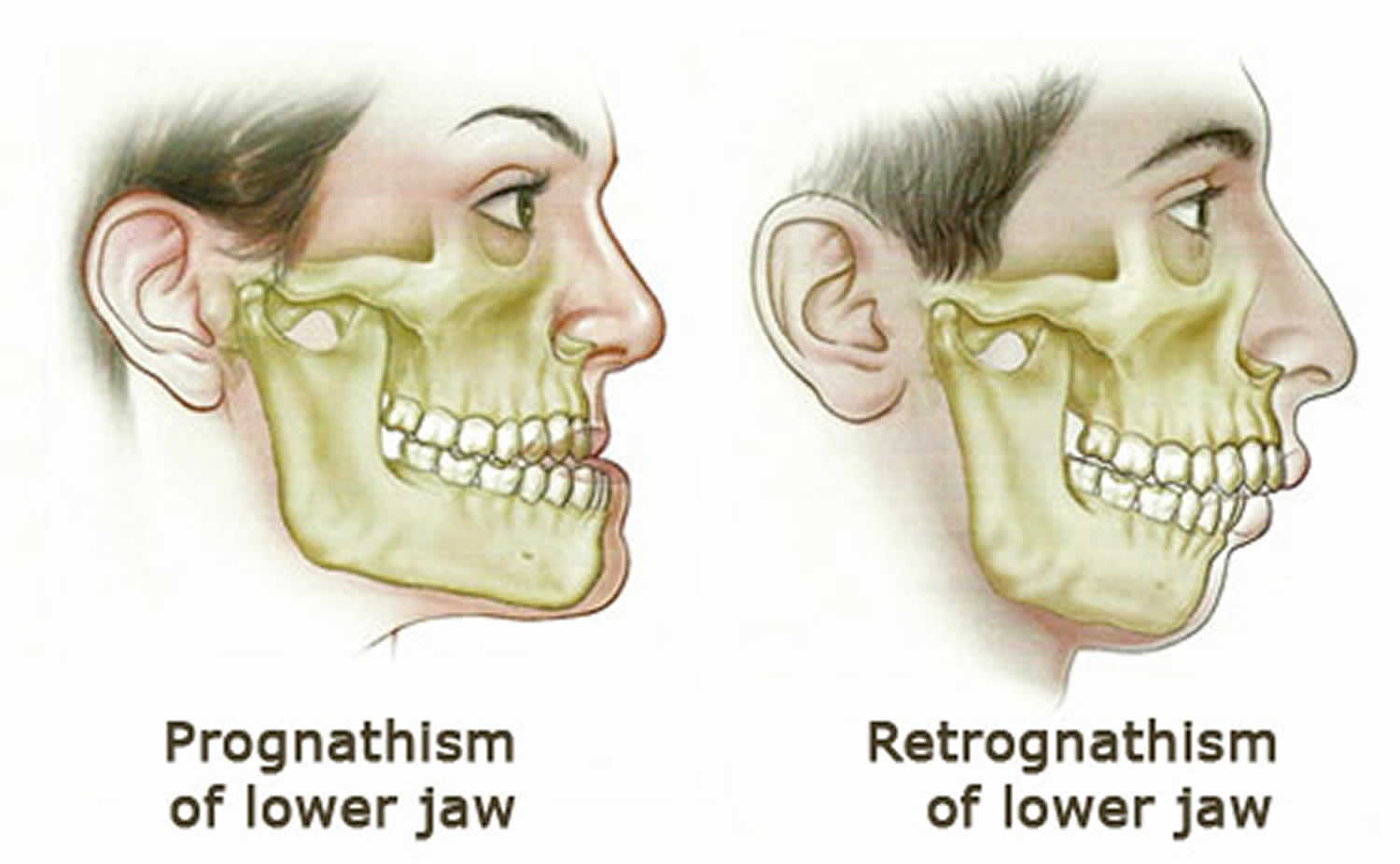
Retrognathism
Retrognathism also called retrognathia, is a type of malocclusion which refers to an abnormal posterior positioning of the maxilla or mandible 1, particularly the mandible, relative to the facial skeleton and soft tissues 2. Retrognathia, from the Latin retro, “backward” and from the Greek, gnathos, jaw, is a dentofacial deformity in which both the upper and lower jaws are misaligned with each other causing an anteroposterior discrepancy between the upper jaw and the mandible (lower jaw): the first lower molar is posterior (or more towards the back of the mouth) than the first upper molar, which makes it appear that a person has a severe overbite. Often, this difference in the location between the lower and upper jaw is not noticeable in front, but it is very noticeable in the patient’s side profile. That is, when viewed from the side, the mandible is posterior to and behind where it should be.
