Papillary thyroid carcinoma
Papillary carcinoma of the thyroid also is also called papillary carcinomas or papillary adenocarcinomas, is the most common cancer of the thyroid gland. Papillary carcinoma appears as an irregular solid or cystic mass or nodule in a normal thyroid parenchyma. About 85% of all thyroid cancers diagnosed in the United States are the papillary carcinoma type 1. Papillary thyroid cancer is more common in women than in men. Papillary thyroid cancer may occur in childhood, but is most often seen in adults between ages 20 and 60.
In a report based upon the Surveillance, Epidemiology, and End Results (SEER) database from 1975 to 2012, the incidence of papillary carcinoma increased from 4.8 to 14.9 per 100,000 2. Papillary thyroid carcinoma occurs predominantly in middle-aged adults with a 3:1 female-to-male ratio and the median age at presentation is 50 years. Even though rare in children, papillary carcinoma is still the most common pediatric thyroid malignancy. It affects whites more commonly than blacks 3.
Thyroid papillary carcinoma tend to grow very slowly and usually develop in only one lobe of the thyroid gland. Even though they grow slowly, papillary thyroid cancers often spread to the lymph nodes in the neck. Even when papillary thyroid cancers have spread to the lymph nodes, they can often be treated successfully and are rarely fatal.
There are several subtypes of thyroid papillary carcinomas. Of these, the follicular subtype also called mixed papillary-follicular variant, is most common 4. It has the same good outlook (prognosis) as the standard type of papillary cancer when found early, and they are treated the same way. Other subtypes of papillary carcinoma (columnar, tall cell, insular, and diffuse sclerosing) are not as common and tend to grow and spread more quickly.
The cause of papillary thyroid cancer is unknown. A genetic defect or family history of papillary thyroid cancer may also be a risk factor.
Radiation increases the risk of developing thyroid cancer. Exposure may occur from:
- High-dose external radiation treatments to the neck, especially during childhood, used to treat childhood cancer or some noncancerous childhood conditions
- Radiation exposure from nuclear plant disasters
Radiation given through a vein (through an IV) during medical tests and treatments does not increase the risk of developing thyroid cancer.
Papillary thyroid cancer causes
Papillary thyroid cancer is linked with a number of inherited conditions, but the exact cause of most thyroid cancers is not yet known.
There are few familial syndromes associated with papillary carcinoma, including familial adenomatous polyposis—Gardner syndrome, Werner syndrome, and Carney complex type 1. Familial papillary carcinoma cases have been reported in 5% of all patients with papillary carcinoma and may portend a more aggressive disease course 5.
There is also a higher incidence of papillary carcinoma in regions with high dietary iodine intake and in patients who have preexisting benign thyroid disease.
The incidence of papillary thyroid cancer is greater in people who have a history of exposure to significant ionizing radiation. External low-dose radiation therapy to the head and neck during childhood, used in the 1940s to 1960s to treat various benign diseases, predispose to papillary carcinoma. The average time from irradiation to the recognition of the tumor is approximately 10 years but may be longer than 30 years 6. High radiation doses (> 2000 cGy) used in the treatment of malignant diseases have also been associated with an increased risk of papillary carcinoma. Environmental exposure:The Chernobyl nuclear accident, which occurred on April 26, 1986, led to a 3- to 75-fold increase in the incidence of papillary carcinoma in fallout regions, especially in younger children.
Several DNA mutations (changes) have been found in papillary thyroid cancer. Many of these cancers have changes in specific parts of the RET gene. The altered form of this gene, known as the PTC oncogene, is found in about 10% to 30% of papillary thyroid cancers overall, and in a larger percentage of these cancers in children and/or linked with radiation exposure. These RET mutations usually are acquired during a person’s lifetime rather than being inherited. They are found only in cancer cells and are not passed on to the person’s children.
Many papillary thyroid cancers have a mutated BRAF gene. The BRAF mutation is less common in thyroid cancers in children and in cancers thought to develop because of exposure to radiation. Cancers with BRAF changes tend to grow and spread to other parts of the body more quickly.
Both BRAF and RET/PTC changes are thought to make cells grow and divide. It is extremely rare for papillary cancers to have changes in both the BRAF and RET/PTC genes. Some doctors now advise testing thyroid biopsy samples for these gene mutations, as they can help diagnose cancer and may also affect the patient’s outlook (see Tests for thyroid cancer).
