Seminoma cancer
Seminoma is a type cancer derived from germ cell tumor (malignant germ cell tumor) that involves most commonly the testicle where it’s called seminoma testicular cancer or less frequently the mediastinum (area between the lungs) where it’s called mediastinal seminoma, the retroperitoneum (the back wall of the abdomen) where it’s called retroperitoneal seminoma, or other extra-gonadal sites where it’s called extra-gonadal seminoma (see Figure 4 below) 1. Seminomas in the testicle are common among men ages 15 to 34 years old 1. Most testicular cancers are germ cell tumors and about half of these are seminomas, which tend to affect older men, with a peak incidence in men aged 30 to 34 years 2. In the United States, testicular seminoma is the most common subtype of testicular cancer 3. A higher incidence of seminoma is seen among Whites than in African Americans, and the rate has increased in the White population over recent decades 4. In 2021, there were an estimated 299,845 men living with testicular cancer in the United States 5.
The 2 main types of testicular germ cell tumors are seminomas and nonseminomas. These 2 types grow and spread differently and are treated differently. Seminomas tend to grow and spread more slowly than non-seminoma germ cell tumor (i.e., embryonal carcinoma, yolk sac carcinoma, choriocarcinoma and teratoma), although some seminomas can grow very rapidly too. Nonseminomas tend to grow and spread more quickly than seminomas. Seminomas are more sensitive to radiation. A testicular tumor that contains both seminoma and nonseminoma cells is treated as a nonseminoma.
Seminomas can be subdivided into one of 3 categories based on histology:
- Classic seminoma: 95 percent of seminomas are classic
- Anaplastic seminoma
- Spermatocytic seminoma: tend to occur in older men and has an excellent prognosis.
Seminoma usually presents as a nodule or painless swelling of the testis. It may be an incidental finding by the patients or his partner. Patients sometimes complain of a dull ache or heavy sensation in the lower abdomen, perineal area, or scrotum. Rarely, acute pain or blood in semen (hematospermia) may be the presenting symptoms. Cases of advanced disease, with metastases, present as a neck mass (cervical or supraclavicular lymph node metastases), cough or shortness of breath (pulmonary metastases), anorexia, nausea, vomiting, or gastrointestinal hemorrhage (gastroduodenal metastases), bone pain (skeletal metastases), central or peripheral nerve involvement (cerebral, spinal cord, or peripheral nerve involvement) 1. History of undescended testicle or cryptorchidism and orchiopexy (a surgery that moves an undescended testicle into the scrotum) is noted in some cases.
In men with a suspected testicular tumor, initial workup includes laboratory tests and imaging results. Serum tumor marker levels, including alpha-fetoprotein (AFP), beta-human chorionic gonadotropin (beta-HCG), and lactate dehydrogenase (LDH), are measured 1. Serum beta-HCG and LDH levels can be elevated in seminomas while AFP is not raised in pure seminomas 1. Lactate dehydrogenase (LDH) is a less specific marker, but levels can correlate with overall tumor burden. Beta-human chorionic gonadotropin (beta-HCG) levels are increased in 5-10% of patients with seminoma, and levels may correlate with metastatic disease but not with overall survival 1. Placenta-like alkaline phosphatase (ALP) may be elevated in patients with seminoma, especially when the tumor burden increases; however, these may also be increased with smoking 1.
Scrotal ultrasound is done to rule out other conditions. Scrotal ultrasound shows a homogeneous hypoechoic intratesticular mass, more extensive lesions may be inhomogeneous. Cystic areas and calcifications are less common in seminomas than in non-seminomatous tumors 1. For a definitive diagnosis, surgery to remove a testicle through an incision in the groin (inguinal orchiectomy) is performed, which is diagnostic as well as therapeutic. If your doctor thinks a lump on your testicle may be cancerous, you might have surgery to remove the testicle through an incision in the groin. NOTE: The surgeon does not cut through the scrotum into the testicle to remove a sample of tissue for biopsy, because if cancer is present, this procedure could cause it to spread into the scrotum and lymph nodes. It’s important to choose a surgeon who has experience with this kind of surgery.
Histologic and laboratory results confirm the diagnosis and help differentiate the type of testicular cancers. If cancer is found, the cell type (seminoma or nonseminoma) is determined in order to help plan treatment.
Once the diagnosis is confirmed, a chest x-ray or chest CT scan, abdominal and pelvic CT scan, MRI brain, and bone scan may be done to look for metastases (spread). PET can be used to assess disease activity following chemotherapy treatment and to identify recurrences 6. Risk stratification of seminomas is not dependent on serum tumor markers (unlike non-seminomatous germ cell tumors) but rather based on the presence or absence of nonpulmonary visceral metastases 7.
Seminoma is one of the treatable and curable cancers, with a survival rate above 95% if discovered in early stages 8, 9, 10, 11. Radical orchiectomy provides both diagnostic and therapeutic implications in seminoma. Radical orchiectomy involves removing the testicle and spermatic cord where it exits the body to identify and likely treat the majority of cancers localized to the testis 12. Radical orchiectomy is indicated for all stages of seminoma testicular cancer. Adjuvant (add-on) chemotherapy or radiotherapy depends upon the clinical staging that follows radical inguinal orchiectomy.
Generally, testicular seminoma treatment plans are as follows 13, 14, 15:
- Stage 1 testicular cancer: For patients with stage 1 seminoma, orchiectomy is usually curative 16, 17. Options for post-orchiectomy management include surveillance alone or adjuvant chemotherapy with one single infusion of carboplatin or prophylactic radiotherapy (declining interest).
- Stage 2 testicular cancer: Following radical inguinal orchiectomy, the treatment of stage 2 testicular seminoma depends on the extent of the lymph node involvement. Radiation therapy with or without cisplatin-based chemotherapy is recommended.
- Stage 3 testicular cancer: For stage 3 testicular seminomas, chemotherapy with bleomycin, etoposide, and cisplatin (BEP) or etoposide and cisplatin (EP) is preferred. Radiotherapy may be indicated in select cases 18. In patients with an intermediate prognosis, it might be hard to tolerate bleomycin, and therefore the addition of ifosfamide to etoposide and cisplatin (VIP) is reasonable 19.
After treatment patient requires life long follow up. Surveillance includes the following, with the frequency determined by the disease stage and duration of follow up.
- History and physical examination
- Serum tumor markers ( beta-hCG, LDH, AFP)
- Chest radiography
- CT scan of the abdomen, with or without CT scan of the pelvis
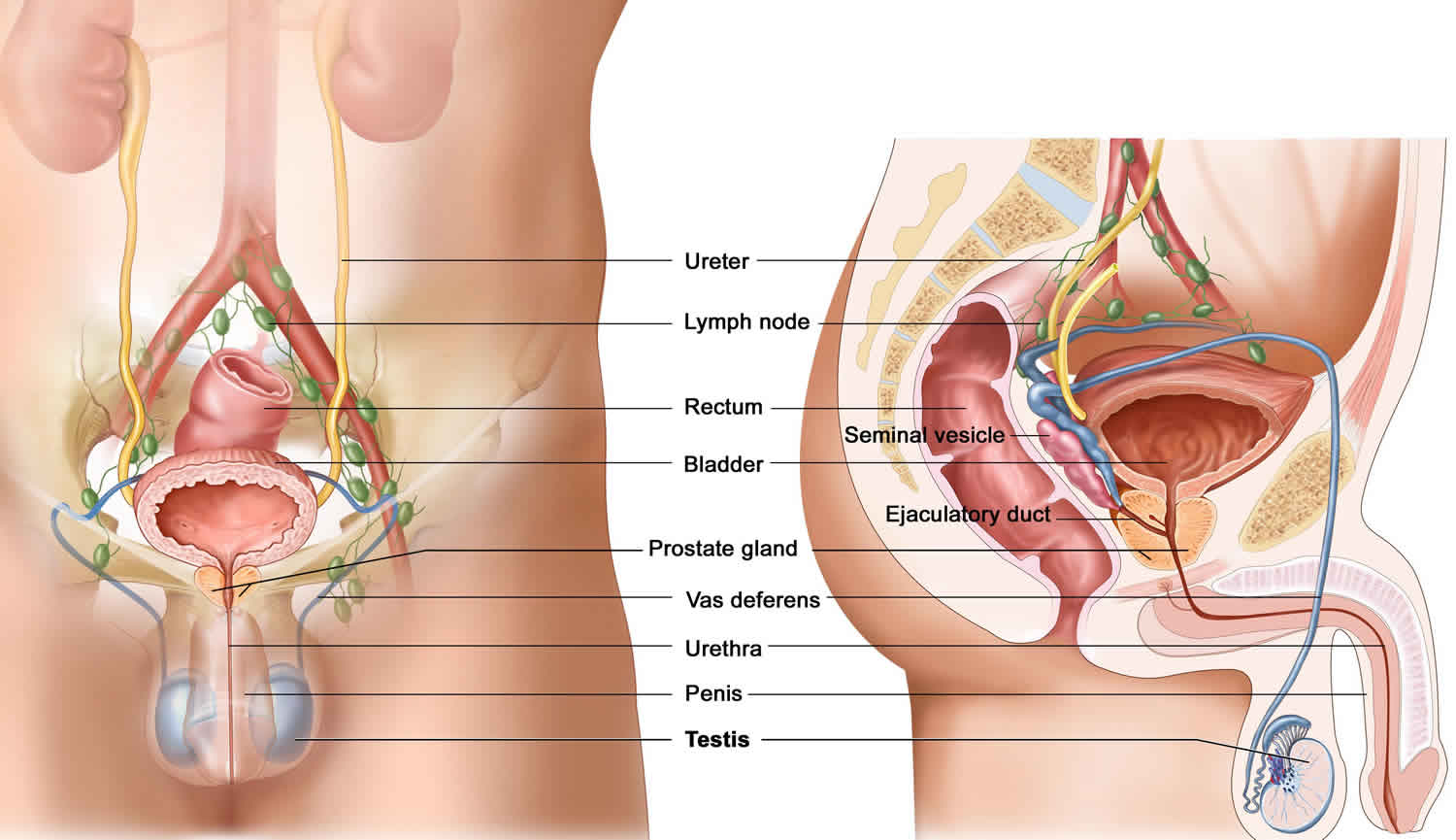
Testis anatomy
The testes or testicles (a single testicle is called a testis), are paired oval glands in the scrotum measuring about 5 cm (2 inch) long and 2.5 cm (1 inch) in diameter. Testicles are part of the male reproductive system. Each testis (singular) has a mass of 10–15 grams. The 2 oval glands are each normally a little smaller than a golf ball in adult males. They’re held within a sac of skin called the scrotum. The scrotum hangs under the base of the penis.
Testicles have 2 main functions:
- They make male hormones (androgens) such as testosterone.
- They make sperm, the male cells needed to fertilize a female egg cell to start a pregnancy.
The testes develop near the kidneys, in the posterior portion of the abdomen and they usually begin their descent into the scrotum through the inguinal canals (passageways in the lower anterior abdominal wall) during the latter half of the seventh month of fetal development.
A serous membrane called the tunica vaginalis, which is derived from the peritoneum and forms during the descent of the testes, partially covers the testes. A collection of serous fluid in the tunica vaginalis is called a hydrocele. It may be caused by injury to the testes or inflammation of the epididymis. Usually, no treatment is required. Internal to the tunica vaginalis the testis is surrounded by a white fibrous capsule composed of dense irregular connective tissue, the tunica albuginea; it extends inward, forming septa that divide the testis into a series of internal compartments called lobules. Each of the 200–300 lobules contains one to three tightly coiled tubules, the seminiferous tubules, where sperm are produced. The process by which the seminiferous tubules of the testes produce sperm is called spermatogenesis.
The seminiferous tubules contain two types of cells: spermatogenic cells, the sperm-forming cells, and sustentacular cells or Sertoli cells, which have several functions in supporting spermatogenesis. Stem cells called spermatogonia develop from primordial germ cells that arise from the yolk sac and enter the testes during the fifth week of development. In the embryonic testes, the primordial germ cells differentiate into spermatogonia, which remain dormant during childhood and actively begin producing sperm at puberty. Toward the lumen of the seminiferous tubule are layers of progressively more mature cells. In order of advancing maturity, these are primary spermatocytes, secondary spermatocytes, spermatids, and sperm cells. After a sperm cell, or spermatozoon, has formed, it is released into the lumen of the seminiferous tubule. Sperm cells are then stored in a small coiled tube behind each testicle called the epididymis. This is where they mature.
During ejaculation, sperm cells are carried from the epididymis through the vas deferens to seminal vesicles, where they mix with fluids made by the vesicles, prostate gland, and other glands to form semen. This fluid then enters the urethra, the tube in the center of the penis through which both urine and semen leave the body.
Embedded among the spermatogenic cells in the seminiferous tubules are large sustentacular cells or Sertoli cells, which extend from the basement membrane to the lumen of the tubule. Internal to the basement membrane and spermatogonia, tight junctions join neighboring sustentacular cells to one another. These junctions form an obstruction known as the blood–testis barrier because substances must first pass through the sustentacular cells before they can reach the developing sperm. By isolating the developing gametes from the blood, the blood–testis barrier prevents an immune response against the spermatogenic cell’s surface antigens, which are recognized as “foreign” by the immune system. The blood–testis barrier does not include spermatogonia.
