Radial head fracture
Radial head fractures represent approximately one-third of elbow fractures and 1% to 4% of fractures in adults. Radial head fractures are common injuries, occurring in about 20% of all acute elbow injuries. About 33% of elbow fractures and dislocations include injury to the radial head, the radial neck, or both. Many elbow dislocations also involve fractures of the radial head.
While the majority radial head fractures are isolated, a number of other injuries may also be seen 1:
- fracture of the coronoid process of the ulna
- medial collateral ligament tear
- interosseous membrane injury
- triangular fibrocartilage complex injury at the wrist (Essex-Lopresti fracture-dislocation)
Radial head fractures are more frequent in women than in men, and are more likely to happen in people who are between 30 and 40 years of age.
Radial head fractures and dislocations are traumatic injuries that require adequate treatment to prevent disability from stiffness, deformity, posttraumatic arthritis, nerve damage, or other serious complications. Radial head fractures and dislocations may be isolated just to the radial head (and neck) and the lateral elbow (and proximal forearm), or they may be part of a combined complex fracture injury pattern involving the other structures of the elbow, distal humerus, or forearm and wrist.
Radial head fracture treatment depends on the degree of displacement and involvement of the articular surface (as well as associated injuries). In general type I (see Mason classification below) injuries can be treated conservatively whereas type II injuries require open reduction and internal fixation (ORIF) 2. Type III injuries often require early complete excision of the radial head 1.
