Second impact syndrome
Second-impact syndrome (SIS) also called repetitive head injury syndrome, is a rare traumatic brain injury that occurs in athletes receiving a second head injury while still symptomatic from a prior head injury 1. Second impact syndrome consists of two events. Second-impact syndrome typically involves an athlete suffering post-concussive symptoms following a head injury 2. If, within several weeks, the athlete returns to play and sustains a second head injury, diffuse cerebral swelling, brain herniation, and death can occur 3. Second-impact syndrome can occur with any two events involving head trauma. While it is a relatively rare condition, second-impact syndrome is devastating in that young, healthy patients may die within a few minutes. Emergency physicians should be aware of second-impact syndrome and educate patients who have experienced or are at risk of experiencing a head injury and their parents concerning when to allow an athlete to return to play, as second impact syndrome is often deadly 4.
The term second impact syndrome entered the medical lexicon in 1984 when Saunders and Harbaugh wrote an article describing a case report of a football player who died four days after suffering a head injury after he returned to play on the day of his death 5. He collapsed and died after a presumed second head injury. Recently SIS has gained increased attention as many cite athletes sustaining a concussion and returning to the sport early as being particularly at risk.
A review article in 2016 completed a PubMed search and found only been 36 cases reported in 15 publications with 17 cases meeting inclusion criteria 6. The characteristics of an athlete susceptible to a second impact injury were male gender, ages 13-24, contact sports like American football, boxing, and hockey. Only seven of the 17 receiving a direct blow to the head and the others were thought to have received a blow to the body and the forces transmitted to the head. CT imaging demonstrated diffuse cerebral edema with midline shift leading to herniation in 4 of the cases. Additionally, all of the cases had either thin or moderate subdural hematomas, and 2 of the cases had a subarachnoid hemorrhage, and three suffered an ischemic stroke.
Second impact syndrome causes
There have been very few confirmed cases of second-impact syndrome to date; therefore, the exact incidence, risk, and pathophysiology of second-impact syndrome are poorly understood. According to the Centers for Disease Control and Prevention (CDC), an estimated 1.6 to 3.8 million sports-related concussions occur in the United States each year 5. This is widely regarded as an underestimation, as many people suffering from mild traumatic brain injuries do not seek medical attention 7. Several studies have also demonstrated increasing incidence of sport-related concussion in recent decades 8.
While the cause of a concussion is generally understood, the cause of a second impact syndrome is not well understood. The generally accepted cause relates to sustaining a second concussion before the brain has a chance to recover from the initial insult fully. The athlete will rapidly develop altered mental status and a loss of consciousness within seconds to minutes of the second hit resulting in catastrophic neurological injury 6. The catastrophic injury results from the dysfunctional cerebral blood flow autoregulation leading to an increase in intracranial pressure. The pressure rapidly develops and eventually results in brain herniation. The herniation may occur either medially across the falx cerebri or inferiorly through the foramen magnum, resulting in brain stem injury and rapid deterioration and leading to death within 2 to 5 minutes.
Following an initial insult, there is characteristic ionic fluxes, acute metabolic changes, and cerebral blood flow alterations that occur immediately after cerebral concussions. Extracellular potassium concentration can increase massively in the brain, followed by hypermetabolism which can last up to ten days. This makes the brain more vulnerable and susceptible to death after a second sub-lethal insult of even less intensity.
A recent case report sheds some light on the injury pattern 9. An athlete returned to hitting drills five days after his initial concussion. He had a normal CT scan on day four but had a persistent severe headache. After getting hit at practice one day later, he collapsed several plays later after complaining of headaches and not being able to feel his legs. A second CT done in a local emergency room demonstrated bilateral but thin subdural hematomas. However, a subsequent MRI demonstrated caudal displacement of midline structures with injury to both thalami resulting in transtentorial herniation 9.
Second impact syndrome prevention
At this point, prevention seems to be the most logical answer for a second impact syndrome. Parents and athletes should be educated on the potential complications of a concussion, symptoms, and an expected time course for recovery.
Any athlete who still shows signs of concussion should not be allowed to return to play. Such signs include fatigue, headache, disorientation, nausea, vomiting, feeling “in a fog” or “slowed down,” as well as other differences from a patient’s baseline 10. If there are any doubts about the severity of injury, the patient or athlete should not be allowed to resume play.
The difficulty lies in deciding the appropriate return to play when the athlete is completely asymptomatic 3. Parents, teachers and the coach must observe the athlete closely. High school athletes and those with scholarship possibilities, especially, will try to convince parents and coaches that they feel fine, in order to resume play. There are differences of opinion as to when it is appropriate for a post-concussive patient to resume play. Cantu 10 suggests a grading system to rate the severity of concussions, ranging from Grade 1 through Grade 3 (Table 1). Three widely referenced clinical guidelines advise on the timing and level of participation after a first concussion 11. Unfortunately, none are evidence based, and their recommendations differ widely. Some even discuss a stepwise approach to return to play. The emergency physician should focus on the initial stabilization, imaging and the exclusion of a life-threatening or surgically-treatable lesion. The emergency physician should also ensure appropriate outpatient follow up by a neurosurgeon or a sports physician who has expertise with concussive symptoms. Although information on second-impact syndrome is present in the medical literature, its description in 1984 may leave some non-specialists unaware of the potential danger. Currently the guidelines suggested by the American Academy of Neurology 12 listed in Table 2 are the most widely disseminated and used.