Sustentacular cells (Sertoli cells) support and protect developing spermatogenic cells in several ways. They nourish spermatocytes, spermatids, and sperm; phagocytize excess spermatid cytoplasm as development proceeds; and control movements of spermatogenic cells and the release of sperm into the lumen of the seminiferous tubule. They also produce fluid for sperm transport, secrete the hormone inhibin, and regulate the effects of testosterone and FSH (follicle-stimulating hormone).
In the spaces between adjacent seminiferous tubules are clusters of cells called interstitial cells or Leydig cells. These cells secrete testosterone, the most prevalent androgen. An androgen is a hormone that promotes the development of masculine characteristics. Testosterone also promotes a man’s libido (sexual drive).
The scrotum (bag), the supporting structure for the testes, consists of loose skin and underlying subcutaneous layer that hangs from the root (attached portion) of the penis. Externally, the scrotum looks like a single pouch of skin separated into lateral portions by a median ridge called the raphe. Internally, the scrotal septum divides the scrotum into two compartments, each containing a single testis. The location of the scrotum and the contraction of its muscle fibers regulate the temperature of the testes. Normal sperm production requires a temperature about 2–3°C below core body temperature. This lowered temperature is maintained within the scrotum because it is outside the pelvic cavity. In response to cold temperatures, the cremaster and dartos muscles contract. Contraction of the cremaster muscles moves the testes closer to the body, where they can absorb body heat. Contraction of the dartos muscle causes the scrotum to become tight (wrinkled in appearance), which reduces heat loss. Exposure to warmth reverses these actions.
Figure 1. Male reproductive system
Figure 2. Testicle anatomy
Figure 3. Scanning electron micrograph of the seminiferous tubules
Testicular cancer
Testicular cancer is a growth of cancerous cells that starts in the testicles. The testicles also called testes, are in the scrotum. The scrotum is a loose bag of skin underneath the penis. The testicles make sperm and the hormone testosterone.
There are 3 main types of primary testicular tumor:
- Germ cell tumors. Almost all testicular cancers start in the germ cells. Germ cell tumors are classified histologically into 2 broad classes: Seminomas and Non-seminomas. These 2 types grow and spread differently and are treated differently. Around 55 – 60 out of every 100 testicular cancers (around 55 – 60%) are pure seminomas. Seminoma testicular cancers tend to happen at an older age with a peak incidence in men aged 30 to 34 years. Seminomas often grow and spread (metastasize) more slowly than nonseminomas testicular cancer 2, 20. Nonseminoma testicular cancers tend to grow and spread more quickly than seminomas. Seminomas are more sensitive to radiation. Seminomas generally have a good prognosis, while non-seminomatous tumors are much more likely to present with metastatic disease as well as mixed germ cell tumors comprising of two or more than two different germ cell tumor components. A testicular tumor that contains both seminoma and nonseminoma cells is treated as a nonseminoma.
- Sex cord-stroma tumors also called gonadal stromal tumors. Sex cord-stroma tumors are tumors that develop from the supportive tissues around the germ cells in the testicle. These tumors are rare, making up less than 5 percent of testis cancers, and have an excellent prognosis if surgically resected. There are two types of stromal tumors:
- Leydig cell tumors: Leydig cells make the male hormone testosterone. Leydig cell tumors can develop in both adults and children. These tumors often make androgens (male hormones), but sometimes they make estrogens (female sex hormones). Most Leydig cell tumors are not cancer (benign). Leydig cell tumors seldom spread beyond the testicle and are most often cured with surgery. Still, a small number of Leydig cell tumors do spread to other parts of the body. These tend to have a poor outlook because they usually don’t respond well to chemo or radiation therapy.
- Sertoli cell tumors: Sertoli cell tumors start in normal Sertoli cells, which support and nourish the sperm-making germ cells. Like the Leydig cell tumors, sertoli cell tumors are usually benign. But if they spread, they usually don’t respond well to chemo or radiation therapy.
- Secondary testicular cancers. Cancers that start in another organ and then spread (metastasize) to the testicle are called secondary testicular cancers. These are not true testicular cancers – they don’t start in the testicles. They’re named and treated based on where they started. Lymphoma is the most common secondary testicular cancer. Testicular lymphoma is more common in men older than 50 than primary testicular tumors. The outlook depends on the type and stage of lymphoma. The usual treatment is surgical removal, followed by radiation and/or chemotherapy. In boys with acute leukemia, the leukemia cells can sometimes form a tumor in the testicle. Along with chemotherapy to treat the leukemia, this might require treatment with radiation or surgery to remove the testicle. Cancers of the prostate, lung, skin (melanoma), kidney, and other organs also can spread to the testicles. The prognosis for these cancers tends to be poor because these cancers have usually spread widely to other organs as well. Treatment depends on the specific type of cancer.
Testicular cancer is a rare type of cancer but it’s one of the most common cancers in young men. Testicular cancer can happen at any age, but it happens most often in men between the ages of 15 and 35. It is estimated that up to 10,000 American men will develop testicular cancer each year.
Not all men with testicular cancer experience symptoms, but many testicular cancers present as a small bump or lump on a testicle.
Testicular cancer can grow quickly. They often spread outside the testicle to other parts of the body.
Fortunately, testicular cancer is highly treatable, even when it spreads to other parts of the body. Treatments depend on the type of testicular cancer that you have and how far it has spread. Common treatments include surgery and chemotherapy.
Germ cell tumor
Germ cell tumors are tumors derived from a mass made of reproductive cells, also called primordial germ cells that migrate during embryogenesis from the yolk sac through the mesentery to the gonads (testicles and ovaries) (see Figure 3) 21, 22. “Germ” is short for “germinate”, which means to mature. For women germ cells eventually mature into eggs. For men germ cells mature into sperm. Germ cell tumors can generally be divided into gonadal (testicles and ovaries) and extragonadal (outside of the gonads). Germ cell tumors most often form where eggs get made (ovaries) and where sperm gets made (testicles). Less commonly, germ cell tumors form in body parts other than your ovaries and testicles, including your abdomen, chest, low back, tailbone and brain. These tumors are called extragonadal tumors.
Germ cell tumors may be malignant (cancerous) or benign (noncancerous). Both types of tumors can grow larger, but only cancerous (malignant) germ cell tumors can spread to other parts of your body. Cancer that’s spread (metastasized) can damage your organs and is more difficult to treat.
Germ cell tumors can also be broadly classified as teratomas, yolk sac tumors (endodermal sinus tumors), germinomas, embryonal cell carcinoma, polyembryomas, choriocarcinomas or mixed germ cell tumors.
- Teratomas are tumors that contain tissue like teeth, hair, muscle and bone. They may be mature or immature. Mature teratomas (dermoid cysts) are the most common type of ovarian germ cell tumor. They’re usually benign. Immature teratomas are typically cancerous, and they grow fast.
- Yolk sac tumors (endodermal sinus tumors) contain cells similar to those in a developing embryo. These tumors are cancerous, and they spread fast to lymph nodes and other organs. Yolk sac tumors are the most common malignant germ cell tumor diagnosed in children.
- Germinomas are cancerous tumors that may appear in your ovaries or testicles. Still, they’re most common in the brain and spinal cord (central nervous system). They’re called dysgerminoma when they’re in your ovaries and seminoma when they’re in your testicles.
- Embryonal cell carcinoma is a rare, cancerous germ cell tumor. It may exist in a pure form, but it often appears alongside other tumor types in a mixed germ cell tumor.
- Polyembryomas contain components that resemble embryos. They’re rare, fast-growing cancerous tumors often mixed with other types of germ cell tumors.
- Choriocarcinomas consist of cells that form the placenta during pregnancy. The placenta is an organ that allows the gestational parent to share nutrients with a fetus. Choriocarcinoma is a rare and cancerous germ cell tumor that can form in your ovaries or testicles but often occurs in the uterus. It can spread to both the fetus and the parent.
- Mixed germ cell tumors contain two or more types of malignant germ cell tumors. Many germ cell tumors are mixed.
Germ cell tumors in children are rare, making up only 3.5% of cancer diagnoses. Germ cell tumors are more common in adolescents and young adults, making up 13.9% of cancers diagnosed between ages 15 to 19. Germ-cell tumors affect predominantly younger males aged between 15 and 40 years, with nearly 74 500 new cases estimated globally in 2020 23, 24.
Germ cell tumors are classified histologically into 2 broad classes: Seminomas and Non-seminomas 2. Seminomas are the most common of germ cell tumors. However, both seminoma and non seminoma germ cell tumor (NSGCT) occur at about the same rate, and men can have either seminoma or nonseminomatous germ cell tumors (NSGCT) or a combination of both. Non-seminoma germ cell tumor (NSGCT) is the most likely testicular cancer to cause metastases which typically affect the lungs, liver, central nervous system, and bone in order of frequency 25.
For treatment planning, germ cell tumors are broadly divided into seminomas and nonseminomas because they have different prognostic and treatment algorithms 26. The good news is the prognosis for most germ cell tumors is excellent. For patients with seminomas (all stages combined), the cure rate exceeds 90%. For patients with low-stage seminomas or nonseminomas, the cure rate approaches 100% 27, 28, 29, 30, 31.
Figure 3. Germ cell tumors
[Source 32 ]Who is affected by germ cell tumors?
Anyone can have germ cell tumors, but infants, children, teens and young adults get them most often. Diagnoses increase and decrease based on age. For instance, diagnoses occur relatively frequently from infancy up to age 4 compared to the years immediately after. Germ cell tumor diagnoses increase as puberty approaches.
- Ovarian germ cell tumors are most common in people aged 10 to 14, but they also affect people in their 20s and 30s. Mature teratomas, which are benign, are the most common germ cell tumor diagnosis.
- Testicular germ cell tumors make up 75% of testicular cancer diagnoses in children and 90% of testicular cancers total. They’re more common in children younger than 4 and people ages 15 to 35.
- Extragonadal germ cell tumors account for 40% to 50% of germ cell tumor diagnoses from infancy to age 4. Still, children and young adults get them, too. In infants and children, these tumors most commonly appear at the base of their spine (sacrum) or tailbone (coccyx). In teens and young adults, extragonadal germ cell tumors occur most often in the center of their chest (mediastinum). Brain germ cell tumors — although rare — are more commonly diagnosed in people between 11 and 30.
Germ cell tumor symptoms
The symptoms of a germ cell tumor depend on factors like the tumor’s size and location in your body.
Ovarian germ cell tumors
Ovarian germ cell tumors don’t always cause symptoms. For instance, mature teratomas may not cause symptoms until they’ve grown large enough to create pressure in your abdomen. Often, they’re discovered on an ultrasound to determine what’s causing pelvic pain.
Ovarian germ cell tumor symptoms may include:
- Pelvic discomfort or pain.
- Painful mass in your ovary.
- Swollen belly (abdomen).
- Abdominal pain (similar to appendicitis).
- Irregular vaginal bleeding.
- Nausea.
Testicular germ cell tumors
The symptoms of testicular germ cell tumors are the same as those of testicular cancer.
Testicular germ cell tumor symptoms include:
- a lump or swelling in your testicle, but it can affect both testicles (>85% of men)
- your testicle getting bigger
- an ache or pain in your testicle or scrotum (the skin that covers the testicles) (about 20% to 30% of men experience a heavy dragging feeling or general ache)
- your scrotum feeling heavy, firm or hard
Other symptoms can include:
- a dull ache or pain in your back, groin or lower tummy
- back pain
- sudden swelling in the scrotum
- losing weight without trying
- a cough
- difficulty breathing or swallowing
- enlargement or tenderness of the breast tissue
- A small percentage present with symptoms of metastatic disease and infertility.
Extragonadal germ cell tumors
“Extragonadal” means outside of the gonads or outside of the sex organs (testicles and ovaries) 33. When germ cells that are meant to form sperm in the testicles or eggs in the ovaries travel to other parts of the body, they may grow into extragonadal germ cell tumors. Extragonadal germ cell tumors may begin to grow anywhere in the body but usually begin in organs such as the pineal gland in the brain, in the mediastinum (area between the lungs), or in the retroperitoneum (the back wall of the abdomen) (see Figure 4 below).
Extragonadal germ cell tumors can be benign (noncancer) or malignant (cancer) 33:
- Benign extragonadal germ cell tumors are called benign teratomas. These are more common than malignant extragonadal germ cell tumors and often are very large.
- Malignant extragonadal germ cell tumors are divided into two types, nonseminoma and seminoma. Nonseminomas tend to grow and spread more quickly than seminomas. They usually are large and cause signs and symptoms. If untreated, malignant extragonadal germ cell tumors may spread to the lungs, lymph nodes, bones, liver, or other parts of the body.
Risk factors for malignant extragonadal germ cell tumors include the following 33:
- Being male.
- Being age 20 or older.
- Having Klinefelter syndrome.
- Having Turner syndrome.
Figure 4. Extragonadal germ cell tumor
[Source 33 ]Extragonadal germ cell tumor symptoms
Signs and symptoms of extragonadal germ cell tumors include breathing problems and chest pain. Malignant extragonadal germ cell tumors may cause signs and symptoms as they grow into nearby areas. Check with your doctor if you have any of the following:
- Chest pain.
