Taeniasis
Taeniasis is a parasitic infection in human caused by the tapeworm species beef tapeworm (Taenia saginata), pork tapeworm (Taenia solium), and Asian tapeworm (Taenia asiatica). Humans are the only definitive hosts for these three species. Adult tapeworms live in the human small intestine. Humans can become infected with these tapeworms by eating raw or undercooked beef (Taenia saginata) or pork (Taenia solium and Taenia asiatica). People with taeniasis may not know they have a tapeworm infection because symptoms are usually mild or nonexistent. Taenia solium tapeworm (pork tapeworm) infections can lead to cysticercosis, which is a disease that can cause seizures, so it is important seek treatment. Cysticercosis is a parasitic tissue infection caused by larval cysts of the tapeworm Taenia solium (pork tapeworm). These larval cysts infect brain, muscle, or other tissue, and are a major cause of adult onset seizures in most low-income countries. A person gets cysticercosis by swallowing eggs found in the feces of a person who has an intestinal pork tapeworm (Taenia solium). People living in the same household with someone who has a pork tapeworm (Taenia solium) have a much higher risk of getting cysticercosis than people who don’t. People do not get cysticercosis by eating undercooked pork. Eating undercooked pork can result in intestinal pork tapeworm if the pork contains larval cysts. Pigs become infected by eating tapeworm eggs in the feces of a human infected with a pork tapeworm (Taenia solium).
People get cysticercosis when they swallow Taenia solium (pork tapeworm) eggs that are passed in the feces of a human with a pork tapeworm (Taenia solium). Tapeworm eggs are spread through food, water, or surfaces contaminated with feces. Humans swallow the eggs when they eat contaminated food or put contaminated fingers in their mouth. Importantly, someone with a tapeworm can infect him-or herself with tapeworm eggs (this is called autoinfection), and can infect others in the family. Eating pork cannot give you cysticercosis.
Taenia saginata (beef tapeworm) and Taenia solium (pork tapeworm) are worldwide in distribution. Taenia solium (pork tapeworm) is more prevalent in poorer communities where humans live in close contact with pigs and eat undercooked pork. The highest rates of infection are found in areas of Latin America, Asia, and Africa that have poor sanitation and free-ranging pigs that have access to human feces. Although uncommon, cysticercosis can occur in people who have never traveled outside of the United States. For example, a person infected with a tapeworm who does not wash his or her hands might accidentally contaminate food with tapeworm eggs while preparing it for others. Taenia asiatica (Asian tapeworm) is limited to Asia and is seen mostly in the Republic of Korea, China, Taiwan, Indonesia, and Thailand.
Taeniasis causes
Humans become infected by eating raw or undercooked infected beef or pork. Once ingested, cysticerci attach to the small intestine and develop into adult tapeworms over the course of 2 months. The adult tapeworms produce proglottids that mature, detach, and migrate to the anus and are then passed in the feces. Taeniasis is endemic in countries where both Taenia saginata and Taenia solium are common and public hygiene is poor.
Cysticercosis, which is caused by ingesting eggs of Taenia solium (pork tapeworm), occurs when larvae are deposited in skeletal muscle, brain, eyes, and other organs.
Taenia saginata (beef tapeworm) are usually 4-12 m in length, but can grow to be 25 m; the adult tapeworms produce 1,000 to 2,000 proglottids/ worm and may produce up to 100,000 eggs per worm.
Taenia solium (pork tapeworm) are smaller, 2-8 m in length, produce an average of 1,000 proglottids/worm, and may produce 50,000 eggs per worm.
Taenia asiatica (Asian tapeworm) range in size from 4-8 m, produce 700 proglottids/worm and may produce 80,000 eggs per proglottid.
