Simple prostatectomy
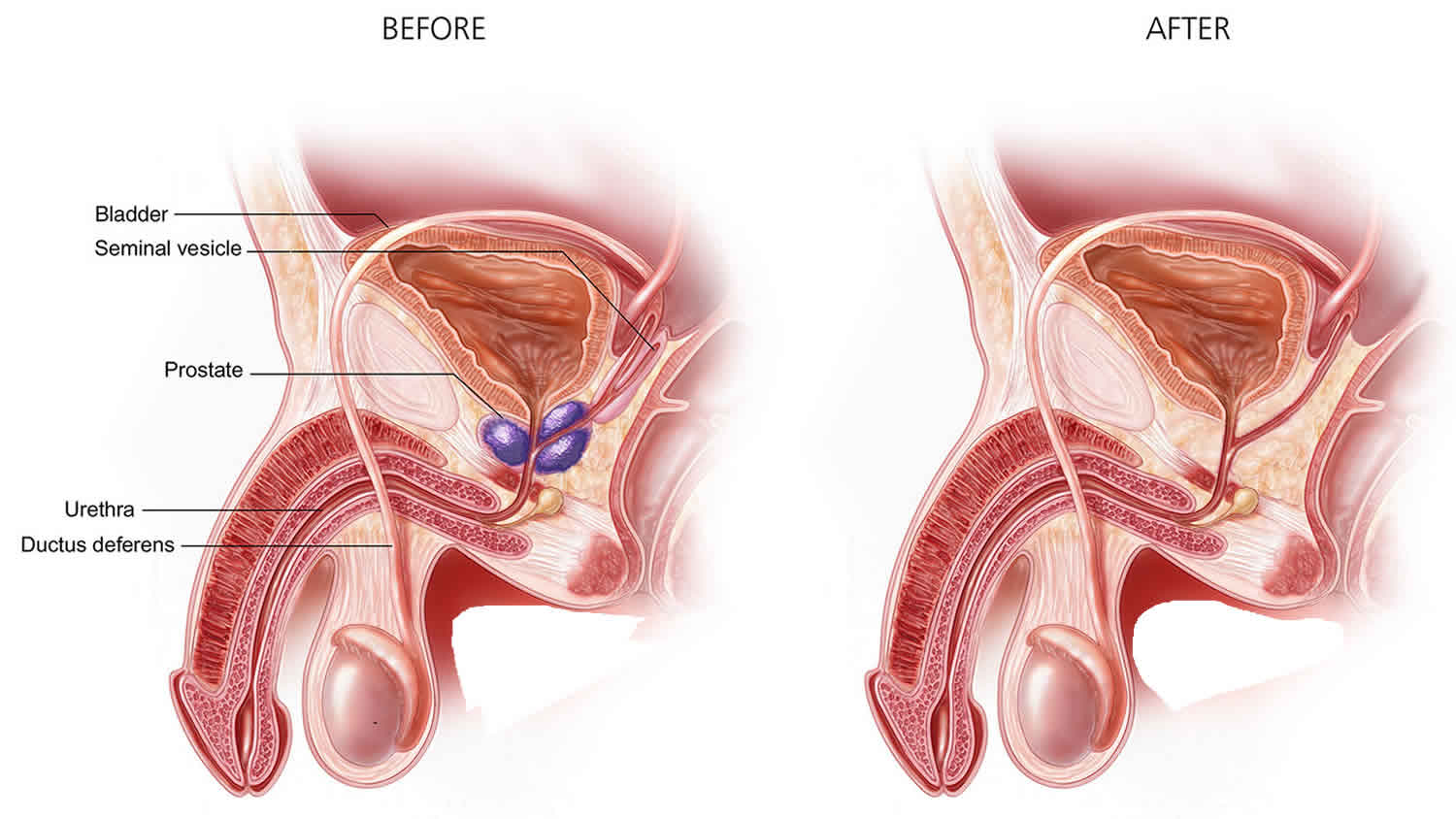
Simple prostatectomy is a surgical procedure to remove the inside part of your prostate gland to treat an enlarged prostate. Simple prostatectomy is done through a surgical cut in your lower belly. Simple prostatectomy is generally recommended for men with severe urinary symptoms and very enlarged prostate glands (rather than prostate cancer), and can be performed open or robotically. This enlargement of the prostate is called benign prostatic hyperplasia, or BPH. Simple prostatectomy doesn’t remove the entire prostate, as in a radical prostatectomy, but instead removes just the obstructive part of the prostate that’s blocking the flow of urine.
