Reticulocytosis
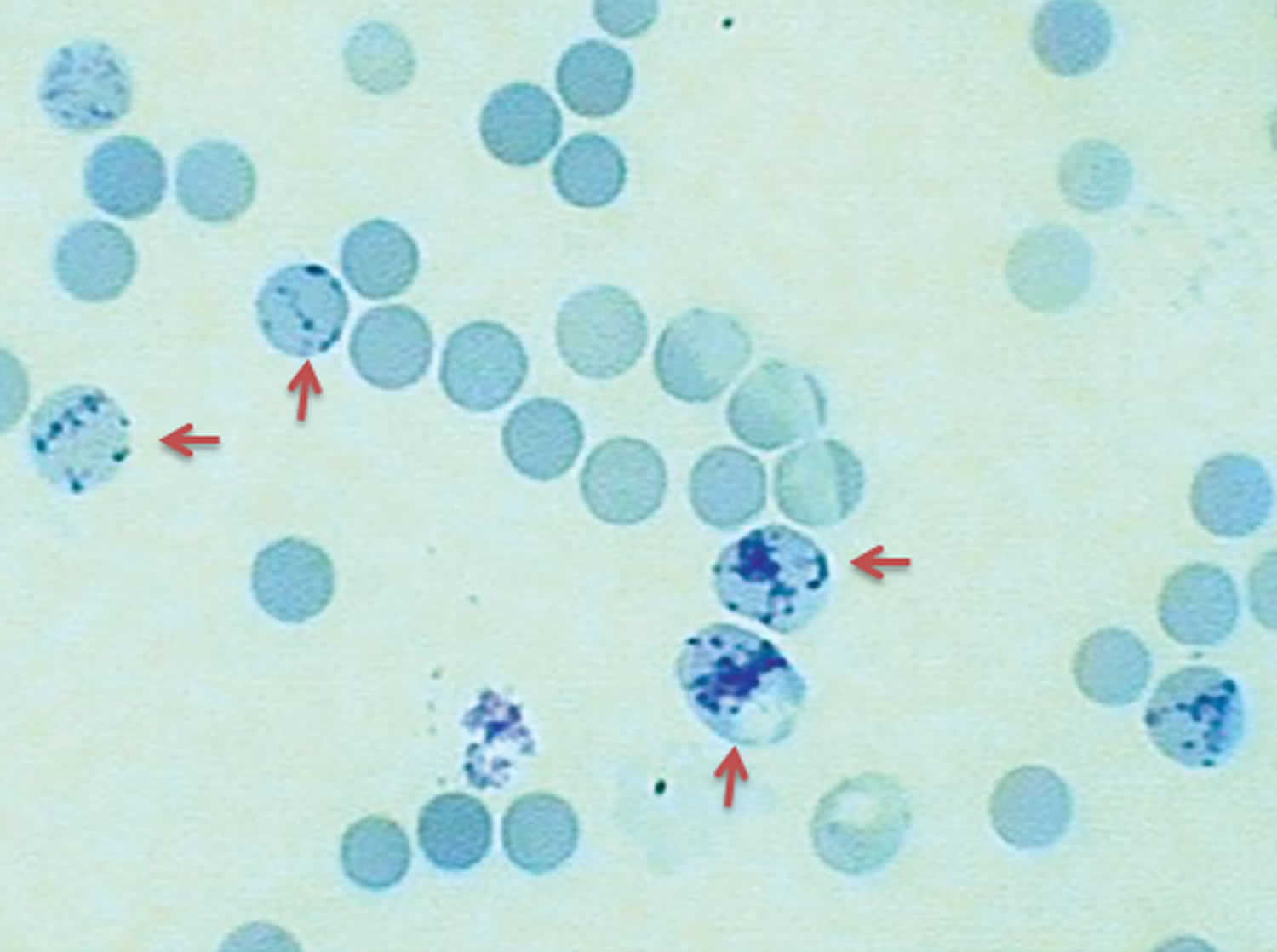
Reticulocytosis is a condition where there is an increase in reticulocytes, which are immature red blood cells that contain ribosomal RNA 1. Reticulocytes are immature red blood cells produced in the bone marrow and released into the peripheral blood where they mature into red blood cells within 1 to 2 days 2. During this time, the reticulocyte undergoes many changes to become a mature functioning red blood cell. An increase in erythropoietin (EPO) levels stimulates the bone marrow to increase reticulocyte production. EPO (erythropoietin) levels normally elevate for 3 to 4 days before an increase in the reticulocyte count presents 3. An increase or decrease in reticulocyte count can be an indicator of erythropoiesis activity or failure of, especially relative to anemias particularly congenital hemolytic anemia and bone marrow dysfunction 3.