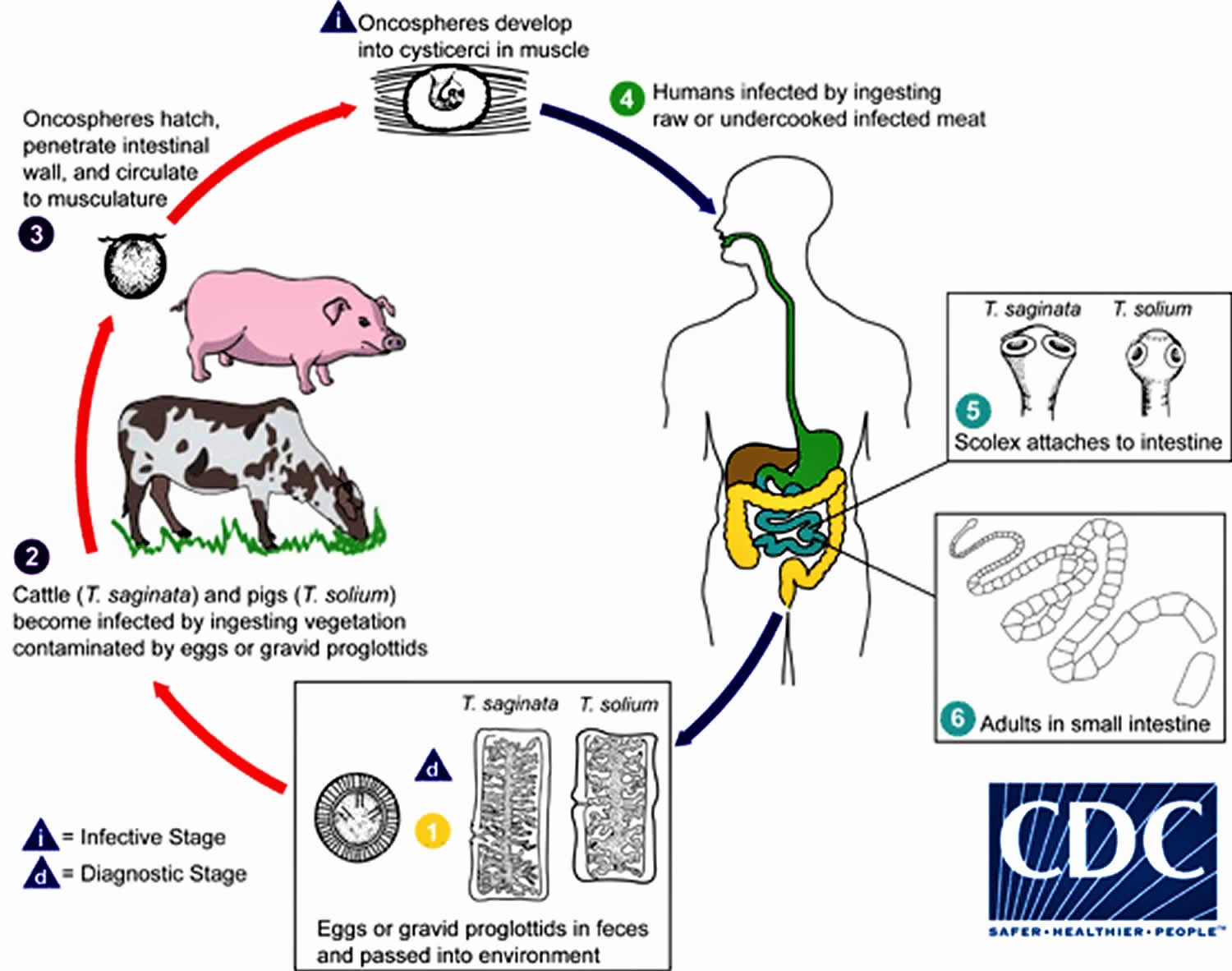
Taeniasis life cycle
Taeniasis is the infection of humans with the adult tapeworm of Taenia saginata, Taenia solium or Taenia asiatica. Humans are the only definitive hosts for these three species. Eggs or gravid proglottids are passed with feces (number #1); the eggs can survive for days to months in the environment. Cattle (Taenia saginata) and pigs (Taenia solium and Taenia asiatica) become infected by ingesting vegetation contaminated with eggs or gravid proglottids (number #2). In the animal’s intestine, the oncospheres hatch (number #3), invade the intestinal wall, and migrate to the striated muscles, where they develop into cysticerci. A cysticercus can survive for several years in the animal. Humans become infected by ingesting raw or undercooked infected meat (number #4). In the human intestine, the cysticercus develops over 2 months into an adult tapeworm, which can survive for years. The adult tapeworms attach to the small intestine by their scolex (number #5) and reside in the small intestine (number #6). Length of adult worms is usually 5 m or less for Taenia saginata (however it may reach up to 25 m) and 2 to 7 m for Taenia solium. The adults produce proglottids which mature, become gravid, detach from the tapeworm, and migrate to the anus or are passed in the stool (approximately 6 per day). Taenia saginata adults usually have 1,000 to 2,000 proglottids, while Taenia solium adults have an average of 1,000 proglottids. The eggs contained in the gravid proglottids are released after the proglottids are passed with the feces. Taenia saginata may produce up to 100,000 and Taenia solium may produce 50,000 eggs per proglottid respectively.
Figure 1. Taeniasis life cycle
Taeniasis prevention
- Wash your hands with soap and warm water after using the toilet, changing diapers, and before handling food
- Teach children the importance of washing hands to prevent infection
- Wash and peel all raw vegetables and fruits before eating
- Use good food and water safety practices while travelling in developing countries such as:
