Pilomatricoma
Pilomatricoma also called pilomatrixoma, trichomatricoma or calcifying epithelioma of Malherbe, is an uncommon, harmless, hair follicle tumor derived from hair matrix cells (from the cells at the base of hair follicles) 1, 2. Pilomatricoma tumors only occur in hair-bearing areas. Case studies report pilomatricoma tumor occurring in other areas of the body including the periocular and on the scrotum and vulva 3, 4, 5. These tumor cells can differentiate into hair matrix, hair cortex, follicular infundibulum, outer root sheath, and hair bulge 1. Pilomatricomas are typically found in the head and neck region, but also occur in the upper extremities and are rarely reported in other sites 6. The largest case series in the literature includes 346 pilomatrixomas of which 15.3 percent were observed in the upper extremities 7.
A pilomatricoma normally appears as a single pink or purplish lump containing white areas. The white areas are due to calcium (chalky) deposits and makes the lump feel hard as a bone.
Pilomatricomas are usually less than 3 cm in diameter, although rarely can be larger. They are most common on the head and neck or the upper body in children and teenagers, but can develop anywhere on the body at any age.
Pilomatricoma is most often diagnosed in young children but may also affect adults. The mean age of onset is 4.5 years, and 90% of patients are younger than ten years old 1. It is unusual in infants. There is a bimodal distribution, with a peak incidence between 0 and 20 years old and a second peak incidence between 50 and 65 years old 1. Pilomatricoma appears to be slightly more common in females than males and it occurs more commonly in whites 1, 8.
Cases have been reported of multiple pilomatricomas in association with the rare neurological condition myotonic dystrophy 8. Individual cases have also been reported of pilomatricomas arising in patients with a variety of other genetic disorders 8. However, the vast majority are not associated with any other abnormality 8.
Most people with isolated pilomatricoma do not have any other affected family members. However, rare families with multiple affected members have been reported. In these cases, the inheritance pattern of the condition (if any) is unknown 9.
Your doctor may suspect the diagnosis on examining the skin and may refer you for an ultrasound scan. The diagnosis is confirmed by specialist examination of a small tissue sample (a biopsy – when a tiny piece of skin is removed under local anesthetic).
Treatment may include surgery to cut out the lump. Surgery may be done if the pilomatrixoma is uncomfortable, is cosmetically bothersome, or to confirm the diagnosis.
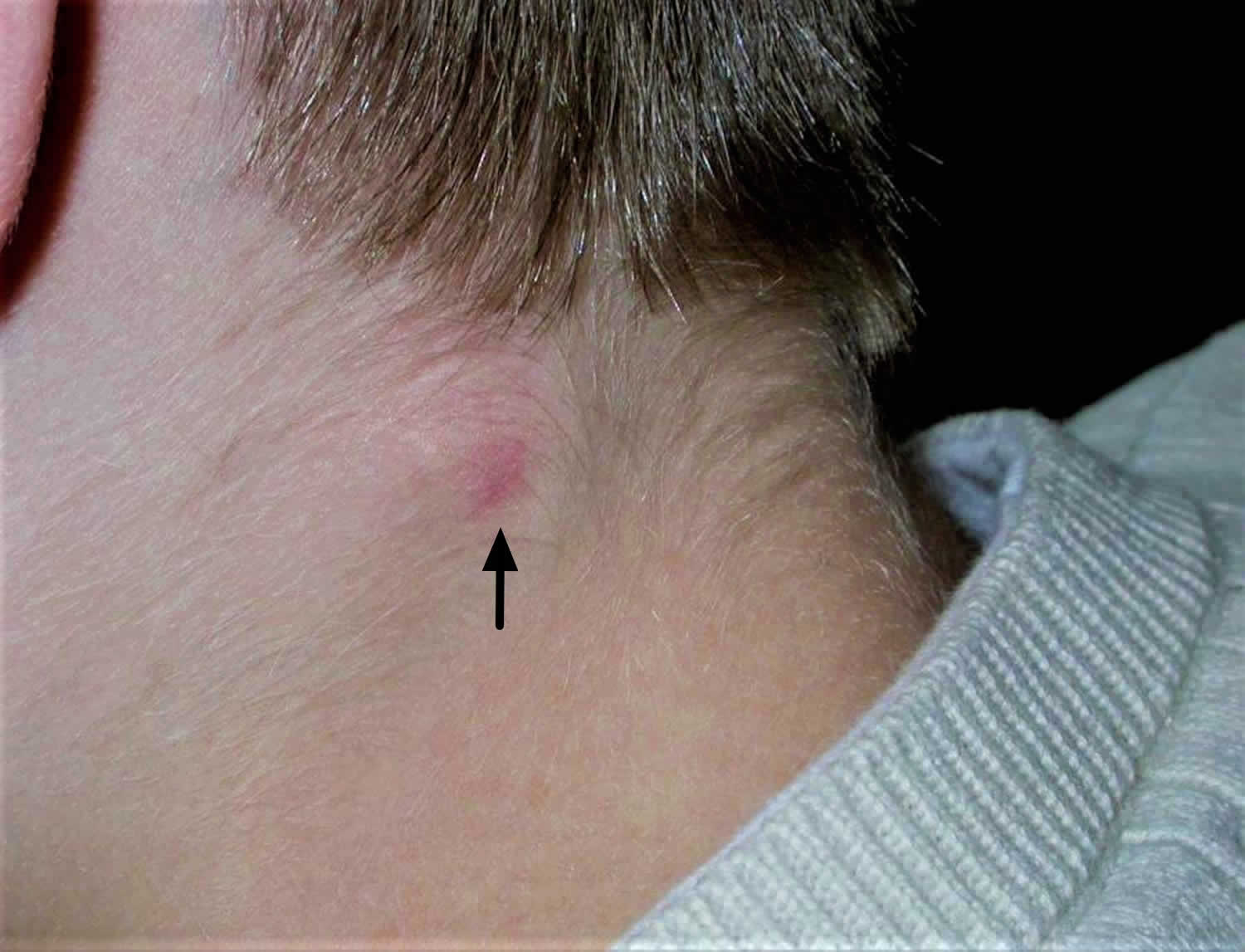
Figure 1. Pilomatricoma
[Source 10 ]Figure 2. Pilomatricoma
[Source 10 ]Figure 3. Pilomatrixoma
[Source 8 ]Figure 4. Giant pilomatricoma
[Source 8 ]Can a pilomatricoma be cured?
