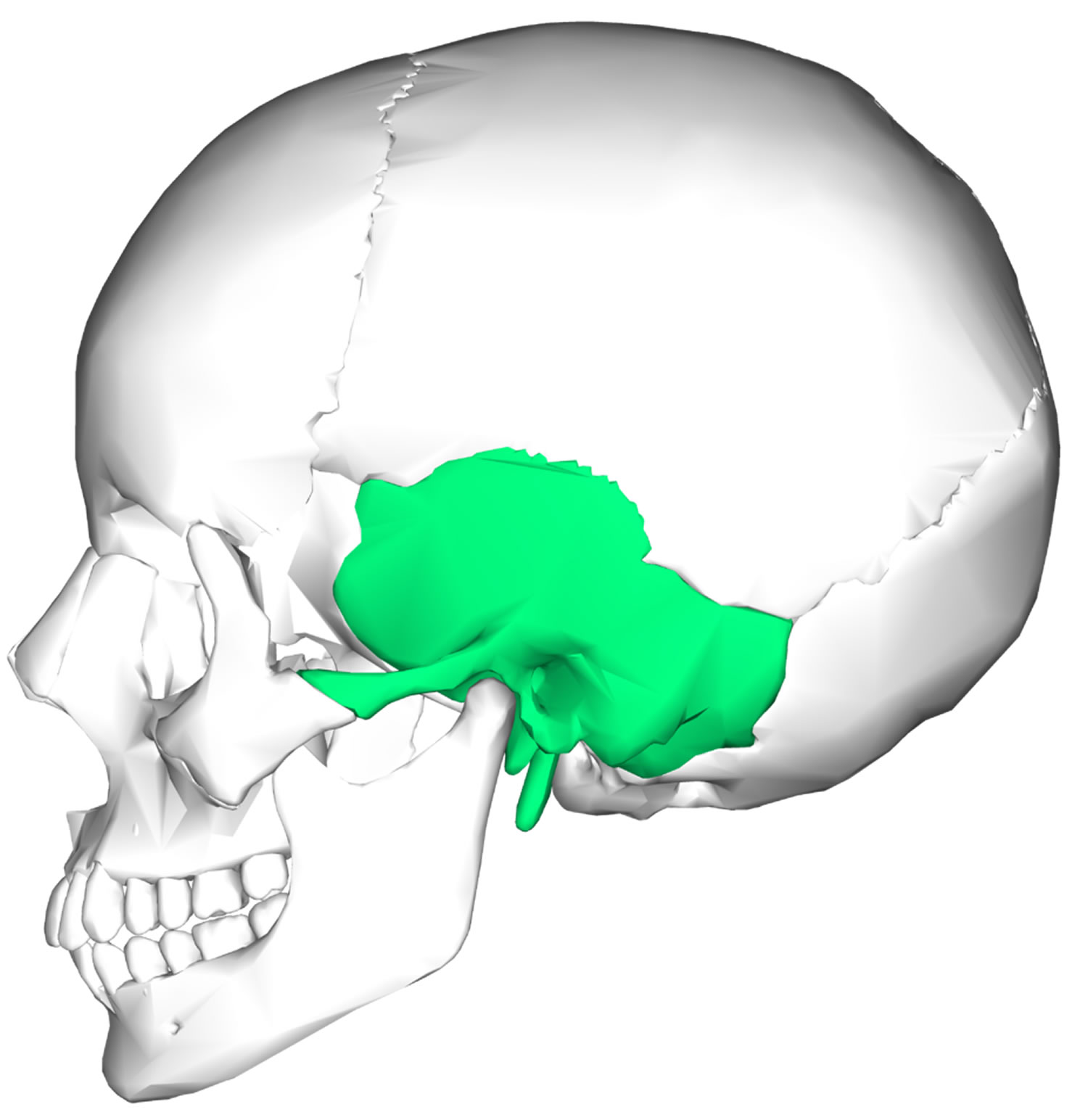
Temporal bone
The temporal bone is a paired component of the skull base. The temporal bones are the thickest skull base components. The temporal bone is best viewed laterally (Figure 1). The temporal bone lies inferior to the parietal bone and form the inferolateral region of the skull and parts of the cranial floor. The temporal bones articulate posteriorly with the occipital bone, superiorly with the parietal bones, and anteriorly with the sphenoid bone creating the occipitomastoid, squamous and sphenosquamosal sutures, respectively. The terms temporal and temple, from the Latin word for “time,” refer to the fact that gray hairs, a sign of time’s passage, appear first at the temples. Each temporal bone has an intricate shape and is described in terms of its three major parts: the squamous, tympanic, and petrous parts.