- Breathing problems.
- Cough.
- Fever.
- Headache.
- Change in bowel habits.
- Feeling very tired.
- Trouble walking.
- Trouble in seeing or moving the eyes.
Extragonadal germ cell tumor diagnosis
The following tests and procedures may be used to diagnose extragonadal germ cell tumors:
- Physical exam and health history: An exam of the body to check general signs of health, including checking for signs of disease, such as lumps or anything else that seems unusual. The testicles may be checked for lumps, swelling, or pain. A history of the patient’s health habits and past illnesses and treatments will also be taken.
- Chest x-ray: An x-ray of the organs and bones inside the chest. An x-ray is a type of energy beam that can go through the body and onto film, making a picture of areas inside the body.
- Serum tumor marker test: A procedure in which a sample of blood is examined to measure the amounts of certain substances released into the blood by organs, tissues, or tumor cells in the body. Certain substances are linked to specific types of cancer when found in increased levels in the blood. These are called tumor markers. The following three tumor markers are used to detect extragonadal germ cell tumor:
- Alpha-fetoprotein (AFP).
- Beta-human chorionic gonadotropin (beta-hCG).
- Lactate dehydrogenase (LDH).
- Blood levels of the tumor markers help determine if the tumor is a seminoma or nonseminoma.
- CT scan (CAT scan): A procedure that makes a series of detailed pictures of areas inside the body, taken from different angles. The pictures are made by a computer linked to an x-ray machine. A dye may be injected into a vein or swallowed to help the organs or tissues show up more clearly. This procedure is also called computed tomography, computerized tomography, or computerized axial tomography. Sometimes a CT scan and a PET scan are done at the same time. A PET scan is a procedure to find malignant tumor cells in the body. A small amount of radioactive glucose (sugar) is injected into a vein. The PET scanner rotates around the body and makes a picture of where glucose is being used in the body. Malignant tumor cells show up brighter in the picture because they are more active and take up more glucose than normal cells do. When a PET scan and CT scan are done at the same time, it is called a PET-CT.
- Biopsy: The removal of cells or tissues so they can be viewed under a microscope by a pathologist to check for signs of cancer. The type of biopsy used depends on where the extragonadal germ cell tumor is found.
- Excisional biopsy: The removal of an entire lump of tissue.
- Incisional biopsy: The removal of part of a lump or sample of tissue.
- Core biopsy: The removal of tissue using a wide needle.
- Fine-needle aspiration (FNA) biopsy: The removal of tissue or fluid using a thin needle.
After an extragonadal germ cell tumor has been diagnosed, tests are done to find out if cancer cells have spread to other parts of the body.
Extragonadal germ cell tumor treatment
There are different types of treatment for patients with extragonadal germ cell tumors. Some treatments are standard (the currently used treatment), and some are being tested in clinical trials.
There are currently 3 types of standard treatment used to treat patients with extragonadal germ cell tumors:
- Radiation therapy. Radiation therapy is a cancer treatment that uses high-energy x-rays or other types of radiation to kill cancer cells or keep them from growing. The way the radiation therapy is given depends on the type and stage of the cancer being treated. There are two types of radiation therapy:
- External radiation therapy uses a machine outside the body to send radiation toward the area of the body with cancer. External radiation therapy is used to treat seminoma.
- Internal radiation therapy uses a radioactive substance sealed in needles, seeds, wires, or catheters that are placed directly into or near the cancer.
- Chemotherapy. Chemotherapy is a cancer treatment that uses drugs to stop the growth of cancer cells, either by killing the cells or by stopping them from dividing. When chemotherapy is taken by mouth or injected into a vein or muscle, the drugs enter the bloodstream and can reach cancer cells throughout the body (systemic chemotherapy). When chemotherapy is placed directly in the cerebrospinal fluid, an organ, or a body cavity such as the abdomen, the drugs mainly affect cancer cells in those areas (regional chemotherapy). The way the chemotherapy is given depends on the type and stage of the cancer being treated.
- Surgery. Patients who have benign tumors or tumor remaining after chemotherapy or radiation therapy may need to have surgery.
As you go through treatment, you will have follow-up tests or check-ups. Some tests that were done to diagnose or stage the cancer may be repeated to see how well the treatment is working. Decisions about whether to continue, change, or stop treatment may be based on the results of these tests.
Some of the tests will continue to be done from time to time after treatment has ended. The results of these tests can show if your condition has changed or if the cancer has recurred (come back).
After initial treatment for extragonadal germ cell tumors, blood levels of alpha-fetoprotein (AFP), beta-human chorionic gonadotropin (beta-hCG) and lactate dehydrogenase (LDH) are continue to be checked to find out how well the treatment is working.
Treatment of extragonadal germ cell tumors that are recurrent (come back after being treated) or refractory (do not get better during treatment) may include the following:
- Chemotherapy.
- A clinical trial of high-dose chemotherapy with stem cell transplant. High-dose chemotherapy with stem cell transplant is being studied in clinical trials. For some patients, taking part in a clinical trial may be the best treatment choice. Clinical trials are done to find out if new cancer treatments are safe and effective or better than the standard treatment. Patients can enter clinical trials before, during, or after starting their cancer treatment. In high-dose chemotherapy with stem cell transplant, high doses of chemotherapy are given to kill cancer cells. Healthy cells, including blood-forming cells, are also destroyed by the cancer treatment. Stem cell transplant is a treatment to replace the blood-forming cells. Stem cells (immature blood cells) are removed from the blood or bone marrow of the patient or a donor and are frozen and stored. After the patient completes chemotherapy, the stored stem cells are thawed and given back to the patient through an infusion. These reinfused stem cells grow into (and restore) the body’s blood cells.
- A clinical trial of a new treatment.
Extragonadal germ cell tumor prognosis
Good prognosis
- Nonseminoma extragonadal germ cell tumor is in the good prognosis group if:
- the tumor is in the back of the abdomen; and
- the tumor has not spread to organs other than the lungs; and
- the levels of tumor markers alpha-fetoprotein (AFP) and beta-human chorionic gonadotropin (beta-hCG) are normal and lactate dehydrogenase (LDH) is slightly above normal.
- Seminoma extragonadal germ cell tumor is in the good prognosis group if:
- the tumor has not spread to organs other than the lungs; and
- the level of alpha-fetoprotein (AFP) is normal; beta-human chorionic gonadotropin (beta-hCG) and lactate dehydrogenase (LDH) may be at any level.
Intermediate prognosis
- Nonseminoma extragonadal germ cell tumor is in the intermediate prognosis group if:
- the tumor is in the back of the abdomen; and
- the tumor has not spread to organs other than the lungs; and
- the level of any one of the tumor markers (AFP, beta-hCG, or LDH) is more than slightly above normal.
- Seminoma extragonadal germ cell tumor is in the intermediate prognosis group if:
- the tumor has spread to organs other than the lungs; and
- the level of alpha-fetoprotein (AFP) is normal; beta-human chorionic gonadotropin (beta-hCG) and lactate dehydrogenase (LDH) may be at any level.
Poor prognosis
- Nonseminoma extragonadal germ cell tumor is in the poor prognosis group if:
- the tumor is in the chest; or
- the tumor has spread to organs other than the lungs; or
- the level of any one of the tumor markers (AFP, beta-hCG, or LDH) is high.
- Seminoma extragonadal germ cell tumor does not have a poor prognosis group.
Mediastinal seminoma cancer
Seminomas grow relatively slowly and can become very large before causing symptoms 20. Mediastinal seminoma cancer can grow up to 30 cm in diameter with minimal symptom 20. Approximately 20 to 30% of mediastinal seminomas are detected by routine chest X-ray while still asymptomatic 34. The most common initial symptom of mediastinal seminoma is a sensation of pressure or dull retrosternal chest pain 20. Additional symptoms include exertional shortness of breath (dyspnea), cough, difficulty swallowing foods or liquids (dysphagia), and hoarseness. Superior vena caval syndrome develops in approximately 10% of patients 20. Systemic symptoms related to metastatic lesions are uncommon.
At the time of diagnosis, only 30 to 40% of patients with mediastinal seminoma have localized disease; the remainder have one or more sites of distant metastases 35, 36. The lungs and other intrathoracic structures are the most common metastatic sites. The skeletal system is the most frequently involved extrathoracic metastatic site; the propensity of advanced testicular seminoma to metastasize to bone has also been recognized. The retroperitoneum is an uncommon site of metastasis in patients with mediastinal seminoma 37, 38, 35.
Pure seminoma appears radiographically as a large, noncalcified anterior mediastinal mass, which can compress or deviate the trachea or bronchi if of sufficient size 20. A computed tomography (CT) scan of the chest typically shows a large homogeneous anterior mediastinal mass that obliterates the fat planes surrounding mediastinal vascular structures 39. The radiographic findings are not specific enough to allow the distinction of mediastinal seminoma from other mediastinal tumors.
Elevated serum levels of human chorionic gonadotropin (hCG) are detected in approximately 10% of mediastinal seminomas 35. This incidence is similar to that reported in advanced testicular seminoma 20. Levels of hCG exceeding 100 ng/mL are unusual, and suggest the presence of nonseminomatous elements 20. The serum alpha-fetoprotein (AFP) level is always normal in pure mediastinal seminoma, and any elevation of alpha-fetoprotein (AFP) tumor marker indicates the presence of nonseminomatous elements 20. Serum lactate dehydrogenase (LDH) is also elevated in the majority of patients with mediastinal seminoma 35.
Mediastinal seminoma cancer treatment
Pure mediastinal seminomas are curable in the large majority of patients, even when metastatic at the time of diagnosis 20. Mediastinal seminomas are highly sensitive to radiation therapy and to combination chemotherapy, and selection of treatment therefore depends on disease stage and size of mediastinal tumor 20.
Approximately 20% of mediastinal seminomas are diagnosed after a chest radiograph reveals an asymptomatic anterior mediastinal mass 20. Some of these patients have relatively small tumors, and a complete surgical resection can be easily accomplished at the time of surgical biopsy for diagnosis 20. Although surgical resection alone is curative in some of these patients, a course of postoperative radiation therapy to the mediastinum should always be administered in order to prevent local recurrence 40, 41, 42. Because other highly effective treatment modalities exist, extensive surgical procedures for resection or debulking of large mediastinal seminomas are contraindicated 20.
The large majority of patients with mediastinal seminoma (at least 80%) are not candidates for surgical resection because of the large size of the mediastinal primary tumor or the presence of distant metastases 20. Pure mediastinal seminomas share the radiosensitivity of testicular seminoma, and primary radiation therapy is often curative in these tumors 20. Although most reported series are relatively small, approximately 60% of patients achieve long-term disease-free survival following mediastinal irradiation 35, 41, 43, 44, 45. Most treatment failures are a result of the appearance of distant metastases, rather than a result of inadequate local tumor control. The majority of patients who relapse after radiation therapy can be salvaged with subsequent chemotherapy.
Highly effective systemic combination chemotherapy now offers the best option for curative treatment of patients with mediastinal seminoma. When used in advanced testicular seminoma, intensive cisplatin-based regimens are at least as active as they are against nonseminomatous germ cell tumors. Even with bulky local tumors and frequent metastatic disease, all recent series have shown cure rates of > 80% with initial cisplatin-based chemotherapy 20.
Patients with bulky seminoma at any site frequently have residual radiographic abnormalities after chemotherapy 20. In most patients, these masses represent dense scirrhous reactions (production of connective tissue stroma with lots of collagen by a neoplasm) rather than viable seminoma or benign teratoma 46, 47, 48. Because of the dense fibrosis, retroperitoneal node dissection in such patients is difficult, is frequently incomplete, and can be associated with high mortality. When residual lesions are less than 3 cm in maximum diameter, residual active tumor is rare, and patients should be followed with serial chest CT scans 20. Residual seminoma becomes more frequent when residual masses are > 3 cm, and biopsy should be considered 49. If immediate biopsy is not performed, these patients should be monitored very closely (ie, CT scans every 2 months during the first year), with early biopsy of any enlarging mass on chest radiograph or chest CT 20.
In summary, most patients with mediastinal seminoma can be cured with surgery to remove the tumor followed by radiation therapy and chemotherapy, and all patients should be approached with this intent 20. Patients with small tumors (usually asymptomatic) that appear resectable should undergo thoracotomy and attempted complete resection 20. Radical debulking procedures for patients with larger tumors are not indicated. In the subset of patients who undergo complete excision, postoperative radiotherapy (4,000 to 4,500 cGy) is curative in almost all patients and is the treatment of choice 20. All other patients should receive initial cisplatin-based chemotherapy, unless they have a specific medical contraindication to such therapy. In such patients with localized tumors in the mediastinum, radiation therapy is an acceptable alternative. Optimal chemotherapy includes four courses of bleomycin, etoposide, and cisplatin, as is recommended for poor-prognosis testicular germ cell tumors 28.
Non seminoma testicular cancer
Nonseminoma testicular cancers tend to happen earlier in life. Nonseminoma testicular cancer grows and spreads quickly. Several types of nonseminomas exist with variable appearance and prognosis. There are four main types of non-seminoma germ cell tumor that can appear alone, but most often appear as a “mixed” non seminoma germ cell tumor, with more than one type present:
- Embryonal carcinoma: present in about 40 percent of tumors and among the most rapidly growing and potentially aggressive tumor types. Embryonal carcinoma can secrete human chorionic gonadotropin (hCG) or alpha fetoprotein (AFP).