Radial head replacement is also an option, to help stabilize the elbow joint and prevent proximal migration of the radius 1.
Generally, patients can expect a good outcome although secondary osteoarthritic change is certainly encountered in patients with intra-articular fractures.
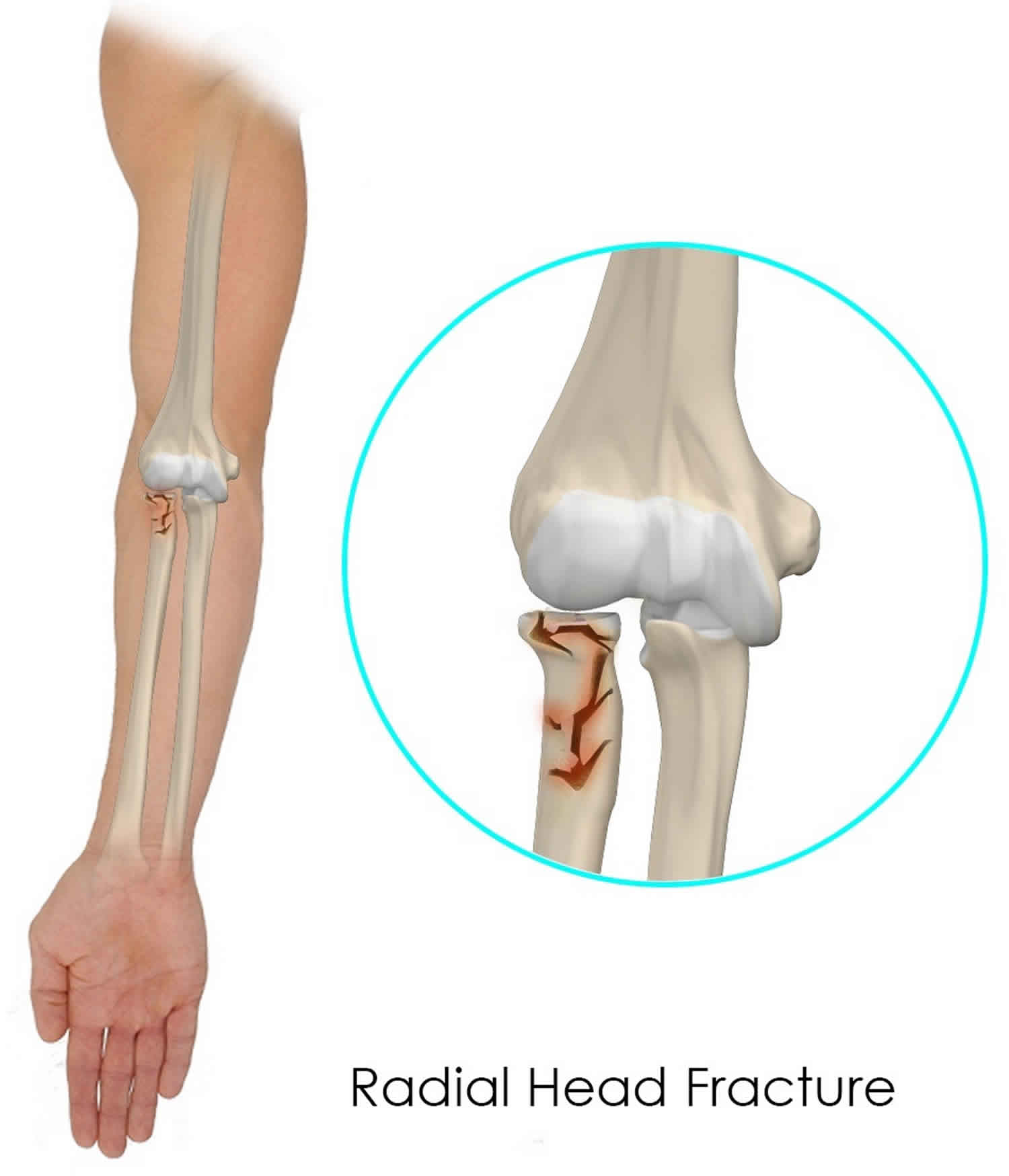
Figure 1. Radial head fracture
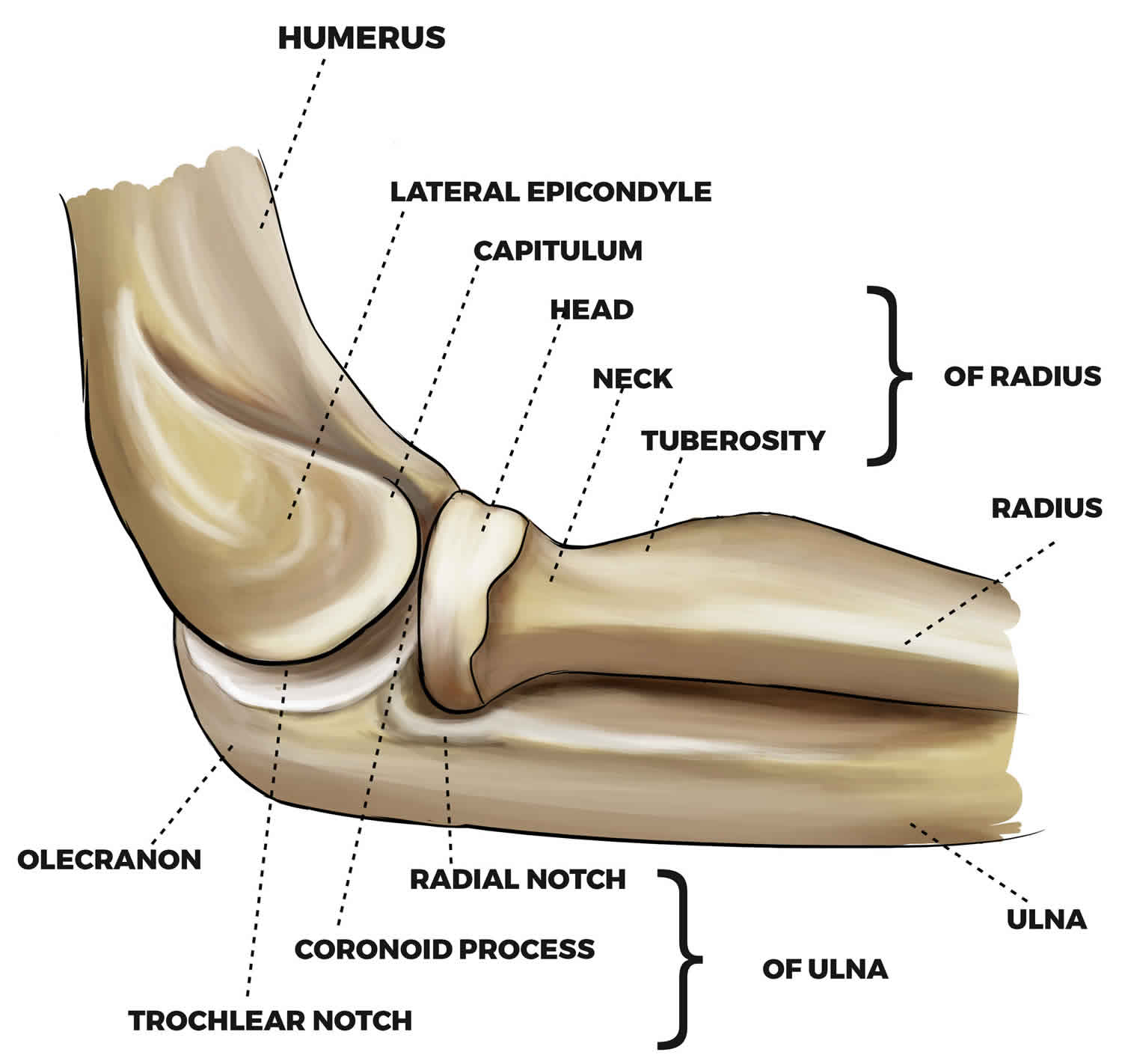
Elbow joint anatomy
The elbow is a joint made up of three bones—the humerus, radius, and ulna.
- The humerus is the upper arm bone between the shoulder and the elbow.
- The radius is one of the forearm bones between the elbow and wrist. The radius is on the “thumb side” of the forearm.
- The ulna is the other forearm bone between the elbow and wrist, running next to the radius. The ulna is on the “pinky finger side” of the forearm.
Ligaments on the inner and outer sides of the elbow hold the joint together and muscles surround the joint on the front and back sides. The elbow joint is crossed by three major nerves.
The annular and radial collateral ligaments stabilize the radial head. These ligaments stretch or rupture during radial head dislocation 3. The radial head articulates with the humeral capitellum and the radial notch of the proximal ulna. The radius and ulna are closely invested by the interosseous membrane, which accounts for the increased risk of displacement or injury to the radius when the ulna fractures.