Benign growths like benign prostatic hyperplasia (BPH):
- Are rarely a threat to life
- Don’t invade the tissues around them
- Don’t spread to other parts of the body
- Can be removed and can grow back very slowly (but usually don’t grow back)
The prostate goes through two main growth cycles during a man’s life. The first occurs early in puberty, when the prostate doubles in size. The second phase of growth starts around age 25 and goes on for most of the rest of a man’s life. Benign prostatic hyperplasia most often occurs during this second growth phase.
As the prostate enlarges, it presses against the urethra. The bladder wall becomes thicker. One day, the bladder may weaken and lose the ability to empty fully, leaving some urine in the bladder. Narrowing of the urethra and urinary retention – being unable to empty the bladder fully – cause many of the problems of benign prostatic hyperplasia.
Benign prostatic hyperplasia is benign. This means it is not cancer. It does not cause or lead to cancer. However, benign prostatic hyperplasia and cancer can happen at the same time.
Benign prostatic hyperplasia is common. About half of all men between ages 51 and 60 have benign prostatic hyperplasia (BPH). Up to 90% of men over age 80 have it.
When the prostate is enlarged, it can bother or block the bladder. Needing to urinate often is a common symptom of benign prostatic hyperplasia. This might be every 1 to 2 hours, mainly at night.
Other symptoms include:
- Feeling that your bladder is full, even right after urinating
- Feeling that urinating “can’t wait”
- A weak flow of urine
- Needing to stop and start urinating several times
- Trouble starting to urinate
- Trouble starting to urinate
- Needing to push or strain to urinate
If benign prostatic hyperplasia becomes severe, you might not be able to urinate at all. This is an emergency that must be treated right away.
In most men, benign prostatic hyperplasia gets worse with age. It can lead to bladder damage and infection. It can cause blood in the urine and cause kidney damage.
