Retropharyngeal abscess
Retropharyngeal abscess is an uncommon but potentially life-threatening infection and a collection of pus in the tissues in the back of the throat involving the retropharyngeal space which requires prompt diagnosis and aggressive therapy 1. A retropharyngeal abscess is most common in children under the age of five with 75% of cases occurring before the age of 5 years, and often in the first year of life 2, but it also occurs in adults 3. Typically patients under the age of five have an antecedent upper respiratory tract infection leading to suppurative cervical lymphadenitis and eventually retropharyngeal abscess 3. In older children and adults, a retropharyngeal abscess is caused by trauma to the posterior pharynx which leads to inoculation of the retropharyngeal space and results in abscess formation. As a retropharyngeal abscess grows in size, it can lead to upper airway obstruction and asphyxiation if left untreated. Although the mortality from sepsis does occur in these patients, the number one cause of death in patients with retropharyngeal abscess remains upper airway occlusion 4.
Retropharyngeal abscesses are often polymicrobial infections. Bacteria which commonly contribute to these infections include Group A Streptococcus pyrogens, Staphylococcus aureus, Fusobacterium, Haemophilus species, and other respiratory anaerobic organisms.
Treatment of retropharyngeal abscess ranges from prolonged courses of intravenous antibiotics to surgical incision and drainage 5.
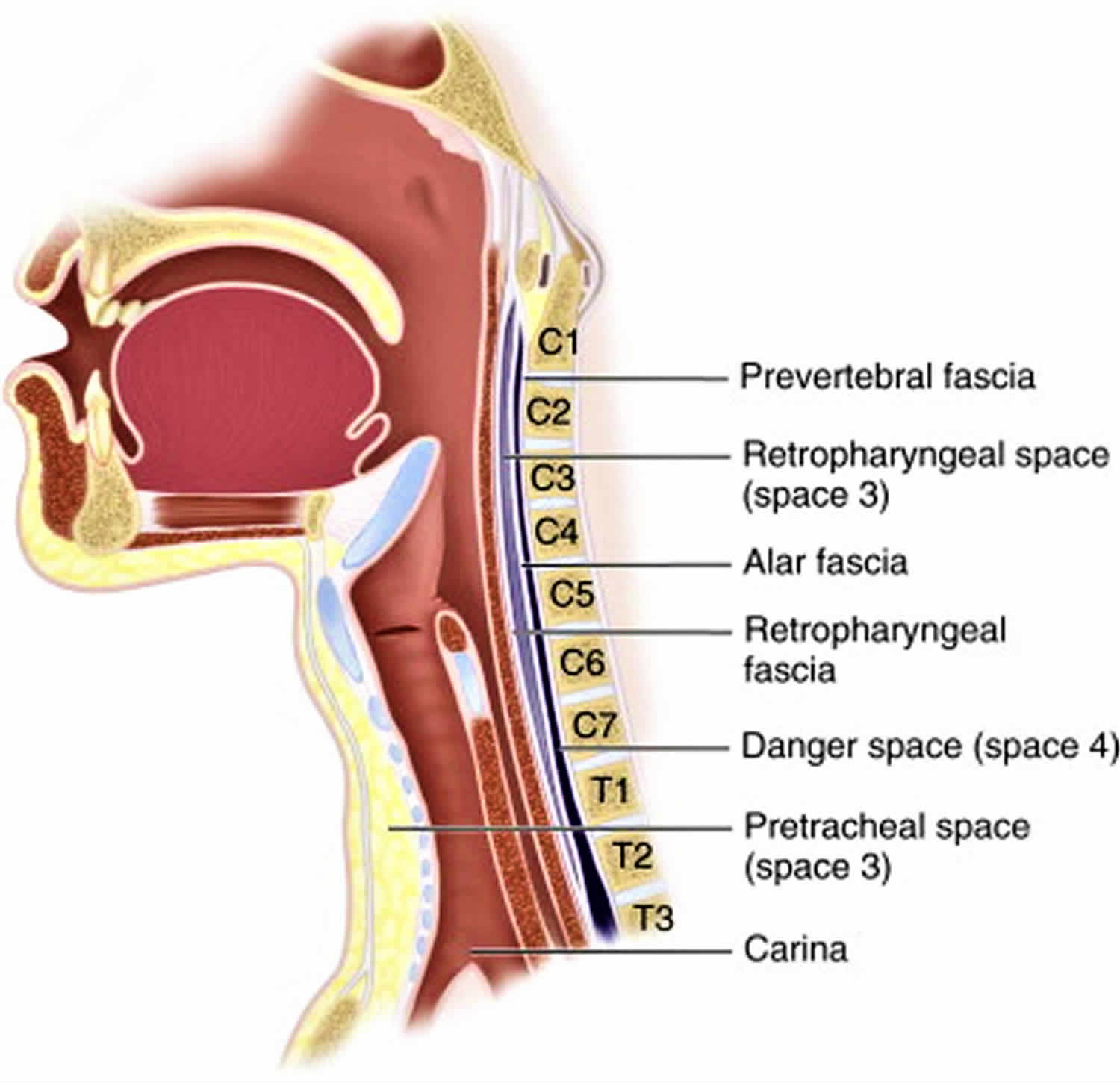
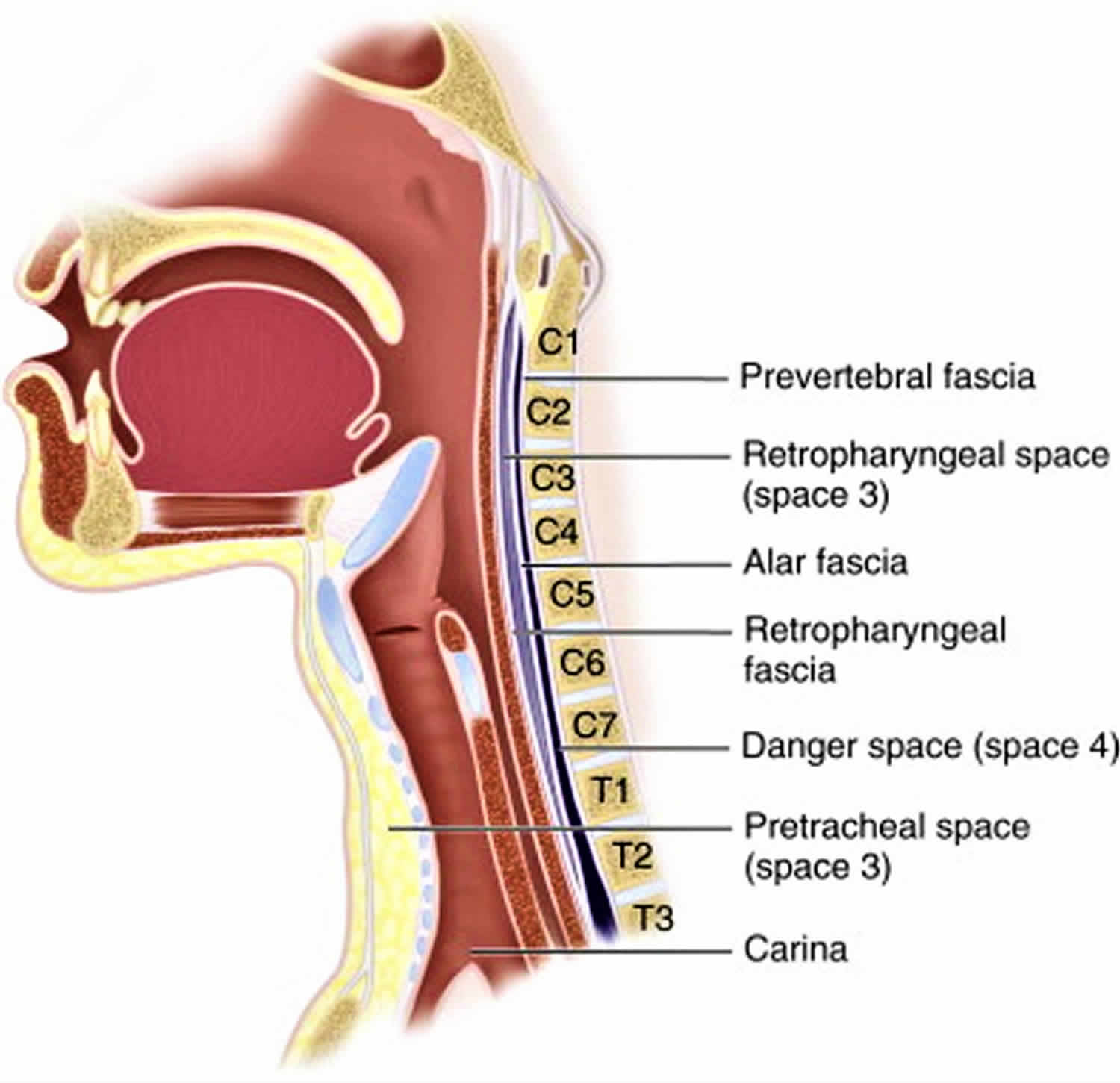
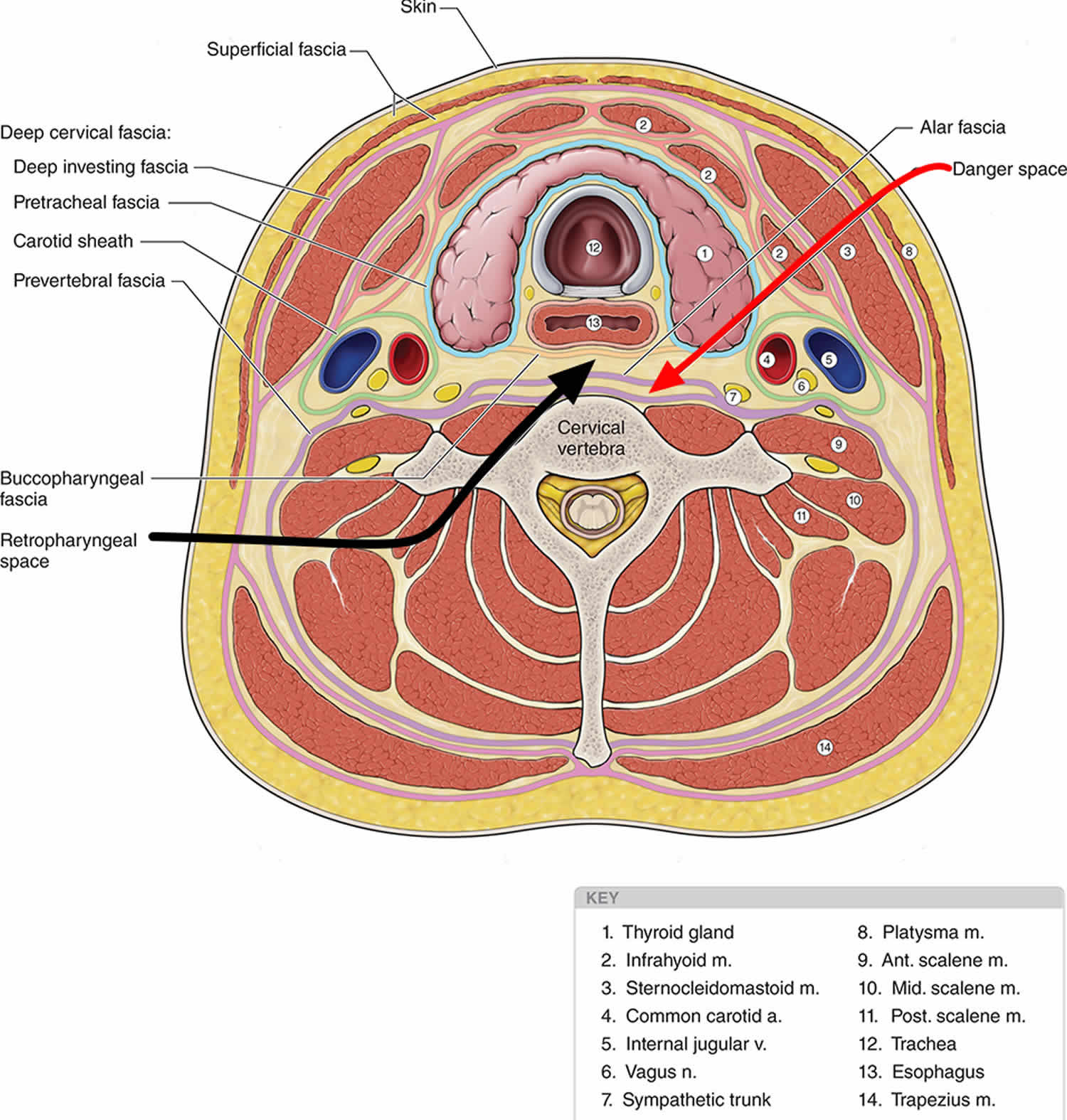
Figure 1. Retropharyngeal space
Retropharyngeal abscess causes
The retropharyngeal space contains chains of lymph nodes that drain the nasopharynx, adenoids, posterior paranasal sinuses, and middle ear. These lymph node chains are present in young children, but atrophy and involute typically by age four to five years old 3. In one-half of cases of retropharyngeal abscess patients report an antecedent upper respiratory tract infection. Upper respiratory tract infections result in suppurative adenitis of these retropharyngeal lymph nodes and eventual abscess formation.