To the specialists (otolaryngologists, oral and maxillofacial surgeons, dentists and dental specialists, like orthodontists), describing a patient as retrognathic specifically means the patient is deficient in the anterior-posterior (AP) plane of growth 3. There is often a vertical component in growth deficiency and sometimes a transverse issue, but they are less critical in thinking about retrognathia unless one is planning a surgical correction. To summarize, when dental professionals describe a patient as retrognathic, it implies the mandible is deficient in growth, particularly in the anterior-posterior plane.
Retrognathia creates a posterior displacement of the tongue base, which further narrows the upper airway and is associated with a high-arched (ogival) palate due to tongue position 4.
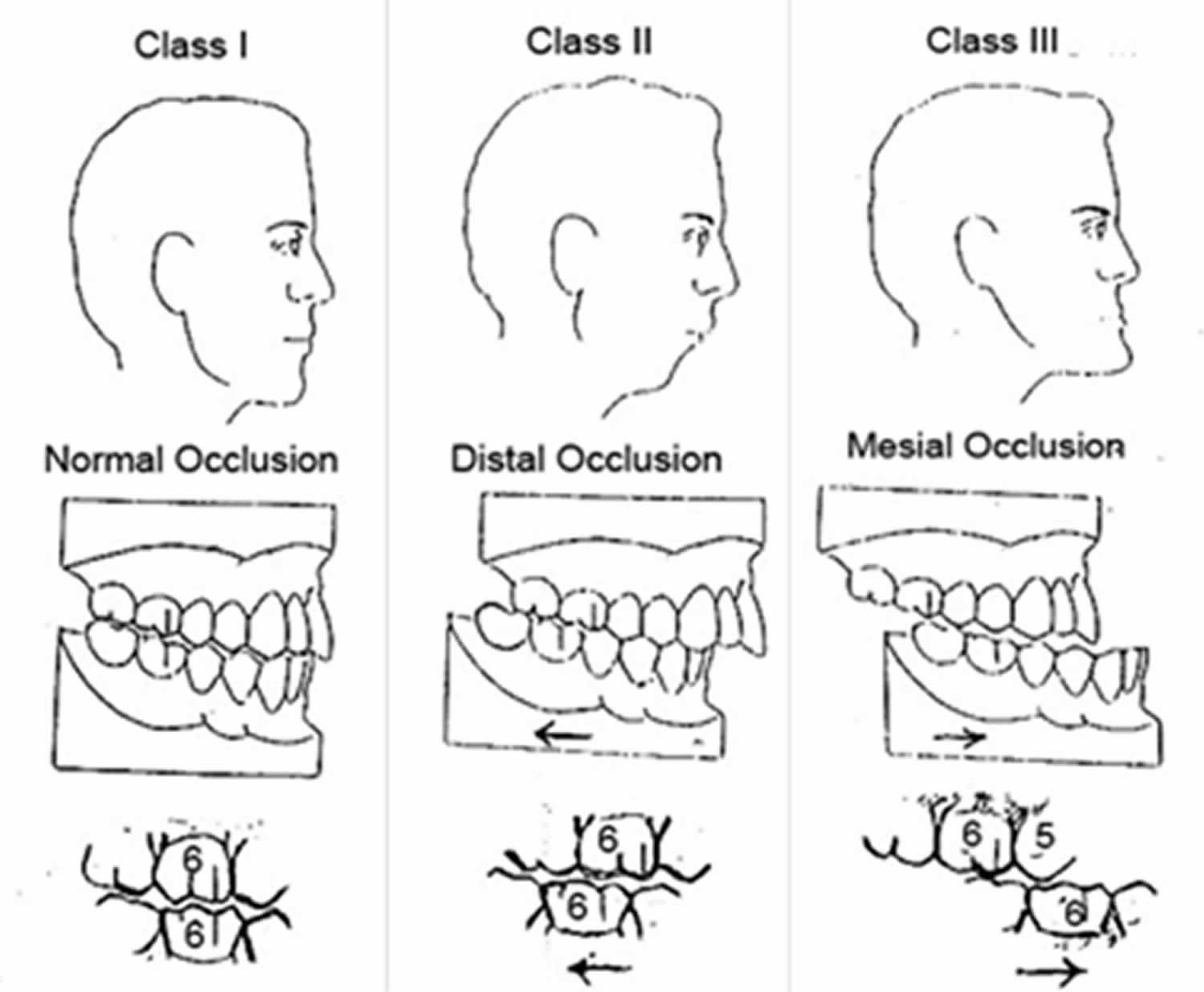
Dr. Edward Angle, widely known as the father of orthodontics, created a classification system for the occlusion of teeth and how they relate to each other (see Figure 1). It is based on the relationship between certain parts of the first molars and canines:
- Class 1 occlusion means there is an appropriate relationship between the maxillary teeth and mandibular teeth.