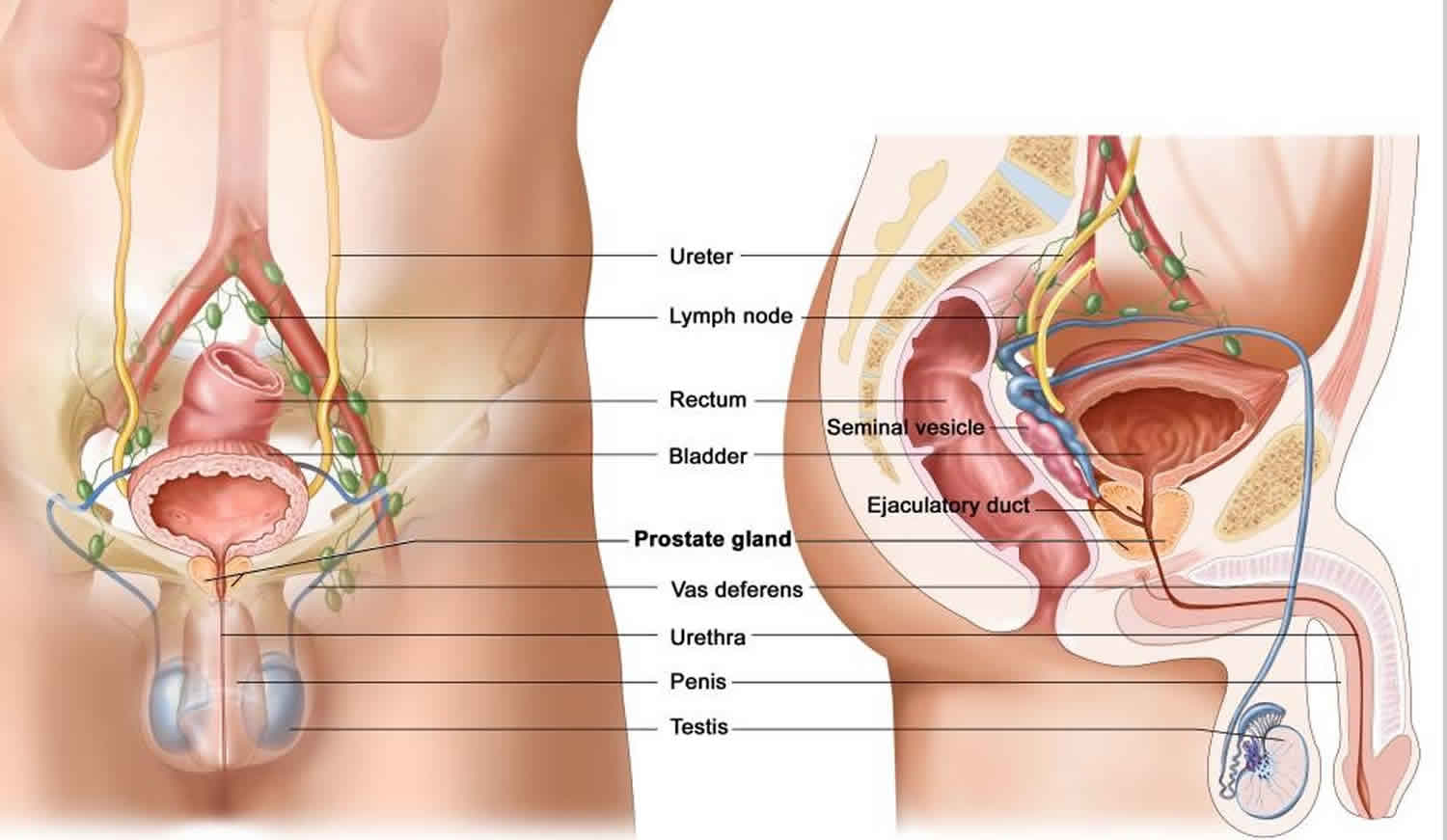
Prostate gland
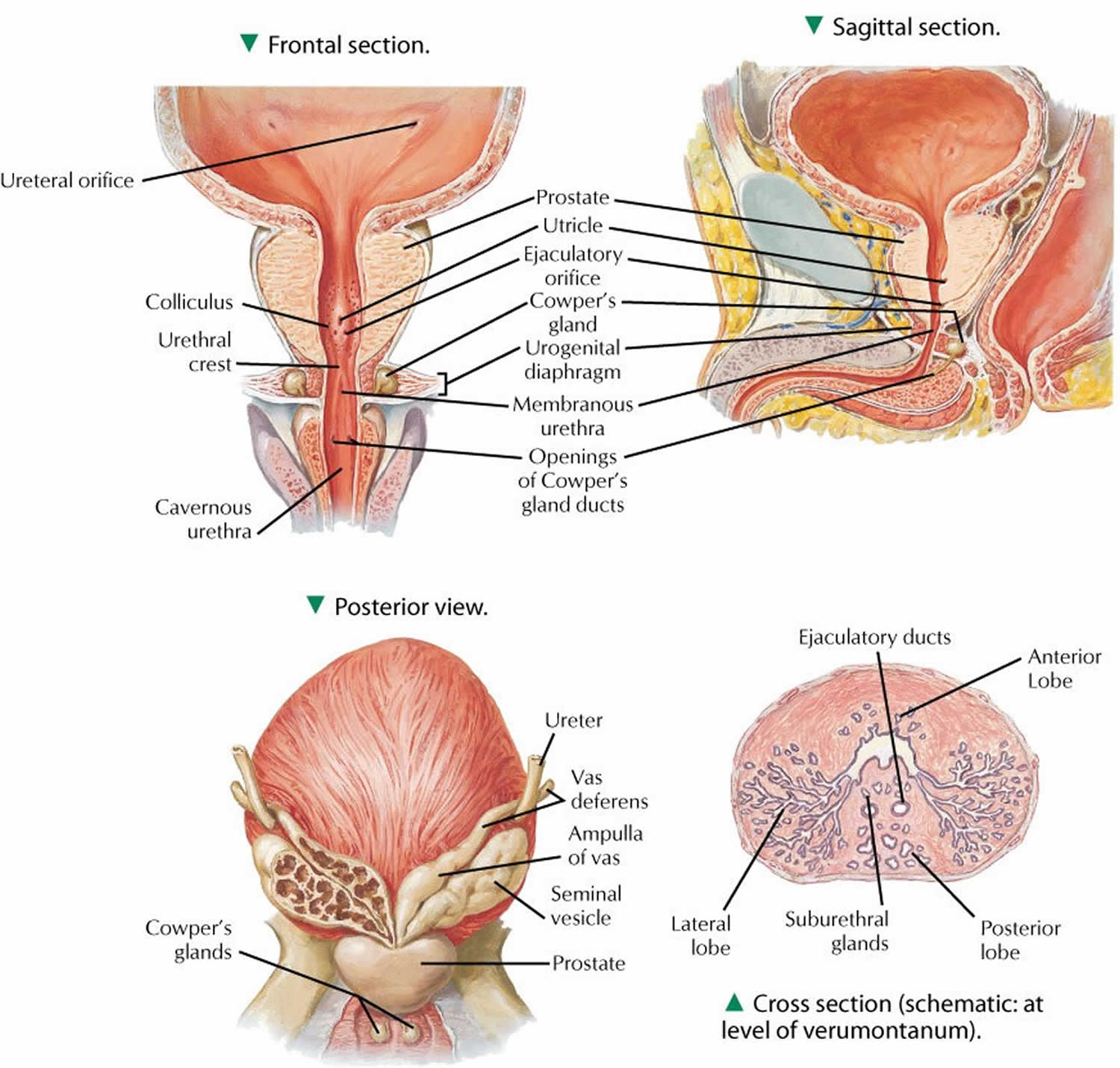
The prostate and seminal vesicles are part of the male reproductive system. The prostate is about the size of a walnut and weighs about one ounce. The seminal vesicles are two much smaller paired glands. These glands are attached to each side of the prostate. Some have said that the seminal vesicles look like rabbit ears attached to the prostate. The prostate is below the bladder and in front of the rectum. The prostate surrounds the urethra. The urethra is a tube that carries urine from the bladder out through the penis. This is why men with an enlarged prostate have difficulty urinating. It can disrupt the flow of urine from the bladder.
The main job of the prostate and seminal vesicles is to make fluid to bathe semen. During ejaculation, sperm is made in the testicles, and then moves to the urethra. At the same time, fluid from the prostate and the seminal vesicles also moves into the urethra. This mixture of semen and fluid from the prostate and seminal vesicles forms the ejaculate that passes through the urethra and out of the penis.
When prostate cancer occurs, it starts in the prostate gland and occasionally spreads to the seminal vesicles.
Figure 1. Prostate gland anatomy
Simple prostatectomy indications
Benign prostatic hyperplasia can cause problems with urinating. This can lead to urinary tract infections. Taking out part of your prostate gland can often make these symptoms better. Before you have surgery, your doctor may tell you some changes you can make in how you eat or drink. You may also be asked to try taking medicine.
Surgery is the treatment of choice for patients with benign prostatic hyperplasia (BPH) who have failed medical treatment and watchful waiting 1. Prostate removal can be done in many different ways. The kind of procedure you will have depends on the size of the prostate and what caused your prostate to grow. Transurethral resection of the prostate (TURP) and open simple prostatectomy are the conventional surgical options. Open simple prostatectomy is often used when the prostate is too large for less invasive surgery. However, this method does not treat prostate cancer. Radical prostatectomy may be needed for prostate cancer.