- Yolk sac carcinoma: the most common type of germ cell tumor in children; responds well to chemotherapy in children and adults. Yolk sac tumors almost always secrete alpha fetoprotein (AFP)
- Choriocarcinoma: very rare and very aggressive form of testicular cancer. Can secrete hCG.
- Teratoma: most often appear as a mixed non seminoma germ cell tumor; usually grow locally but can appear in retroperitoneal lymph nodes. Teratoma is chemotherapy- and radiation-resistant and best treated with surgical removal.
Seminoma cancer causes
Testicular seminoma is a germ cell tumor originating from the seminiferous tubules, due to malignant transformation of primordial germ cells 1. The exact molecular genetic derangements underlying this transformation are not clearly understood, but the most common genetic finding is the gain of genetic material from chromosome 12p 50, 51. Some of the mutations noticed in germ cell tumors include BRAF, KIT, KRAS, NRAS, and TP53, although single-gene mutations are relatively uncommon 52.
Nearly all testicular cancers begin in the germ cells 53. The germ cells in the testicle make sperm. Scientists aren’t sure what causes seminomas and germ cell tumors 1.
Normal germ cells form in a developing human embryo. These cells eventually travel to the embryo’s ovaries or testicles, becoming egg cells or sperm cells. In contrast, germ cell tumors consist of cells that don’t develop into fully formed eggs or sperm. The germ cells divide abnormally and become a tumor in your ovaries or testicles instead. In the case of extragonadal tumors, the germ cells travel to odd places in your body — like your chest, brain, belly, low back and tailbone — to form tumors.
The following factors are associated with an increase in the risk of seminoma 1:
- History of undescended testicle (cryptorchidism): Risk of seminoma increases with the history of cryptorchidism. There is 10 to 40 times higher risk in patients with an undescended testis, 10% of the patients with cryptorchidism develop germ cell tumor 54. An abdominal testis usually develops seminoma while a testis surgically brought to the scrotum by orchiopexy is a non-seminomatous germ cell tumor.
- Environmental exposure: Exposure to chemical compounds like organochlorines, polychlorinated biphenyls, polyvinyl chlorides, phthalates, marijuana, and tobacco is associated with an increased risk of seminoma or other germ cell tumors 55, 56.
- Infections: History of mumps viral infection is related to increased risk of germ cell tumors 57.
- Other factors include trauma, maternal estrogen exposure, family history of testicular tumors, intersex syndromes (insensitive androgen syndrome and gonadal dysgenesis), and history of cancer in the other testicle 58.
- Genetics: Genetic changes in the form of amplification and deletions are seen in chromosome arm 12p11.2-p12.1 chromosomal regions 50, 51. Coffey and colleagues demonstrated that only seminomas contain activating mutations of the KIT gene 59.
Risk factors for seminoma testicular cancer
Anything that increases your chance of getting a disease is called a risk factor. Factors that may increase your risk of testicular cancer include 53:
- Having an undescended testicle (cryptorchidism). The testes form in the belly during fetal development. They typically descend into the scrotum before birth. If you have a testicle that never descended, your risk of testicular cancer is higher. The risk is increased even if you’ve had surgery to move the testicle to the scrotum.
- Having a family history (especially in a father or brother) of testicular cancer. If testicular cancer runs in your family, you might have an increased risk.
- Personal history of testicular cancer
- Having had abnormal development of the testicles.
- Being a young adult. Testicular cancer can happen at any age. But it’s most common in teens and young adults between 15 and 35.
- Being white. Testicular cancer is most common in white people.
- Men with HIV or AIDS are reported to be at increased risk of developing testicular seminomas 60. But most cases of testicular cancer are not linked to being HIV positive. You usually have antiviral drugs to treat HIV/AIDS. Some evidence suggests that these drugs cancel the increased risk linked with HIV infection.
The most common risk factor for testis cancer is a history of undescended testicle or cryptorchidism. Normally in the developing male fetus, the testicles form near the kidneys in the abdomen (belly). About the eighth month of pregnancy, the testicles descend, exit the body and settle in the scrotum. About 3% of boys have one or both testicles that fail to make it into the scrotum. Testicles can settle in the abdomen or in the inguinal canal or groin where the testicle exits the body wall and enters the scrotum. Most of the time, an undescended testicle will move down and settle into the scrotum within the first year of life. Sometimes surgery is required to bring down and fix the testicle to the scrotum, this surgery is called an orchiopexy.
Boys with a history of cryptorchidism have an increased risk of testicular cancer. The risk of testicular cancer is not directly related to the fact that the testicle does not descend, but it is believed that the abnormality in descent likely indicates an abnormality in the testicle that makes cancer more likely. This belief is based on the following observations: The testicular cancer usually develops in the undescended testicle (four- to sixfold increased risk of cancer), but the risk of cancer is also higher in the normal testicle (less than twofold increased risk). In addition, generally the higher the testicle, the higher the risk of testicular cancer — intra-abdominal testis have a much higher risk of cancer than those in the inguinal canal. Early surgery (orchiopexy) reduces the risk of testis cancer (two- to threefold risk if the surgery is performed prior to puberty) but does not erase the chance for that boy to develop testicular cancer later in life.
Testicular germ-cell tumors is associated with cryptorchidism, hypospadias and decreased fertility is often referred to as the testicular dysgenesis syndrome 61. In utero exposure to endocrine disruption chemicals might increase the likelihood of testicular dysgenesis syndrome 62. Among these chemicals, organochlorine insecticides have been demonstrated to increase the risk of testicular germ-cell tumor 63.
Furthermore, a family history of testicular cancer is another common risk factor, with an eight- to twelvefold risk if a man has a brother with testicular cancer and a two- to fourfold risk if his father has testicular cancer. While there is not a specific gene linked to testicular cancer, the cancer is highly heritable and can be passed from generation to generation. In addition, the average age at diagnosis is two to three years younger than the general population if a first-degree relative has testicular cancer. However, it should be remembered that testicular cancer is rare, and it is therefore rare for this cancer to run in families.
Men with a personal history of testicular cancer have the highest risk of developing another cancer. Fortunately, only 2% of men will develop cancer in both testicles, but that risk is twelvefold higher than men without testis cancer. In addition, men who develop testis cancer in their 20s or earlier, men with seminoma and men with germ cell neoplasia is situ formerly known as carcinoma in situ (CIS) or intratubular germ cell neoplasia (ITGCN) have a higher risk of developing a second testis cancer.
Most testis cancer arises from the precursor lesion known as germ cell neoplasia is situ (GCNIS). Germ cell neoplasia is situ (GCNIS) is present adjacent to testis cancer in 80–90% of patients. For men in whom germ cell neoplasia is situ (GCNIS) is found for other reasons, the risk of subsequent testis cancer is 50% at five years and 70% at seven years. Therefore, germ cell neoplasia is situ (GCNIS) is the last well-known risk factor for testis cancer.
Microlithiasis or small calcifications (stones) in the testicle found on ultrasound, was once believed to be a risk factor for testicular cancer. Microlithiasis is not a risk factor for testicular cancer for most men; however, if one of the other risk factors (above) exists, microlithiasis may indicate a higher risk of cancer and warrants monthly testicular self-examination and routine follow-up with a doctor.
Seminoma cancer symptoms
Seminoma testicular cancer usually only affects one testicle, but it can affect both.
Signs and symptoms of testicular cancer include:
- a lump or swelling in your testicle, but it can affect both testicles (>85% of men)
- your testicle getting bigger
- an ache or pain in your testicle or scrotum (the skin that covers the testicles) (about 20% to 30% of men experience a heavy dragging feeling or general ache)
- your scrotum feeling heavy, firm or hard
Other symptoms can include:
- a dull ache or pain in your back, groin or lower tummy
- back pain
- sudden swelling in the scrotum
- losing weight without trying
- a cough
- difficulty breathing or swallowing
- enlargement or tenderness of the breast tissue
- A small percentage present with symptoms of metastatic disease and infertility.
Most testicular cancers present as a mass confined to the one testicle, but it can affect both. Therefore, the most common presentation is a painless testicular mass. Most of these masses can be felt and of significant size (a few to several centimeters). Small, nonpalpable lesions without pain and in the absence of distant disease have a higher likelihood of being a benign tumor. In a number of studies, upwards of 80 percent of nonpalpable, asymptomatic masses that are 2 cm or smaller will be benign tumors. Benign lesions may include testicular cysts, varicocele, small infarcts or small Leydig cell or Sertoli cell tumors.
Serious, acute pain is associated with rapidly growing tumors and associated bleeding or infarction (if the tumor outgrows its blood supply). Most patients with pain complain of dull scrotal discomfort or heaviness. Rarely, trauma can lead to a diagnosis, mostly because it brings a mass or pain to the patient’s awareness.
For the upwards of 30 percent of men who present with metastatic cancer, symptoms of metastases can be the presenting complaint. Bulky retroperitoneal lymphadenopathy (enlarged lymph nodes) can lead to abdominal mass; abdominal, flank or back pain due to direct invasion or obstruction of muscles, blood vessels or the ureters; lower extremity swelling if the inferior vena cava (IVC) is compressed or gastrointestinal symptoms if the intestines are involved. Lung metastases can present as chest pain, shortness of breath and cough.
As testis cancers can lead to diminished spermatogenesis (sperm production), rarely infertility can be the initial presentation in men with testicular cancer.
Seminoma cancer diagnosis
You might find lumps, swelling or other symptoms of testicular cancer on your own. Testicular cancers can be detected during an exam by a doctor too. You’ll need other tests to see if testicular cancer is causing your symptoms.
Tests used to diagnose testicular cancer include:
- Testicular ultrasound (scrotal ultrasound). A testicular ultrasound test uses sound waves to make pictures. It can be used to make pictures of the scrotum and testicles. During an ultrasound you lie on your back with your legs spread. A doctor puts a clear gel on the scrotum. A hand-held probe is moved over the scrotum to make the pictures. Ultrasound gives your doctor more clues about any lumps around the testicle. It can help your doctor see whether the lumps look like something that isn’t cancer or if they look like cancer. An ultrasound shows whether the lumps are inside or outside the testicle. Lumps inside the testicle are more likely to be testicular cancer. Radical orchiectomy (surgery to remove the testicle) should strongly be considered for any intratesticular mass and suspicion of testis cancer.
- Serum testicular tumor markers. A blood test can detect proteins made by testicular cancer cells. This type of test is called a tumor marker test. Tumor markers for testicular cancer include beta-human chorionic gonadotropin (hCGβ), alpha-fetoprotein (AFP) and lactate dehydrogenase (LDH). Having these substances in your blood doesn’t mean you have cancer. Having levels higher than is typical is a clue your doctor uses to understand what’s going on in your body.
- Surgery to remove a testicle through an incision in the groin (Inguinal orchiectomy). If your doctor thinks a lump on your testicle may be cancerous, you might have surgery to remove the testicle through an incision in the groin. NOTE: The surgeon does not cut through the scrotum into the testicle to remove a sample of tissue for biopsy, because if cancer is present, this procedure could cause it to spread into the scrotum and lymph nodes. It’s important to choose a surgeon who has experience with this kind of surgery. The testicle is sent to a lab for testing. A tissue sample from the testicle is then viewed under a microscope to check for cancer cells. If cancer is found, the cell type (seminoma or nonseminoma) is determined in order to help plan treatment.
- Advanced imaging. Additional imaging can be performed before or after the diagnosis of cancer is confirmed, based on the strength of suspicion for cancer. Imaging of the chest, abdomen and pelvis are typically required to evaluate for spread of testicular cancer — this process is called staging. CT, MRI and X-ray can be used for staging. PET scan or bone scan are not recommended for the routine evaluation of testicular cancer.
Histological findings
Most commonly, there is a diffuse arrangement of pale cells that is interrupted by fibrovascular septa containing lymphocytes 64. The tumor cells characteristically have pale to clear cytoplasm, with crisp cytoplasmic membranes and polygonal nuclei with finely granular chromatin and frequently flattened edges 64. One or more large, centrally located nucleoli are present. The abundant cytoplasm results in relatively evenly spaced, non-overlapping nuclei in most cases. The cytoplasmic clarity is attributable to abundant glycogen particles demonstrable with the periodic acid-Schiff stain. Less commonly, the cytoplasm is denser, and the nuclei more crowded. This may result in a plasmacytoid appearance. A variably prominent lymphocytic infiltrate occurs in almost every case and a granulomatous reaction in more than half. Approximately 10-20% of tumors contain admixed syncytiotrophoblast cells that vary in prominence from widely scattered to prominent aggregates 65.
Immunohistochemical findings
Seminomas stain for antigens characteristic of immature, fetal-type germ cells (gonocytes), including placental alkaline phosphatase (86-95%; cytoplasmic membrane), KIT (90-100%; cytoplasmic membrane), OCT3/4 (100%; nuclear), SALL4 (100%; nuclear), and SOX17 (95%; nuclear) 64. Podoplanin is also positive (100%; cytoplasmic membrane). Cytokeratin AE1/AE3 immunoreactivity varies (20-36%), but is often negative or stains the cytoplasm of only a minority of tumor cells, often in a para nuclear dot-like pattern. CD30 is characteristically negative, as is epithelial membrane antigen (2%). Stains for alpha-fetoprotein are always negative 64.