- Class 2 means that the mandibular teeth are posterior as in patients with retrognathia.
- Class 3 indicates that the mandibular teeth are anterior to the where they should be (think of a bulldog with the lower jaw sticking out).
In dental terminology, mandibular retrognathia is also called Class 2 occlusion. A skeletal Class 2 malocclusion may be the result of:
- A prognatic or overdeveloped upper jaw
- A retrognathic or underdeveloped jaw
- And / or the combination of both.
However, you must keep in mind that your teeth can hide this as your bodies will often dentally compensate for skeletal discrepancies 5.
Often just looking at the patient extraorally can help your dentist can determine if they are retrognathic. When viewed from the side, you will notice an exaggerated convex facial profile. On grown adults, as part of a standard airway examination, examining the thyromental distance can be a predictor of a difficult airway. This implies retrognathia if the patient has a mandible that has not developed, the thyromental distance will be less than the standard three finger’s breadth, or approximately 7 mm 6.
Some people with retrognathism have trouble breathing, especially when they sleep, since their airways are narrower than normal, which can cause snoring, or even obstructive sleep apnea (OSA), a syndrome that affects a little more of 25% of the population, and causes a person to stop breathing several times a night, often without realizing that this is happening. Retrognathism affects not only their night rest, but also their daily activity, as they feel often drowsy and fatigued. In extreme cases retrognathia can even lead to death.
Radiology plays a significant role in determining retrognathia. The standard lateral cephalometric radiograph and associated analysis are part of the determination. There are hundreds of different interpretations and, suffice to say, that there are many points and combinations of angles that measure the relationship between the cranial vault and the facial skeleton to determine growth and are used in treatment planning for orthodontics and orthognathic surgery 7.
The most common diagnosis in the practice of orthodontics and oral and maxillofacial surgery associated with retrognathia is mandibular anterior-posterior hypoplasia, a common diagnosis that supports a surgical correction of their deficiency, most commonly through a bilateral sagittal split osteotomy of the mandible 8.
Depending on the patient age and especially with infants and children, an astute practitioner must keep in mind some associated syndromes and conditions that are often associated with a hypoplastic mandible. This includes Pierre-Robin Sequence, Hemifacial Microsomia, DiGeorge syndrome, Nager syndrome, Treacher Collins, Goldenhar syndrome, and Mobius syndrome.
Prior surgery to the head and neck or history of trauma can also produce retrognathia. For example, a male in his twenties with a history of a fall off his bicycle in the second grade. This caused trauma to one of his condyles and a unilateral aplasia in that location, resulting in a crooked face and retrognathic appearance, warranting surgical correction. Because of the condylar portion of the growth of the mandible, temporomandibular trauma can restrict growth. Any blow to the chin or lower face, if severe enough, can cause this type of growth pattern and result in retrognathia and is worth asking about during a history.
Depending on the causes of retrognathia, treatment may include orthodontic braces, conventional orthodontics and / or surgical intervention. It is essential to differentiate the dominant causal factor from skeletal Class 2 malocclusion, since the orthopedic / orthognathic surgical treatment plan varies accordingly. In mild cases, no treatment is needed.
Figure 1. Angle’s classification of malocclusion
Why does retrognathia matter as a diagnosis?