Reticulocytes are as a useful clinical indicator of anemias and bone marrow response to anemia. Reticulocyte count in a healthy person should be between 0.5 to 2.5% 4. When a patient is anemic, and the bone marrow is unable to respond, reticulocyte count will be low. When the bone marrow can respond appropriately, the reticulocyte count will increase 3.
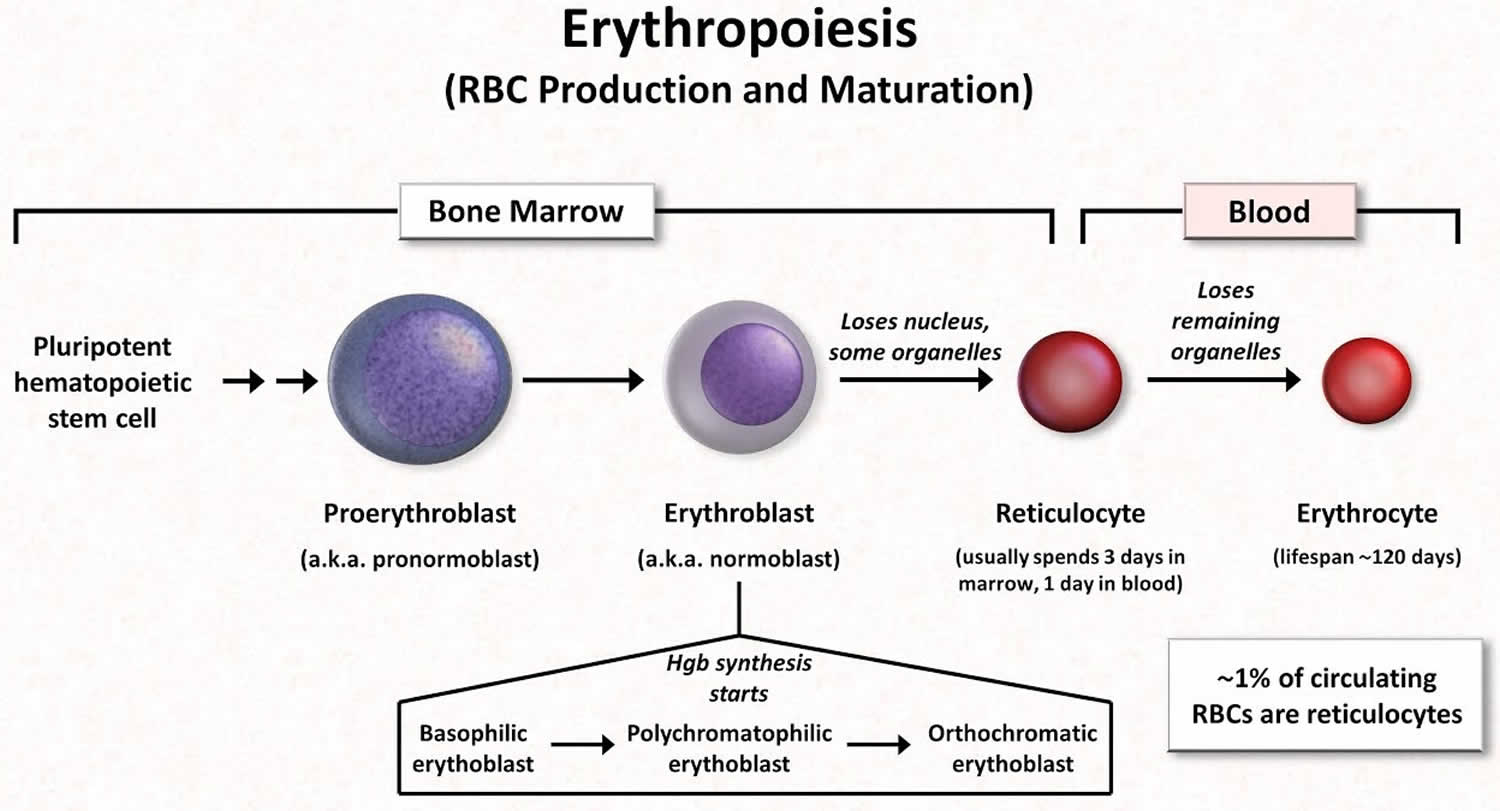
Figure 1. Red blood cell production and maturation
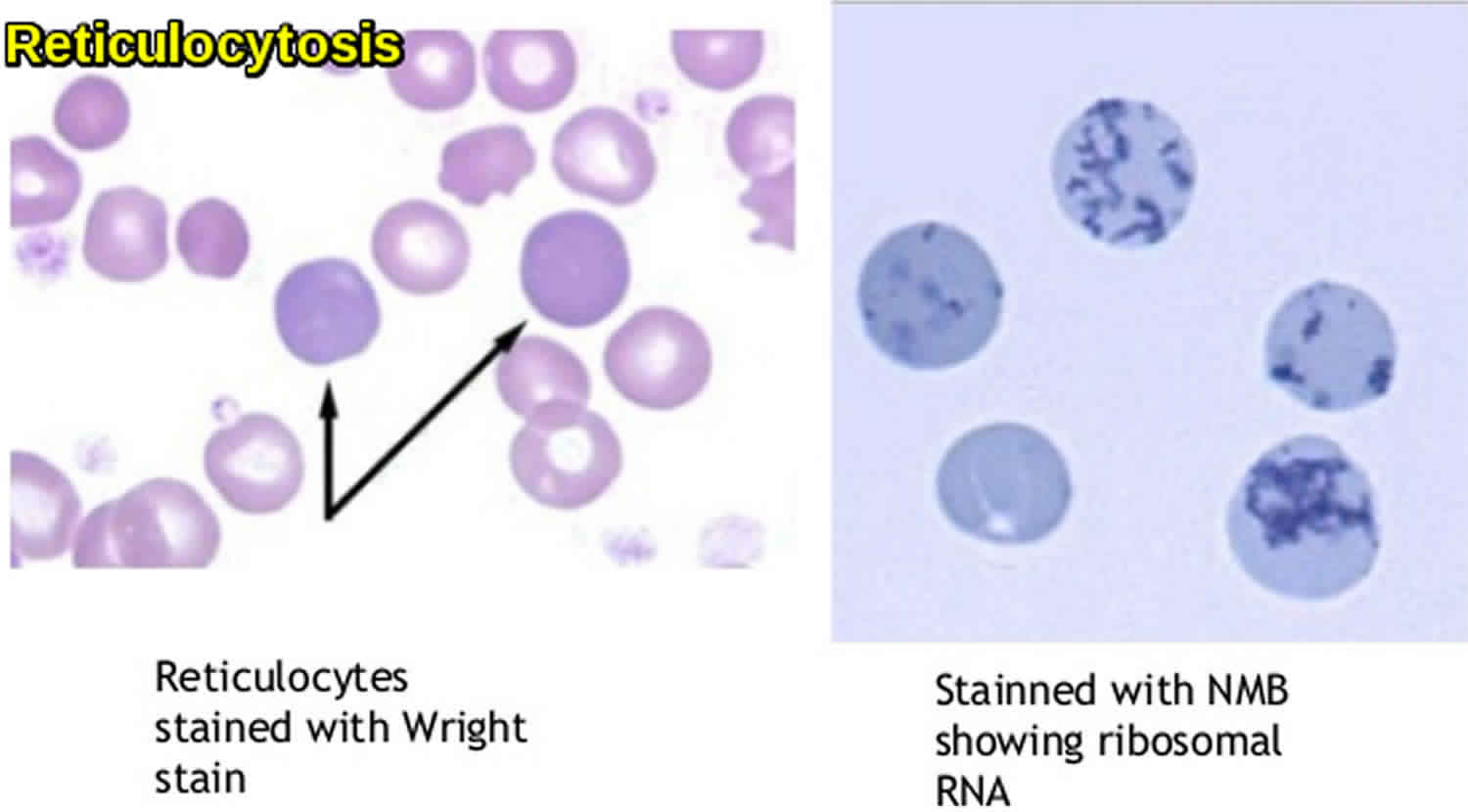
Figure 2. Reticulocytes
Reticulocytosis causes
Common causes of increased reticulocyte count or reticulocytosis include 5:
- Hemolytic anemias: These anemias are a result of red blood cell destruction. The bone marrow is still functional and has the required components to create reticulocytes. It responds to the anemia by increasing the synthesis of reticulocytes.
- Immune hemolytic anemia
- Primary red blood cell membrane defects
- Sickle cell diseases
- Enzyme defects
- Exposure to toxins
- Blood loss or hemorrhage: An acute or chronic blood loss will cause an increase in erythropoiesis.