Changes in other genes have also been linked to papillary thyroid cancer, including those in the NTRK1 gene.
Risk factors for thyroid cancer
A risk factor is anything that increases a person’s chance of getting a disease such as cancer. Scientists have found a few risk factors that make a person more likely to develop thyroid cancer.
Gender and age
For unclear reasons thyroid cancers (like almost all diseases of the thyroid) occur about 3 times more often in women than in men.
Thyroid cancer can occur at any age, but the risk peaks earlier for women (who are most often in their 40s or 50s when diagnosed) than for men (who are usually in their 60s or 70s).
Hereditary conditions
Several inherited conditions have been linked to different types of thyroid cancer, as has family history. Still, most people who develop thyroid cancer do not have an inherited condition or a family history of the disease.
People with certain inherited medical conditions have a higher risk of more common forms of thyroid cancer. Higher rates of thyroid cancer occur among people with uncommon genetic conditions such as:
- Familial adenomatous polyposis (FAP): People with this syndrome develop many colon polyps and have a very high risk of colon cancer. They also have an increased risk of some other cancers, including papillary thyroid cancer. Gardner syndrome is a subtype of FAP in which patients also get certain benign tumors. Both Gardner syndrome and FAP are caused by defects in the gene APC.
- Cowden disease: People with this syndrome have an increased risk of thyroid problems and certain benign growths (including some called hamartomas). They also have an increased risk of cancers of the thyroid, uterus, breast, as well as some others. The thyroid cancers tend to be either the papillary or follicular type. This syndrome is most often caused by defects in the gene PTEN. It is also known as Multiple Hamartoma Syndrome and PTEN Hamartoma Tumor Syndrome
- Carney complex, type I: People with this syndrome may develop a number of benign tumors and hormone problems. They also have an increased risk of papillary and follicular thyroid cancers. This syndrome is caused by defects in the gene PRKAR1A.
- Familial nonmedullary thyroid carcinoma: Thyroid cancer occurs more often in some families, and is often seen at an earlier age. The papillary type of thyroid cancer most often runs in families. Genes on chromosome 19 and chromosome 1 are suspected of causing these familial cancers.
If you suspect you might have a familial condition, talk with your doctor, who might recommend genetic counseling if your medical history warrants it.
Family history
Having a first-degree relative (parent, brother, sister, or child) with thyroid cancer, even without a known inherited syndrome in the family, increases your risk of thyroid cancer. The genetic basis for these cancers is not totally clear.
Iodine in the diet
Follicular thyroid cancers are more common in areas of the world where people’s diets are low in iodine. On the other hand, a diet high in iodine may increase the risk of papillary thyroid cancer. In the United States, most people get enough iodine in their diet because it is added to table salt and other foods.
Radiation
Radiation exposure is a proven risk factor for thyroid cancer. Sources of such radiation include certain medical treatments and radiation fallout from power plant accidents or nuclear weapons.
Having had head or neck radiation treatments in childhood is a risk factor for thyroid cancer. Risk depends on how much radiation is given and the age of the child. In general, the risk increases with larger doses and with younger age at treatment.
Before the 1960s, children were sometimes treated with low doses of radiation for things we wouldn’t use radiation for now, like acne, fungus infections of the scalp (ringworm), or enlarged tonsils or adenoids. Years later, the people who had these treatments were found to have a higher risk of thyroid cancer. Radiation therapy in childhood for some cancers such as lymphoma, Wilms tumor, and neuroblastoma also increases risk. Thyroid cancers that develop after radiation therapy are not more serious than other thyroid cancers.
Imaging tests such as x-rays and CT scans also expose children to radiation, but at much lower doses, so it’s not clear how much those tests might raise the risk of thyroid cancer (or other cancers). If there is an increased risk it is likely to be small, but to be safe, children should not have these tests unless they are absolutely needed. When they are needed, they should be done using the lowest dose of radiation that still provides a clear picture.
