How to treat a smashed finger
Smashed finger is an injury involving trauma to one or more fingers. If an injury to a finger occurs at the tip and does not involve the joint or nail bed, you may not need the help of a health care provider. Smashed finger, causing direct trauma to one or more fingers, should initially be treated with ice to reduce swelling. If blood builds up under a fingernail, a heated wire may be used to burn a hole through the nail. If only the tip of your finger bone is broken, your doctor may not recommend a splint.
Finger(s) can be smashed by a hammer blow, car door, desk drawer, baseball, or some other force.
Seek medical attention right away for any of the following:
- The finger is bent and you can’t straighten it.
- The injury is involves the palm or any of the joints, such as a finger or the wrist.
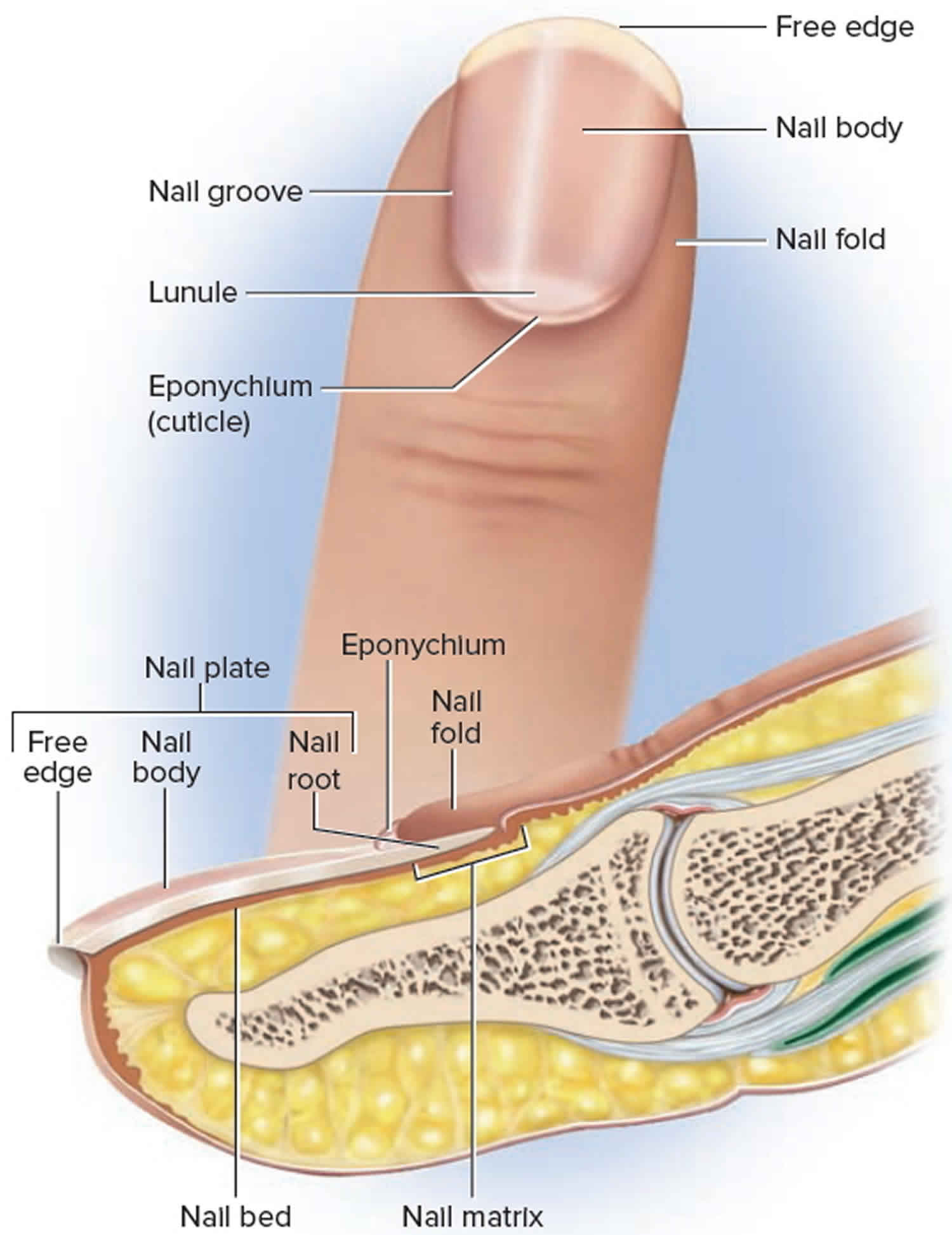
Figure 1. Fingernail anatomy
Smashed finger symptoms
Smashed finger symptoms may include any of the following:
- Difficulty moving the tip of the finger
- Discoloration or bruising of the finger or bleeding under the fingernail
- Finger pain from mild to severe
- Loss of fingernail
- Swelling
- Inflammation
- Redness
- Stiffness
- Movement difficulty
- Loss of sensation in the fingertip
Smashed finger types of injuries
Smashed finger injuries can be classified based on the nature and anatomic location of injury. By nature they may include simple or complex lacerations, avulsion injuries, amputations or associated paronychial injuries or fractures. A thorough assessment of the injury preferably under block or anaesthesia is essential to find the extent of damage so that repair or replacement of the injured structures can be made.
Smashed finger – closed injuries
Closed injuries to the fingernail can happen when there is a mild crushing of the finger tip as in a door crush injury or when a weight like hammer falls over it. This can result in a subungual hematoma – collection of blood between the nail bed and the nail plate.
Fingernails originate from the germinal matrix, and injury to this structure can result in permanent nail deformity. When assessing fingertip injuries, it is important to note the size and level of the defect as well as the presence or absence of exposed bone.