Serum tumor markers
Alpha-fetoprotein (AFP), beta-human chorionic gonadotropin (beta-hCG), and lactate dehydrogenase (LDH) play an important role as serum tumor markers in the staging and monitoring of germ cell tumors and should be measured prior to removing the involved testicle 66. For patients with nonseminomas, one of the most significant predictors of prognosis is the degree of tumor-marker elevation after the cancerous testicle has been removed 7. Elevated levels of serum tumor markers are often the earliest sign of relapse (recurrence), making these markers useful for monitoring all stages of nonseminomas and metastatic seminomas 26.
Significant and unambiguously rising levels of alpha-fetoprotein (AFP) and/or beta-human chorionic gonadotropin (beta-hCG) signal relapsed germ cell tumor in most cases and are an indication for treatment even in the absence of radiological evidence of metastatic disease 26. However, tumor marker elevations need to be interpreted with caution. For example, false-positive beta-hCG levels can result from cross reactivity of the assay with luteinizing hormone (LH) in which case an intramuscular injection of testosterone should result in normalization of beta-hCG values 26. There are also clinical reports of marijuana use resulting in elevations of serum beta-hCG and some experts recommend querying patients about drug use and retesting beta-hCG levels after a period of abstinence from marijuana use 26. Similarly, AFP is chronically mildly elevated in some individuals for unclear reasons and can be substantially elevated by liver disease 26.
Alpha-fetoprotein (AFP)
Elevation of serum alpha-fetoprotein (AFP) is seen in 40% to 60% of men with nonseminomas. Seminomas do not produce alpha-fetoprotein (AFP). Men who have an elevated serum AFP have a mixed germ cell tumor (i.e., nonseminomatous germ cell tumors [NSGCT]) even if the pathology shows a pure seminoma—unless there is a more persuasive explanation for the elevated AFP, such as liver disease 26.
Beta-human chorionic gonadotropin (beta-hCG)
Elevation of beta-human chorionic gonadotropin (beta-hCG) is found in approximately 14% of patients with stage 1 pure seminomas before orchiectomy (surgery to remove the testicle) and in about one-half of patients with metastatic seminomas 67, 68, 69. Approximately 40% to 60% of men with nonseminomas have an elevated serum beta-hCG 26.
Lactate dehydrogenase (LDH)
Seminomas and nonseminomas alike may result in elevated lactate dehydrogenase (LDH) but such values are of unclear prognostic significance because LDH may be elevated in many conditions unrelated to cancer. A study evaluated the utility of lactate dehydrogenase (LDH) in 499 patients with a testicular germ cell tumor who were undergoing surveillance after orchiectomy or treatment of stage 2 or 3 disease. It found that 7.7% of patients had elevated lactate dehydrogenase (LDH) unrelated to cancer, while only 1.4% of patients had cancer-related increases in LDH 70. Among 15 patients with relapsed disease, LDH was elevated in six patients and was the first sign of relapse in one patient 70. Over 9% of the men had a persistent false-positive increase in LDH. The positive predictive value for an elevated LDH was 12.8% 70.
A second study reported that among 494 patients with stage 1 germ cell tumors who subsequently had a relapse, 125 had an elevated LDH at the time of relapse 71. Of these 125 patients, all had other evidence of relapse: 112 had a concurrent rise in AFP and/or beta-hCG, one had computed tomography (CT) evidence of relapse before the elevation in LDH, one had palpable disease on examination, and one complained of back pain that led to imaging that revealed retroperitoneal relapse 71. On one hand, measuring LDH appears to have little value for predicting relapse during surveillance of germ cell tumors. On the other hand, for patients with metastatic non-seminoma germ cell tumor (NSGCT), large studies of prognostic models have found the LDH level to be a significant independent predictor of survival 7, 27.
Testicular cancer screening
Some doctors recommend regular testicle self-exams. During a testicular self-exam you feel your testicles for any lumps or other changes. If you notice any changes that last longer than two weeks, make an appointment with your doctor.
Testicular cancer staging
Once your doctor confirms your diagnosis, the next step is to see whether the testicular cancer has spread beyond the testicle to other parts of your body. This is called the cancer’s stage. It helps your health care team understand your prognosis and how likely your cancer is to be cured.
The following tests and procedures may be used in the testicular cancer staging process:
- Chest x-ray: An x-ray of the organs and bones inside the chest. An x-ray is a type of energy beam that can go through the body and onto film, making a picture of areas inside the body.
- Computerized tomography (CT) scan also called computed tomography, computerized tomography, or computerized axial tomography. CT scans take a series of X-ray pictures of your belly, chest and pelvis. A dye may be injected into a vein or swallowed to help the organs or tissues show up more clearly. A doctor checks the pictures for signs that cancer has spread.
- MRI (magnetic resonance imaging): A procedure that uses a magnet, radio waves, and a computer to make a series of detailed pictures of areas inside the body, such as the abdomen. This procedure is also called nuclear magnetic resonance imaging (NMRI).
- Abdominal lymph node dissection: A surgical procedure in which lymph nodes in the abdomen are removed and a sample of tissue is checked under a microscope for signs of cancer. This procedure is also called lymphadenectomy. For patients with nonseminoma, removing the lymph nodes may help stop the spread of disease. Cancer cells in the lymph nodes of seminoma patients can be treated with radiation therapy.
- Serum testicular tumor markers. Tumor marker tests such as beta-human chorionic gonadotropin (beta-hCG), alpha-fetoprotein (AFP) and lactate dehydrogenase (LDH) are often repeated after surgery to remove the testicle. The results help your doctor decide whether you might need additional treatments to kill the cancer cells. Tumor marker tests might be used during and after cancer treatment to monitor your condition. Tumor marker levels are measured again, after inguinal orchiectomy and biopsy, in order to determine the stage of the cancer. This helps to show if all of the cancer has been removed or if more treatment is needed. Tumor marker levels are also measured during follow-up as a way of checking if the cancer has come back.
The stages of testicular cancer range from 0 to 3.
- Stage 0 and stage 1 testicular cancers only affect the testicle and the area around it. At these early stages, the cancer hasn’t spread to the lymph nodes or other parts of the body.
- Stage 2 testicular cancers have spread to the lymph nodes. When testicular cancer spreads to other parts of the body, it is stage 3. Not all stage 3 cancers have spread though.
- Stage 3 testicular cancers can also mean that the cancer is in the lymph nodes and the tumor marker results are very high.
Stage 0 testicular cancer (germ cell neoplasia in situ or testicular intraepithelial neoplasia)
Stage 0 testicular cancer is also called germ cell neoplasia in situ (GCNIS) or testicular intraepithelial neoplasia. In stage 0, abnormal cells are found in the tiny tubules where the sperm cells begin to develop. These abnormal cells may become cancer and spread into nearby normal tissue. All tumor marker levels are normal.
Around 5% of testicular cancer patients have germ-cell neoplasia in situ (GCNIS) in the other testis with the highest risk (∼30%) in men with testicular atrophy (volume <12 ml) and age <40 years 62. Approximately 30%-40% of patients with retroperitoneal extragonadal germ cell tumors (extragonadal germ cell tumor) harbor testicular germ-cell neoplasia in situ (intratubular germ cell neoplasia in situ) 72, 73, 74.
Stage 1 testicular cancer
Stage 1 testicular cancer is limited to the testis. Stage 1 testicular cancer is divided into stages 1A, 1B, and 1S.
In stage 1A, cancer is found in the testicle, including the rete testis, but has not spread to the blood vessels or lymph vessels in the testicle.
- All tumor marker levels such as beta-human chorionic gonadotropin (beta-hCG), alpha-fetoprotein (AFP) and lactate dehydrogenase (LDH) are normal.
In stage 1B, cancer:
- is found in the testicle, including the rete testis, and has spread to the blood vessels or lymph vessels in the testicle; or
- has spread into the hilar soft tissue (tissue made of fibers and fat with blood vessels and lymph vessels), the epididymis, or the outer membranes around the testicle; or
- has spread to the spermatic cord; or
- has spread to the scrotum.
- All tumor marker levels such as beta-human chorionic gonadotropin (beta-hCG), alpha-fetoprotein (AFP) and lactate dehydrogenase (LDH) are normal.
In stage 1S, cancer is found anywhere in the testicle and may have spread into the spermatic cord or scrotum. Tumor marker levels range from slightly above normal to high.
Stage 2 testicular cancer
Stage 2 testicular cancer involves the testis and the retroperitoneal or periaortic lymph nodes usually in the region of the kidney. Stage 2 testicular cancer is divided into stages 2A, 2B, and 2C.
In stage 2A, cancer is found anywhere in the testicle and may have spread into the spermatic cord or scrotum. Cancer has spread to 1 to 5 nearby lymph nodes and the lymph nodes are 2 centimeters or smaller.
- All tumor marker levels are normal or slightly above normal.
In stage 2B, cancer is found anywhere in the testicle and may have spread into the spermatic cord or scrotum. Cancer has spread to:
- 1 nearby lymph node and the lymph node is larger than 2 centimeters but not larger than 5 centimeters; or
- more than 5 nearby lymph nodes and the lymph nodes are not larger than 5 centimeters; or
- a nearby lymph node and the cancer has spread outside the lymph node.
- All tumor marker levels are normal or slightly above normal.
In stage 2C, cancer is found anywhere in the testicle and may have spread into the spermatic cord or scrotum. Cancer has spread to a nearby lymph node and the lymph node is larger than 5 centimeters.
- All tumor marker levels are normal or slightly above normal.
Stage 3 testicular cancer
Stage 3 testicular cancer has spread beyond the retroperitoneal nodes based on physical examination, imaging studies, and/or blood tests (i.e., patients with retroperitoneal adenopathy and highly elevated serum tumor markers are stage 3). Stage 3 testicular cancer is divided into stages 3A, 3B, and 3C.
In stage 3A, cancer is found anywhere in the testicle and may have spread into the spermatic cord or scrotum. Cancer may have spread to one or more nearby lymph nodes. Cancer has spread to distant lymph nodes or to the lungs.
- All tumor marker levels are normal or slightly above normal.
In stage 3B, cancer is found anywhere in the testicle and may have spread into the spermatic cord or scrotum. Cancer has spread:
- to one or more nearby lymph nodes and has not spread to other parts of the body; or
- to one or more nearby lymph nodes. Cancer has spread to distant lymph nodes or to the lungs.
- The level of one or more tumor markers is moderately above normal.
In stage 3C, cancer is found anywhere in the testicle and may have spread into the spermatic cord or scrotum. Cancer has spread:
- to one or more nearby lymph nodes and has not spread to other parts of the body; or
- to one or more nearby lymph nodes. Cancer has spread to distant lymph nodes or to the lungs.
- The level of one or more tumor markers is high.
OR
- Cancer is found anywhere in the testicle and may have spread into the spermatic cord or scrotum. Cancer has not spread to distant lymph nodes or the lung, but has spread to other parts of the body, such as the liver or bone.
- Tumor marker levels may range from normal to high.
Seminoma cancer treatment
Testicular cancer treatment options depend on the following:
- Whether the tumor is nonseminoma or seminoma.
- The size of the tumor and where it is in the body.
- The blood levels of alpha-fetoprotein (AFP), beta-human chorionic gonadotropin (hCGβ), and lactate dehydrogenase (LDH).
- Whether the tumor has spread to other parts of the body.
- The way the tumor responds to initial treatment.
- Whether the tumor has just been diagnosed or has recurred (come back).
Testicular cancer treatment often involves surgery and chemotherapy. Which treatment options are best for you depends on the type of testicular cancer you have and its stage. Your cancer treatment team will also considers your overall health and your preferences.
Generally, testicular seminoma treatment plans are as follows 13, 14, 15:
- Stage 1 testicular cancer: For patients with stage 1 seminoma, orchiectomy is usually curative 16, 17. Options for post-orchiectomy management include surveillance alone or adjuvant chemotherapy with one single infusion of carboplatin or prophylactic radiotherapy (declining interest).
- Stage 2 testicular cancer: Following radical inguinal orchiectomy, the treatment of stage 2 testicular seminoma depends on the extent of the lymph node involvement. Radiation therapy with or without cisplatin-based chemotherapy is recommended.
- Stage 3 testicular cancer: For stage 3 testicular seminomas, chemotherapy with bleomycin, etoposide, and cisplatin (BEP) or etoposide and cisplatin (EP) is preferred. Radiotherapy may be indicated in select cases 18. In patients with an intermediate prognosis, it might be hard to tolerate bleomycin, and therefore the addition of ifosfamide to etoposide and cisplatin (VIP) is reasonable 19.
After treatment patient requires life long follow up. Surveillance includes the following, with the frequency determined by the disease stage and duration of follow up.
- History and physical examination
- Serum tumor markers ( beta-hCG, LDH, AFP)
- Chest radiography
- CT scan of the abdomen, with or without CT scan of the pelvis
Surgery
Surgery to remove the testicle (inguinal orchiectomy) and some of the lymph nodes may be done at diagnosis and staging. Tumors that have spread to other places in the body may be partly or entirely removed by surgery.