Trauma to the posterior pharynx resulting in retropharyngeal infection and eventual abscess formation is typically the cause of retropharyngeal abscess in adults and older children. One-fourth of retropharyngeal abscesses is attributed to the trauma of the posterior pharynx resulting in inoculation of the retropharyngeal space, cellulitis, phlegmon formation, and eventually, retropharyngeal abscess 6.
Risk factors for retropharyngeal space infection include poor oral hygiene, diabetes, immunocompromised, and low socioeconomic status.
Retropharyngeal abscess symptoms
Retropharyngeal abscess symptoms include:
- Breathing difficulty
- Difficulty swallowing (dysphagia)
- Painful swallowing (odynophagia)
- Drooling
- Inability to tolerate oral secretions
- Trismus (reduced opening of the jaws)
- High fever
- High-pitched sound when inhaling (stridor)
- Change in voice, “hot potato voice,” muffled voice
- Muscles between the ribs pull in when breathing (intercostal retractions)
- Severe throat pain
- Neck stiffness
- Difficulty turning the head
- Refusal to extend neck due to pain or discomfort
- Torticollis (wry neck where the neck muscles contract, causing the head to twist to one side)
- Neck swelling, cervical lymphadenopathy
- Chest pain (mediastinal extension)
- Respiratory distress (stridor, tachypnea, retractions)
Early retropharyngeal abscess presents similarly to uncomplicated pharyngitis. Aspects of a patient’s history that are concerning for early retropharyngeal abscess would be antecedent upper respiratory tract infection or trauma to the posterior pharynx. As this infection progresses, symptoms related to upper aerodigestive obstruction become more prominent and typically progress over days.
Patients who present with retropharyngeal abscess typically are febrile and ill appearing. Early in the illness, patients may only have mild to moderate pharyngeal erythema and refusal to tolerate anything by mouth. As the disease progresses, pharyngeal erythema and swelling will become more prominent, and patients will be unable to tolerate even their oral secretions. Patients typically will have extreme discomfort with neck extension and often will prefer to hold their neck in flexion, as opposed to epiglottitis where patients will preferentially hold their necks in extension.