Traditionally it has been said that if the surface area of hematoma is less than 50% of the nail surface area or the patient is asymptomatic and if the X ray does not show any fracture it may be managed conservatively 1. If the surface area is more or if the patient is very symptomatic it requires drainage by drilling holes in the overlying nail using aseptic precautions to prevent chances of infection. Recent studies show that if the nail is not unduly elevated and not displaced it can be managed by trephination of the nail. The trephination can be done with a hot wire and less preferably by a large bore needle like 18 G needle which can injure the nail bed if not handled carefully 1.
If the X-ray shows any fractures it is better to remove the nail plate, look for the laceration and repair it using fine absorbable sutures such as 6-0/7-0 chromic cat gut 1.. This effort will by itself help a good reduction of fracture, more so in the case of children.
The wound heals in a period of 2 weeks and till that time it is covered with non-adherent dressings. The new nail will grow completely at around three months. Till a period of three weeks a protective splinting for the finger is advised either by a volar slab or a finger splint.
Replacing the nail plate is generally not recommended except in case of comminuted fracture of distal phalanx where it can splint the bone or in cases of lacerations in the nail bed and eponychial fold where its interpostition can prevent formation of synechiae between the nail bed and the eponychial fold. It is very important to prevent collection of blood underneath it to avoid any further complications such as infection. This can be done by making a hole in the nail in an area not overlying the nail bed laceration. The nail will be lifted off by the newly growing nail. If the nail plate is not available, a non-adherent gauze will do the same function. If available, mouldable meshed titanium plate can be used.
Figure 2. Smashed finger with subungual hematoma
Smashed finger with open injuries without nail bed loss
In these cases the fingernail plate may be partially or totally avulsed exposing the underlying laceration in the nail bed or the fracture sites. If the nail plate is still partially attached it may be removed using a blunt instrument between it and the nail bed gently. The management is similar to that which is described previously by suturing the nail bed and splinting the finger for three weeks when the fractures will heal. The amount of soft tissue attachment on the volar side may vary which determines the vascularity of the tip. Care should be taken not to disturb this attachment and jeopardize the vascularity of the finger tip. If the laceration extends on to the paronychium it has to be repaired meticulously. Even if the laceration is very complex, very often all the pieces survive if sutured meticulously.