Prostate removal may be recommended if you have 2:
- Problems emptying your bladder (urinary retention)
- Frequent urinary tract infections
- Frequent bleeding from the prostate
- Bladder stones with prostate enlargement
- Very slow urination
- Damage to the kidneys
Your prostate may also need to be removed if taking medicine and changing your diet do not help your symptoms.
Open prostatectomy
Patients who present for open simple prostatectomy are typically age 60 years or older. Open prostatectomy has 3 different approaches:
- Retropubic open simple prostatectomy,
- Suprapubic open simple prostatectomy,
- Perineal open simple prostatectomy.
Simple retropubic prostatectomy is the enucleation of a hyperplastic prostatic adenoma through a direct incision of the anterior prostatic capsule. Simple suprapubic prostatectomy is the enucleation of the hyperplastic prostatic adenoma through an extraperitoneal incision of the lower anterior bladder wall 3.
The indications for either simple prostatectomy or transurethral resection of the prostate (TURP) include the following 4:
- Acute urinary retention
- Persistent or recurrent urinary tract infections
- Significant hemorrhage or recurrent hematuria
- Bladder calculi secondary to bladder outlet obstruction
- Significant symptoms from bladder outlet obstruction that are not responsive to medical or minimally invasive therapy
- Renal insufficiency secondary to chronic bladder outlet obstruction
The advantages of open (simple) prostatectomy over TURP (transurethral resection of the prostate) include the complete removal of the prostatic adenoma under direct visualization in the suprapubic and retropubic approaches. However, these procedures do not obviate the need for further prostate cancer surveillance because the posterior zone of the prostate remains as a potential source of carcinoma formation.