The oropharynx of a patient with a suspected retropharyngeal abscess only should be thoroughly examined with palpation or probing by clinicians who are experienced in emergent airway management. Abscess rupture can occur during the examination of the posterior pharynx, leading to aspiration and potential asphyxiation. It has been suggested that this exam should be performed with patients in the Trendelenburg position to prevent aspiration in case of abscess rupture, and suction equipment should be readily available.
Retropharyngeal abscess complications
Retropharyngeal abscess complications may include:
- Airway obstruction
- Aspiration
- Bronchial erosion
- Mediastinitis
- Sepsis
- Acute respiratory distress syndrome (ARDS)
- Cranial nerve palsies
- Esophageal perforation
- Erosion into carotid artery or jugular vein
- Meningoencephalitis
- Osteomyelitis
Retropharyngeal abscess diagnosis
The oropharynx of a patient with a suspected retropharyngeal abscess only should be thoroughly examined with palpation or probing by clinicians who are experienced in emergent airway management. Your health care provider will perform a physical exam and look inside the throat. Your health care provider may gently rub the back of the throat with a cotton swab. This is to take a sample of tissue to check it more closely. It is called a throat culture.
Other tests may include:
- Complete blood count (CBC)
- CT scan of the neck
- X-ray of the neck
- Fiber optic endoscopy
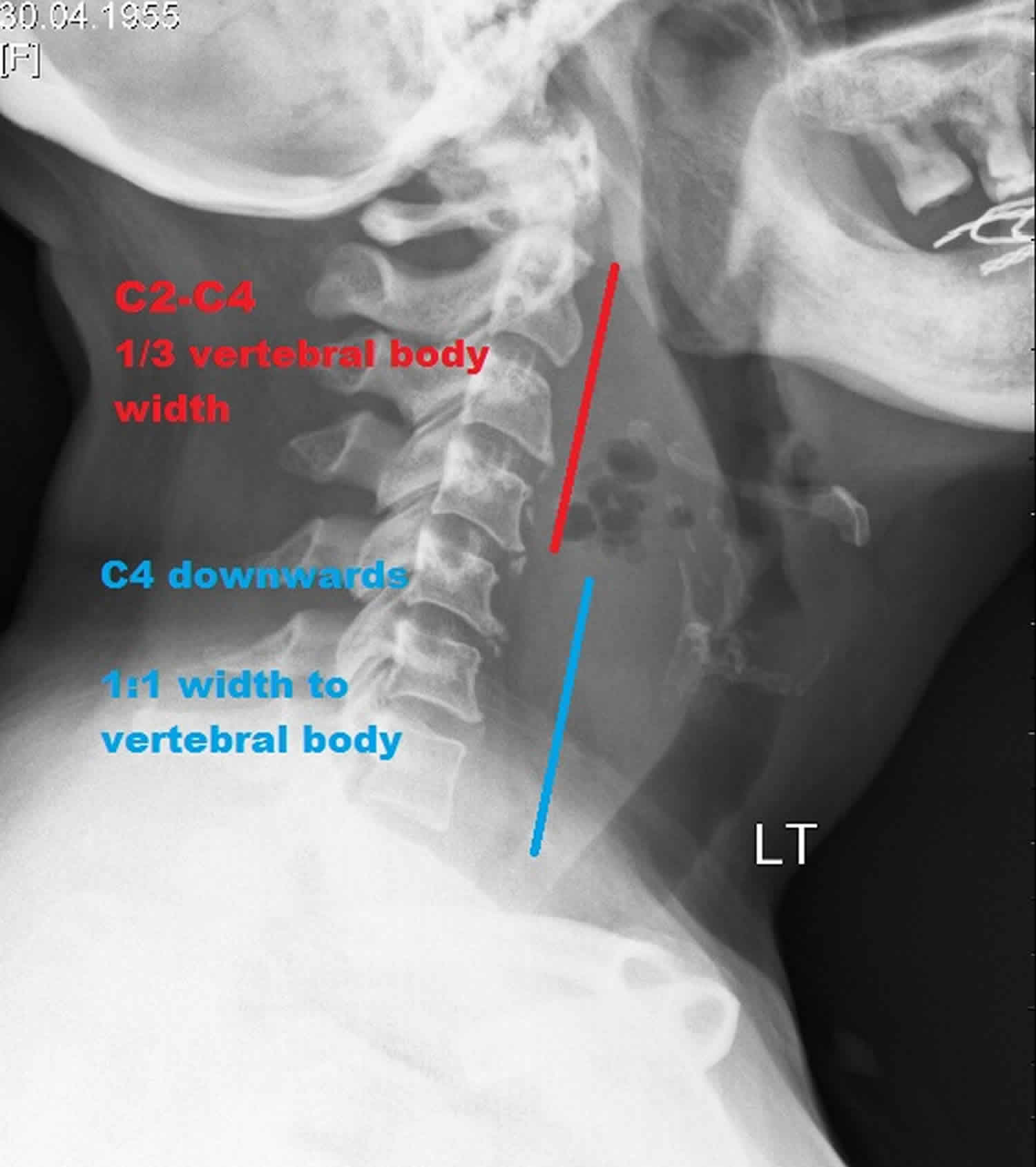
Lateral neck radiographs are typically the imaging study of choice in the initial evaluation of suspected retropharyngeal abscess, especially in young children. Lateral neck radiographs have the benefit of lower radiation exposure and tend to be better tolerated by patients who are exhibiting signs of airway compromise. Lateral neck x-rays should be obtained during inspiration with the neck held in normal extension. Improper technique in obtaining this imaging study can result in false positives for retropharyngeal infection. When the retropharyngeal infection is present, the depth of the prevertebral space will be increased on the lateral neck x-ray. In healthy individuals, the upper limit of normal of the prevertebral space is 7 mm at C2 and 14 mm at C6 in children. In healthy adults, the upper limit of normal of the prevertebral space is 7 mm at C2 and 2 mm at C6. A width of 30 mm at C6 indicates abscess collection.