Several studies have pointed to an increased risk of thyroid cancer in children because of radioactive fallout from nuclear weapons or power plant accidents. For instance, thyroid cancer was many times more common than normal in children who lived near Chernobyl, the site of a 1986 nuclear plant accident that exposed millions of people to radioactivity. Adults involved with the cleanup after the accident and those who lived near the plant have also had higher rates of thyroid cancer. Children who had more iodine in their diet appeared to have a lower risk.
Some radioactive fallout occurred over certain regions of the United States after nuclear weapons were tested in western states during the 1950s. This exposure was much, much lower than that around Chernobyl. A higher risk of thyroid cancer has not been proven at these low exposure levels. If you are concerned about possible exposure to radioactive fallout, discuss this with your doctor.
Being exposed to radiation when you are an adult carries much less risk of thyroid cancer.
Papillary thyroid cancer prevention
Most people with thyroid cancer have no known risk factors, so it is not possible to prevent most cases of thyroid cancer.
Radiation exposure, especially in childhood, is a known thyroid cancer risk factor. Because of this, doctors no longer use radiation to treat less serious diseases. Imaging tests such as x-rays and CT scans also expose children to radiation, but at much lower doses, so it’s not clear how much they might raise the risk of thyroid cancer (or other cancers). If there is an increased risk it is likely to be small, but to be safe, children should not have these tests unless they are absolutely needed. When they are needed, they should be done using the lowest dose of radiation that still provides a clear picture.
Papillary thyroid cancer symptoms
Papillary thyroid cancer often begins as a painless small lump (nodule) in the thyroid gland with or without enlargement of regional (cervical) lymph nodes 7.
While some small lumps may be cancer, most (90%) thyroid nodules are harmless and are not cancerous.
Most of the time, there are no other symptoms.
Some patients with thyroid cancer have persistent cough, difficulty breathing, or difficulty swallowing. Hoarseness and dysphagia occur in approximately 20% of cases, signaling recurrent laryngeal nerve involvement with vocal cord paralysis or tracheal compression 7. Pain is seldom an early warning sign of thyroid cancer. Other symptoms (eg, pain, stridor, vocal cord paralysis, hemoptysis, rapid enlargement) are rare, and can be caused by less serious problems.
Nodal metastases in the lateral neck are reported in 27% of patients at presentation most often originating from tumors in the ipsilateral thyroid lobe 8.