The most sensible approach to prevention is to prevent the first concussion. For soccer, Kangaroo Soccer Headgear, similar to that used in martial arts, is primarily intended to provide protection for children and youth players. Coverage extends around the head, including the ears. The headgear is intended to protect against player-to-player impacts 13. These headgear models did provide measurable benefit during head-to-head impacts, but not necessarily with ball impact. Experts advise wearing a helmet during high-impact contact sports and preventing or mitigating especially head-to-head contact.
Table 1. Data-driven Cantu grading system for concussion
| Grade 1 (mild) |
| No loss of consciousness; post-traumatic amnesia* or post-concussion signs or symptoms lasting less than 30 minutes |
| Grade 2 (moderate) |
| Loss of consciousness lasting less than 1 minute; Post-traumatic amnesia* or post-concussion signs or symptoms lasting longer than 30 minutes but less than 24 hours |
| Grade 3 (severe) |
| Loss of consciousness lasting more than 1 minute or post-traumatic amnesia* lasting longer than 24 hours; Post-concussion signs or symptoms lasting longer than 7 days |
Footnote: *Retrograde and anterograde
[Source 10 ]Table 2. Guidelines for the Management of Sport-Related Concussion
| Symptoms | First Concussion | Second Concussion |
|---|---|---|
| Grade 1: No loss of consciousness, transient confusion, resolution of symptoms and mental abnormalities in <15 minutes | Remove from play. Examine at 5-min intervals. May return to play if symptoms disappear and results of mental-function exam return to normal within 15 min | Allow return to play after 1 week if there are no symptoms at rest or with exertion. |
| Grade 2: As above, but with mental symptoms for >15 minutes | Remove from play and disallow play for rest of day. Examine for signs of intracranial lesion at sidelines and obtain further exam by a trained person the same day. Allow return to play after 1 week if neurological exam is normal. | Allow return to play after 2-week period of no symptoms at rest or with exertion. Remove from play for season if imaging shows abnormality. |
| Grade 3: Any loss of consciousness | Perform thorough neurological exam in hospital and obtain imaging studies when indicated. Assess neurologic status daily until post-concussive symptoms resolve or stabilize. Remove from play for 1 week if loss of consciousness lasts seconds; for 2 weeks if it lasts minutes; must be asymptomatic at rest and with exertion to return to play. |
Second impact syndrome symptoms
The typical second-impact syndrome scenario occurs usually when an athlete sustains an initial head injury with post-concussion symptoms such as a headache, dizziness and vertigo, then he suffers a second head injury before the symptoms associated with the first impact have cleared. The athlete during the second head injury precipitously lapses into a coma with signs of brain herniation.
Any athlete who has returned to play after a concussion should be watched carefully, even if they have had an appropriate recovery period and completed a return to play protocol. A concussed patient will report any combination of symptoms including a headache, nausea, memory loss, dizziness, blurry vision, confusion, fatigue, photo- or phonophobia, motor or sensory loss, poor hand-eye coordination, or emotional irritability/labiality 4. On physical examination, the patient may have an altered level of consciousness, retrograde, or post-traumatic amnesia, but generally, difficulty concentrating and balance seems to be consistently impaired. Additionally, there may be sensory or motor abnormalities, visual abnormalities. Unless the player has been knocked out, if they remain on the field of play may show signs of ataxia, running in the wrong direction, or slowed reaction time.
As concussions have been more widely recognized and the complications related to insufficient recovery have become better recognized, sideline evaluations have developed. Sideline evaluation of cognitive function is an essential component in the assessment of this injury. Brief neuropsychological test batteries that assess attention and memory function have been shown to be practical and effective.