- Drink only bottled or boiled (1 minute) water or carbonated (bubbly) drinks in cans or bottles
- Filter unsafe water through an “absolute 1 micron or less” filter AND dissolve iodine tablets in the filtered water; “absolute 1 micron” filters can be found in camping and outdoor supply stores.
Prevention and control of Taenia solium infection as recommended by World Health Organization 2019 1
- Mass drug administration for taeniasis
- Identification and treatment of taeniasis cases
- Health education, including hygiene and food safety
- Improved sanitation
- Improved cultivation and production of pig
- Anthelmintic treatment of pigs (oxfendazole)
- Vaccination of pigs (TSOL18 vaccine)
- Improved meat inspection and processing of meat products
Taeniasis symptoms
Taeniasis due to Taenia solium, Taenia saginata or Taenia asiatica is usually characterized by mild and non-specific symptoms. Because of the large size of Taenia saginata tapeworms (beef tapeworm), Taenia saginata taeniasis is more frequently symptomatic compared to Taenia solium (pork tapeworm) or Taenia asiatica (Asian tapeworm) taeniasis. Typical symptoms of Taenia saginata (beef tapeworm) taeniasis include mild epigastric discomfort, nausea, flatulence, diarrhea, constipation or hunger pains may arise when the tapeworms become fully developed in the intestine, approximately 8 weeks after ingestion of meat containing cysticerci. In some instances, passage (active and passive) of tapeworm proglottids through the anus and in the feces. Occasionally, appendicitis or cholangitis can result from migrating proglottids that may become lodged in the appendiceal lumen, or bile or pancreatic ducts. Taenia solium (pork tapeworm) taeniasis is less frequently symptomatic than Taenia saginata taeniasis. The main symptom is often the passage (passive) of proglottids. These symptoms may continue until the tapeworm dies following treatment, otherwise it may live for a number of years. It is considered that untreated infections with Taenia solium tapeworms generally persist for 2–3 years.