At the time of diagnosis, 10-15% of patients with papillary thyroid carcinoma have distant metastases to the bones and lungs. Initially, these patiens are evaluated for pulmonary or osteoarticular manifestations (eg, pathologic fracture, spontaneous fracture).
Papillary thyroid cancer possible complications
Papillary thyroid cancer complications include:
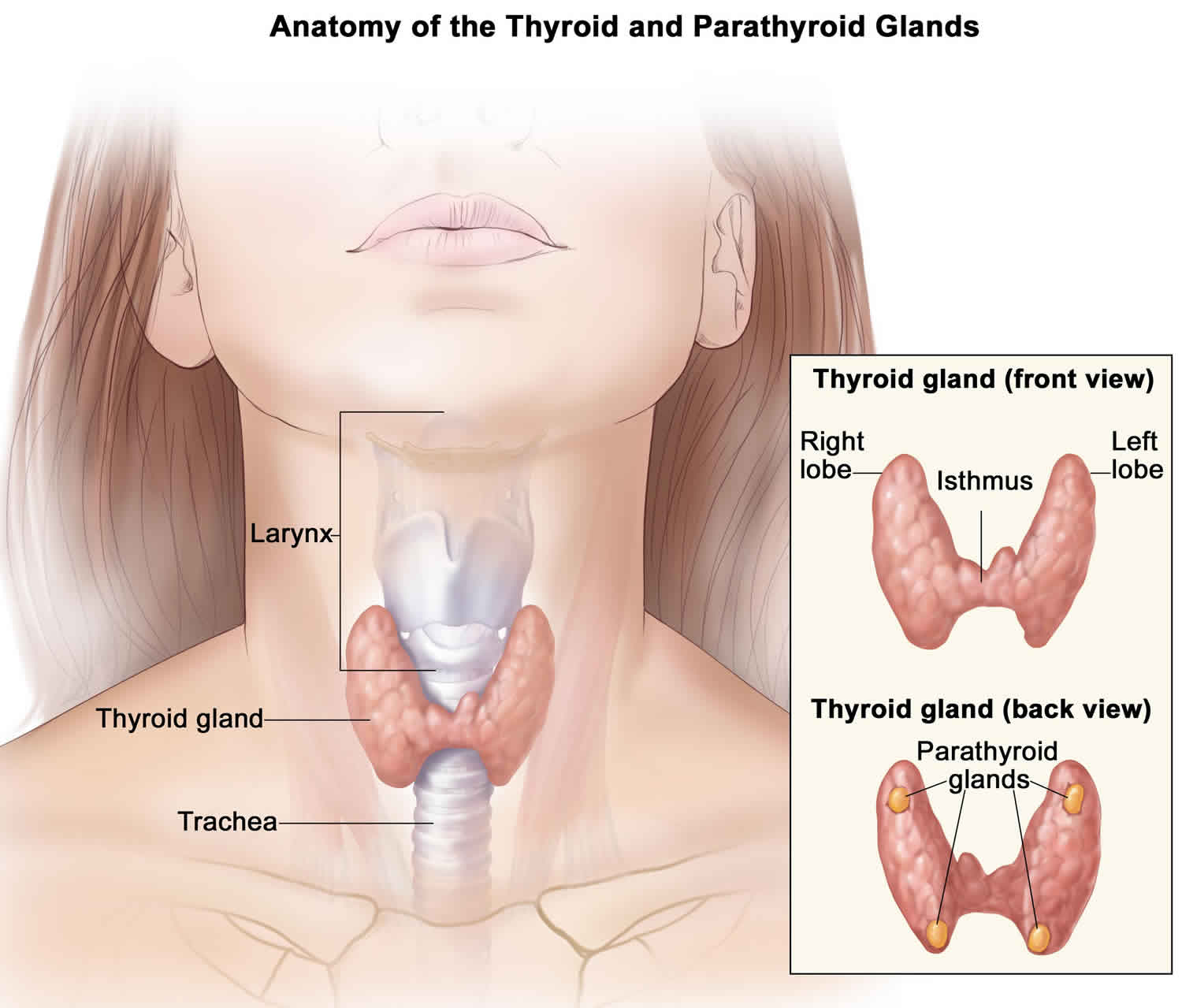
- Accidental removal of the parathyroid gland, which helps regulate blood calcium levels
- Damage to a nerve that controls the vocal cords
- Spreading of cancer to lymph nodes (rare)
- Spreading of cancer to other sites (metastasis). Distant metastasis occurs in only 1% to 25% mostly in the lungs and bones. Other less common sites are the brain, liver, and skin 9.
- Extra-thyroidal extension occurs in 8% to 32% of cases 10.
- Local or regional recurrences occur in 5 to 15% of patients with papillary carcinoma 11.
Papillary thyroid cancer diagnosis
If you have a lump on your thyroid, your health care provider will order blood tests and possibly an ultrasound of the thyroid gland. Ultrasound is noninvasive and inexpensive, and it represents the most sensitive procedure for identifying thyroid lesions and for determining the diameters of a nodule. Ultrasound is also useful for localizing lesions when a nodule is difficult to palpate or is deeply seated. The images can help determine if a lesion is solid or cystic and can help detect the presence of calcifications.
If the ultrasound shows that the lump is less than 1 centimeter, a special procedure called a fine needle aspiration biopsy (FNAB) may be performed. This test helps determine if the lump is cancerous. The accuracy of FNAB results is better than any other test for detecting papillary thyroid carcinoma. The sensitivity of the procedure is near 80%, the specificity is near 100%, and errors can be diminished using ultrasonographic guidance. False-negative and false-positive results occur less than 6% of the time, as the pathologist may experience difficulty distinguishing some benign cellular adenomas from their malignant counterparts 12.
CT scan of the neck may also be done to determine the size of the tumor. One problem using CT scans is that the CT contrast dye contains iodine, which interferes with radioiodine scans. For this reason, many doctors prefer MRI scans for differentiated thyroid cancer.
MRI scans use magnets instead of radiation to create detailed cross-sectional images of your body. A MRI can be used to look for cancer in the thyroid, or cancer that has spread to nearby or distant parts of the body. But ultrasound is usually the first choice for looking at the thyroid. MRI can provide very detailed images of soft tissues such as the thyroid gland. MRI scans are also very helpful in looking at the brain and spinal cord.