First, to rule out associated syndromes with far-reaching health effects, to recognize and be able to appropriately refer for orthodontic evaluation with possible need for surgery surgical correction, to consider if you are a health care professional who would ever deal with or manage an airway, and to consider the implications in the setting of obstructive sleep apnea (OSA).
Mandibular retrognathism causes
If the infant or child presents with retrognathia, or even if they are older and have associated findings that lead you to suspect a syndrome or myriad of issues, consider the following conditions:
- Pierre-Robin Sequence: The classic triad of micrognathia (colloquially synonymous with retrognathia), glossoptosis, and cleft palate. Airway obstruction is likely, though the disease can present with a range from mild to severe. The patient will need a referral to a cleft and craniofacial team for evaluation and treatment 9.
- Hemifacial Microsomia: Part of the spectrum of Oculo-Auriculo-Vertebral Syndromes, this is another entity with variable penetrance. It arises due to pathologic dysregulation of the first and second pharyngeal arches and can be unilateral or bilateral. It results in hypoplastic growth of not only the mandible and lower face but can affect the midface, temporomandibular joint, orbits, ears, and soft tissue. A common classification system used is the Kaban Classification (Types 1, 2a, 2b, and 3), which help guide surgical correction. If discovered as an infant, the patient will need a referral to a cleft and craniofacial team for evaluation and treatment. A surprisingly high number of adults have a mild expression which needs to be taken into close account during facial and orthognathic surgical planning 10.
- Goldenhar Syndrome: Part of the spectrum of Oculo-Auriculo-Vertebral Syndromes, the cause behind Goldenhar Syndrome is unclear, with multiple chromosomes potentially affected and only theories offered as to a cause. This entity combines features of Hemifacial Microsomia with further facial clefting, colobomas of the eyes, vertebral anomalies, and other findings. The patient will need a referral to a cleft and craniofacial team for evaluation and treatment as well as ophthalmology 11.
- Treacher Collins Syndrome: Treacher Collins syndrome is an autosomal dominant condition of a mutation of the TCOF1 gene with variable expression. Patients will have a unique facial appearance with extreme retrognathia leading to a very convex facial profile when viewed from the side, antimongoloid slanting eyes (that is the lateral corners of the eyes are turned down), colobomas, significant facial hypoplasia of the midface of the hard and soft tissues, and auricular deformities. Once born, these infants will need immediate and intense multidisciplinary therapy 12.
- Nager Syndrome: Similar to Treacher Collins. However, the cause is unknown. Similar therapies 13.
- Mobius Syndrome: A very rare entity with etiology unclear, this presents with a characteristic “masklike face” as a component is paralysis of some or all of cranial nerves III, IV, V, VI, VII, IX, X, and XII. Retrognathia, ocular deformities, and other skeletal and limb abnormalities. The patient will need a referral to a cleft and craniofacial team for evaluation and treatment, as well as any other specialties warranted 14.
In most cases, class 2 mandibular retrognathism are inherited genetically, and may be due to insufficient growth of the lower jaw, excessive growth of the upper jaw or a combination of both. According to some studies, the main contributing factor for class 2 skeletal malocclusion is mandibular retrognathism, followed by maxillary prognathism and with a small percentage of cases that combine both factors.
A class 2 malocclusion may also be aggravated by environmental factors such as finger sucking, allergies, poor respiratory function, atypical swallowing, or chronic mouth breathing. There may also be other factors for retrognathia, such as a retracted chin that lacks forward projection; or it may be due to a purely dental problem.
The mandible develops in the same area as the first pharyngeal arch and is associated with Meckel’s cartilage, though Meckel’s cartilage does not become the mandible 3. The mandible begins as a condensation of mesenchymal tissue lateral to Meckel’s cartilage and proceeds through development via intramembranous bone formation. At six weeks in utero, it starts to ossify. The condyle of the mandible, which articulates with the skull as part of the temporomandibular joint, develops as independent secondary cartilage, at approximately ten weeks, and undergoes endochondral ossification.
Simply put, the mandible grows down and forward, or anteriorly and inferiorly. It does this through a combination of processes. These include concurrent resorption of bone from the anterior surface of the ramus with apposition of bone along the posterior surface of the mandible. This process, in conjunction with growth at the condyle, creates the anterior and inferior vector of growth 15.