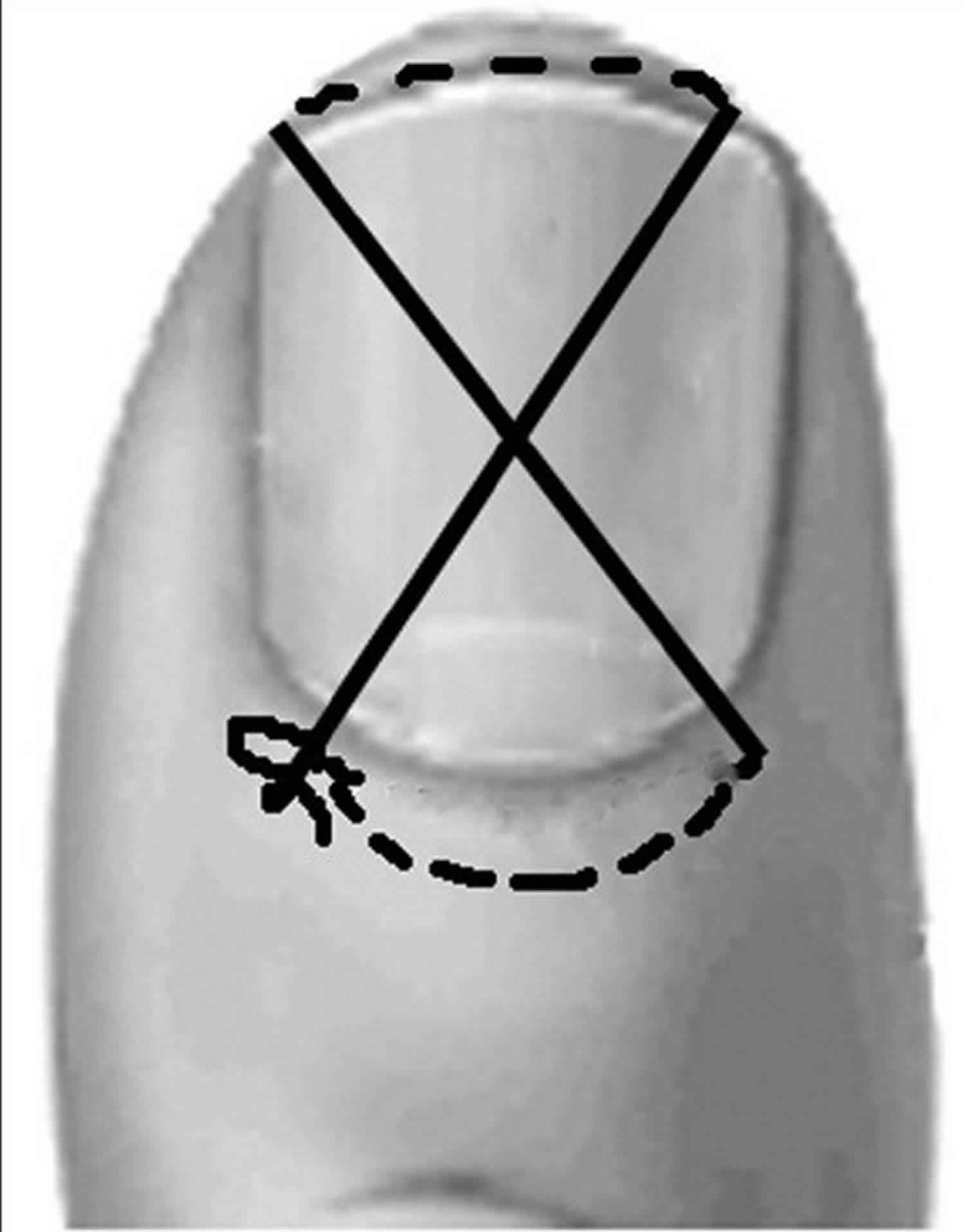
Approximately 50% of nail bed injuries are associated with distal phalangeal fracture. A majority of these are comminuted tuft fractures which do not need any specific treatment. Good approximation of the nail bed not only restores the good fracture reduction but also prevents scarring the nail bed which may give rise to deformities of nail like ridging or narrowing of the tip. If the injury is proximal it may need additional procedures like two parallel K wire fixation or placing the nail plate as a splint and anchoring it with a figure of 8 suture to retain it in place (Figure 3) 2.