The distal ulna and radius also articulate at the distal radioulnar joint 4. The ulna provides a stable platform for rotation of the radius and forearm. The ulna and interosseous membrane also may provide stable platforms for dislocation of the proximal radius, leading to the Monteggia fracture.
The posterior interosseous nerve travels around the neck of the radius and dives under the supinator as it courses into the forearm. The median and ulnar nerves enter the antecubital fossa just distal to the elbow. The close proximity of these nerves may lead to injuries when a radial head fracture occurs. Neural injuries are generally traction injuries and result from stretching around the displaced bone or from energy dispersed during the initial injury.
Biomechanics
A 180-degree arch in the pronation and supination is allowed by the articulation of the proximal end of the radius with the distal humerus (capitulum), and with the ulna in the lesser sigmoid cup (trochoid joint). Cartilage covers the radial head except for the anterolateral third that lacks subchondral bone, and it is easily fractured. It has a 40-degree central cavity, and it is oval-size-like. The head and neck are not collinear with the diaphysis and complete a 15-degree offset angle. They are closely related to the lateral ligament complex, mainly the annular ligament and radial collateral ligament 5.
The physiologic elbow range of movement is zero to 150 degrees of flexion and extension, and 85 degrees of pronation and 75 degrees of supination 6.
The radial head stabilizes in valgus when the internal ligament complex is injured, and it does not take part when being harmless (secondary stabilizer). Moreover, it is involved in the longitudinal stability 7.