Yes, if a pilomatricoma is completely removed surgically (cut out or excised), it is considered to be cured. It is very unlikely that they will grow back after being removed. They do not tend to go away by themselves and will either stay the same size or slowly grow over the years.
Pilomatricoma causes
The cause of pilomatricoma (pilomatrixoma) is now known to be due to a localized mutation in a hair matrix cell 8. A familial component is seen in some cases as there is a genetic component to these lesions. Mutations in the exon 3 of the B-catenin (CTNNB1) gene are found in almost all cases of isolated pilomatricoma. An overactive proto-oncogene called BCL-2 suggests the normal process of cell death is suppressed, and mutations in CTNNB1 (exon 3 of the B-catenin) gene in most cases suggest loss of regulation of a protein complex called beta-catenin or LEF-1 8, 1. These mutations are somatic, which means they are acquired during a person’s lifetime and are present only in tumor cells. Somatic mutations are not inherited.
The CTNNB1 gene provides instructions for making a protein called beta-catenin 9. B-catenin protein plays an important role in sticking cells together (cell adhesion) and in communication between cells. B-catenin is a component of the cadherin protein, and it plays a role in hair follicle differentiation 1. B-catenin is also involved in cell signaling as part of the Wnt signaling pathway and this is seen in the hair matrix cells that are proliferating. This pathway promotes the growth and division (proliferation) of cells and helps determine the specialized functions a cell will have (differentiation). Wnt signaling is involved in many aspects of development before birth, as well as the maintenance and repair of adult tissues.
Among its many activities, beta-catenin appears to be necessary for the normal function of hair follicles 1. B-catenin protein is active in cells that make up a part of the hair follicle known as the matrix. These cells divide and mature to form the different components of the hair follicle and the hair shaft. As matrix cells divide, the hair shaft is pushed upward and extends beyond the skin.
Mutations in the CTNNB1 gene lead to a version of beta-catenin that is always turned on (constitutively active). The overactive protein triggers matrix cells to divide too quickly and in an uncontrolled way, leading to the formation of a pilomatricoma. Overexpression of BCL2 proto-oncogene also has been seen in immunohistochemical studies.
Most pilomatrix carcinomas, the malignant version of pilomatricoma, also have somatic mutations in the CTNNB1 gene. It is unclear why some pilomatricomas are cancerous but most others are not.
A small percentage (3.9%) of cases are caused by an external insult such as trauma, insect bites, or surgery 11, 12, 13.
Are pilomatricomas hereditary?
Most pilomatricomas do not run in families, but very rarely (less than 1 in 100,000) there may be a link to rare (less than 1 in 10,000) genetic disorders.