Advantages of retropubic prostatectomy
Advantages of the retropubic technique over the suprapubic approach include the following:
- Superb anatomic prostatic exposure
- Direct visualization of the adenoma during enucleation to ensure complete removal
- Precise division of the prostatic urethra, optimizing preservation of urinary continence
- Direct visualization of the prostatic fossa after enucleation for hemorrhage control
- Minimal to no surgical trauma to the bladder
Advantages of suprapubic prostatectomy
The major advantage of the suprapubic approach over the retropubic approach is that it permits better visualization of the bladder neck and ureteral orifices and is therefore better suited for patients with the following conditions:
- Enlarged, protuberant, median prostatic lobe
- Concomitant symptomatic bladder diverticulum
- Large bladder calculus
- Obesity (to a degree that makes access to the retropubic space more difficult)
Advantages of simple perineal prostatectomy
Advantages of perineal prostatectomy include the following:
- Ability to treat clinically significant prostatic abscess and prostatic cysts
- Less postoperative pain
- Ability to avoid the retropubic space
With regard to the last point, above, retropubic or suprapubic surgery is more difficult in patients who have had prior retropubic surgery.
Other considerations
Other considerations include congestive heart failure, prostate size, and bladder pathology.
The transurethral resection (TUR) syndrome of dilution hyponatremia is unique to TURP (transurethral resection of the prostate) and does not occur with open (simple) prostatectomy. The incidence of TUR syndrome during a TURP is roughly 2%. Thus, in patients with a greater risk of congestive heart failure caused by underlying cardiopulmonary disease, open prostatectomy has a much smaller risk of intraoperative fluid challenge.
Consider open (simple) prostatectomy, using either the retropubic or suprapubic approach, when the prostate is larger than 75 g or larger than the surgeon can resect reliably with TURP in 60-90 minutes.
In patients with concomitant bladder pathology that complicates their outlet obstruction (eg, a large or hard bladder calculus, symptomatic bladder diverticulum), open prostatectomy remains the procedure of choice. Additionally, patients with musculoskeletal disease that precludes proper patient positioning in the dorsal lithotomy position for TURP may benefit from an open prostatectomy.
Open prostatectomy contraindications
Open (simple) prostatectomy is contraindicated in the presence of prostate cancer. If cancer is suspected, a formal prostate biopsy should be performed before surgery is considered.
If cystoscopy findings indicate that the obstructing adenoma primarily involves the median lobe, the suprapubic approach may be preferred to the retropubic technique, because the suprapubic procedure optimizes anatomic exposure.
In addition, retropubic prostatectomy offers only limited access to the bladder, which is an important consideration if a bladder diverticulum requiring excision coexists or if a large bladder calculus must be directly removed.
The perineal approach can be contraindicated in patients in whom sexual potency remains important. In this procedure, the perineal neurovascular anatomy is invaded more extensively than it is in the other available open techniques.
Open prostatectomy disadvantages
Open (simple) prostatectomy does have disadvantages when compared with TURP. These include the morbidity and longer hospitalization associated with the open procedure and the potential for greater intraoperative hemorrhage.
A disadvantage to the use of suprapubic approach relates to reduced visualization of the apical prostatic adenoma and the potential complications of postoperative urinary incontinence and intraoperative bleeding.
Simple prostatectomy procedure
Before the simple prostatectomy procedure
You will have many visits with your doctor and tests before your surgery:
- Complete physical exam
- Visits with your doctor to make sure medical problems (such as diabetes, high blood pressure, and heart or lung diseases) are being treated well
- Additional testing to confirm bladder function
If you are a smoker, you should stop several weeks before the surgery. Your provider can help.
Always tell your provider what drugs, vitamins, and other supplements you are taking, even ones you bought without a prescription.
During the weeks before your surgery:
- You may need to stop taking aspirin, ibuprofen (Advil, Motrin), naproxen (Aleve, Naprosyn), vitamin E, clopidogrel (Plavix), warfarin (Coumadin), and any other medicines like these.
- Ask your doctor which medicines you should still take on the day of your surgery.
- You may take a special laxative the day before your surgery. This will clean out the contents of your colon.
On the day of your surgery:
- DO NOT eat or drink anything after midnight the night before your surgery.
- Take the drugs you were told to take with a small sip of water.
- You will be told when to arrive at the hospital.