Figure 3. Figure of 8 suture
Smashed finger with nail bed avulsions
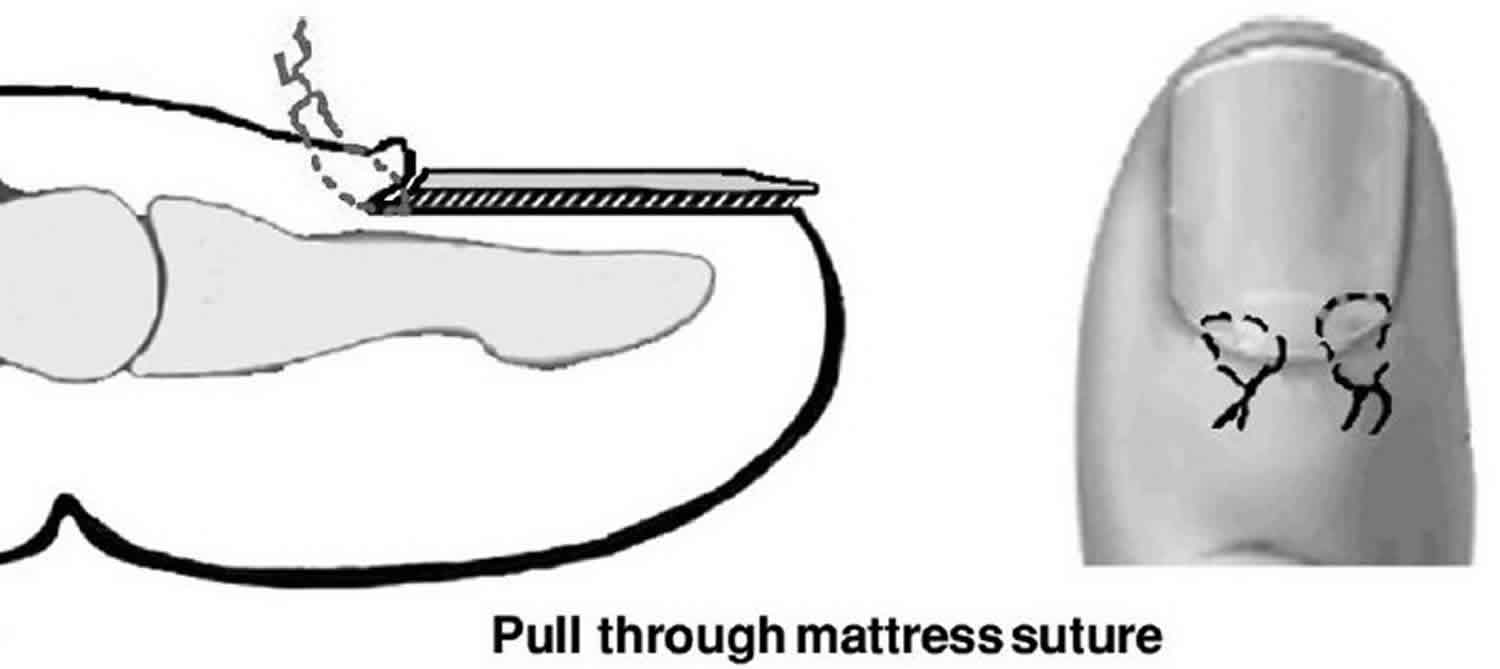
Sometimes the nail bed is intact but avulsed from the germinal matrix with the fracture of bone. In this case it is reattached to the sulcus using mattress sutures (Figure 4). This by itself will reduce the fracture and get the bone properly aligned and only very rarely a K wire is needed to the fix the fracture. If proximal nail bed is available it can be approximated with 6-0/7-0 chromic catgut.