Additionally, patients who are presenting with a concerning story for retropharyngeal abscess which is also endorsing chest pain should have a chest x-ray obtained to investigate for mediastinal involvement.
CT of the neck with intravenous contrast is the best imaging study to evaluate patients with a retropharyngeal abscess. If there is a concern for airway compromise in these patients, a clinician who is trained in emergency airway management should be present while the CT scan is being obtained. Patients may require an emergent surgical airway if upper airway obstruction occurs. The sensitivity of CT scan for detecting retropharyngeal abscess varies in the literature ranging from 64% to 100%.
In children, ultrasound is preferred as it does not involve radiation and is portable. In experienced hands, US can help determine the size and location of the abscess.
Labs including complete blood count, blood cultures, and preoperative labs are necessary if a retropharyngeal abscess is suspected. However, obtaining these labs should be delayed if phlebotomy will cause additional distress to the patient. This additional distress to the patient can cause early upper airway obstruction to become complete upper airway obstruction, especially in younger children. Both aerobic and anaerobic blood cultures should be obtained. In patients with retropharyngeal abscess white blood cell counts are greater than 12,000 in 91% of individuals 7.
Figure 2. Retropharyngeal abscess neck X-ray
Footnote: 55 year old lady, with pain in the neck on swallowing following perceived fish bone ingestion 4 days earlier. Known diabetic. This case illustrates a large retropharyngeal abscess, which was subsequently surgically drained.
[Source 8 ]Retropharyngeal abscess treatment
All patients presenting with a confirmed diagnosis of retropharyngeal infection require hospital admission, intravenous antibiotics, and otolaryngology consultation. Antibiotic therapy should cover upper respiratory organisms including anaerobic organisms. Patients presenting airway compromise should have immediate surgical incision and drainage performed to relieve their upper airway obstruction 9.