The most important feature of Taenia solium (pork tapeworm) taeniasis is the risk of development of cysticercosis. Cysticercosis is a parasitic tissue infection caused by larval cysts of the tapeworm Taenia solium (pork tapeworm). These larval cysts infect brain, muscle, or other tissue, and are a major cause of adult onset seizures in most low-income countries. A person gets cysticercosis by swallowing eggs found in the feces of a person who has an intestinal tapeworm. People living in the same household with someone who has a tapeworm have a much higher risk of getting cysticercosis than people who don’t. People do not get cysticercosis by eating undercooked pork. Eating undercooked pork can result in intestinal tapeworm if the pork contains larval cysts. Pigs become infected by eating tapeworm eggs in the feces of a human infected with a pork tapeworm (Taenia solium).
Cysticercosis signs and symptoms
Cysticercosis signs and symptoms will depend on the location and number of cysts in your body.
- Cysts in the muscles: Cysts in the muscles generally do not cause symptoms. However, you may be able to feel lumps under your skin. The lumps sometimes become tender.
- Cysts in the eyes: Although rare, cysts may float in the eye and cause blurry or disturbed vision. Infection in the eyes may cause swelling or detachment of the retina.
- Neurocysticercosis (cysts in the brain, spinal cord): Symptoms of neurocysticercosis depend upon where and how many cysts are found in the brain. Seizures and chronic headaches are the most common symptoms. However, confusion, lack of attention to people and surroundings, difficulty with balance, excess fluid around the brain (called hydrocephalus) may also occur. Symptoms may also include blindness, meningitis, dementia, and symptoms caused by lesions occupying spaces of the central nervous system. Changes in personality and mental status occur more often in adults than in children, behavioral changes and learning disabilities were reported in a study of 25 affected children 2. The disease can result in death.
Symptoms can occur months to years after infection, usually when the cysts start dying. When cysts die, the brain or other tissue around the cyst may swell. The pressure of the swelling is what usually causes the symptoms of the infection. Sometimes symptoms are caused by the pressure of cyst in a small space.
In some endemic regions (particularly in Asia), infected people may develop visible or palpable nodules (a small solid bump or node that can be detected by touch) beneath the skin (subcutaneous).
Taeniasis diagnosis
Your health care provider will ask you about your symptoms, where you have traveled, and the kinds of foods you eat.
Microscopic identification of eggs and proglottids in feces is diagnostic for taeniasis; however, eggs and proglottids are not released into the feces until approximately 2 to 3 months after the adult tapeworm is established in the upper jejunum. Repeated examination and concentration techniques will increase the likelihood of detecting light infections. Examination of 3 stool samples collected on different days is recommended to increase the sensitivity of microscopic methods. Eggs of Taenia spp. cannot be differentiated; a species determination may be possible if mature, gravid proglottids (or, more rarely, examination of the scolex) are present.
Recently developed coproantigen and molecular assays are more sensitive than stool examination, but these assays are not yet available outside of the research laboratory. Serologic methods, which are available only in research settings, may be used to identify Taenia solium tapeworm carriers.
Household contacts of neurocysticercosis cases should be evaluated for taeniasis to reduce the risk of cysticercosis.
Diagnosis of neurocysticercosis is usually made by MRI or CT brain scans. Blood tests are available to help diagnose an infection, but may not always be accurate. If surgery is necessary to remove a cyst, the diagnosis can be made by the pathologist who looks at the cyst.
An enzyme-linked immunotransfer blot (EITB) assay is the test of choice to confirm the diagnosis of neurocysticercosis indicated by clinical and radiologic findings. Test specificity is 100% and sensitivity is 90% with more than 2 lesions; sensitivity declines to 50-70% with a solitary lesion. Therefore, enzyme-linked immunotransfer blot (EITB) assay may have limited value for children because most present with a single lesion. A serum immunoblot assay is more sensitive than the assay using CSF, thus obtaining CSF solely for that purpose is unnecessary.
Although an enzyme-linked immunosorbent assay (ELISA) can be performed on both CSF and serum, CSF provides better reliability. ELISA may provide either false-positive or false-negative results. ELISA provides a reported sensitivity of 75%. ELISA can aid in diagnosis in patients with few CNS lesions and relatively mild disease. Newer serologic methods may allow improved diagnostic testing 3.