Figure 2. Elbow joint bones
Figure 3. Elbow joint
Radial head fracture classification
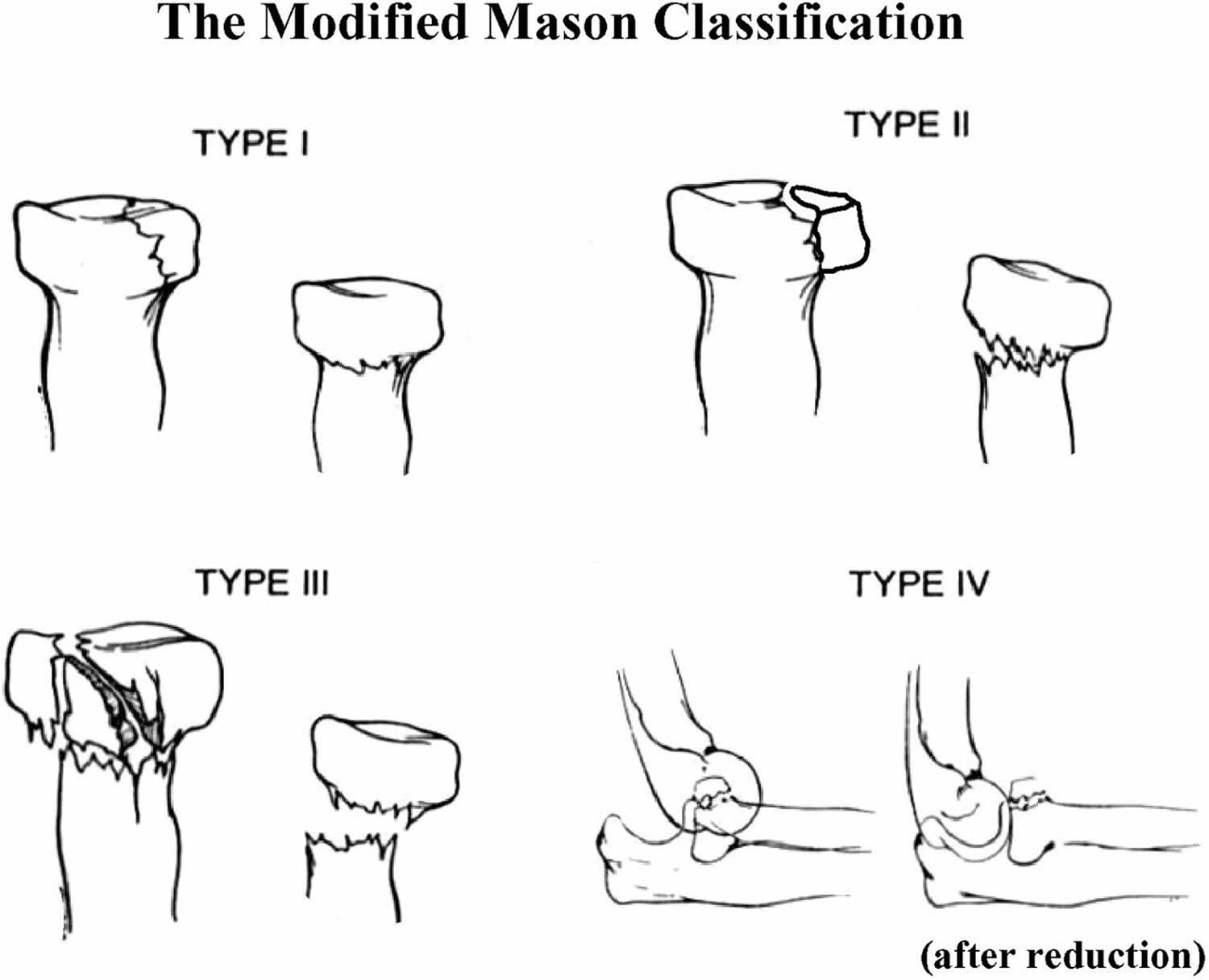
The Mason classification is used to classify radial head fractures and is useful when assessing further treatment options 8.