Temporal bones house numerous nerves, therefore, fracture of the temporal bone carries a risk of concomitant functional deficits.
Temporal bones also house the internal carotid arteries and internal jugular veins, which play a role supplying oxygenated blood and venous drainage to and from the brain.
Figure 1. Temporal bone
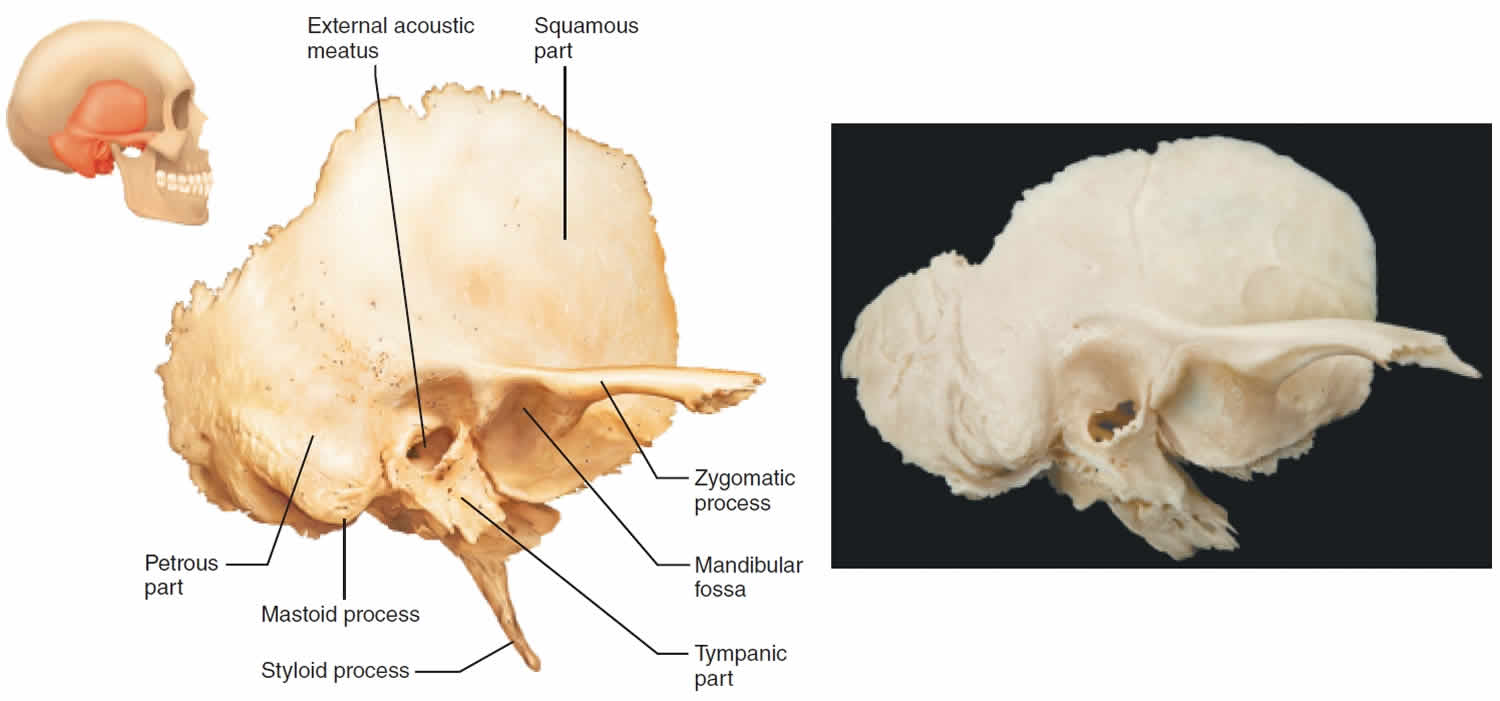
Temporal bone anatomy
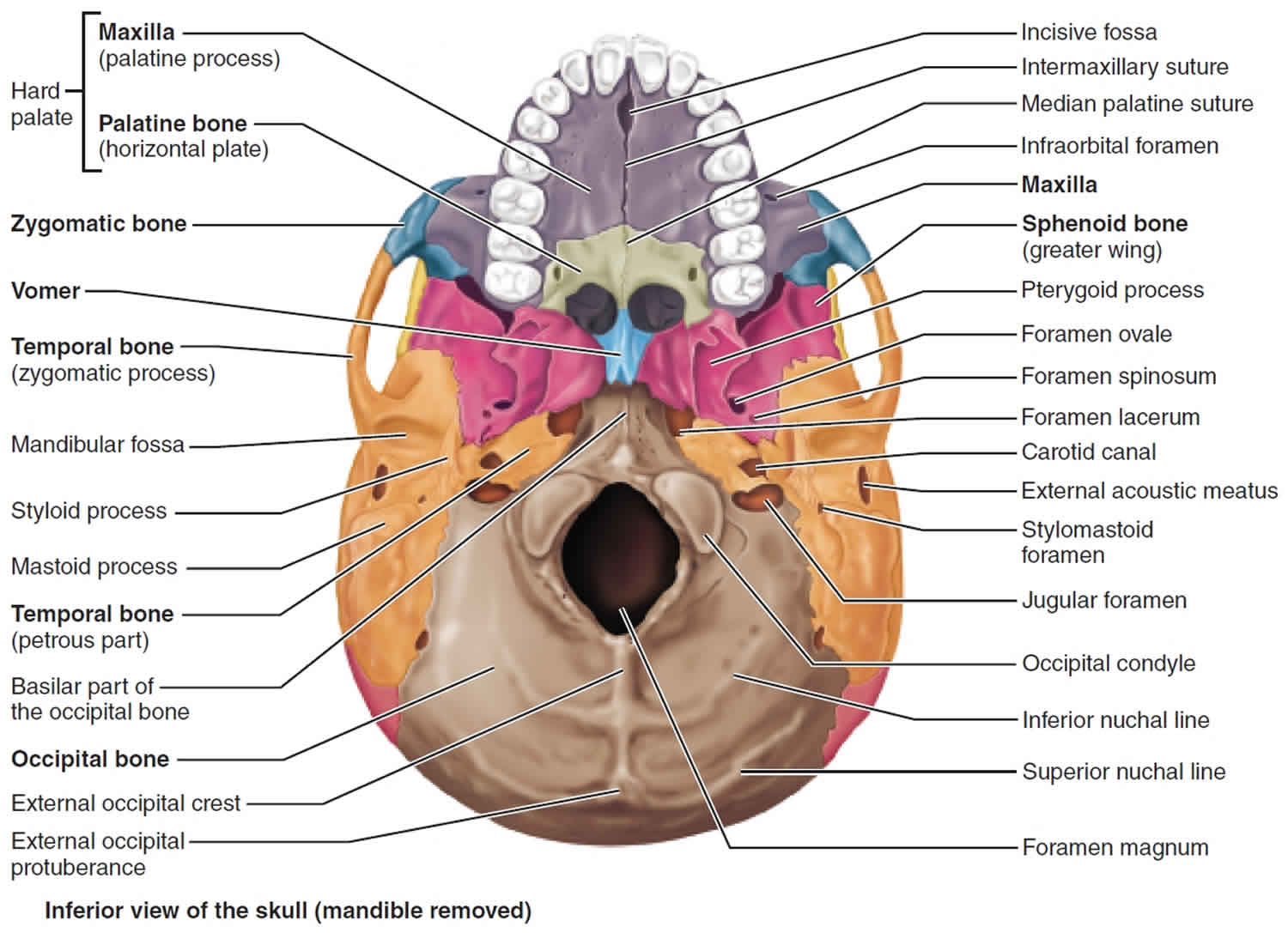
The temporal bone has complex anatomy including four geographic parts (squamous, mastoid, petrous, tympanic) and numerous foramen/canals (foramen lacerum, carotid canal, internal acoustic meatus, jugular foramen).