Laboratory diagnosis
Microscopy
Microscopic identification of eggs and proglottids in feces is diagnostic for taeniasis, but is not possible during the first 3 months following infection, prior to development of adult tapeworms. Repeated examination and concentration techniques will increase the likelihood of detecting light infections. Nevertheless, identification of Taenia is not possible if solely based on microscopic examination of eggs, because all Taenia species produce eggs that are morphologically identical. Eggs of Taenia spp. are also indistinguishable from those produced by cestodes of the genus Echinococcus (tapeworms of dogs and other canid hosts). Microscopic identification of gravid proglottids (or, more rarely, examination of the scolex) allows species determination.
Separation of Taenia saginata and Taenia solium is best accomplished by examination of mature proglottids. Taenia saginata has 12-30 primary lateral uterine branches, while Taenia solium has 7-13 primary lateral uterine branches. Visualization of the branches can be improved by clearing the specimen in lactophenol followed by India ink injection into the lateral genital pore. The procedure is as follows:
- Clear the formalin-fixed proglottids in lactophenol (50/50 liquefied phenol crystals in lactic acid) for at least 30 minutes (thicker specimen may take a few hours to overnight).
- Gently sandwich the proglottids between two glass microscope slides, with the genital pore exposed along the edge of the two slides.
- Using a small gauge (25 or 27 g) tuberculin syringe, slowly inject India ink into the genital pore.
- Allow the ink to flow down the uterine stem and into the primary uterine branches.
- Count the number of primary uterine branches to determine the species (7-13 for Taenia solium and 12-30 for Taenia saginata).
Antibody detection
May prove useful especially in the early invasive stages, when the eggs and proglottids are not yet apparent in the stools.
Copro-Ag ELISA can be used to detect Taenia solium tapeworm carrier with sensitivity of 84.5% and specificity of 92% 4.
Molecular analysis
- Copro-PCR has been used to detect Taenia solium carrier with sensitivity of 82.7% and specificity of 99% 4.
- Multiplex loop-mediated isothermal amplification (multiplex LAMP) targeting mitochondrial cytochrome c oxidase subunit 1 ( cox 1) gene couple with dot enzyme-linked immunosorbent assay (dot-ELISA) help identify human Taenia species ( Taenia solium, Taenia saginata and Taenia asiatica). This technique is easy to perform and interpret and does not require expensive equipment which make it feasible to perform in resource-limited settings 5. Unfortunately, these molecular methods are not commercially available.
Taeniasis treatment
Praziquantel is the medication most often used to treat active taeniasis, given at 5-10 mg/kg orally once for adults and 5-10 mg/kg orally once for children. If the patient has cysticercosis in addition to taeniasis, praziquantel should be used with caution. Praziquantel is cysticidal and can cause inflammation around dying cysts in those with cysticercosis, which may lead to seizures or other symptoms. Niclosamide is an alternative, given at 2 g orally once for adults and 50 mg/kg orally once for children. After treatment, stools should be collected for 3 days to search for tapeworm proglottids for species identification. Stools should be re-examined for Taenia eggs 1 and 3 months after treatment to be sure the infection is cleared.
Oral praziquantel is available for human use in the United States.
Niclosamide is NOT available for human use in the United States.
In neurocysticercosis, since the destruction of cysts may lead to an inflammatory response, treatment of active disease may include long courses with praziquantel and/or albendazole, as well as supporting therapy with corticosteroids and/or anti-epileptic drugs, and possibly surgery. The dosage and the duration of treatment can vary greatly and depend mainly on the number, size, location and developmental stage of the cysts, their surrounding inflammatory edema, acuteness and severity of clinical symptoms or signs.