- Type I: non-displaced radial head fractures <2mm (or small marginal fractures), also known as a “chisel” fracture
- Type II: partial articular fractures with displacement (>2 mm)
- Type III: comminuted fractures involving the entire radial head
- IIIa: fracture of the entire radial neck, with the head, completely displaced from the shaft
- IIIb: articular fracture involving the entire head, consisting of more than two large fragments
- IIIc: fracture with a tilted and impacted articular segment
- Type IV: fracture of the radial head with dislocation of the elbow joint
In general type I injuries can be treated conservatively whereas type II injuries require open reduction and internal fixation (ORIF). Type III injuries often require early complete excision of the radial head 1.
Figure 4. Radial head fracture classification (Mason classification)
Radial head fracture causes
Radial head fractures usually occur as a result of indirect trauma, with most resulting from a fall on an abducted arm with minimal or moderate flexion of the elbow joint (0-80 degrees) 1. This results in valgus pronation stress with the radial head forcibly pushed against the capitulum of the humerus 9. In practice, the history is often, a fall onto an outstretched arm. A direct blow to the elbow can also cause a radial head fracture but is uncommon.
Radial head fracture symptoms
The most common symptoms of a radial head fracture include:
- Pain on the outside of the elbow
- Swelling in the elbow joint
- Difficulty in bending or straightening the elbow accompanied by pain
- Inability or difficulty in turning the forearm (palm up to palm down or vice versa)
A patient with radial head fracture-dislocations usually presents with a history of a fall on the outstretched hand. Blunt or penetrating trauma rarely causes radial head injury. The wrist, especially the distal radioulnar joint, may be damaged simultaneously, and the presence of wrist pain, grinding, or swelling should be determined.
The presence of bleeding, even with small puncture wounds, should alert the examiner to the possibility of open injury. Neurovascular symptoms of numbness, tingling, or loss of sensation should be identified to rule out nerve or vascular injury. The presence of severe pain should alert the examiner to the possibility of compartment syndrome.
Radial head fracture diagnosis
Patients with radial head fractures and dislocations present with localized swelling, tenderness, and decreased motion. The physician must carefully examine any wounds to make sure that no open fractures are present. Evaluating wounds over the subcutaneous border of the ulna is especially important in fracture-dislocations for ensuring that open fractures are not missed. The examiner should palpate the elbow, especially the radial head, feeling for deformity, and should also examine the wrist, especially feeling for stability of the distal radioulnar joint.
Because all three major nerves of the forearm are in danger with elbow fractures and dislocations, the examiner should also carefully assess neurovascular function for all of the nerves of the forearm and hand. Radial nerve function is especially important to assess with displaced fractures through the neck of the radius. The motor (posterior interosseous) branch provides extension for the fingers and wrist.
The examiner must also assess the firmness of all compartments, check for pain with passive stretch, and measure compartment pressures if in doubt to avoid missing compartment syndromes. Elbow stability needs to be assessed even with seemingly nondisplaced radial neck fractures. The elbow is tested with valgus stress at 30° of flexion to determine the competency of the medial collateral ligament.
Imaging studies
Most radial head injuries can be assessed adequately with standard plain radiography of the elbow. Normal radiographic examination findings demonstrate that the radial head is aligned with the capitellum on all views. A dislocation of the radial head can be easily missed if all radiographs are not carefully examined for this relation. For the normal elbow, a line drawn through the radial head and shaft should always line up with the capitellum, and with a supinated lateral view, lines drawn tangential to the head anteriorly and posteriorly should enclose the capitellum.
With a radial head dislocation, these radiographic findings are disrupted. The images below are examples of an injury that appears to be a simple ulna fracture when only the anteroposterior (AP) view is evaluated but that clearly has a dislocated radial head on the lateral view. As with any fracture assessment, two views perpendicular to each other are always required.
In rare circumstances, computed tomography (CT) of the elbow is useful to define fracture patterns.
