normal or hyperpigmented skin occur within the white patches
Piebaldism is present at birth and in most cases remain unchanged throughout life (do not increase in size or number).
People with piebaldism usually have other unpigmented patches of skin, typically appearing symmetrically on both sides of the body. There may be spots or patches of pigmented skin within or around the borders of the unpigmented areas.
The unpigmented patches are at increased risk of sunburn and skin cancer related to excessive sun exposure. Some people with piebaldism are self-conscious about the appearance of the unpigmented patches, which may be more noticeable in darker-skinned people. Aside from these potential issues, this condition has no effect on the health of the affected individual.
Piebaldism is inherited in an autosomal dominant fashion and is caused by mutations in the KIT gene and SNAI2 gene 3.
Although the depigmented areas of piebaldism are benign and stable, the appearance can be socially and psychologically debilitating for some patients. Treatment is challenging and focuses on improving cosmesis 3. Although temporary, cosmetic camouflage (make-up) and hair dye can improve quality of life 4. The depigmented areas have been successfully treated using dermabrasion and split-skin grafting, autologous melanocyte transplantation, epidermal sheet grafting, and autologous cell suspension transplantation after superficial full surface ablation 5. Due to the absence of the photoprotective effects of epidermal melanin, patients with piebaldism should receive education on proper sun protection of depigmented areas of the skin, including sunscreen and protective clothing.
What causes piebaldism?
Piebaldism can be caused by mutations in the KIT and SNAI2 genes. Piebaldism may also be a feature of other conditions, such as Waardenburg syndrome; these conditions have other genetic causes and additional signs and symptoms.
The KIT proto-oncogene provides instructions for making a protein that is involved in signaling within cells. KIT protein signaling is important for the development of certain cell types, including melanocytes. The KIT proto-oncogene mutations responsible for piebaldism lead to a nonfunctional KIT protein. The loss of KIT signaling is thought to disrupt the growth and division (proliferation) and movement (migration) of melanocytes during development, resulting in patches of skin that lack pigmentation.