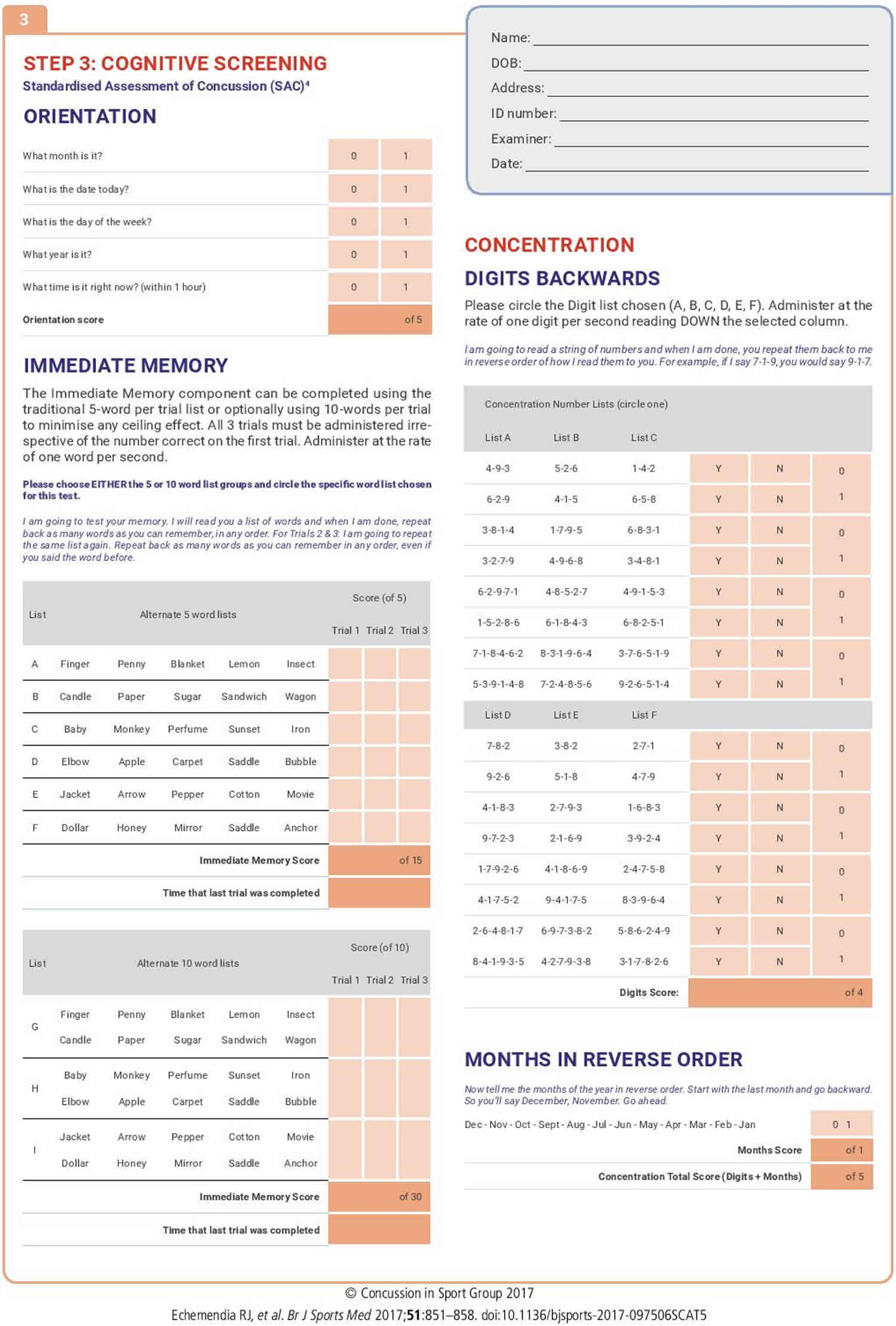
Standardised Assessment of Concussion (SAC) 14, which measures orientation, immediate memory, concentration, and delayed recall, and, when compared with a baseline score, has been found to have high sensitivity and specificity for diagnosing sport-related concussion 15.
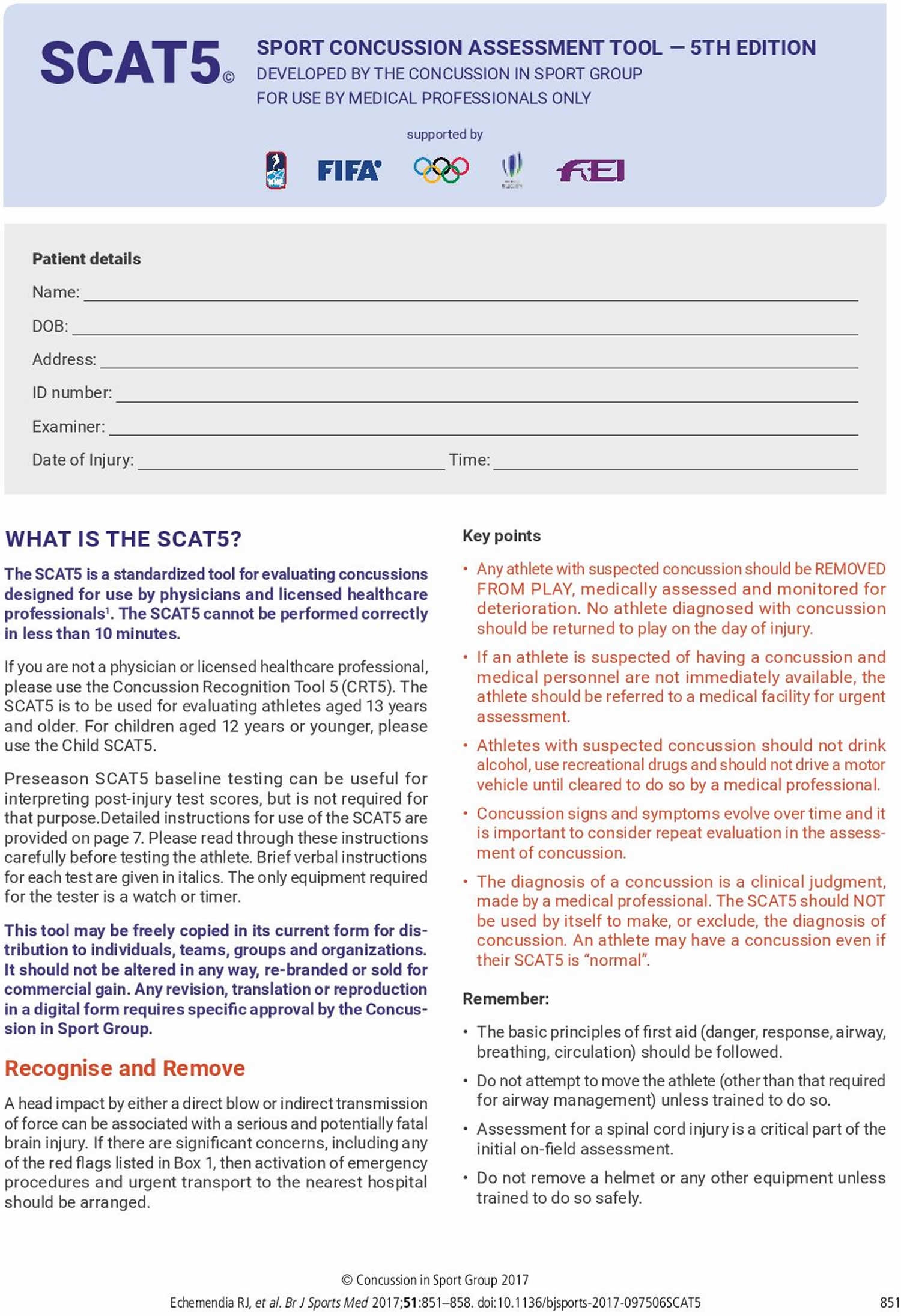
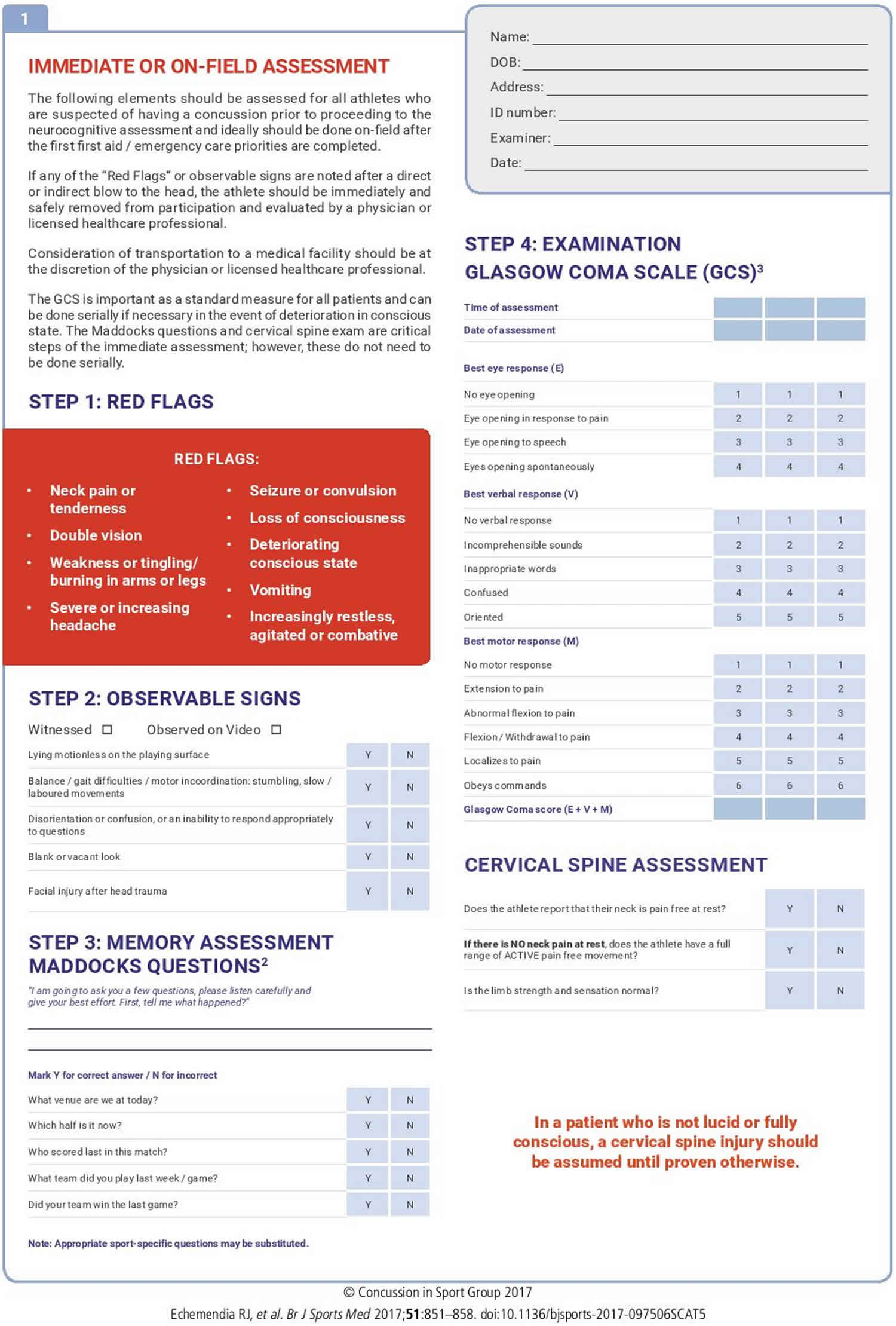
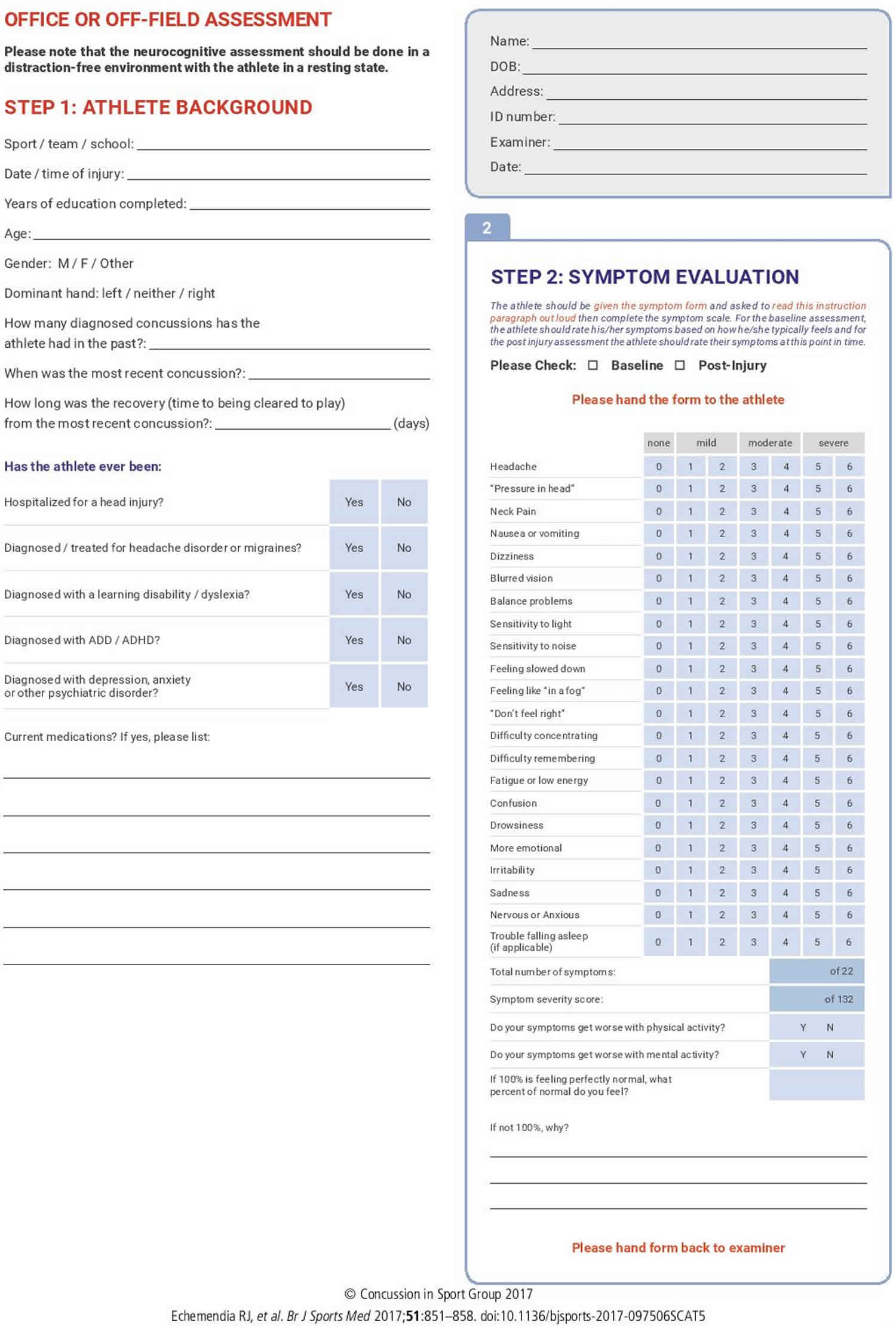
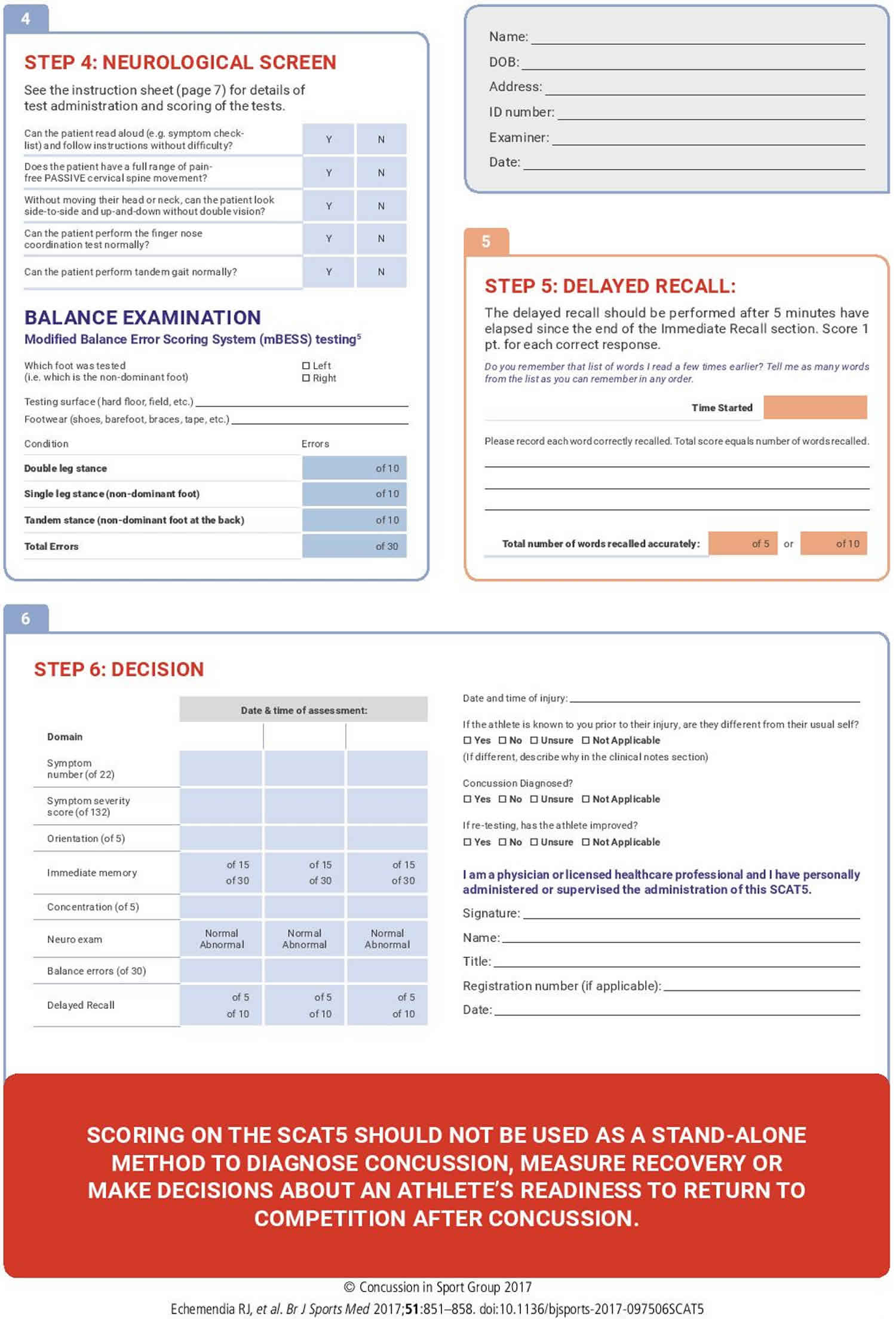
Today, perhaps the most well-known and comprehensive evaluation is the Sport Concussion Assessment Tool (SCAT), which has undergone several iterations to optimize its power and utility. Of note, the SCAT includes the aforementioned Standardised Assessment of Concussion (SAC). The SCAT5 is the most recent version and starts with an immediate on-field assessment, which sequentially involves identification of red flags warranting immediate medical attention, observable signs, orientation assessment (Maddocks’ questions) 16, Glasgow Coma Scale (GCS), cognitive assessment (SAC), postural stability, and a cervical spine assessment (Figure 1). The entire SCAT5 is lengthy and not administered entirely on the sideline, but elements can be used immediately, saving the rest for a more controlled environmental setting (e.g., locker room or office examination room).
For an athlete who has collapsed with a suspected second-impact syndrome, a Glasgow Coma Scale (GCS) score, pupillary reactivity, deep tendon reflexes, upper/lower extremity clonus, and the presence or absence of a Babinski reflex can be done prior to transport or upon arrival at the emergency room.
Due to the challenges of what constitutes a second impact syndrome, the paucity of research, and the rapidly progressing nature of the condition, it is difficult to provide good guidance on an appropriate history and physical exam. Perhaps clinicians should change their mindset and think every concussion they see, especially in male athlete ages 13-24, could be a second impact syndrome and observe the injured athlete closely for progressing signs or symptoms 4.
Figure 1. SCAT5
[Source 17 ]Second impact syndrome diagnosis
Obtaining a thorough history is critical in evaluating a patient with a suspected brain injury. Though the patient will unlikely be able to provide a good history, one should gather as much information from those who may have witnessed the incident. It is especially important to determine how the injury occurred, if there is any seizure or concussion history, if alcohol or illicit drug use was involved, whether or not there was any loss of consciousness, any resultant weakness or paresthesias, difficulty walking, or incontinence of the bladder or bowel.
Patients who have experienced significant injury or loss of consciousness, continued symptoms, deterioration in neurologic function, or neurologic deficits should be evaluated with imaging studies.
Screening for alcohol or illicit drugs would be recommended. Computed tomography (CT) scanning is the preferred imaging modality for acute head trauma. It is a more sensitive imaging modality for detecting acute hemorrhage (e.g., non-enhanced CT). It provides better delineation of bone (e.g., for detecting any skull fractures) and more sensitive in detecting acute hemorrhage and identifying any surgically reversible injuries.
Current guidelines recommend a CT for a suspected skull fracture, intracranial bleeding, or other intracranial disorders based on physical exam findings 18. Since a second impact syndrome injuries generally cause loss of consciousness, it would seem prudent to start with a CT scan of the head.
Second impact syndrome treatment
The management of second impact syndrome is limited due to the limited understanding of the condition, paucity of research, and the controversial nature of the condition 4. The management of second impact syndrome starts with prompt recognition of a sports-related concussion and protecting the athlete until they recover from the initial injury. The current treatment guidelines consist of relative rest, both cognitive and physical, and then a graded return to play. This should be supervised ideally by the team physician (with experience in managing concussions) and athletic training staff. The athlete should not be cleared to return to full participation until they have completed a return to play protocol, and the medical staff gives clearance 19.