Figure 5. Radial head fracture (Type 1)
Footnote: There is a mildly displaced intra-articular fracture of the radial head, with a ~2mm articular step-off. Joint effusion noted.
Radial head fracture treatment
Doctors classify fractures according to the degree of displacement (how far out of normal position the bones are) (see Figure 4). Treatment is determined by the type of fracture, according to the classification below.
Type I Fractures
Type I fractures are generally small, like cracks, and the bone pieces remain fitted together.
- The fracture may not be visible on initial x-rays, but can usually be seen if the x-ray is taken 3 weeks after the injury.
- Nonsurgical treatment involves using a splint or sling for a few days, followed by an early and gradual increase in elbow and wrist movement (depending on the level of pain).
- If too much motion is attempted too quickly, the bones may shift and become displaced.
Type II Fractures
Type II fractures are slightly displaced and involve a larger piece of bone.
- If displacement is minimal, a sling or splint may be used for 1 to 2 weeks, followed by range-of-motion exercises.
- Small fragments of broken bone may be surgically removed if they prevent normal elbow movement or could cause long-term problems with the elbow.
- If a fragment is large and out of place enough, the orthopaedic surgeon will first attempt to hold the bones together with screws, or a plate and screws. If this is not possible, the surgeon will remove the broken pieces of the radial head.
- The surgeon will also correct any other soft-tissue injury, such as a torn ligament.
Type III Fractures
Type III fractures have multiple broken pieces of bone which cannot be put back together for healing.
- In most Type III radial head fractures, there is also significant damage to the elbow joint and the ligaments that surround the elbow.
- Surgery is always required to either fix or remove the broken pieces of bone and repair the soft-tissue damage. If the damage is severe, the entire radial head may need to be removed. In some cases, an artificial radial head may be placed to improve long-term function.
- Early movement to stretch and bend the elbow is necessary to avoid stiffness.
Even the simplest of fractures may result in some loss of movement in the elbow. Regardless of the type of fracture or the treatment used, exercises to restore movement and strength will be needed before resuming full activities.
Patients whose medical condition is too unstable to allow safe surgery when surgery would otherwise be indicated can also be treated with splinting followed by early motion, but the prognosis is guarded for achieving optimal function.
Joint aspiration to relieve pressure has been employed as an initial treatment measure, but its efficacy is unclear 10.
Indications for surgery
Surgical treatment is indicated for all unstable radial head (and neck) fractures and dislocations. As described above, the rule of threes can be used for determining the need for surgical intervention: Surgery is required if the fracture involves more than 33% of the articular surface, is angulated more than 30°, or is displaced more than 3 mm. A mechanical block to motion always requires open treatment to remove the blocking bone or osteochondral fragment or fragments.
Open fractures are also surgical emergencies. They require surgical irrigation and debridement in an operating room with appropriate antibiotics even if the wound is small. At the same time, immediate stabilization of the bone injury is also performed.
Surgical treatment
- Radial head excision: Indication in severe pain in selected cases for instance older adults with a low demand with complex fractures but no associated fractures which compromise stability. One option is the differed excision with the same indication to the mentioned one or to enhance pronation-supination 7.
- Open or arthroscopic: Fragment excision may be indicated in cases where these can obstruct joints and are too small for osteosynthesis and should not be part of the proximal radio-ulnar joint.
- Osteosynthesis: As regards isolated fractures, it is an absolute indication when they cause a joint blockage. (Mason type 2) Step over 2 mm, joint fragment over 30%, neck fractures with angling over 30 degrees 11.
- Arthroplasty: Indication for non-repairable fractures. A prosthesis-sized appropriate choice is important to avoid articular stiffness 12.
Low profile plates and screws implants or cannulated are applied.
Kocher surgical approach between the anconeus and extensor carpi ulnaris, it provides good access to the back fragments and safety to the posterior interosseous nerve. Another option is extensor digitorium comunis splinting to avoid iatrogenic injuries.