- Foramen lacerum: Great petrosal nerve
- Carotid canal: Internal carotid artery
- Internal acoustic meatus: Cranial nerve VII and cranial nerve VIII
- Jugular foramen: Internal jugular vein, posterior meningeal artery, cranial nerve IX, cranial nerve X and cranial nerve XI
Additionally, there are 3 bony processes (zygomatic, mastoid, styloid).
Figure 2. Parts of temporal bone
Parts of temporal bone
Temporal bone consists of five parts:
- Squamous part
- Mastoid portion
- Petrous portion
- Tympanic part
- Styloid process (temporal)
The plate-shaped squamous part (Figure 2) abuts the squamous suture. It has a barlike zygomatic process (“cheek”) that projects anteriorly to meet the zygomatic bone of the face. Together, these two bony structures form the zygomatic arch, commonly called the cheek bone. The oval mandibular fossa on the inferior surface of the zygomatic process receives the condylar process of the mandible (lower jawbone), forming the freely movable temporomandibular joint (jaw joint).
The tympanic (“eardrum”) part surrounds the external acoustic meatus, or external ear canal. It is through this canal that sound enters the ear. The external acoustic meatus and the tympanic membrane (eardrum) at its deep end are parts of the external ear. In a dried skull, the tympanic membrane has been removed. Thus, part of the middle ear cavity deep to the tympanic region may be visible through the meatus.
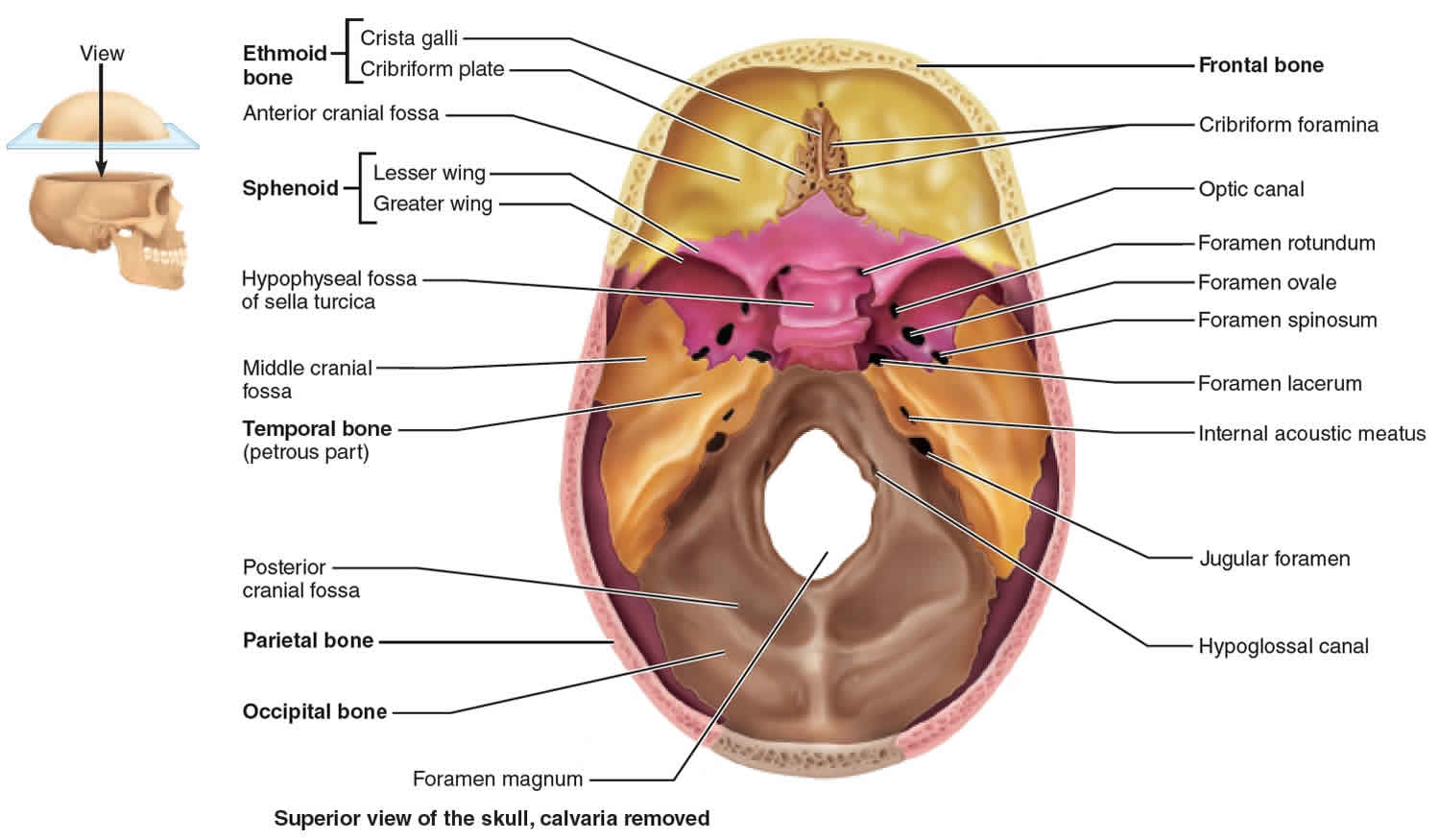
The petrous (“rocky”) part of the temporal bone contributes to the cranial base. It forms a bony wedge between the occipital bone posteriorly and the sphenoid bone anteriorly (Figure 3). From within the cranial cavity this very dense region looks like a mountain ridge (Figure 3). The posterior slope of this ridge lies in the posterior cranial fossa, whereas the anterior slope is in the middle cranial fossa, the fossa that holds the temporal lobes of the brain. Housed inside the petrous part are the cavities of the middle and inner ear, which contain the sensory apparatus for hearing and balance.