The SNAI2 gene (often called SLUG) provides instructions for making a protein called snail 2. Research indicates that the snail 2 protein is required during embryonic growth for the development of cells called neural crest cells. Neural crest cells migrate from the developing spinal cord to specific regions in the embryo and give rise to many tissues and cell types, including melanocytes. The snail 2 protein probably plays a role in the formation and survival of melanocytes. SNAI2 gene mutations that cause piebaldism probably reduce the production of the snail 2 protein. Shortage of the snail 2 protein may disrupt the development of melanocytes in certain areas of the skin and hair, causing the patchy loss of pigment.
Piebaldism is sometimes mistaken for another condition called vitiligo, which also causes unpigmented patches of skin. People are not born with vitiligo, but acquire it later in life, and it is not caused by specific genetic mutations. For unknown reasons, in people with vitiligo the immune system appears to damage the melanocytes in the skin.
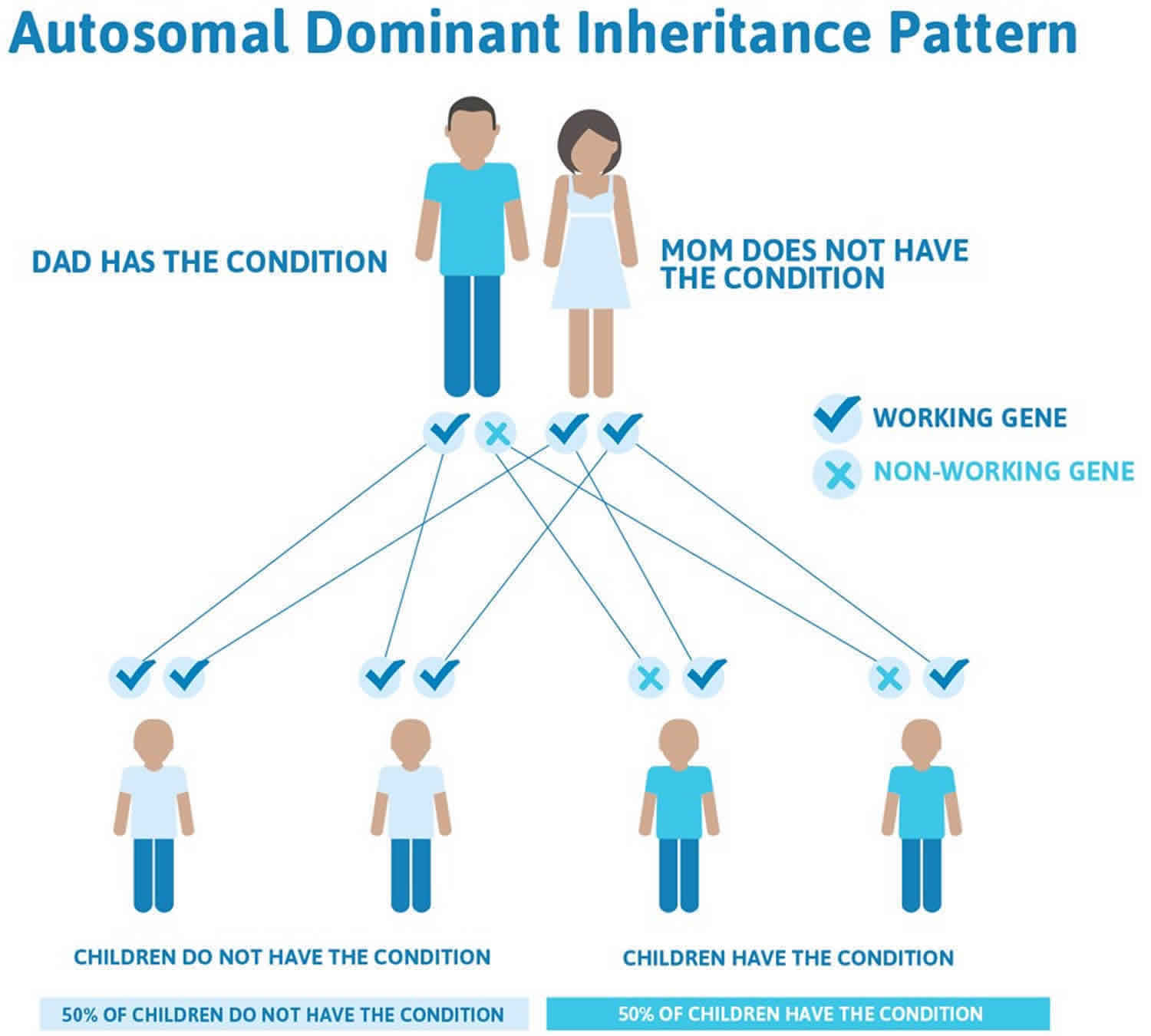
Piebaldism inheritance pattern
Piebaldism is inherited in an autosomal dominant pattern, which means one copy of the altered gene in each cell is sufficient to cause the disorder.
Often autosomal dominant conditions can be seen in multiple generations within the family. If one looks back through their family history they notice their mother, grandfather, aunt/uncle, etc., all had the same condition. In cases where the autosomal dominant condition does run in the family, the chance for an affected person to have a child with the same condition is 50% regardless of whether it is a boy or a girl. These possible outcomes occur randomly. The chance remains the same in every pregnancy and is the same for boys and girls.
- When one parent has the abnormal gene, they will pass on either their normal gene or their abnormal gene to their child. Each of their children therefore has a 50% (1 in 2) chance of inheriting the changed gene and being affected by the condition.
- There is also a 50% (1 in 2) chance that a child will inherit the normal copy of the gene. If this happens the child will not be affected by the disorder and cannot pass it on to any of his or her children.
There are cases of autosomal dominant gene changes, or mutations, where no one in the family has it before and it appears to be a new thing in the family. This is called a de novo mutation. For the individual with the condition, the chance of their children inheriting it will be 50%. However, other family members are generally not likely to be at increased risk.
Figure 1 illustrates autosomal dominant inheritance. The example below shows what happens when dad has the condition, but the chances of having a child with the condition would be the same if mom had the condition.
Figure 1. Piebaldism autosomal dominant inheritance pattern
People with specific questions about genetic risks or genetic testing for themselves or family members should speak with a genetics professional.