A PET scan can be very useful if your thyroid cancer is one that doesn’t take up radioactive iodine. In this situation, the PET scan may be able to tell whether the cancer has spread.
If you have been diagnosed with thyroid cancer (especially follicular thyroid cancer), a plain x-ray of your chest may be done to see if cancer has spread to your lungs.
Thyroid function tests are often normal in people with thyroid cancer. No available blood tests are specific for papillary cancer of the thyroid. Higher-than-normal levels of thyroxine (reference range is 4.5-12.5 mcg/dL), triiodothyronine (reference range is 100-200 ng/dL), and thyroid-stimulating hormone (TSH) (reference range is 0.2-4.7 mIU/dL) may or may not be associated with thyroid cancer.
TSH suppression test
Thyroid cancer is autonomous and does not require TSH for growth, whereas benign lesions do require TSH. When exogenous thyroid hormone feeds back to the pituitary to decrease the production of TSH, thyroid nodules that continue to enlarge are likely to be malignant. However, 15-20% of malignant nodules are suppressible.
Preoperatively, the TSH suppression test is useful for patients with nontoxic solitary benign nodules and for women with repeated nondiagnostic test results. Postoperatively, the test is useful for monitoring papillary thyroid cancer cases.
Papillary thyroid cancer stages
After someone is diagnosed with thyroid cancer, doctors will try to figure out if it has spread, and if so, how far. This process is called staging. The stage of a cancer describes how much cancer is in the body. It helps determine how serious the cancer is and how best to treat it. Doctors also use a cancer’s stage when talking about survival statistics.
Thyroid cancers range from stages I (1) through IV (4). As a rule, the lower the number, the less the cancer has spread. A higher number, such as stage IV, means cancer has spread more. And within a stage, an earlier letter means a lower stage. Although each person’s cancer experience is unique, cancers with similar stages tend to have a similar outlook and are often treated in much the same way.
The staging system most often used for thyroid cancer is the AJCC (American Joint Committee on Cancer) TNM system, which is based on 3 key pieces of information:
- The extent (size) of the tumor (T): How large is the cancer? Has it grown into nearby structures?
- The spread to nearby lymph nodes (N): Has the cancer spread to nearby lymph nodes?
- The spread (metastasis) to distant sites (M): Has the cancer spread to the distant organs such as the lungs or liver?
The systems described below are the most recent American Joint Committee on Cancer (AJCC) systems effective January 2018 and applies to differentiated, anaplastic and medullary thyroid cancers.
Numbers or letters after T, N, and M provide more details about each of these factors. Higher numbers mean the cancer is more advanced. Once a person’s T, N, and M categories have been determined, this information is combined in a process called stage grouping to assign an overall stage.
Cancer staging can be complex, so ask your doctor to explain it to you in a way you understand.
The staging system in the table below uses the pathologic stage also called the surgical stage. It is determined by examining tissue removed during an operation. Sometimes, if surgery is not possible right away or at all, the cancer will be given a clinical stage instead. This is based on the results of a physical exam, biopsy, and imaging tests. The clinical stage will be used to help plan treatment. Sometimes, though, the cancer has spread further than the clinical stage estimates, and might not predict the patient’s outlook as accurately as a pathologic stage.
Younger people have a low likelihood of dying from differentiated (papillary or follicular) thyroid cancer. The TNM stage groupings for these cancers take this fact into account. So, all people younger than 55 years with these cancers are stage I if they have no distant spread and stage II if they have distant spread. This table includes patients 55 or older as well as younger than 55.