Several foramina penetrate the petrous part (Figure 3). The large jugular foramen is located where the petrous part joins the occipital bone. Through this foramen pass the largest vein of the head, the internal jugular vein, and cranial nerves IX, X, and XI. The carotid canal opens on the skull’s inferior aspect, just anterior to the jugular foramen. The internal carotid artery, the main artery to the brain, passes through it into the cranial cavity. The foramen lacerum (“lacerated”) is a jagged opening between the medial tip of the petrous part of the temporal bone and the sphenoid bone. This foramen is almost completely closed by cartilage in a living person. The internal acoustic meatus lies in the cranial cavity on the posterior face of the petrous part. It transmits cranial nerves VII and VIII, the facial and vestibulocochlear nerves.
Projecting inferiorly from the petrous part of the temporal bone is the needle-like styloid process (“stakelike”). This process is an attachment point for some muscles of the tongue and pharynx and for a ligament that connects the skull to the hyoid bone of the neck.
Lateral and posterior to the styloid process is the prominent mastoid process (mastoid; “breast-shaped”), an anchoring site for some neck muscles. This process can be felt as a lump just posterior to the ear. The stylomastoid foramen is located between the styloid and mastoid processes. A branch of cranial nerve VII, the facial nerve, leaves the skull through this foramen.
The mastoid process is full of air sinuses called mastoid air cells, which lie just posterior to the middle ear cavity. Infections can spread from the throat to the middle ear to the mastoid cells. Such an infection, called mastoiditis, can even spread to the brain, from which the mastoid air cells are separated by only a thin roof of bone. This was a serious problem before the late 1940s, when antibiotics became available.