Praziquantel
Note on treatment in pregnancy
Pregnancy Category B: Either animal-reproduction studies have not demonstrated a fetal risk but there are no controlled studies in pregnant women or animal-reproduction studies have shown an adverse effect (other than a decrease in fertility) that was not confirmed in controlled studies in women in the first trimester (and there is no evidence of a risk in later trimesters).
Praziquantel is pregnancy category B. There are no adequate and well-controlled studies in pregnant women. However, the available evidence suggests no difference in adverse birth outcomes in the children of women who were accidentally treated with praziquantel during mass prevention campaigns compared with those who were not. In mass prevention campaigns for which the World Health Organization (WHO) has determined that the benefit of treatment outweighs the risk, WHO encourages the use of praziquantel in any stage of pregnancy. For individual patients in clinical settings, the risk of treatment in pregnant women who are known to have an infection needs to be balanced with the risk of disease progression in the absence of treatment.
Note on treatment during breastfeeding
Praziquantel is excreted in low concentrations in human milk. According to WHO guidelines for mass prevention campaigns, the use of praziquantel during lactation is encouraged. For individual patients in clinical settings, praziquantel should be used in breast-feeding women only when the risk to the infant is outweighed by the risk of disease progress in the mother in the absence of treatment.
Note on treatment in children
The safety of praziquantel in children aged less than 4 years has not been established. Many children younger than 4 years old have been treated without reported adverse effects in mass prevention campaigns and in studies of schistosomiasis. For individual patients in clinical settings, the risk of treatment of children younger than 4 years old who are known to have an infection needs to be balanced with the risk of disease progression in the absence of treatment.
Niclosamide
Note on treatment in pregnancy
Pregnancy Category B: Either animal-reproduction studies have not demonstrated a fetal risk but there are no controlled studies in pregnant women or animal-reproduction studies have shown an adverse effect (other than a decrease in fertility) that was not confirmed in controlled studies in women in the first trimester (and there is no evidence of a risk in later trimesters).
Niclosamide is in pregnancy category B. Data on the use of niclosamide in pregnant women are limited. Niclosamide is not thought to be systemically absorbed. Niclosamide should be used during pregnancy only if the potential benefit justifies the potential risk to the fetus.
Note on treatment during breastfeeding
It is not known whether niclosamide is excreted in breast milk, although niclosamide is not thought to be systemically absorbed. The World Health Organization (WHO) classifies niclosamide as compatible with breastfeeding, although data on the use of niclosamide during lactation are limited.
Note on treatment in children
The safety of niclosamide in children has not been established, although niclosamide is not thought to be systemically absorbed. Available evidence suggests that the safety profiles are comparable in children 2 years or older and adults.
References- World Health Organization. Taeniasis/cysticercosis. 18 June 2019. https://www.who.int/news-room/fact-sheets/detail/taeniasis-cysticercosis
- Morales NM, Agapejev S, Morales RR, Padula NA, Lima MM. Clinical aspects of neurocysticercosis in children. Pediatr Neurol. 2000 Apr. 22(4):287-91.
- Lee YM, Handali S, Hancock K, Pattabhi S, Kovalenko VA, Levin A, et al. Serologic diagnosis of human Taenia solium cysticercosis by using recombinant and synthetic antigens in QuickELISA™. Am J Trop Med Hyg. 2011 Apr. 84(4):587-93.
- Praet N, Verweij JJ, Mwape KE, et al. Bayesian modelling to estimate the test characteristics of coprology, coproantigen ELISA and a novel real-time PCR for the diagnosis of taeniasis. Trop Med Int Health. 2013 Mar 7. 18(5):608-14.
- Nkouawa A, Sako Y, Okamoto M, Ito A. Simple Identification of Human Taenia Species by Multiplex Loop-Mediated Isothermal Amplification in Combination with Dot Enzyme-Linked Immunosorbent Assay. Am J Trop Med Hyg. 2016 Jun 1. 94(6):1318–1323.