Pilomatricoma signs and symptoms
A pilomatricoma does not normally cause any symptoms unless it becomes inflamed or infected; when it becomes red and sore. Occasionally the growth may burst and release white and yellow chalky fluid. Pilomatricomas can sometimes be uncomfortable.
Pilomatricoma presents as a single skin-colored or purplish lesion 8:
- They are usually found on the head and neck, but they may occur on any site.
- They don’t usually cause any symptoms, but they may be tender.
- They may be skin colored, white or red.
- They may be regular or irregular in shape.
- Most pilomatricomas are 5–10 mm in diameter.
- They may remain stable for years or slowly grow in size up to several centimeters in diameter.
Pilomatricoma is characterized by calcification within the lesion, which makes it feel hard and bony, and often results in an angulated shape (the ‘tent’ sign).
Pilomatrixomas usually occur as solitary lesions, but multiple lesions can occur, often seen in syndromes such as myotonic dystrophy, Familial adenomatous polyposis, Gardner syndrome, Turner syndrome, xeroderma pigmentosum, Rubinstein-Taybi syndrome, Sotos syndrome, and basal cell nevus syndrome 1, 9.
Pilomatricoma complications
Complications of pilomatricoma are rare 14. Pilomatrix carcinoma is locally aggressive and can recur and approximately 90 cases have been reported in the literature. In several cases, it has demonstrated metastases. Many key features are similar between these benign and malignant counterparts; the primary differentiating characteristics include a high mitotic rate with atypical mitoses, central necrosis, infiltration of the skin and soft tissue, and invasion of blood and lymphatic vessels 15.
A few cases have been reported of multiple pilomatricomas in association with the rare neurological condition myotonic dystrophy. Individual cases have also been reported of pilomatricomas arising in patients with a variety of other genetic disorders. The vast majority are not associated with any other abnormality.
Disorders that can be associated with pilomatricoma include Gardner syndrome, which is characterized by multiple growths (polyps) and cancers of the colon and rectum; myotonic dystrophy, which is a form of muscular dystrophy; and Rubinstein-Taybi syndrome, which is a condition that affects many parts of the body and is associated with an increased risk of both benign and malignant tumors 9.
Pilomatricoma diagnosis
If pilomatricoma is suspected, dermoscopy may be helpful, showing a central whitish or grayish-blue structureless area. Redness and telangiectasia are sometimes observed 8.
If the nature of the skin lesions is uncertain, ultrasound scan may be recommended. The ultrasound scan of pilomatricoma is described as a doughnut within the dermis (mid layer of the skin) with a tail (the tail denotes calcification). Alternatively, the calcification may be detected by X-ray.
A biopsy will help to establish the cause of the lesion. Alternatively the whole lesion can be removed, providing both diagnosis and treatment. The histology of pilomatricoma is striking. It may show a sharply demarcated tumor surrounded by a fibrous capsule or a poorly demarcated tumor without capsule. There are darkly stained ‘basophilic’ cells and ‘shadow’ cells with missing nuclei. Calcium deposits are found in most lesions.
Pilomatricoma histopathology
Histopathology of pilomatrixoma shows a well-demarcated tumor with a surrounding capsule 1. Dermal cells extend into the subcutaneous tissue. There are islands of epithelial cells that contain basaloid matrical cells, shadow, ghost, or anucleated cells with eosinophilic cytoplasm, foreign body giant cells, and calcifications.
Pilomatrix carcinoma shows basaloid cells, atypia, and a high mitotic rate on histology. Ghost cells are present. Not many calcifications are seen. The histological features between pilomatrixoma and pilomatrix carcinoma are similar and can be difficult to differentiate.
Pilomatricoma treatment
The normal treatment for a pilomatricoma is to completely remove the lump surgically with a procedure known as ‘excision’. They do not disappear by themselves, and if not completely removed, they may recur. The recurrence rate is low, ranging from 0 to 3 percent 16. If a lesion recurs after excision or rapidly enlarges, it should be excised due to malignant potential or possible misdiagnosis.