Figure 3. Petrous part of temporal bone
Temporal bone fracture
Temporal bone fractures are caused by a lateral force/impact to the cranium 1. Temporal bones are the thickest skull base bones and require a great force to fracture. Dynamic loading studies have yielded a minimum lateral impact force of 6000 to 8000 Newton (N) necessary to cause a temporal bone fracture 2. As with all fractures, the fracture force chooses a path of least resistance, which often means disrupting native temporal bone foramina. Temporal bone fractures can lead to high morbidity and/or mortality.
Roughly one-third of temporal bone fractures in the general population are as a result of motor vehicle accidents, assaults, and falls. About a quarter of temporal bone fractures are attributed to sports injuries, gunshot wounds, bicycle accidents, and other miscellaneous injuries. Males are at least 3-times more likely as females to suffer temporal bone fractures. Temporal bone fractures are typically unilateral, and more than half of temporal bone fractures are considered “open” fractures 3.
Any history of significant trauma to the head, especially that with associated loss of consciousness, should elicit suspicion for cranial bone fractures. On physical examination, patients with temporal bone fractures may present with hemorrhagic otorrhea, hemotympanum, vertigo, nystagmus, facial paralysis, and/or Battle’s sign (bruising over the mastoid process) 4. Patients will often present with altered mental status or abnormal Glasgow coma scale (GCS) scores secondary to concomitant, acute, intracranial pathology.
Temporal bone fractures key points
- Temporal bones require an immense amount of lateral force to fracture.
- Look for hemorrhagic otorrhea, hemotympanum, nystagmus, facial paralysis, Battle’s sign.
- Fractures should be classified as either otic capsule sparing or violating.
- High-resolution non-contrast CT with slice thickness less than or equal to 1.5 mm is the modality of choice.
- Look for associated intracranial and cervical pathology.
- Once stabilized, temporal bone fracture complications can be treated.
- Common complications include facial nerve paralysis, CSF leak, hearing loss, vertigo.
- Some complications may self-remit, and treatment options exist for those that persist.
Temporal bone fracture diagnosis
Imaging plays a crucial role in the evaluation and subsequent management of temporal bone fractures. CT has a significantly higher sensitivity for temporal bone fractures than a physical examination 5. A non-contrast high-resolution CT with less than 1.5-mm slice thickness and coronal/sagittal reconstructions is recommended. Temporal bone fractures have an exceedingly high association with intracranial injury. Along with the careful evaluation of the osseous structures, the brain should be scrutinized for a possible subdural/epidural hematoma, cerebral contusion and/or hemorrhage, subarachnoid hemorrhage and tension pneumocephalus. Trauma to the head necessitates evaluation of the cervical spine. CT angiography should be obtained in the assessment of the intracranial vasculature, specifically the temporal portion of the internal carotid artery. Cisternograms are utilized to diagnose and localize cerebrospinal fluid (CSF) leaks.
Once the patient is stable, an MRI can be obtained for patients who suffer cranial nerve palsy not explained by CT findings, and patients that will require surgical intervention for temporal bone fracture. MRI can help differentiate between a fluid-filled mastoid and a mastoid containing herniated intracranial contents. MRI may also reveal intracranial pathology not previously diagnosed on CT 6.
The first temporal bone fracture classification system described 2 types of fractures dependent on the plane relative to the long axis of the petrous ridge: Fractures that course parallel are considered longitudinal and fractures that course perpendicular are considered transverse 7. A more clinically relevant classification describes fractures relative to the otic capsule involvement. Fractures are either otic capsule sparing or otic capsule violating. Temporal bone fractures that violate the otic capsule have a much higher association with CSF leak, sensorineural hearing loss, and certain intracranial pathology 8.
Electromyography and electroneuronography can be used in cases of immediate facial paralysis.
Temporal bone fracture complications
- Facial paralysis: cranial nerve VII damage
- Sensorineural hearing loss: cranial nerve VIII damage
- Conductive hearing loss: Ossicle/tympanic membrane disruption, hemotympanum
- Vertigo: cranial nerve VIII damage, perilymph fistula, post-traumatic perilymphatic hydrops
- CSF leak
- Cranial nerve palsies: cranial nerves IX, X, XI
- Internal carotid artery dissection and/or thrombus
- Meningocele
- Cholesteatoma
Temporal bone fracture treatment
Treatment and management of associated life-threatening, intracranial pathology should be the primary focus. The management of temporal bone fracture complications should be addressed once the patient is stable.