Osteosynthesis should be placed in the safe interval to avoid interference with the proximal radio-ulnar joint which is located 110 external degrees with the elbow in neutral pronation-supination.
In complex fractures, osteosynthesis or prosthesis? It is convenient not to get more than three fragments with no impaction or deformity with enough bone quality and without metaphyseal bone loss to achieve a stable internal fixation. In many cases, these fracture features are determined at surgery time.
Long-term monitoring
Rehabilitation with range-of-motion exercises is begun as soon as the wound is healed, depending on the type of fracture and stability of fixation. The typical time to union is 6-8 weeks. Casting with the elbow in 90° of flexion is rarely needed to maintain the radial head reduction, but if the radial head is unstable, the surgeon needs to search for other causes, such as interposed annular ligament or osteochondral fragment or poorly reduced fracture.
Radial head fracture complications
Early complications of radial head or neck fractures or dislocations include the following:
- Compartment syndrome
- Neurovascular injury
- Infection
Late complications include the following:
- Nonunion
- Hardware failure
- Malunion
- Infection
- Synostosis
- Persistent pain
Compartment syndrome after isolated radial head fracture is unlikely but could occur with Monteggia fractures, floating elbow injuries, and associated crush injuries to the forearm. Compartment syndromes usually occur in high-energy trauma but can occur with prolonged low-energy injuries and gunshot injuries. Predisposing factors include vascular injury, coagulopathy, and limb compression. Prevent iatrogenic compartment syndrome during surgery by obtaining good hemostasis and by not closing the fascia at surgery.
Early diagnosis is necessary. The treating physician needs to have a high index of suspicion, remembering the standard signs and symptoms of increased compartment pressure: pain on passive stretch, palpable firmness or tightness of the compartment, altered sensation or paresthesias, pain out of proportion to that expected, pallor, pulselessness, and less than 30 mm Hg difference between compartment pressure and diastolic pressure. All affected compartments should be released.
Stiffness due to prominent hardware in osteosynthesis or to the oversized prosthesis in arthroplasties. It can also be found due to capsular contracture and ossification. Avoiding the problem by early motion is preferable to trying to deal with it after contracture has already occurred.
Synostosis after radial head fracture or dislocation can be a disabling complication because it limits motion, especially rotation of the forearm. Risks include closed head injury, surgical delay longer than 2 weeks, and penetration of the interosseous membrane by bone graft or screws, bone fragments, or surgical instruments. Treatment by resection with an interposition spacer restores motion in about 50% of patients. Generally, the surgeon should wait at least a year or until the bone is metabolically inactive on bone scanning. Surgery should generally be completed before 3 years. The first image below shows an example of a patient who developed synostosis. The second image below shows the synostosis. The synostosis was resected, and an interposition fat spacer was used with early motion.
Aseptic necrosis and nonunion after osteosynthesis failure. Treatment of nonunion requires restoration of normal biomechanics with stable internal fixation or radial head excision or replacement, depending on the fracture and wrist and elbow stability.
Malunion is less frequent post osteosynthesis than in nonsurgical treatment. Arthritis according to clinical x-ray studies but with no clinical correlation.
Instability is less frequent. It is important to manage injuries to avoid this complication adequately.
Aseptic necrosis and nonunion after osteosynthesis failure. Malunion is less frequent post osteosynthesis than in nonsurgical treatment.
Arthritis according to clinical x-ray studies but with no clinical correlation.
Infection after radial head fracture can occur either early or late. Treatment requires irrigation and debridement and appropriate antibiotics (usually administered intravenously). If the fracture is healed or the hardware is loose, the hardware should be removed. If the fracture has not healed and the hardware is stable, the hardware is maintained.
Persistent pain after radial head fracture may be due to the hardware, intra-articular cartilage injury and posttraumatic arthritis, adhesions, malalignment, or associated nerve or muscle injuries. Hardware removal may be helpful, but potential complications, including iatrogenic nerve injury when dissecting through scar, may outweigh the benefits. Persistent pain may be due to nonunion. The images below show a patient who had persistent painful clicking after his radial head fixation, which resolved after hardware removal.