Figure 4. Nail bed reinsertion
Smashed finger with nail bed loss
Nail bed is very essential for the growth of the nail and in its absence the nail cannot be adherent and can be deformed. Any area of nail bed loss can be managed by replacing it with a split thickness nail bed graft which can be harvested from the adjacent nail bed when the loss is very small or from the great toe nail when it is large. It is harvested using a 15 blade scalpel. These grafts take surprisingly well over the distal phalanx.
In case of loss of distal part of the nail bed if there is bony support it can be placed as a graft. If not the exposed bone can be covered with a local V-Y advancement flap and the nail bed graft may be placed over the advancing edge of the flap which gives gratifying results (Figure 5) 3.
In case of total loss of nail bed with scarring vascularised nail bed grafts can be used which transfer the nail from the great toe or second toe by microvascular transfer 4.
Figure 5. Amputated thumb tips
Footnote: (a) Stumps of both thumbs. (b) Amputated thumb tips. (c) After advancement of VY flaps. (d) With nail bed grafts in position. (e) Late postoperative picture with nail growth.
[Source 1 ]Mallet injury
A mallet finger deformity is a flexion deformity of the distal interphalangeal (DIP) joint caused by the disruption of the extensor mechanism, and is often the result of a direct end-on impact to the finger while in extension 5. Mallet finger deformity can also occur with the most trivial injuries that might not be immediately reported to the physician. X-ray scans should be obtained, as mallet fingers can be associated with avulsion fractures of the base of the distal phalanx where the extensor tendon inserts (Figure 6). Management of mallet finger deformities involves uninterrupted splinting of the DIP joint in hyperextension for 6 to 8 weeks, followed by another 4 weeks of night splinting 5. A 1.25-cm aluminum splint applied to the dorsum of the DIP joint prevents flexion of the DIP joint but permits flexion of the proximal interphalangeal joint 5. An alternative splint is the stack splint; however, this might not be superior to an aluminum splint 6. Most patients are able to return to work wearing the splint. Experts recommend that individuals keep the finger and splint dry, as moisture can macerate the skin. If the tape holding the splint in place becomes dirty, we advise leaving it in place and covering it with clean tape. Repeated removals of the splint increase the risk of recurrence of the mallet finger and should be discouraged. Referral should be considered if there is a bony avulsion involving more than one-third of the articular surface or if reduction is inadequate 7.
Figure 6. Mallet finger deformity
Tendon lacerations
Extensor tendon lacerations might be the result of direct laceration, crush injury, avulsion, burn, bite, or deep abrasion 8. Tendon lacerations are often easily visualized with manipulation of the joint and overlying skin. Closed-fist injuries involving teeth or “fight bites” are often missed because the laceration is proximal to the skin wound owing to the position of the clenched fist. An open wound over a knuckle should be considered a human bite until proven otherwise. These wounds should be left open and allowed to heal by secondary intention. Septic arthritis is a very serious complication of a human bite that requires urgent referral. An x-ray scan of the joint should be taken to rule out the presence of a broken tooth in the joint.
Management of extensor tendon lacerations should include tetanus prophylaxis and x-ray scans to rule out possible fractures and foreign bodies. After thorough irrigation and debridement, tendon lacerations should be repaired if the laceration is more than 50% of the tendon width, as these lacerations are at risk of delayed rupture 7.
Flexor tendon injuries can be closed or open injuries. Avulsion of the flexor digitorum profundus at the distal phalanx is known as Jersey finger. Clinical diagnosis can be made based on the inability to flex the distal interphalangeal (DIP) joint 9. Patients with flexor tendon injuries should be urgently referred to specialists because of the complex anatomy, proximity of the neurovascular bundles, and importance of a low-friction repair to ensure unrestricted tendon glide.
Fractures
As a general principle, all fractures need to be reduced to their anatomic position and protected with some type of splint or fixation until they heal 10. Management of closed fractures involves reduction and splinting for 3 to 4 weeks 11. An open fracture requires immediate referral to a hand surgeon. The wound should be irrigated, debrided, and loosely closed until the patient can be seen by a hand surgeon for definitive management.