Facial nerve paralysis
Immediate paralysis and/or significant degeneration on electroneuronography is more likely to reflect nerve transection which requires surgical repair. Delayed onset paralysis usually indicates the development of neural edema or compression by hematoma which can be treated with 1- to 3-week course of corticosteroids 9.
Cerebrospinal fluid (CSF) Leak
Conservative management including elevation of the head, bedrest, avoidance of straining. Antibiotic use is a controversial prophylactic strategy to avoid the development of meningitis 10. A small minority of patients will require surgical repair.
Hearing loss
Early evaluation is recommended to establish a baseline followed by a full audiologic evaluation several weeks post-injury. Persistent conductive hearing loss is an indication for surgical exploration with ossiculoplasty. Persistent sensorineural hearing loss can be treated with hearing aids or cochlear implants.
Vertigo
Vestibular function testing should be performed. In cases of perilymph fistula, surgical repair is warranted. Post-traumatic perilymphatic hydrops should be managed with corticosteroids and diuretics 3.
Temporal bone fracture prognosis
Overall the patient prognosis depends on intracranial involvement. The prognoses of common temporal bone fracture complications are as follows:
- Facial nerve paralysis: Transected nerves can be surgically repaired. Compression of a nerve can be treated with surgery or corticosteroids depending on the situation.
- CSF leak: The majority of CSF leaks will resolve within two weeks with only conservative measures. Surgical repair of the leak is possible in refractory cases.
- Hearing loss: Hearing loss may resolve or improve within several months post-injury. Treatment options exist for both persistent conductive and sensorineural hearing loss.
- Vertigo: Vertigo may improve within several months post-injury. Treatment options exist in refractory cases.
- Patel A, Varacallo M. Temporal Fracture. [Updated 2019 Aug 14]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK535391[↩]
- Travis LW, Stalnaker RL, Melvin JW. Impact trauma of the human temporal bone. J Trauma. 1977 Oct;17(10):761-6.[↩]
- Johnson F, Semaan MT, Megerian CA. Temporal bone fracture: evaluation and management in the modern era. Otolaryngol. Clin. North Am. 2008 Jun;41(3):597-618, x.[↩][↩]
- Diaz RC, Cervenka B, Brodie HA. Treatment of Temporal Bone Fractures. J Neurol Surg B Skull Base. 2016 Oct;77(5):419-29.[↩]
- Jones RM, Rothman MI, Gray WC, Zoarski GH, Mattox DE. Temporal lobe injury in temporal bone fractures. Arch. Otolaryngol. Head Neck Surg. 2000 Feb;126(2):131-5.[↩]
- Jones RM, Rothman MI, Gray WC, Zoarski GH, Mattox DE. Temporal lobe injury in temporal bone fractures. Arch. Otolaryngol. Head Neck Surg. 2000 Feb;126(2):131-5. [↩]
- Cannon CR, Jahrsdoerfer RA. Temporal bone fractures. Review of 90 cases. Arch Otolaryngol. 1983 May;109(5):285-8.[↩]
- Dahiya R, Keller JD, Litofsky NS, Bankey PE, Bonassar LJ, Megerian CA. Temporal bone fractures: otic capsule sparing versus otic capsule violating clinical and radiographic considerations. J Trauma. 1999 Dec;47(6):1079-83.[↩]
- Darrouzet V, Duclos JY, Liguoro D, Truilhe Y, De Bonfils C, Bebear JP. Management of facial paralysis resulting from temporal bone fractures: Our experience in 115 cases. Otolaryngol Head Neck Surg. 2001 Jul;125(1):77-84.[↩]
- Brodie HA, Thompson TC. Management of complications from 820 temporal bone fractures. Am J Otol. 1997 Mar;18(2):188-97.[↩]