Operations used to treat testicular cancer include:
- Surgery to remove the testicle also called a radical inguinal orchiectomy. It’s the first treatment for most testicular cancers. To remove the testicle, a surgeon makes a cut in the groin. The entire testicle is pulled out through the opening. A prosthetic, gel-filled testicle can be inserted if you choose. This might be the only treatment needed if the cancer hasn’t spread beyond the testicle.
- Surgery to remove nearby lymph nodes. If there’s concern that your cancer may have spread beyond your testicle, you might have surgery to remove some lymph nodes. To remove the lymph nodes, the surgeon makes a cut in the belly. The lymph nodes are tested in a lab to look for cancer. Surgery to remove lymph nodes is often used to treat the nonseminoma type of testicular cancer.
Radical inguinal orchiectomy is the standard procedure for diagnostic and therapeutic purposes. Radical inguinal orchiectomy surgery involves removing the testicle and spermatic cord where it exits the body to identify and likely treat the majority of cancers localized to the testis. Trans scrotal orchiectomy or biopsy of the testicular mass is contraindicated for the risk of tumor seeding of the lymphatic drainage. Spinal or general anesthesia may be used. An inguinal incision is made to expose the external and internal iliac canal. External iliac fascia is opened, revealing the spermatic cord. The spermatic cord is controlled to stop retroperitoneal lymphatic and venous drainage of tumor cells. After that, deliver the testis from the scrotum and ligate vas deferens and spermatic arteries separately. Retroperitoneal lymph node dissection is done if necessary. Reapproximate the external oblique fascia and close the skin in standard fashion. Conduct a follow-up study by staging and referring the patient for appropriate adjuvant therapies.
After the doctor removes all the cancer that can be seen at the time of the surgery, some patients may be given chemotherapy or radiation therapy after surgery to kill any cancer cells that are left. Treatment given after the surgery, to lower the risk that the cancer will come back, is called adjuvant (add-on) therapy.
Testicular cancer surgery carries a risk of bleeding and infection. If you have surgery to remove lymph nodes, there’s also a risk that a nerve might be cut. Surgeons take great care to protect the nerves. Sometimes cutting a nerve can’t be avoided. This can lead to problems with ejaculating, but it generally doesn’t affect your ability to get an erection. Ask your surgeon about options for preserving your sperm before surgery.
Ilioinguinal nerve injury can occur if the nerve is damaged during dissection of the spermatic cord. This is more common in men who underwent prior inguinal surgery (usually for an undescended testicle or hernia repair) and can occur during dissection or be inadvertently trapped in the closure of the external oblique fascia. The deficit is often decreased sensation to the medial thigh, scrotum or base of the penis. It is often transient, but can take several weeks or months to improve.
Inguinal hernia can occur if the external oblique fascia is not closed properly or if the closure breaks down. It is important to minimize strenuous activities for two to four weeks to prevent development of a hernia.
Chemotherapy
Chemotherapy treatment uses chemo drugs to kill cancer cells. Chemotherapy travels throughout the body. It can kill cancer cells that may have spread beyond the testicle. Chemotherapy is often used after surgery. It can help kill any cancer cells that are still in the body. When testicular cancer is very advanced, sometimes chemotherapy is used before surgery.
Side effects of chemotherapy depend on the specific medicines being used. Common side effects include fatigue, hearing loss and an increased risk of infection.
Chemotherapy also may cause your body to stop making sperm. Often, sperm production starts again as you get better after cancer treatment. But sometimes losing sperm production is permanent. Ask your doctor about your options for preserving your sperm before chemotherapy.
Radiation therapy
Radiation therapy uses high-powered energy beams to kill cancer cells. The radiation can come from X-rays, protons and other sources. During external radiation therapy, you’re positioned on a table and a large machine moves around you. The machine points the energy beams at precise points on your body.
Radiation therapy is sometimes used to treat the seminoma testicular cancer. Radiation therapy may be recommended after surgery to remove your testicle.
Radiation therapy typically isn’t used to treat the nonseminoma testicular cancer.
Side effects may include nausea and fatigue. Radiation therapy also can temporarily lower sperm counts. This can affect your fertility. Ask your health care provider about your options for preserving your sperm before radiation therapy.
Immunotherapy
Immunotherapy is treatment with medicine that helps your body’s immune system kill cancer cells. Your immune system fights off diseases by attacking germs and other cells that shouldn’t be in your body. Cancer cells survive by hiding from the immune system. Immunotherapy helps the immune system cells find and kill the cancer cells.
Immunotherapy is sometimes used for advanced testicular cancer 75. It might be an option if the cancer doesn’t respond to other treatments.
Stage 0 testicular cancer treatment
Treatment of stage 0 testicular cancer may include the following:
- Radiation therapy.
- Surveillance.
- Surgery to remove the testicle.
Stage 1 testicular cancer treatment
Treatment of stage 1 testicular cancer depends on whether the cancer is a seminoma or a nonseminoma.
Treatment of seminoma testicular cancer may include the following:
- Surgery to remove the testicle, followed by surveillance.
- For patients who want active treatment rather than surveillance, treatment may include:
- Surgery to remove the testicle, followed by chemotherapy.
Treatment of nonseminoma testicular cancer may include the following:
- Surgery to remove the testicle, with long-term follow-up.
- Surgery to remove the testicle and lymph nodes in the abdomen, with long-term follow-up.
- Surgery followed by chemotherapy for patients at high risk of recurrence, with long-term follow-up.
Stage 2 testicular cancer treatment
Treatment of stage 2 testicular cancer depends on whether the cancer is a seminoma or a nonseminoma.
Treatment of seminoma testicular cancer may include the following:
- When the tumor is 5 centimeters or smaller:
- Surgery to remove the testicle, followed by radiation therapy to lymph nodes in the abdomen and pelvis.
- Combination chemotherapy.
- Surgery to remove the testicle and lymph nodes in the abdomen.
- When the tumor is larger than 5 centimeters:
- Surgery to remove the testicle, followed by combination chemotherapy or radiation therapy to lymph nodes in the abdomen and pelvis, with long-term follow-up.
Treatment of nonseminoma testicular cancer may include the following:
- Surgery to remove the testicle and lymph nodes, with long-term follow-up.
- Surgery to remove the testicle and lymph nodes, followed by combination chemotherapy and long-term follow-up.
- Surgery to remove the testicle, followed by combination chemotherapy and a second surgery if cancer remains, with long-term follow-up.
- Combination chemotherapy before surgery to remove the testicle, for cancer that has spread and is thought to be life-threatening.
Stage 3 testicular cancer treatment
Treatment of stage 3 testicular cancer depends on whether the cancer is a seminoma or a nonseminoma.
Treatment of seminoma testicular cancer may include the following:
- Surgery to remove the testicle, followed by combination chemotherapy. If there are tumors remaining after chemotherapy, treatment may be one of the following:
- Surveillance with no treatment unless tumors grow.
- Surveillance for tumors smaller than 3 centimeters and surgery to remove tumors larger than 3 centimeters.
- A PET scan two months after chemotherapy and surgery to remove tumors that show up with cancer on the scan.
- A clinical trial of chemotherapy.
Treatment of nonseminoma testicular cancer may include the following:
- Surgery to remove the testicle, followed by combination chemotherapy.
- Combination chemotherapy followed by surgery to remove the testicle and all remaining tumors. Additional chemotherapy may be given if the tumor tissue removed contains cancer cells that are growing or if follow-up tests show that cancer is progressing.
- Combination chemotherapy before surgery to remove the testicle, for cancer that has spread and is thought to be life-threatening.
- A clinical trial of chemotherapy.
Treatment of recurrent testicular cancer
Testicular cancer can recur (come back) after it has been treated.
Treatment of recurrent testicular cancer may include the following:
- Combination chemotherapy.
- High-dose chemotherapy and stem cell transplant.
- Surgery to remove cancer that has either:
- come back more than 2 years after complete remission; or
- come back in only one place and does not respond to chemotherapy.
- A clinical trial of a new therapy.
Surveillance for seminomas after initial management
Surveillance for seminomas after initial management is as follows:
Clinical stage 1 seminoma after radical inguinal orchiectomy alone:
- Year 1: History and physical examination (H&P) every 3-6 months, CT scan of abdomen +/- pelvis at 3, 6, and 12 months.
- Years 2 and 3: History and physical examination and CT scan of abdomen +/- pelvis every 6-12 months.
- Years 4 and 5: History and physical examination annually, and CT scan of abdomen +/- pelvis every 12-24 months.
*At any point in five years, a chest x-ray is recommended as clinically indicated, and chest CT with contrast is obtained if the patient is symptomatic. Serum tumor markers are optional with history and physical examination.
Clinical stage 1 seminoma after adjuvant therapy (chemotherapy or radiation):
- Years 1 and 2: History and physical examination every 6-12 months, and CT scan of abdomen +/- pelvis annually
- Year 3: History and physical examination and CT of abdomen +/- pelvis annually
- Years 4 and 5: History and physical examination annually
*At any point in five years, a chest x-ray is recommended as clinically indicated, and chest CT with contrast is obtained if the patient is symptomatic. Serum tumor markers are optional with H&P.
Clinical stage 2A and non-bulky 2B seminoma after radiation or chemotherapy:
- Year 1: History and physical examination every three months, CT scan of abdomen +/- pelvis at three months and then every 6-12 months, and chest x-ray every six months.
- Year 2: History and physical examination every six months, CT scan of abdomen +/- pelvis annually, and chest x-ray every six months.
- Year 3: History and physical examination every six months, and CT scan of abdomen +/- pelvis annually.
- Year 4 and 5: History and physical examination every six months and CT scan fo abdomen +/- pelvis as clinically indicated.
*Serum tumor markers are optional with history and physical examination.
Clinical bulky stage 2B, 2C, and stage 3 seminoma after chemotherapy:
- Year 1: History and physical examination with serum tumor markers every two months, CT scan of abdomen/pelvis every four months, and chest X-ray every two months.
- Year 2: History and physical examination with serum tumor markers every three months, CT scan of abdomen/pelvis every six months, and chest X-ray every three months.
- Years 3 and 4: History and physical examination with serum tumor markers every six months, CT scan of abdomen/pelvis chest X-ray annually.
- Year 5: History and physical examination with serum tumor markers annually, CT scan of abdomen/pelvis as clinically indicated, and chest X-ray annually.
Seminoma cancer prognosis
Seminoma cancer prognosis and treatment options depend on the following:
- Stage of the cancer (whether it is in or near the testicle or has spread to other places in the body, and blood levels of AFP, beta-hCG, and LDH).
- Type of cancer.
- Size of the tumor.
- Number and size of retroperitoneal lymph nodes.
Testicular tumors are divided into 3 groups, based on how well the tumors are expected to respond to treatment:
- Good Prognosis
- Intermediate Prognosis
- Poor Prognosis
Testicular cancer can usually be cured in patients who receive adjuvant (add-on) chemotherapy or radiation therapy after their primary treatment.
Certain treatments for testicular cancer can cause infertility that may be permanent. Patients who may wish to have children should consider sperm banking before having treatment. Sperm banking is the process of freezing sperm and storing it for later use.
Good Prognosis
Nonseminoma
- Testis/retroperitoneal primary, and
- No nonpulmonary visceral metastases, and
- Good markers–all of:
- Alpha-fetoprotein (AFP) less than 1,000 ng/mL, and
- Beta-human chorionic gonadotropin (beta-hCG) less than 5,000 IU/mL (1,000 ng/mL), and
- Lactate dehydrogenase (LDH) less than 1.5 × the upper limit of normal
A total of 56% to 61% of nonseminomas are good prognosis. The 5-year progression-free survival rate is 89%; the 5-year survival rate is 92%–94%.
Seminoma
- Any primary site, and
- No nonpulmonary visceral metastases, and
- Normal alpha-fetoprotein (AFP), any beta-human chorionic gonadotropin (beta-hCG), any lactate dehydrogenase (LDH)
A total of 90% of seminomas are good prognosis. The 5-year progression-free survival rate is 82%; the 5-year survival rate is 86%.
Intermediate Prognosis
Nonseminoma
- Testis/retroperitoneal primary, and
- No nonpulmonary visceral metastases, and
- Intermediate markers–any of:
- Alpha-fetoprotein (AFP) 1,000 ng/mL or more and 10,000 ng/mL or less, or
- Beta-human chorionic gonadotropin (beta-hCG) 5,000 IU/L or more and 50,000 IU/L or less, or
- Lactate dehydrogenase (LDH) 1.5 or more × N* and less than 10 × N*
- *[Note: N indicates the upper limit of normal for the LDH assay.]
A total of 13% to 28% of nonseminomas are intermediate prognosis. The 5-year progression-free survival rate is 75%; the 5-year survival rate is 80%–83%.
Seminoma
- Any primary site, and
- Nonpulmonary visceral metastases, and
- Normal alpha-fetoprotein (AFP), any
- beta-human chorionic gonadotropin (beta-hCG), any lactate dehydrogenase (LDH)
A total of 10% of seminomas are intermediate prognosis. The 5-year progression-free survival rate is 67%; the 5-year survival rate is 72%.