Return to play
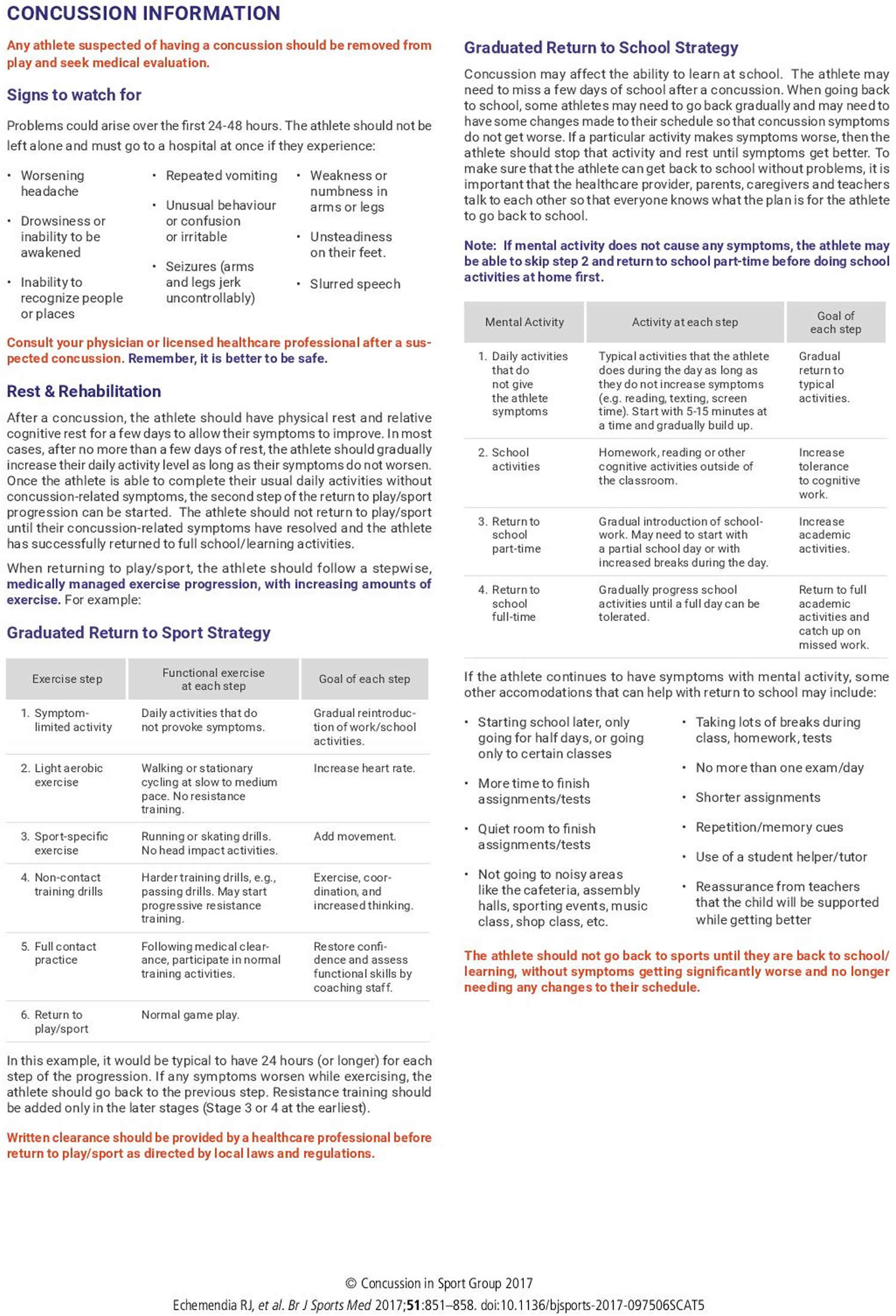
Return to play is the resumption of athletic participation following return to neurologic baseline. It is suggested that this occur after return to learn, which is resumption of classroom learning with tolerable or resolved symptoms. The return to play process suggested by McCrory et al. and the Concussion in Sport Group is a stepwise process, outlined below in stages 20.
- Stage 1: Activity limited by symptoms: Introduction of daily activities that do not provoke symptoms.
- Stage 2: Light aerobic exercise of low intensity: Elevation of heart rate above baseline activity with actions such as walking or cycling at a leisurely pace.
- Stage 3: Exercise specific to sport: Begin sport-specific movement such as running; contact strictly avoided.
- Stage 4: Training without contact: Resume drills with continued strict avoidance on contact with the goal of resuming coordination.
- Stage 5: Resumed full contact practice: Participate in practice drills including contact. Close monitoring is suggested.
- Stage 6: Full return to play: Resume normal participation in the sport.
For youth athletes, each stage lasts for 24 hour before progression onto the next stage. In the United States, progression through the return to play steps is often mandated by state law. Should symptoms be provoked at any stage, there is ceasing of activity and a day of rest, then a subsequent resumption of the previous stage 20. Return to learn is accomplished in the first stage, suggesting that the cognitive baseline should be reached before beginning to incorporate exercise into the recovery 21.