During the simple prostatectomy procedure
You will be given general anesthesia (asleep, pain-free) or spinal anesthesia (sedated, awake, pain-free). The procedure takes about 2 to 4 hours.
Your surgeon will make a surgical cut in your lower belly. The cut will go from below the belly button to just above the pubic bone or it may be made horizontally just above the pubic bone. The bladder is opened and the prostate gland is removed through this cut.
The surgeon removes only the inner part of the prostate gland. The outer part is left behind. The process is similar to scooping out the inside of an orange and leaving the peel intact. After removing part of your prostate, the surgeon will close the outer shell of the prostate with stitches. A drain may be left in your belly to help remove extra fluids after surgery. A catheter may also be left in the bladder. This catheter may be in the urethra or in the lower abdomen or you may have both. These catheters allow the bladder to rest and heal.
After the simple prostatectomy procedure
You will stay in the hospital for about 2 to 4 days.
- You will need to stay in bed until the next morning.
- After you are allowed to get up you will be asked to move around as much as possible.
- Your nurse will help you change positions in bed.
- You will also learn exercises to keep blood flowing, and coughing/deep breathing techniques.
- You should do these exercises every 3 to 4 hours.
- You may need to wear special compression stockings and use a breathing device to keep your lungs clear.
You will leave surgery with a Foley catheter in your bladder. Some men have a suprapubic catheter in their belly wall to help drain the bladder.
Many men recover in about 6 weeks. You can expect to be able to urinate as usual without leaking urine.
Simple prostatectomy risks
Although simple prostatectomy works well at relieving urinary symptoms, it has a higher risk of complications and a longer recovery time than other enlarged prostate procedures such as transurethral resection of the prostate (TURP), laser photoselective vaporization of the prostate (PVP) surgery or holmium laser prostate surgery (HoLEP).
Risks of open simple prostatectomy include:
- Bleeding
- Injury to adjacent structures
- Damage to internal organs
- Passing semen back up into the bladder instead of out through the urethra (retrograde ejaculation) or dry orgasm
- Erectile dysfunction (impotence)
- Loss of the ability for sperm to leave the body resulting in infertility
- Problems with urine control (incontinence)
- Narrowing of the urinary outlet from scar tissue (urethral stricture) or bladder neck stricture
Risks for any surgery are:
- Blood clots in the legs that may travel to the lungs
- Blood loss
- Breathing problems
- Heart attack or stroke during surgery
- Infection, including in the surgical wound, lungs (pneumonia), or bladder or kidney
- Reactions to medicines
Robotic assisted simple prostatectomy
Laparoscopy has become a well-established tool in the management of prostatic carcinoma. In 2002 Mariano et al 5 first reported the use of laparoscopic prostatectomy for benign prostatic hypertrophy. Recently, these authors published their six-year experience with laparoscopic simple prostatectomy for BPH in larger sized glands. Sixty patients were treated with transperitoneal laparoscopic prostatectomy with vascular control. The average prostate gland weight was 144.50±41.74 gm with mean operative time of 138.48±23.38 minutes and mean estimated blood loss of 330.98±149.52 mL. None of these patients experienced postoperative urinary incontinence 6. Van Velthoven et al. 7 reported their initial experience with laparoscopic extraperitoneal (Millin) retropubic prostatectomy in 18 patients. Their technique included hemostatic control of lateral venous vesicoprostatic pedicles, transverse anterior incision of the prostate capsule, adenoma enucleation using harmonic scalpel, and reconstruction of the posterior bladder neck and prostate capsule. Mean operative time was 145 minutes and mean blood loss 192 cc. Sotelo et al. published their experience with laparoscopic simple retropubic prostatectomy in 17 patients. This technique included transverse cystotomy just proximal to the prostatovesical junction, subcapsular development of the surgical plane, prostatic adenomectomy, prostatic fossa trigonization, and prostatic capsule suture repair. Mean operative time was 156 min (range 85-380 min). Mean blood loss was 516 mL (range 100-2500 mL). All patients reported complete continence during a follow-up period of 1 month to 2 years 8.
Baumert et al. 9 compared laparoscopic and open simple prostatectomy and concluded that laparoscopic simple prostatectomy was superior to open technique with regard to hospital stay, duration of urethral catheterization, and blood loss. Porpiglia et al. 10 also concluded that laparoscopic technique was comparable to that of open surgery but offered the advantage of lower peri-operative blood loss. As the experience of routine laparoscopic simple prostatectomy has increased, robot-assisted and single port laparoscopic techniques have been applied to the field with promising results 11.