Poor Prognosis
Nonseminoma
- Mediastinal primary, or
- Nonpulmonary visceral metastases, or
- For markers–any of:
- Alpha-fetoprotein (AFP) more than 10,000 ng/mL, or
- Beta-human chorionic gonadotropin (beta-hCG) more than 50,000 IU/mL (10,000 ng/mL), or
- Lactate dehydrogenase (LDH) more than 10 × the upper limit of normal
A total of 16% to 26% of nonseminomas are poor prognosis. The 5-year progression-free survival rate rate is 41%; the 5-year survival rate is 71%.
Seminoma
There is no poor prognosis grouping for seminoma testicular tumors. Seminoma is one of the treatable and curable cancers, with a survival rate above 95% if discovered in early stages 8, 9, 10, 11.
Seminoma cancer life expectancy
According to information from the Surveillance, Epidemiology, and Rend-Results (SEER) 2024 database, the 5-year relative survival rates for testicular cancer are 5:
- Because testicular cancer usually can be treated successfully, a man’s lifetime risk of dying from this cancer is very low. 5-Year Relative Survival is 95%. A relative survival rate compares people with the same type and stage of cancer to those in the overall population. For example, if the 5-year relative survival rate for a specific stage of testicular cancer is 95%, it means that people who have that cancer are, on average, about 95% as likely as people who don’t have that cancer to live for at least 5 years after being diagnosed.
- Localized disease (stage 1) 99%
- Regional disease (stage 2) 96%
- Distant disease (Stage 3) 73%
Patients with testicular cancer are at an increased risk of secondary cancers because of their young age at diagnosis, high cure rate, and exposure to radiation, chemotherapy, or both 64.
Both radiation therapy and chemotherapy have long-term complications in survivors of testicular cancer 64. With post-therapy life expectancy estimates being approximately more than 40 years in these young individuals, the morbidity of long term complications can be very significant.
- Chemotherapy related neurotoxicity: Peripheral neuropathy is a common adverse event of platinum chemotherapy. About 20 to 40% of patients will develop neurotoxicity, which can be painful and also cause permanent sensory abnormalities.
- Cardiovascular complications: There can be up to a seven-fold increased risk of developing a cardiac event in survivors of testicular cancer who received cisplatin-based chemotherapy 76.
- Infertility and hypogonadism: Chemotherapy and the use of radiation to seminoma affected scrotum can result in oligospermia and infertility. Thus, sperm banking must be offered to all patients before undergoing chemotherapy or radiotherapy. The risk of infertility is directly proportional to the intensity and duration of the treatment. Hypogonadism or testicular dysfunction is a common sequela among survivors of testicular cancer.
- Ototoxicity: Cisplatin can cause permanent, sensorineural hearing loss and tinnitus.
- Secondary tumors: Both chemotherapy and radiotherapy can increase the risk of secondary malignant tumors in survivors. Etoposide can cause treatment-related leukemia, and risk is proportional to the total dose administered. Radiation therapy, often used in the management of pure seminomatous germ cell cancers, has been linked to the development of secondary cancers, especially solid tumors in the radiation portal, usually after a latency period of a decade or more 77, 78. These secondary cancers include melanoma and cancers of the stomach, bladder, colon, rectum, pancreas, lung, pleura, prostate, kidney, connective tissue, and thyroid.
- Lamichhane A, Mukkamalla SKR. Seminoma. [Updated 2023 Aug 8]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK560513/[↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩]
- Chung P, Warde P. Testicular cancer: germ cell tumours. BMJ Clin Evid. 2016 Jan 7;2016:1807. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4704678/[↩][↩][↩]
- Ghazarian AA, Trabert B, Devesa SS, McGlynn KA. Recent trends in the incidence of testicular germ cell tumors in the United States. Andrology. 2015 Jan;3(1):13-8. doi: 10.1111/andr.288[↩]
- Nigam M, Aschebrook-Kilfoy B, Shikanov S, Eggener S. Increasing incidence of testicular cancer in the United States and Europe between 1992 and 2009. World J Urol. 2015 May;33(5):623-31. doi: 10.1007/s00345-014-1361-y[↩]
- Testicular Cancer — Cancer Stat Facts. https://seer.cancer.gov/statfacts/html/testis.html[↩][↩]
- Zores T, Mouracade P, Duclos B, Saussine C, Lang H, Jacqmin D. Surveillance des séminomes testiculaires de stade I: résultats oncologiques sur 20ans [Surveillance of stage I testicular seminoma: 20 years oncological results]. Prog Urol. 2015 Apr;25(5):282-7. French. doi: 10.1016/j.purol.2015.01.009[↩]
- International Germ Cell Consensus Classification: a prognostic factor-based staging system for metastatic germ cell cancers. International Germ Cell Cancer Collaborative Group. J Clin Oncol. 1997 Feb;15(2):594-603. doi: 10.1200/JCO.1997.15.2.594[↩][↩][↩]
- Bokemeyer C, Nichols CR, Droz JP, Schmoll HJ, Horwich A, Gerl A, Fossa SD, Beyer J, Pont J, Kanz L, Einhorn L, Hartmann JT. Extragonadal germ cell tumors of the mediastinum and retroperitoneum: results from an international analysis. J Clin Oncol. 2002 Apr 1;20(7):1864-73. doi: 10.1200/JCO.2002.07.062[↩][↩]
- Dieckmann KP, Richter-Simonsen H, Kulejewski M, Ikogho R, Zecha H, Anheuser P, Pichlmeier U, Isbarn H. Testicular Germ-Cell Tumours: A Descriptive Analysis of Clinical Characteristics at First Presentation. Urol Int. 2018;100(4):409-419. doi: 10.1159/000488284[↩][↩]
- Chung P, Warde P. Testicular cancer: seminoma. BMJ Clin Evid. 2011 Jan 25;2011:1807. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3217763/[↩][↩]
- Fung C, Dinh PC, Fossa SD, Travis LB. Testicular Cancer Survivorship. J Natl Compr Canc Netw. 2019 Dec;17(12):1557-1568. doi: 10.6004/jnccn.2019.7369[↩][↩]
- Radical Orchiectomy. https://www.hopkinsmedicine.org/health/conditions-and-diseases/testicular-cancer/radical-orchiectomy[↩]
- Stokes W, Amini A, Maroni PD, Kessler ER, Stokes C, Cost CR, Greffe BS, Garrington TP, Liu AK, Cost NG. Patterns of care and survival outcomes for adolescent and young adult patients with testicular seminoma in the United States: A National Cancer Database analysis. J Pediatr Urol. 2017 Aug;13(4):386.e1-386.e7. doi: 10.1016/j.jpurol.2016.12.009[↩][↩]
- Chovanec M, Hanna N, Cary KC, Einhorn L, Albany C. Management of stage I testicular germ cell tumours. Nat Rev Urol. 2016 Nov;13(11):663-673. doi: 10.1038/nrurol.2016.164[↩][↩]
- Motzer RJ, Jonasch E, Agarwal N, Beard C, Bhayani S, Bolger GB, Chang SS, Choueiri TK, Costello BA, Derweesh IH, Gupta S, Hancock SL, Kim JJ, Kuzel TM, Lam ET, Lau C, Levine EG, Lin DW, Michaelson MD, Olencki T, Pili R, Plimack ER, Rampersaud EN, Redman BG, Ryan CJ, Sheinfeld J, Shuch B, Sircar K, Somer B, Wilder RB, Dwyer M, Kumar R. Testicular Cancer, Version 2.2015. J Natl Compr Canc Netw. 2015 Jun;13(6):772-99. doi: 10.6004/jnccn.2015.0092[↩][↩]
- Faouzi S, Ouguellit S, Loriot Y. Tumeurs germinales de stade I [Stage 1 germ-cell tumour]. Bull Cancer. 2019 Oct;106(10):887-895. French. doi: 10.1016/j.bulcan.2019.03.010[↩][↩]
- Stephenson A, Eggener SE, Bass EB, Chelnick DM, Daneshmand S, Feldman D, Gilligan T, Karam JA, Leibovich B, Liauw SL, Masterson TA, Meeks JJ, Pierorazio PM, Sharma R, Sheinfeld J. Diagnosis and Treatment of Early Stage Testicular Cancer: AUA Guideline. J Urol. 2019 Aug;202(2):272-281. doi: 10.1097/JU.0000000000000318[↩][↩]
- Alsdorf W, Seidel C, Bokemeyer C, Oing C. Current pharmacotherapy for testicular germ cell cancer. Expert Opin Pharmacother. 2019 May;20(7):837-850. doi: 10.1080/14656566.2019.1583745[↩][↩]
- Fizazi K, Delva R, Caty A, Chevreau C, Kerbrat P, Rolland F, Priou F, Geoffrois L, Rixe O, Beuzeboc P, Malhaire JP, Culine S, Aubelle MS, Laplanche A. A risk-adapted study of cisplatin and etoposide, with or without ifosfamide, in patients with metastatic seminoma: results of the GETUG S99 multicenter prospective study. Eur Urol. 2014 Feb;65(2):381-6. doi: 10.1016/j.eururo.2013.09.004[↩][↩]
- Hainsworth JD, Greco FA. Malignant Germ Cell Tumors. In: Kufe DW, Pollock RE, Weichselbaum RR, et al., editors. Holland-Frei Cancer Medicine. 6th edition. Hamilton (ON): BC Decker; 2003. Available from: https://www.ncbi.nlm.nih.gov/books/NBK12497/[↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩]
- Dehner LP. Gonadal and extragonadal germ cell neoplasia of childhood. Hum Pathol. 1983 Jun;14(6):493-511. doi: 10.1016/s0046-8177(83)80004-5[↩]
- McIntyre A, Gilbert D, Goddard N, Looijenga L, Shipley J. Genes, chromosomes and the development of testicular germ cell tumors of adolescents and adults. Genes Chromosomes Cancer. 2008 Jul;47(7):547-57. doi: 10.1002/gcc.20562[↩]
- Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, Bray F. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J Clin. 2021 May;71(3):209-249. doi: 10.3322/caac.21660[↩]
- Ghazarian AA, et al. Future of testicular germ cell tumor incidence in the United States: forecast through 2026. Cancer. 2017;123(12):2320–2328. doi: 10.1002/cncr.30597[↩]
- Nauman M, Leslie SW. Nonseminomatous Testicular Tumors. [Updated 2023 Aug 14]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK568754[↩]
- PDQ Adult Treatment Editorial Board. Testicular Cancer Treatment (PDQ®): Health Professional Version. 2024 Mar 15. In: PDQ Cancer Information Summaries [Internet]. Bethesda (MD): National Cancer Institute (US); 2002-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK65777/[↩][↩][↩][↩][↩][↩][↩][↩]
- van Dijk MR, Steyerberg EW, Habbema JD. Survival of non-seminomatous germ cell cancer patients according to the IGCC classification: An update based on meta-analysis. Eur J Cancer. 2006 May;42(7):820-6. doi: 10.1016/j.ejca.2005.08.043[↩][↩]
- Williams SD, Birch R, Einhorn LH, Irwin L, Greco FA, Loehrer PJ. Treatment of disseminated germ-cell tumors with cisplatin, bleomycin, and either vinblastine or etoposide. N Engl J Med. 1987 Jun 4;316(23):1435-40. doi: 10.1056/NEJM198706043162302[↩][↩]
- Nichols CR, Catalano PJ, Crawford ED, Vogelzang NJ, Einhorn LH, Loehrer PJ. Randomized comparison of cisplatin and etoposide and either bleomycin or ifosfamide in treatment of advanced disseminated germ cell tumors: an Eastern Cooperative Oncology Group, Southwest Oncology Group, and Cancer and Leukemia Group B Study. J Clin Oncol. 1998 Apr;16(4):1287-93. doi: 10.1200/JCO.1998.16.4.1287[↩]
- Hinton S, Catalano PJ, Einhorn LH, Nichols CR, David Crawford E, Vogelzang N, Trump D, Loehrer PJ Sr. Cisplatin, etoposide and either bleomycin or ifosfamide in the treatment of disseminated germ cell tumors: final analysis of an intergroup trial. Cancer. 2003 Apr 15;97(8):1869-75. doi: 10.1002/cncr.11271[↩]