Fractures of the middle and proximal phalanx might involve the shaft, condyles, or base. Unicondylar and bicondylar fractures are inherently unstable, and patients with such fractures should be referred to hand surgeons. Fractures of the shaft might be transverse, oblique, or spiral in nature (Figure 7). Nondisplaced fractures can be treated with splinting with the metacarpophalangeal joints in flexion and the interphalangeal joints in extension to prevent contractures 11. Closed reduction should be attempted for displaced, angulated, or rotated fractures. Transverse fractures of the phalanges are inherently unstable and require weekly x-ray scans if they are splinted to ensure that they have not displaced between visits. Patients with fractures that cannot be reduced or that involve the articular surface require referral for surgical fixation 11. Patients with intra-articular fractures should be referred if the articular surface reveals a step of more than 1 mm. Intra-articular fractures involving the base of the thumb metacarpal are known as Rolando or Bennett fractures and often require surgical fixation 12.
Figure 7. Oblique fracture of the proximal phalanx (anterior-posterior (left) and lateral (right) views)
Smashed finger treatment
Apply an ice pack to decrease swelling. Be sure to wrap the pack in a clean cloth first to prevent cold injury to the skin.
Over-the-counter pain medicines may help relieve discomfort. There are medications available over-the-counter (OTC) that can alleviate pain and reduce inflammation. Many are available to buy online, including:
- ibuprofen
- acetaminophen
If pain becomes severe, with blood under the fingernail, see your doctor. Your doctor may guide you in taking measures to relieve the pressure and prevent the fingernail from falling off.
DO NOT
- DO NOT splint a smashed finger without first consulting your provider.
- DO NOT drain blood from under the fingernail unless your doctor instructs you to do so.
- Bharathi RR, Bajantri B. Nail bed injuries and deformities of nail. Indian J Plast Surg. 2011;44(2):197-202. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3193631/[↩][↩][↩][↩]
- Patankar HS. Use of Modified Tension Band Sutures for Finger Nail Disruptions. J Hand Surg Eur Vol. 2007;32:668–74.[↩]
- Brown RE, Zook EG, Russell RC. Fingertip Reconstruction with Flaps and Nail Bed Grafts. J Hand Surg Am. 1999;24:345–51.[↩]
- Tamai S. Springer-Verlag Tokyo; 2003. Experimental and Clinical Reconstructive Microsurgery; pp. 384–7.[↩]
- Handoll HH, Vaghela MV. Interventions for treating mallet finger injuries. Cochrane Database Syst Rev. 2004;(3):CD004574[↩][↩][↩]
- Smit JM, Beets MR, Zeebregts CJ, Rood A, Welters CF. Treatment of options for mallet finger: a review. Plast Reconstr Surg. 2010;126(5):1624–9.[↩]
- Lalonde DH, Kozin S. Tendon disorders of the hand. Plast Reconstr Surg. 2011;128(1):1e–14e.[↩][↩]
- Cheung K, Hatchell A, Thoma A. Approach to traumatic hand injuries for primary care physicians. Can Fam Physician. 2013;59(6):614-8. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3681444[↩]
- Lehfeldt M, Ray E. MOC-PS CME article: treatment of flexor tendon laceration. Plast Reconstr Surg. 2008;121(4 Suppl):1–12[↩]
- Corley FG, Jr, Schenck RC., Jr Fractures of the hand. Clin Plast Surg. 1996;23(3):447–62[↩]
- Kozin SH, Thoder JJ, Lieberman G. Operative treatment of metacarpal and phalangeal shaft fractures. J Am Acad Orthop Surg. 2000;8(2):111–21[↩][↩][↩]
- Thumb trauma: Bennett fractures, Rolando fractures, and ulnar collateral ligament injuries. Carlsen BT, Moran SL. J Hand Surg Am. 2009 May-Jun; 34(5):945-52.[↩]