Resources for locating a genetics professional in your community are available online:
- The National Society of Genetic Counselors (https://www.findageneticcounselor.com/) offers a searchable directory of genetic counselors in the United States and Canada. You can search by location, name, area of practice/specialization, and/or ZIP Code.
- The American Board of Genetic Counseling (https://www.abgc.net/about-genetic-counseling/find-a-certified-counselor/) provides a searchable directory of certified genetic counselors worldwide. You can search by practice area, name, organization, or location.
- The Canadian Association of Genetic Counselors (https://www.cagc-accg.ca/index.php?page=225) has a searchable directory of genetic counselors in Canada. You can search by name, distance from an address, province, or services.
- The American College of Medical Genetics and Genomics (http://www.acmg.net/ACMG/Genetic_Services_Directory_Search.aspx) has a searchable database of medical genetics clinic services in the United States.
Piebaldism signs and symptoms
White patches on the skin (leukoderma) and decrease or absence of melanin (or color) in forehead hair (poliosis) will be present at birth in a characteristic ventral midline pattern. The most common finding is a white forelock in a triangular shape, which is present in up to 90% of cases of piebaldism (poliosis circumscripta) 6. The medial eyebrows and eyelashes may also be affected. The classic distribution of the well-circumscribed depigmented macules and patches includes the central forehead, anterior torso, and mid-portion of the extremities. Areas of hyperpigmentation may be present within or bordering the areas of depigmentation. Piebaldism is notable for the absence of extra-cutaneous manifestations.
Piebaldism diagnosis
Skin biopsy from patients with piebaldism demonstrates complete lack of melanocytes and melanin pigment. In vitiligo, lesions appear later in life and their configuration and distribution is quite different. If deafness is apparent and the distance between the eyes is greater than normal then the diagnosis of Waardenburg syndrome needs to be considered.
Piebaldism treatment
Piebaldism is a benign disorder. However, patients with piebaldism are at risk of sunburn and other disorders caused by overexposure to the sun. Patients must be educated about use of sunscreens, sun protective measures, and sun avoidance during peak hours of UV exposure, and self examination of the skin to detect any sun damage that may increase the risk of skin cancer.
Patients who are self-conscious about their appearance may benefit from the following treatments:
- Dermabrasion of areas of depigmentation followed by the application of melanocyte-enriched cell suspensions
- Melanocyte transplant by shaving off the top layer of skin (epidermis) and replacing it by shaved-off skin from another site
- Suction epidermal grafting or full-thickness punch grafts
- A combination of these methods may be required and can be augmented by the addition of UV light therapy.
- Less invasive methods for improving appearance can be achieved with cosmetic camouflage techniques.
Piebaldism prognosis
Individuals with piebaldism will present at birth with stable white patches on the skin (leukoderma) and decrease or absence of melanin (or color) in forehead hair (poliosis). Unlike vitiligo, these areas of depigmentation do not progress after birth. However, reports exist of rare cases of spontaneous repigmentation 7.
- Piebaldism. https://www.dermnetnz.org/topics/piebaldism[↩]
- Agarwal S, Ojha A. Piebaldism: A brief report and review of the literature. Indian Dermatol Online J. 2012 May;3(2):144-7[↩]
- Shah M, Zedek D. Piebaldism. [Updated 2019 Jul 14]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK544238[↩][↩]
- Saleem MD. Biology of human melanocyte development, Piebaldism, and Waardenburg syndrome. Pediatr Dermatol. 2019 Jan;36(1):72-84.[↩]
- Lommerts JE, Meesters AA, Komen L, Bekkenk MW, de Rie MA, Luiten RM, Wolkerstorfer A. Autologous cell suspension grafting in segmental vitiligo and piebaldism: a randomized controlled trial comparing full surface and fractional CO2 laser recipient-site preparations. Br. J. Dermatol. 2017 Nov;177(5):1293-1298.[↩]
- Thomas I, Kihiczak GG, Fox MD, Janniger CK, Schwartz RA. Piebaldism: an update. Int. J. Dermatol. 2004 Oct;43(10):716-9.[↩]
- Agarwal S, Ojha A. Piebaldism: A brief report and review of the literature. Indian Dermatol Online J. 2012 May;3(2):144-7.[↩]