In patients not presenting with severe respiratory distress or airway compromise, management typically begins with a 24 to 48 hour trial of intravenous antibiotic therapy. After 24 to 48 hours of antibiotic therapy, the need for surgical incision and drainage will be reevaluated by a trained otolaryngologist. Factors which have been associated with an increased need for surgical incision and drainage include an abscess with a cross-sectional area greater than 2 cm² and symptoms for greater than 2 days. There is no evidence that patients presenting with mature abscesses greater than 3 cm² benefit from surgical intervention before 24 to 48 hours of antibiotic therapy.
All patients must have careful airway monitoring when undergoing treatment of retropharyngeal abscess especially during the first 24 to 48 hours of therapy.
Initial antibiotic therapy should include either ampicillin-sulbactam (50 mg/kg every 6 hours) or clindamycin (15 mg/kg every 8 hours). If patients appear septic or do not respond to initial antibiotic therapy, vancomycin or linezolid also should be administered. Parenteral antibiotics should be continued until patients are clinically improved and afebrile for 24 hours. After patients demonstrate clinical improvement and remain afebrile, they may be transitioned to oral antibiotics. Amoxicillin-clavulanate (45 mg/kg every 12 hours) or Clindamycin (13 mg/kg every 8 hours) are acceptable oral regimens. Oral antibiotics should be prescribed for 14 days, and the patient may be discharged home with strict return precautions.
After surgery, patients should be kept nothing by mouth (NPO) until all signs of the abscess have subsided. Close monitoring of the patient is required in an ICU setting. Most patients need prolonged antibiotics and total parenteral nutrition (TPN) for 4-6 weeks.
Retropharyngeal abscess prognosis
When the diagnosis is made early and treatment instituted, the prognosis is good. But the patient needs aggressive treatment, preferably in the ICU. If there is any delay in treatment, complications are common and the disorder carries a mortality rate of over 40% 10.
- Retropharyngeal abscess. https://medlineplus.gov/ency/article/000984.htm[↩]
- Craig FW, Schunk JE. Retropharyngeal abscess in children: clinical presentation, utility of imaging, and current management. Pediatrics. 2003;111 (6 Pt 1): 1394-8.[↩]
- Gossman W, Knorr TL, Sinha V. Abscess, Retropharyngeal. [Updated 2019 Jul 10]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK441873[↩][↩][↩]
- Argintaru N, Carr D. Retropharyngeal Abscess: A Subtle Presentation of a Deep Space Neck Infection. J Emerg Med. 2017 Oct;53(4):568-569.[↩]
- Angajala V, Hur K, Jacobson L, Hochstim C. Geographic health disparities in the Los Angeles pediatric neck abscess population. Int. J. Pediatr. Otorhinolaryngol. 2018 Oct;113:134-139.[↩]
- Joshua J, Scholten E, Schaerer D, Mafee MF, Alexander TH, Crotty Alexander LE. Otolaryngology in Critical Care. Ann Am Thorac Soc. 2018 Jun;15(6):643-654.[↩]
- Quinn NA, Olson JA, Meier JD, Baskin H, Schunk JE, Thorell EA, Hodo LN. Pediatric lateral neck infections – Computed tomography vs ultrasound on initial evaluation. Int. J. Pediatr. Otorhinolaryngol. 2018 Jun;109:149-153.[↩]
- Retropharyngeal abscess. https://radiopaedia.org/cases/retropharyngeal-abscess-4[↩]
- Adoviča A, Veidere L, Ronis M, Sumeraga G. Deep neck infections: review of 263 cases. Otolaryngol Pol. 2017 Oct 30;71(5):37-42.[↩]
- Côrte FC, Firmino-Machado J, Moura CP, Spratley J, Santos M. Acute pediatric neck infections: Outcomes in a seven-year series. Int. J. Pediatr. Otorhinolaryngol. 2017 Aug;99:128-134.[↩]