- de Wit R, Louwerens M, de Mulder PH, Verweij J, Rodenhuis S, Schornagel J. Management of intermediate-prognosis germ-cell cancer: results of a phase I/II study of Taxol-BEP. Int J Cancer. 1999 Dec 10;83(6):831-3. doi: 10.1002/(sici)1097-0215(19991210)83:6<831::aid-ijc24>3.0.co;2-o[↩]
- Childhood Extracranial Germ Cell Tumors Treatment (PDQ®)–Health Professional Version. https://www.cancer.gov/types/extracranial-germ-cell/hp/germ-cell-treatment-pdq[↩]
- Extragonadal Germ Cell Tumors Treatment (PDQ®)–Patient Version. https://www.cancer.gov/types/extragonadal-germ-cell/patient/extragonadal-treatment-pdq[↩][↩][↩][↩]
- Polansky SM, Barwick KW, Ravin CE. Primary mediastinal seminoma. AJR Am J Roentgenol. 1979 Jan;132(1):17-21. doi: 10.2214/ajr.132.1.17[↩]
- Jain KK, Bosl GJ, Bains MS, Whitmore WF, Golbey RB. The treatment of extragonadal seminoma. J Clin Oncol. 1984 Jul;2(7):820-7. doi: 10.1200/JCO.1984.2.7.820[↩][↩][↩][↩][↩]
- Knapp RH, Hurt RD, Payne WS, Farrow GM, Lewis BD, Hahn RG, Muhm JR, Earle JD. Malignant germ cell tumors of the mediastinum. J Thorac Cardiovasc Surg. 1985 Jan;89(1):82-9.[↩]
- Luna MA, Valenzuela-Tamariz J. Germ-cell tumors of the mediastinum, postmortem findings. Am J Clin Pathol. 1976 Apr;65(4):450-4. doi: 10.1093/ajcp/65.4.450[↩]
- Bagshaw MA, McLaughlin WT, Earle JD. Definitive radiotherapy of primary mediastinal seminoma. Am J Roentgenol Radium Ther Nucl Med. 1969 Jan;105(1):86-94. doi: 10.2214/ajr.105.1.86[↩]
- Levitt RG, Husband JE, Glazer HS. CT of primary germ-cell tumors of the mediastinum. AJR Am J Roentgenol. 1984 Jan;142(1):73-8. doi: 10.2214/ajr.142.1.73[↩]
- Lattes R . Thymoma and other tumors of thymus: analysis of 107 cases. Cancer. 1962;15:1224–60.[↩]
- Martini N, Golbey RB, Hajdu SI, Whitmore WF, Beattie EJ Jr. Primary mediastinal germ cell tumors. Cancer. 1974 Mar;33(3):763-9. doi: 10.1002/1097-0142(197403)33:3<763::aid-cncr2820330323>3.0.co;2-e[↩][↩]
- Schantz A, Sewall W, Castleman B. Mediastinal germinoma. A study of 21 cases with an excellent prognosis. Cancer. 1972 Nov;30(5):1189-94. doi: 10.1002/1097-0142(197211)30:5<1189::aid-cncr2820300508>3.0.co;2-9[↩]
- Dulmet EM, Macchiarini P, Suc B, Verley JM. Germ cell tumors of the mediastinum. A 30-year experience. Cancer. 1993 Sep 15;72(6):1894-901. doi: 10.1002/1097-0142(19930915)72:6<1894::aid-cncr2820720617>3.0.co;2-6[↩]
- Hurt RD, Bruckman JE, Farrow GM, Bernatz PE, Hahn RG, Earle JD. Primary anterior mediastinal seminoma. Cancer. 1982 Apr 15;49(8):1658-63. doi: 10.1002/1097-0142(19820415)49:8<1658::aid-cncr2820490821>3.0.co;2-g[↩]
- Bush SE, Martinez A, Bagshaw MA. Primary mediastinal seminoma. Cancer. 1981 Oct 15;48(8):1877-82. doi: 10.1002/1097-0142(19811015)48:8<1877::aid-cncr2820480827>3.0.co;2-b[↩]
- Peckham MJ, Horwich A, Hendry WF. Advanced seminoma: treatment with cis-platinum-based combination chemotherapy or carboplatin (JM8). Br J Cancer. 1985 Jul;52(1):7-13. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1977156/pdf/brjcancer00093-0008.pdf[↩]
- Schultz SM, Einhorn LH, Conces DJ Jr, Williams SD, Loehrer PJ. Management of postchemotherapy residual mass in patients with advanced seminoma: Indiana University experience. J Clin Oncol. 1989 Oct;7(10):1497-503. doi: 10.1200/JCO.1989.7.10.1497[↩]
- Puc HS, Heelan R, Mazumdar M, Herr H, Scheinfeld J, Vlamis V, Bajorin DF, Bosl GJ, Mencel P, Motzer RJ. Management of residual mass in advanced seminoma: results and recommendations from the Memorial Sloan-Kettering Cancer Center. J Clin Oncol. 1996 Feb;14(2):454-60. doi: 10.1200/JCO.1996.14.2.454[↩]
- Motzer R, Bosl G, Heelan R, Fair W, Whitmore W, Sogani P, Herr H, Morse M. Residual mass: an indication for further therapy in patients with advanced seminoma following systemic chemotherapy. J Clin Oncol. 1987 Jul;5(7):1064-70. doi: 10.1200/JCO.1987.5.7.1064[↩]
- Atkin NB, Baker MC. Specific chromosome change, i(12p), in testicular tumours? Lancet. 1982;2(8311):1349. doi: 10.1016/S0140-6736(82)91557-4[↩][↩]
- Stock C, et al. Isochromosome 12p and maternal loss of 1p36 in a pediatric testicular germ cell tumor. Cancer Genet Cytogenet. 1996;91(2):95–100. doi: 10.1016/0165-4608(95)00190-5[↩][↩]
- Sheikine Y, Genega E, Melamed J, Lee P, Reuter VE, Ye H. Molecular genetics of testicular germ cell tumors. Am J Cancer Res. 2012;2(2):153-67. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3304567/[↩]
- PDQ Adult Treatment Editorial Board. Testicular Cancer Treatment (PDQ®): Patient Version. 2023 May 17. In: PDQ Cancer Information Summaries [Internet]. Bethesda (MD): National Cancer Institute (US); 2002-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK65847/[↩][↩]
- Batool A, Karimi N, Wu XN, Chen SR, Liu YX. Testicular germ cell tumor: a comprehensive review. Cell Mol Life Sci. 2019 May;76(9):1713-1727. doi: 10.1007/s00018-019-03022-7[↩]
- Barchi M, Innocenzi E, Giannattasio T, Dolci S, Rossi P, Grimaldi P. Cannabinoid Receptors Signaling in the Development, Epigenetics, and Tumours of Male Germ Cells. Int J Mol Sci. 2019 Dec 18;21(1):25. doi: 10.3390/ijms21010025[↩]
- Gurney J, Shaw C, Stanley J, Signal V, Sarfati D. Cannabis exposure and risk of testicular cancer: a systematic review and meta-analysis. BMC Cancer. 2015 Nov 11;15:897. doi: 10.1186/s12885-015-1905-6[↩]
- Garolla A, Vitagliano A, Muscianisi F, Valente U, Ghezzi M, Andrisani A, Ambrosini G, Foresta C. Role of Viral Infections in Testicular Cancer Etiology: Evidence From a Systematic Review and Meta-Analysis. Front Endocrinol (Lausanne). 2019 Jun 12;10:355. doi: 10.3389/fendo.2019.00355[↩]
- Fukawa T, Kanayama HO. Current knowledge of risk factors for testicular germ cell tumors. Int J Urol. 2018 Apr;25(4):337-344. doi: 10.1111/iju.13519[↩]
- Coffey J, Linger R, Pugh J, Dudakia D, Sokal M, Easton DF, Timothy Bishop D, Stratton M, Huddart R, Rapley EA. Somatic KIT mutations occur predominantly in seminoma germ cell tumors and are not predictive of bilateral disease: report of 220 tumors and review of literature. Genes Chromosomes Cancer. 2008 Jan;47(1):34-42. doi: 10.1002/gcc.20503[↩]
- Goedert JJ, Purdue MP, McNeel TS, McGlynn KA, Engels EA. Risk of germ cell tumors among men with HIV/acquired immunodeficiency syndrome. Cancer Epidemiol Biomarkers Prev. 2007 Jun;16(6):1266-9. doi: 10.1158/1055-9965.EPI-07-0042[↩]
- Skakkebaek NE, Rajpert-De Meyts E, Buck Louis GM, Toppari J, Andersson AM, Eisenberg ML, Jensen TK, Jørgensen N, Swan SH, Sapra KJ, Ziebe S, Priskorn L, Juul A. Male Reproductive Disorders and Fertility Trends: Influences of Environment and Genetic Susceptibility. Physiol Rev. 2016 Jan;96(1):55-97. doi: 10.1152/physrev.00017.2015[↩]
- Oldenburg J, Berney DM, Bokemeyer C, Climent MA, Daugaard G, Gietema JA, De Giorgi U, Haugnes HS, Huddart RA, Leão R, Sohaib A, Gillessen S, Powles T; ESMO Guidelines Committee. Electronic address: [email protected]; EURACAN. Testicular seminoma and non-seminoma: ESMO-EURACAN Clinical Practice Guideline for diagnosis, treatment and follow-up. Ann Oncol. 2022 Apr;33(4):362-375. doi: 10.1016/j.annonc.2022.01.002[↩][↩]
- Rajpert-De Meyts E, McGlynn KA, Okamoto K, Jewett MA, Bokemeyer C. Testicular germ cell tumours. Lancet. 2016 Apr 23;387(10029):1762-74. doi: 10.1016/S0140-6736(15)00991-5[↩]
- Lamichhane A, Mukkamalla SKR. Seminoma. [Updated 2023 Aug 8]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK560513[↩][↩][↩][↩][↩][↩]
- Tourne M, Radulescu C, Allory Y. Tumeurs germinales du testicule : caractéristiques histopathologiques et moléculaires [Testicular germ cell tumors: Histopathological and molecular features]. Bull Cancer. 2019 Apr;106(4):328-341. French. doi: 10.1016/j.bulcan.2019.02.004[↩]
- Sturgeon CM, Duffy MJ, Stenman UH, et al. National Academy of Clinical Biochemistry. National Academy of Clinical Biochemistry laboratory medicine practice guidelines for use of tumor markers in testicular, prostate, colorectal, breast, and ovarian cancers. Clin Chem. 2008 Dec;54(12):e11-79. doi: 10.1373/clinchem.2008.105601[↩]
- Gholam D, Fizazi K, Terrier-Lacombe MJ, Jan P, Culine S, Theodore C. Advanced seminoma–treatment results and prognostic factors for survival after first-line, cisplatin-based chemotherapy and for patients with recurrent disease: a single-institution experience in 145 patients. Cancer. 2003 Aug 15;98(4):745-52. doi: 10.1002/cncr.11574[↩]
- Oliver RT, Mason MD, Mead GM, von der Maase H, Rustin GJ, Joffe JK, de Wit R, Aass N, Graham JD, Coleman R, Kirk SJ, Stenning SP; MRC TE19 collaborators and the EORTC 30982 collaborators. Radiotherapy versus single-dose carboplatin in adjuvant treatment of stage I seminoma: a randomised trial. Lancet. 2005 Jul 23-29;366(9482):293-300. doi: 10.1016/S0140-6736(05)66984-X[↩]
- Weissbach L, Bussar-Maatz R, Mann K. The value of tumor markers in testicular seminomas. Results of a prospective multicenter study. Eur Urol. 1997;32(1):16-22.[↩]
- Venkitaraman R, Johnson B, Huddart RA, Parker CC, Horwich A, Dearnaley DP. The utility of lactate dehydrogenase in the follow-up of testicular germ cell tumours. BJU Int. 2007 Jul;100(1):30-2. doi: 10.1111/j.1464-410X.2007.06905.x[↩][↩][↩]
- Ackers C, Rustin GJ. Lactate dehydrogenase is not a useful marker for relapse in patients on surveillance for stage I germ cell tumours. Br J Cancer. 2006 May 8;94(9):1231-2. doi: 10.1038/sj.bjc.6603087[↩][↩]
- Gupta M, Cheaib JG, Patel HD, Sharma R, Zhang A, Bass EB, Pierorazio PM. Diagnosis and Management of Intratubular Germ Cell Neoplasia In Situ: A Systematic Review. J Urol. 2020 Jul;204(1):33-41. doi: 10.1097/JU.0000000000000758[↩]
- Kristianslund S, Fosså SD, Kjellevold K. Bilateral malignant testicular germ cell cancer. Br J Urol. 1986 Feb;58(1):60-3. doi: 10.1111/j.1464-410x.1986.tb05429.x[↩]
- Oldenburg J. Hypogonadism and fertility issues following primary treatment for testicular cancer. Urol Oncol. 2015 Sep;33(9):407-12. doi: 10.1016/j.urolonc.2015.01.014[↩]
- Fankhauser CD, et al. Frequent PD-L1 expression in testicular germ cell tumors. Br J Cancer. 2015;113(3):411–413. doi: 10.1038/bjc.2015.244.[↩]
- Huddart RA, Norman A, Shahidi M, Horwich A, Coward D, Nicholls J, Dearnaley DP. Cardiovascular disease as a long-term complication of treatment for testicular cancer. J Clin Oncol. 2003 Apr 15;21(8):1513-23. doi: 10.1200/JCO.2003.04.173[↩]
- Travis LB, Fosså SD, Schonfeld SJ, McMaster ML, Lynch CF, Storm H, Hall P, Holowaty E, Andersen A, Pukkala E, Andersson M, Kaijser M, Gospodarowicz M, Joensuu T, Cohen RJ, Boice JD Jr, Dores GM, Gilbert ES. Second cancers among 40,576 testicular cancer patients: focus on long-term survivors. J Natl Cancer Inst. 2005 Sep 21;97(18):1354-65. doi: 10.1093/jnci/dji278[↩]
- van den Belt-Dusebout AW, de Wit R, Gietema JA, Horenblas S, Louwman MW, Ribot JG, Hoekstra HJ, Ouwens GM, Aleman BM, van Leeuwen FE. Treatment-specific risks of second malignancies and cardiovascular disease in 5-year survivors of testicular cancer. J Clin Oncol. 2007 Oct 1;25(28):4370-8. doi: 10.1200/JCO.2006.10.5296[↩]