In growth and development, there are standard charts commonly used by health care professionals detailing the spectrum of height, weight, age, and growth. It is worth considering there can be significant variation between individuals and that there are both chronologic and biologic ages (considering menarche/puberty). In general, facial height is the last dimension to finish growth and in females will be complete around ages 17-18, and in males in the early twenties. In a retrognathic patient or patients who have hypoplastic mandibles, this growth can be done much earlier.
The timing of this growth and development is crucial when considering skeletal surgery to address retrognathia and is carefully ascertained for each patient 15.
Mandibular retrognathism symptoms
When there is retrognathia or abnormal relationship between the maxilla and the mandible, the disharmony between the two structures causes distinctive facial features on the patient’s face: the face lacks forward projection in its lower third and the upper front teeth and the upper jaw project more forward than the lower teeth and jaw, so there is a convex profile appearance, with a retracted chin and lower lip.
Retrognathia can be a difficult condition to handle. Physically, it can affect the patient’s masticatory and phonatory abilities, Whereas some people with the condition also see their self-esteem or level of confidence affected, since the condition is visually remarkable.
Someone with retrognathia may also develop temporomandibular joint disorder (TMJ), a condition that causes pain and muscle spasms.
Likewise, there are also long-term reasons: as a person with retrognathism ages, their teeth tend to misalign, crowd, or position themselves in unusual positions.
In addition, mandibular retrognathia affects patients not only at aesthetic level: many of the patients who have this type of malformation suffer from obstructive sleep apnea (OSA), a problem in which your breathing pauses during sleep. This occurs because of narrowed or blocked airways.
If you have obstructive sleep apnea (OSA), you usually begin snoring heavily soon after falling asleep.
- The snoring often becomes very loud.
- Snoring is interrupted by a long silent period while your breathing stops.
- The silence is followed by a loud snort and gasp, as you attempt to breathe.
- This pattern repeats throughout the night.
Most people with obstructive sleep apnea (OSA) do not know their breathing starts and stops during the night. Usually, a sleep partner or other family members hear the loud snoring, gasping, and snorting. Snoring can be loud enough to hear through walls. Sometimes, people with obstructive sleep apnea (OSA) wake up gasping for air.
People with sleep apnea may:
- Wake up unrefreshed in the morning
- Feel sleepy or drowsy throughout the day
- Act grumpy, impatient, or irritable
- Be forgetful
- Fall asleep while working, reading, or watching TV
- Feel sleepy while driving or even fall asleep while driving
- Have hard-to-treat headaches
Other problems that may occur include:
- Depression
- Hyperactive behavior, especially in children
- Difficult to treat high blood pressure
- Leg swelling (if apnea is severe)
Retrognathism complications
Retrognathia can produce or lead to some undesirable effects. The malocclusion often associated with retrognathia, and Angle Class 2 malocclusion most commonly prevents patients from chewing properly. There are many associated psychosocial stigmas associated with having a dentofacial deformity, especially in adolescents 16. Obstructive sleep apnea is likely more common in retrognathia patients as the airway is more closed and constricted. Airway management can be significantly more difficult in this patient population.
Retrognathism diagnosis
Physical exam is the best way to analyze patients for retrognathia. On grown adults, as part of a standard airway examination, examining the thyromental distance can be a predictor of a difficult airway. This implies retrognathia if the patient has a mandible that has not developed, the thyromental distance will be less than the standard three finger’s breadth, or approximately 7 mm 6.
A common adjunctive radiological review is the lateral cephalometric x-ray. This is typically traced and measured with a full cranio-cephalometic analysis that is beyond the scope of this article. There are a series of measurements that look at the position of the mandible to skull base to diagnosis mandibular hypoplasia (for example, the Sella-Nasion-B point angle (SNB) is generally 80 degrees in a Caucasian population, so an SNB angle of 72 degrees is indicative of retrognathia) 17.
Retrognathic mandible treatment
Retrognathic mandible treatment and management will depend on what your concerns are and what a patient or their parents desire. Most commonly retrognathia will be identified in children between the ages of four to ten years old and will likely be referred to an orthodontist for evaluation ideally around the ages of seven to eight. Generally, retrognathia is a benign condition without any other effects. This will allow the orthodontist to begin tracking the patient with serial cephalometric radiographs and potentially intervene early with non-surgical therapy like headgear or newer intra-oral techniques that have a similar effect in repositioning the mandible. If the child does not have a dentist or has not seen an orthodontist, a referral is recommended 18.