- Halstead ME, Walter KD., Council on Sports Medicine and Fitness. American Academy of Pediatrics. Clinical report–sport-related concussion in children and adolescents. Pediatrics. 2010 Sep;126(3):597-615.[↩]
- Cantu RC. Second impact syndrome. Clin Sports Med. 1998;17:37–44.[↩]
- Bey T, Ostick B. Second impact syndrome. West J Emerg Med. 2009;10(1):6–10. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2672291[↩][↩]
- May T, Foris LA, Donnally III CJ. Second Impact Syndrome. [Updated 2019 Nov 20]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2020 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK448119[↩][↩][↩][↩]
- Stovitz SD, Weseman JD, Hooks MC, Schmidt RJ, Koffel JB, Patricios JS. What Definition Is Used to Describe Second Impact Syndrome in Sports? A Systematic and Critical Review. Curr Sports Med Rep. 2017 Jan/Feb;16(1):50-55.[↩][↩]
- McLendon LA, Kralik SF, Grayson PA, Golomb MR. The Controversial Second Impact Syndrome: A Review of the Literature. Pediatr. Neurol. 2016 Sep;62:9-17.[↩][↩]
- McKeithan L, Hibshman N, Yengo-Kahn AM, Solomon GS, Zuckerman SL. Sport-Related Concussion: Evaluation, Treatment, and Future Directions. Med Sci (Basel). 2019;7(3):44. Published 2019 Mar 15. doi:10.3390/medsci7030044 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6473667[↩]
- Daneshvar D.H., Nowinski C.J., McKee A.C., Cantu R.C. The epidemiology of sport-related concussion. Clin. Sports Med. 2011;30:1–17. doi: 10.1016/j.csm.2010.08.006[↩]
- Weinstein E, Turner M, Kuzma BB, Feuer H. Second impact syndrome in football: new imaging and insights into a rare and devastating condition. J Neurosurg Pediatr. 2013 Mar;11(3):331-4.[↩][↩]
- Cantu RC. Recurrent athletic head injury: risks and when to retire. Clin Sports Med. 2003;22:593–603.[↩][↩][↩]
- Repetitive Head Injury Syndrome. https://emedicine.medscape.com/article/92189-overview[↩]
- American Academy of Neurology. Practice parameter: the management of concussion in sports (summary statement) – report of the Quality Standards Subcommittee. Neurology. 1997;48:581–585.[↩]
- Withnall C, Shewchenko N, Wonnacott M, Dovrak J. Effectiveness of headgear in football. Brit J Sports Med. 2005;39(Suppl1):i40–i48.[↩]
- McCrea M., Kelly J.P., Randolph C., Kluge J., Bartolic E., Finn G., Baxter B. Standardized assessment of concussion (SAC): On-site mental status evaluation of the athlete. J. Head Trauma Rehabil. 1998;13:27–35. doi: 10.1097/00001199-199804000-00005[↩]
- Giza C.C., Kutcher J.S., Ashwal S., Barth J., Getchius T.S., Gioia G.A., Gronseth G.S., Guskiewicz K., Mandel S., Manley G., et al. Summary of evidence-based guideline update: Evaluation and management of concussion in sports: Report of the Guideline Development Subcommittee of the American Academy of Neurology. Neurology. 2013;80:2250–2257. doi: 10.1212/WNL.0b013e31828d57dd[↩]
- McCrory P, Meeuwisse W, Dvořák J, Aubry M, Bailes J, Broglio S, Cantu RC, Cassidy D, Echemendia RJ, Castellani RJ, Davis GA, Ellenbogen R, Emery C, Engebretsen L, Feddermann-Demont N, Giza CC, Guskiewicz KM, Herring S, Iverson GL, Johnston KM, Kissick J, Kutcher J, Leddy JJ, Maddocks D, Makdissi M, Manley GT, McCrea M, Meehan WP, Nagahiro S, Patricios J, Putukian M, Schneider KJ, Sills A, Tator CH, Turner M, Vos PE. Consensus statement on concussion in sport-the 5th international conference on concussion in sport held in Berlin, October 2016. Br J Sports Med. 2017 Jun;51(11):838-847.[↩]
- Sport concussion assessment tool – 5th edition. Echemendia RJ, et al. Br J Sports Med 2017;51:851–858. doi:10.1136/bjsports-2017-097506SCAT5 https://bjsm.bmj.com/content/bjsports/51/11/851.full.pdf[↩]
- Guenette JP, Shenton ME, Koerte IK. Imaging of Concussion in Young Athletes. Neuroimaging Clin. N. Am. 2018 Feb;28(1):43-53.[↩]
- Harmon KG, Clugston JR, Dec K, Hainline B, Herring S, Kane SF, Kontos AP, Leddy JJ, McCrea M, Poddar SK, Putukian M, Wilson JC, Roberts WO. American Medical Society for Sports Medicine position statement on concussion in sport. Br J Sports Med. 2019 Feb;53(4):213-225.[↩]
- McCrory P., Meeuwisse W., Dvorak J., Aubry M., Bailes J., Broglio S., Cantu R.C., Cassidy D., Echemendia R.J., Castellani R.J., et al. Consensus statement on concussion in sport-the 5th international conference on concussion in sport held in Berlin, October 2016. Br. J. Sports Med. 2017;51:838–847.[↩][↩]
- McAvoy K., Eagan-Johnson B., Halstead M. Return to learn: Transitioning to school and through ascending levels of academic support for students following a concussion. NeuroRehabilitation. 2018;42:325–330. doi: 10.3233/NRE-172381[↩]