Other causes of reticulocytosis:
- Microangiopathic anemia
- Post-splenectomy
- Hemoglobinopathy
- Following treatment of anemias
- Physiologic increase in pregnancy and infants.
Reticulocytosis diagnosis
Reticulocyte analysis, mainly immature reticulocyte fraction, has also been used in chemotherapy patients with leukemia to determine the regenerative activity of the bone marrow during and after treatment. This same idea applies to bone marrow transplant patients 4.
Another clinical use of reticulocyte count is in patients taking hydroxyurea for sickle cell anemia. This medication impairs bone marrow production of reticulocytes, therefore, causing a decrease in the count. For this reason, frequent reticulocyte counts are necessary while on this medication 6.
In end-stage renal disease patients receiving erythropoietin (EPO) therapy, the reticulocyte count has been used as a parameter to measure the response to therapy 3
Other values apart from reticulocyte count that can be calculated to assess function:
- Reticulocyte production index = Reticulocyte count% x [Patient hematocrit/0.45]
- This is a corrected reticulocyte count used in anemias. In anemias, a falsely elevated reticulocyte count can occur. A decrease in red blood cells automatically increases the reticulocyte count even if erythropoiesis has not taken place because the count represents a percentage in comparison to red blood cells. It is possible the appropriate increase of erythropoiesis has not taken place in response to the anemia. This value, therefore, corrects for this issue 7.
- A more accurate method to correct for the effect of anemia is to calculate the absolute number of reticulocytes:
- Absolute reticulocyte count =Reticulocyte count (%) × red blood cell (RBC/mm³)
- The absolute reticulocyte count is normally between 50,000 and 150,000 reticulocytes/mL (5 × 1010 and 1.5 × 1012 reticulocytes/L).
- Immature reticulocyte fraction (IRF): This is a value of the immature reticulocytes measured as a ratio of immature reticulocytes to the total amount of reticulocytes 8.
- Reticulocyte hemoglobin content (Chr): This is a useful indirect measure of iron deficiency anemia. It measures the amount of the iron available in the bone marrow that can be used by the reticulocyte for the production of hemoglobin. Multiple studies have shown a reticulocyte hemoglobin content of less than 28 pg is a good predictor for iron deficiency anemia 9.
Reticulocytosis treatment
Reticulocytosis treatment involves treating the underlying cause.
- Rai D, Wilson AM, Moosavi L. Histology, Reticulocytes. [Updated 2019 Jun 14]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2020 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK542172[↩]
- Mast AE, Blinder MA, Dietzen DJ. Reticulocyte hemoglobin content. Am. J. Hematol. 2008 Apr;83(4):307-10.[↩]
- Riley RS, Ben-Ezra JM, Goel R, Tidwell A. Reticulocytes and reticulocyte enumeration. J. Clin. Lab. Anal. 2001;15(5):267-94.[↩][↩][↩][↩]
- Raja-Sabudin RZ, Othman A, Ahmed-Mohamed KA, Ithnin A, Alauddin H, Alias H, Abdul-Latif Z, Das S, Abdul-Wahid FS, Hussin NH. Immature reticulocyte fraction is an early predictor of bone marrow recovery post chemotherapy in patients with acute leukemia. Saudi Med J. 2014 Apr;35(4):346-9.[↩][↩]
- Riley RS, Ben-Ezra JM, Goel R, Tidwell A. Reticulocytes and reticulocyte enumeration. J Clin Lab Anal. 2001;15(5):267–294. doi:10.1002/jcla.1039 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6808174/pdf/JCLA-15-267.pdf[↩]
- Agrawal RK, Patel RK, Shah V, Nainiwal L, Trivedi B. Hydroxyurea in sickle cell disease: drug review. Indian J Hematol Blood Transfus. 2014 Jun;30(2):91-6.[↩]
- Piva E, Brugnara C, Spolaore F, Plebani M. Clinical utility of reticulocyte parameters. Clin. Lab. Med. 2015 Mar;35(1):133-63.[↩]
- Chang CC, Kass L. Clinical significance of immature reticulocyte fraction determined by automated reticulocyte counting. Am. J. Clin. Pathol. 1997 Jul;108(1):69-73.[↩]
- Karagülle M, Gündüz E, Sahin Mutlu F, Olga Akay M. Clinical significance of reticulocyte hemoglobin content in the diagnosis of iron deficiency anemia. Turk J Haematol. 2013 Jun;30(2):153-6.[↩]