If one is concerned about airway management on a patient with retrognathia, this should be a strong indicator of a potentially difficult airway. Underdeveloped structures, anatomic distortion, potential malpositioning of the epiglottis, and tighter constriction of the muscles and surrounding structures all need to be considered. One is much more likely to have a Cormack and Lehane Grade 3 or 4 view, and that needs to be planned for 19.
A patient who has retrognathia from mandibular anterior-posterior hypoplasia will enter the treatment planning phase of their case during the first visit with the orthodontist. Orthodontists plan treatment years into the future and make movement and teeth extraction decisions based on skeletal growth and facial characteristics. Once the patient is ready for surgical correction, they will be referred to an oral and maxillofacial surgeon. A full series of photos and dental models are generally taken along with radiographs and a full workup completed and discussed with the treatment team, orthodontist, and patient. At this point, the surgical options are presented to the patient, and a surgical course decided upon. The standard workup and planning involving all proposed surgeries be completed on dental models and precise movements documented. Acrylic splints are then fabricated for use in stabilization of the teeth and bones for rigid internal fixation during surgery. More common over the last decade is virtual surgical planning, where a CT scan and patient models are digitally merged, and the operation is virtually planned within 0.01 mm; final surgical splints are custom printed on a 3D printer 20.
Treatments for retrognathic mandible
While people with mild retrognathia may not require any treatment, people with more severe cases may need orthodontic treatment and / or surgery.
In children, retrognathia can be treated with orthodontics. For example, a special harness can make the upper jaw grow more slowly so that the upper and lower jaws are more equal. However, despite the excellent results that can be obtained with current orthodontic methods, no orthodontist or dentist can grow a jaw, and functional devices do not change the skeletal pattern to a significant degree, which is why severe cases of retrognathism in adults and in certain adolescents with low growth potential are best treated surgically or by a combination of surgical and orthodontic methods.
Thus the treatments indicated for retrognathia are:
- If the problem is purely dental, or the patient is happy with his appearance and only wishes to correct his occlusion, the solution is an orthodontic treatment.
- For those patients with a good occlusion, but a retracted chin, a genioplasty, or chin surgery is recommended.
- When there is a skeletal problem or sleep apnea, the indicated treatment is an orthognathic surgery, which may, or may not, be accompanied by an orthodontic treatment depending on the case.
Bimaxillary orthognathic surgery, when the maxillofacial surgeon needs to surgically intervene on the mandibular and maxillary bone
Monomaxillary orthognathic surgery, when the maxillofacial surgeon only acts on one of the two skeletal structures.
It is important to note that after an orthognathic surgery of mandibular advancement, the individual’s jaw may return slightly to its original position. The average setback in the scientific literature is 2 millimeters. However, even with a certain relapse, surgery can greatly correct the condition.
Anyone seeking treatment for retrognathia should speak with a medical professional for more information. Each case is unique, so the orthodontist or maxillofacial surgeon must evaluate, diagnose and treat the condition according to the needs of each individual.
Retrognathism prognosis
The prognosis is benign, unless the retrognathia contributes to another more morbid condition like obstructive sleep apnea, temporomandibular joint dysfunction, or is associated with a more severe syndrome.