A study by Pokorny et al presented the perioperative and short-term functional outcomes of robot-assisted simple prostatectomy in a large series of patients with lower urinary tract symptoms due to large benign prostatic enlargement treated in a high-volume referral center. The data indicated good perioperative outcomes, an acceptable risk profile, and excellent improvements in patient symptoms and flow scores at short-term follow-up following robot-assisted simple prostatectomy 12.
A study by Wang et al 13 that included 27 patients who underwent robotic-assisted urethra-sparing simple prostatectomy via an extraperitoneal approach reported short catheterization time, an acceptable risk profile, significantly improvements of voiding function and maintaining antegrade ejaculation following this urethral- sparing technique.
All these reports have demonstrated that laparoscopic prostatectomy for benign prostatic hyperplasia associated with a large protate gland is feasible and promising. However, with the exception of a single published case performed with robotic assistance, the prostatic urethra was not preserved during surgery, which can lead to retrograde ejaculation 6. In addition, with these techniques, bladder irrigation was needed in the vast majority of patients postoperatively. Also, urethral stricture may be a potential long-term complication of any procedure requiring excision and re-approximation of the prostatic urethra.
- Xing N, Guo Y, Yang F, et al. Laparoscopic simple prostatectomy with prostatic urethra preservation for benign prostatic hyperplasia. Transl Androl Urol. 2012;1(1):9–13. doi:10.3978/j.issn.2223-4683.2012.02.03 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4713215[↩]
- Simple prostatectomy. https://medlineplus.gov/ency/article/007416.htm[↩]
- Moslemi MK, Abedin Zadeh M. A modified technique of simple suprapubic prostatectomy: no bladder drainage and no bladder neck or hemostatic sutures. Urol J. 2010 Winter. 7(1):51-5.[↩]
- Simple Prostatectomy. https://emedicine.medscape.com/article/445996-overview[↩]
- Laparoscopic prostatectomy with vascular control for benign prostatic hyperplasia. Mariano MB, Graziottin TM, Tefilli MV. J Urol. 2002 Jun; 167(6):2528-9.[↩]
- Laparoscopic prostatectomy for benign prostatic hyperplasia–a six-year experience. Mariano MB, Tefilli MV, Graziottin TM, Morales CM, Goldraich IH. Eur Urol. 2006 Jan; 49(1):127-31; discussion 131-2.[↩][↩]
- Laparoscopic extraperitoneal adenomectomy (Millin): pilot study on feasibility. van Velthoven R, Peltier A, Laguna MP, Piechaud T. Eur Urol. 2004 Jan; 45(1):103-9; discussion 109.[↩]
- Laparoscopic retropubic simple prostatectomy. Sotelo R, Spaliviero M, Garcia-Segui A, Hasan W, Novoa J, Desai MM, Kaouk JH, Gill IS. J Urol. 2005 Mar; 173(3):757-60.[↩]
- Laparoscopic versus open simple prostatectomy: a comparative study. Baumert H, Ballaro A, Dugardin F, Kaisary AV. J Urol. 2006 May; 175(5):1691-4.[↩]
- Transcapsular adenomectomy(Millin): a comparative study, extraperitoneal laparoscopy versus open surgery. Porpiglia F, Terrone C, Renard J, Grande S, Musso F, Cossu M, Vacca F, Scarpa RM. Eur Urol. 2006 Jan; 49(1):120-6.[↩]
- Single-port transvesical simple prostatectomy: initial clinical report. Desai MM, Aron M, Canes D, Fareed K, Carmona O, Haber GP, Crouzet S, Astigueta JC, Lopez R, de Andrade R, Stein RJ, Ulchaker J, Sotelo R, Gill IS. Urology. 2008 Nov; 72(5):960-5.[↩]
- Pokorny M, Novara G, Geurts N, Dovey Z, De Groote R, Ploumidis A, et al. Robot-assisted simple prostatectomy for treatment of lower urinary tract symptoms secondary to benign prostatic enlargement: surgical technique and outcomes in a high-volume robotic centre. Eur Urol. 2015 Sep. 68 (3):451-7.[↩]
- Wang P, Xia D, Ye S, Kong D, Qin J, Jing T, et al. Robotic-assisted Urethra-sparing Simple Prostatectomy via an Extraperitoneal Approach. Urology. 2018 Jun 14.[↩]