Radial head fracture prognosis
For radial head and neck fractures and dislocations, the prognosis is generally good when the following are achieved 13:
- Mechanical stability with anatomic reduction and stable internal fixation
- Optimal biology of healing with anatomic reduction, indirect techniques, and maintenance of soft-tissue attachments
A study by Duckworth et al 14 reported excellent long-term results with nonoperative management of isolated stable fractures of the radial head or neck.
- Mirzayan R, Itamura JM. Shoulder and Elbow Trauma. Thieme Medical Pub. (2004) ISBN:1588902196.[↩][↩][↩][↩][↩]
- Pappas N, Bernstein J. Fractures in brief: radial head fractures. Clinical orthopaedics and related research. 468 (3): 914-6. doi:10.1007/s11999-009-1183-1[↩]
- Tan JW, Mu MZ, Liao GJ, Li JM. Pathology of the annular ligament in paediatric Monteggia fractures. Injury. 2008 Apr. 39 (4):451-5.[↩]
- Guitton TG, Ring D, Kloen P. Long-term evaluation of surgically treated anterior monteggia fractures in skeletally mature patients. J Hand Surg Am. 2009 Nov. 34 (9):1618-24.[↩]
- Rausch V, Wegmann S, Hackl M, Leschinger T, Neiss WF, Scaal M, Müller LP, Wegmann K. The radial head size in relation to osseous landmarks of the forearm. Surg Radiol Anat. 2019 Apr;41(4):415-421.[↩]
- Keijsers R, Zwerus EL, van Lith DRM, Koenraadt KLM, Goossens P, The B, van den Bekerom MPJ, Eygendaal D. Validity and Reliability of Elbow Range of Motion Measurements Using Digital Photographs, Movies, and a Goniometry Smartphone Application. J Sports Med (Hindawi Publ Corp). 2018;2018:7906875[↩]
- Mazhar FN, Ebrahimi H, Jafari D, Mirzaei A. Radial head resection versus prosthetic arthroplasty in terrible triad injury: a retrospective comparative cohort study: a retrospective comparative cohort study. Bone Joint J. 2018 Nov;100-B(11):1499-1505.[↩][↩]
- Bhandari M. Evidence-Based Orthopedics. Wiley-Blackwell. (2012) ISBN:1405184760.[↩]
- John SD, Wherry K, Swischuk LE et-al. Improving detection of pediatric elbow fractures by understanding their mechanics. Radiographics. 1996;16 (6): 1443-60.[↩]
- Foocharoen T, Foocharoen C, Laopaiboon M, Tiamklang T. Aspiration of the elbow joint for treating radial head fractures. Cochrane Database Syst Rev. 2014 Nov 22. 11:CD009949[↩]
- Ballesteros-Betancourt JR, Lázaro-Amorós A, García-Tarriño R, Sastre-Solsona S, Combalia-Aleu A, Llusá-Pérez M. Classification of the transverse pattern of Mason II radial head fractures and its usefulness in arthroscopic osteosynthesis. Anatomo-surgical study. Rev Esp Cir Ortop Traumatol. 2019 Jan – Feb;63(1):12-19.[↩]
- Sershon RA, Luchetti TJ, Cohen MS, Wysocki RW. Radial head replacement with a bipolar system: an average 10-year follow-up. J Shoulder Elbow Surg. 2018 Feb;27(2):e38-e44.[↩]
- O’Driscoll SW, Jupiter JB, Cohen MS, et al. Difficult elbow fractures: pearls and pitfalls. Instr Course Lect. 2003. 52:113-34.[↩]
- Duckworth AD, Wickramasinghe NR, Clement ND, Court-Brown CM, McQueen MM. Long-term outcomes of isolated stable radial head fractures. J Bone Joint Surg Am. 2014 Oct 15. 96 (20):1716-23.[↩]