- Oculodentodigital dysplasia with mandibular retrognathism and absence of syndactyly: a case report with a novel mutation in the connexin 43 gene. Int J Oral Maxillofac Surg. 2007 Sep;36(9):858-60. Epub 2007 May 16. https://doi.org/10.1016/j.ijom.2007.03.004[↩]
- Thin-plate Spline Analysis of the Effects of Face Mask Treatment in Children with Maxillary Retrognathism. Journal of the Formosan Medical Association Volume 105, Issue 2, 2006, Pages 147-154 https://doi.org/10.1016/S0929-6646(09)60336-3[↩]
- Jenzer AC, Schlam M. Retrognathia. [Updated 2019 Nov 18]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK538303[↩][↩]
- Chapter 143 – Oropharyngeal Growth and Skeletal Malformations. Principles and Practice of Sleep Medicine (Sixth Edition) 2017, Pages 1401-1422.e7 https://doi.org/10.1016/B978-0-323-24288-2.00143-4[↩]
- Burgaz MA, Eraydın F, Esener SD, Ülkür E. Patient with Severe Skeletal Class II Malocclusion: Double Jaw Surgery with Multipiece Le Fort I. Turk J Orthod. 2018 Sep;31(3):95-102.[↩]
- Cattano D, Killoran PV, Cai C, Katsiampoura AD, Corso RM, Hagberg CA. Difficult mask ventilation in general surgical population: observation of risk factors and predictors. F1000Res. 2014;3:204.[↩][↩]
- Vaden JL, Williams RA, Goforth RL. Class II correction: Extraction or nonextraction? Am J Orthod Dentofacial Orthop. 2018 Dec;154(6):860-876.[↩]
- Riepponen A, Myllykangas R, Savolainen J, Kilpeläinen P, Kellokoski J, Pahkala R. Changes in posterior airway space and hyoid bone position after surgical mandibular advancement. Acta Odontol. Scand. 2017 Jan;75(1):73-78.[↩]
- Morice A, Soupre V, Mitanchez D, Renault F, Fauroux B, Marlin S, Leboulanger N, Kadlub N, Vazquez MP, Picard A, Abadie V. Severity of Retrognathia and Glossoptosis Does Not Predict Respiratory and Feeding Disorders in Pierre Robin Sequence. Front Pediatr. 2018;6:351.[↩]
- Luquetti DV, Speltz ML, Wallace ER, Siebold B, Collett BR, Drake AF, Johns AL, Kapp-Simon KA, Kinter SL, Leroux BG, Magee L, Norton S, Sie K, Heike CL. Methods and Challenges in a Cohort Study of Infants and Toddlers With Craniofacial Microsomia: The Clock Study. Cleft Palate Craniofac. J. 2019 Aug;56(7):877-889.[↩]
- Hartzell LD, Chinnadurai S. Microtia and Related Facial Anomalies. Clin Perinatol. 2018 Dec;45(4):679-697.[↩]
- Shibazaki-Yorozuya R, Nagata S. Preferential Associated Malformation in Patients With Anotia and Microtia. J Craniofac Surg. 2019 Jan;30(1):66-70.[↩]
- Simpson AM, Mehta ST, Siddiqi F, Yamashiro D, Gociman B. Modified Lefort Distraction Osteogenesis for the Treatment of Nager Syndrome-Associated Midface Hypoplasia: Technique and Review. J Craniofac Surg. 2018 Sep;29(6):e621-e623.[↩]
- De Silva SR, Painter SL, Hildebrand D. Möbius syndrome associated with obesity and precocious puberty. BMJ Case Rep. 2018 Dec 07;11(1).[↩]
- Radalj Miličić Z, Kranjčević Bubica A, Nikolov Borić D, Špalj S, Meštrović S. Linear Predictors of Facial Rotation Pattern in Croatian Subjects with Skeletal Class III Malocclusion. Acta Stomatol Croat. 2018 Sep;52(3):227-237.[↩][↩]
- Ribas J, Paço M, Pinho T. Perception of facial esthetics by different observer groups of Class II malocclusion with mandibular retrusion. Int J Esthet Dent. 2018;13(2):208-219.[↩]
- Ardani IGAW, Sanjaya ML, Sjamsudin J. Cephalometric Characteristic of Skeletal Class II Malocclusion in Javanese Population at Universitas Airlangga Dental Hospital. Contemp Clin Dent. 2018 Sep;9(Suppl 2):S342-S346.[↩]
- Rongo R, Antoun JS, Lim YX, Dias G, Valletta R, Farella M. Three-dimensional evaluation of the relationship between jaw divergence and facial soft tissue dimensions. Angle Orthod. 2014 Sep;84(5):788-94.[↩]
- Nejaim Y, Aps JKM, Groppo FC, Haiter Neto F. Evaluation of pharyngeal space and its correlation with mandible and hyoid bone in patients with different skeletal classes and facial types. Am J Orthod Dentofacial Orthop. 2018 Jun;153(6):825-833.[↩]
- Paunonen J, Helminen M, Peltomäki T. Long-term stability of mandibular advancement with bilateral sagittal split osteotomy. J Craniomaxillofac Surg. 2018 Sep;46(9):1421-1426.[↩]