Malignant pilomatrixoma can arise from benign pilomatrixoma through transformation 1. There are 125 reported cases of these rare, malignant pilomatrixoma, which are termed “pilomatrix carcinomas” 1. Pilomatrixomas that are likely to undergo malignant transformation have a higher degree of cellular pleomorphism, high mitotic rate and atypia, central necrosis, and more extensive infiltration into the skin, soft tissue, and blood and lymphatic vessels 1. Pilomatrix carcinoma occurs more commonly in men in the fifth to the seventh decade of life 1. There is only one known case of the carcinoma occurring in a child 1. It presents similar to pilomatrixoma and is firm non-tender nodules on the head or neck. The tumor is locally aggressive and can metastasize in 10% of cases 1. A predictor of metastasis is a local recurrence. The most common site of metastasis is the lungs. Treatment is excision with wide margins (5 to 30 mm), but the recurrence rate is high (50% to 60%) 1. Adjuvant radiation therapy or chemotherapy is used for recurrent disease or metastatic disease 1.
- Le C, Bedocs PM. Calcifying Epithelioma of Malherbe. [Updated 2023 Jun 12]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK493165[↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩]
- Birman MV, McHugh JB, Hayden RJ, Jebson PJ. Pilomatrixoma of the forearm: a case report. Iowa Orthop J. 2009;29:121‐123. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2723706[↩]
- Kim YS, Na YC, Huh WH, Kim JM. Malignant pilomatricoma of the cheek in an infant. Arch Craniofac Surg. 2018 Dec;19(4):283-286. doi: 10.7181/acfs.2018.02138[↩]
- Ciucă EM, Sălan AI, Camen A, Matei M, Şarlă CG, Mărgăritescu C. A patient with pilomatricoma in the parotid region: case report and review of the literature. Rom J Morphol Embryol. 2018;59(3):917-926. https://rjme.ro/RJME/resources/files/590318917926.pdf[↩]
- Arora A, Nanda A, Lamba S. Cyto-Histopathological Correlation of Skin Adnexal Tumors: A Short Series. J Cytol. 2018 Oct-Dec;35(4):204-207. doi: 10.4103/JOC.JOC_63_17[↩]
- Kumaran N, Azmy A, Carachi R, Raine PA, Macfarlane JH, Howatson AG. Pilomatrixoma – accuracy of clinical diagnosis. J Pediatr Surg. 2006;41:1755–1758. https://doi.org/10.1016/j.jpedsurg.2006.05.005[↩]
- Pirouzmanesh A, Reinisch JF, Gonzalez-Gomez I, Smith EM, Meara JG. Pilomatrixoma: A review of 346 cases. Plast Reconstr Surg. 2003;112:1784–1789.[↩]
- Pilomatricoma. https://dermnetnz.org/topics/pilomatricoma[↩][↩][↩][↩][↩][↩][↩][↩][↩][↩]
- Pilomatricoma. https://medlineplus.gov/genetics/condition/pilomatricoma[↩][↩][↩][↩]
- Pilomatricoma (syn. pilomatrixoma). https://www.pcds.org.uk/clinical-guidance/pilomatricoma-syn-pilomatrixoma[↩][↩]
- Lloyd M, Eagle RC, Wasserman BN. Pilomatrixoma Masquerading as Giant Chalazion. Ophthalmology. 2018 Dec;125(12):1936. doi: 10.1016/j.ophtha.2018.09.012[↩]
- Pinheiro TN, Fayad FT, Arantes P, Benetti F, Guimarães G, Cintra LTA. A new case of the pilomatrixoma rare in the preauricular region and review of series of cases. Oral Maxillofac Surg. 2018 Dec;22(4):483-488. doi: 10.1007/s10006-018-0724-8[↩]
- Caprio MG, Di Serafino M, Pontillo G, Vezzali N, Rossi E, Esposito F, Zeccolini M, Vallone G. Paediatric neck ultrasonography: a pictorial essay. J Ultrasound. 2019 Jun;22(2):215-226. doi: 10.1007/s40477-018-0317-2. Epub 2018 Sep 5. Erratum in: J Ultrasound. 2019 Mar;22(1):107. doi: 10.1007/s40477-018-0328-z[↩]
- Pilomatricoma. https://dermnetnz.org/topics/pilomatricoma). However, occasionally they grow to giant size several centimeters in diameter and pilomatrix carcinoma (cancer) has been very rarely reported ((Pilomatricoma. https://dermnetnz.org/topics/pilomatricoma[↩]
- Mikhaeel NG, Spittle MF. Malignant pilomatrixoma with multiple local recurrences and distant metastases: a case report and review of the literature. Clin Oncol (R Coll Radiol). 2001;13(5):386-9. doi: 10.1053/clon.2001.9296[↩]
- Agarwal RP, Handler SD, Matthews MR, Carpentieri D. Pilomatrixoma of the head and neck in children. Otolaryngol. Head and Neck Surg. 2001;125:510–515.[↩]