Table 1. Differentiated papillary thyroid cancer in patients younger than 55
| AJCC Stage | Age at diagnosis | Stage grouping | Differentiated Thyroid Cancer Stage description* |
| I
| Younger than 55 years | Any T Any N M0
| The cancer is any size (Any T) and might or might not have spread to nearby lymph nodes (Any N). It has not spread to distant sites (M0). |
| OR | |||
| 55 years or older | T1 N0 or NX M0 | The cancer is no larger than 2 cm [0.8 inches] across and confined to the thyroid (T1). It has not spread to nearby lymph nodes (N0) or to distant sites (M0). | |
| OR | |||
| 55 years or older | T2 N0 or NX M0 | The cancer is larger than 2 cm [0.8 inches] across but no larger than 4 cm and confined to the thyroid (T2). It has not spread to nearby lymph nodes (N0) or to distant sites (M0). | |
| II | Younger than 55 years | Any T Any N M1 | The cancer can be any size (Any T). It might or might not have spread to nearby lymph nodes (Any N). It has spread to other parts of the body, such as distant lymph nodes, internal organs, bones, etc. (M1). |
| OR | |||
| 55 years or older | T1 N1 M0 | The cancer is no larger than 2 cm [0.8 inches] across and confined to the thyroid (T1). It has spread to nearby lymph nodes (N1). It has not spread to distant sites (M0). | |
| OR | |||
| 55 years or older | T2 N1 M0 | The cancer is larger than 2 cm [0.8 inches] across but no larger than 4 cm and confined to the thyroid (T2). It has spread to nearby lymph nodes (N1). It has not spread to distant sites (M0). | |
| OR | |||
| 55 years or older | T3a or T3b Any N M0 | The cancer is larger than 4 cm but confined to the thyroid (T3a) or it has grown into the strap muscles around the thyroid (T3b). It might or might not have spread to nearby lymph nodes (Any N). It has not spread to distant sites (M0). | |
| III | 55 years or older | T4a Any N M0 | The cancer is any size and has grown extensively beyond the thyroid gland into nearby tissues of the neck, such as the larynx (voice box), trachea (windpipe), esophagus (tube connecting the throat to the stomach), or the nerve to the larynx (T4a). It might or might not have spread to nearby lymph nodes (Any N). It has not spread to distant sites (M0). |
| IVA | 55 years or older | T4b Any N M0 | The cancer is any size and has grown extensively beyond the thyroid gland back toward the spine or into nearby large blood vessels (T4b). It might or might not have spread to nearby lymph nodes (Any N). It has not spread to distant sites (M0). |
| IVB | 55 years or older | Any T Any N M1 | The cancer is any size (Any T) and might or might not have spread to nearby lymph nodes (Any N). It has spread to other parts of the body, such as distant lymph nodes, internal organs, bones, etc. (M1). |
Footnote:
* The following additional categories are not listed on the table above:
- TX: Main tumor cannot be assessed due to lack of information.
- T0: No evidence of a primary tumor. The N categories are described in the table above, except for:
- NX: Regional lymph nodes cannot be assessed due to lack of information.
Papillary thyroid cancer treatment
There are three types of thyroid cancer treatment:
- Surgery
- Radioactive iodine (RAI)
- Thyroid Hormone Treatment
Surgery
Surgery is done to remove as much of the cancer as possible. The bigger the lump, the more of the thyroid gland must be removed. Often, the entire gland is taken out. If surgery is not an option, external radiation therapy can be useful.
A lobectomy is an option for unifocal papillary carcinoma smaller than 4 cm with no evidence of extra-thyroidal extension or lymph node metastasis. For patients with papillary carcinoma >4 cm, or with gross extra-thyroidal extension (clinical T4), or clinically apparent metastatic disease to nodes (clinical N1) or distant sites (clinical M1), the initial surgical procedure should include a near-total or total thyroidectomy and gross removal of all primary tumor unless there are contraindications to this procedure. If surgery is chosen for patients with thyroid cancer <1 cm without extra-thyroidal extension and cN0, the initial surgical procedure should be a thyroid lobectomy unless there are clear indications to remove the contralateral lobe. Thyroid lobectomy alone is sufficient treatment for small, unifocal, intrathyroidal carcinomas in the absence of prior head and neck radiation, familial thyroid carcinoma, or clinically detectable cervical nodal metastases 13. Prophylactic central-compartment neck dissection (ipsilateral or bilateral) should be a consideration in patients with papillary carcinoma with clinically uninvolved central neck lymph nodes (cN0) who have advanced primary tumors (T3 or T4) or clinically involved lateral neck nodes (cN1b), or if the information will be used to plan further steps in therapy.
Adjuvant Radioiodine Therapy
After the surgery, you may receive radioiodine (I 131) therapy, which is often taken by mouth. This substance kills any remaining thyroid tissue. It also helps make medical images clearer, so doctors can see if there is any cancer left behind or if it comes back later.
Radioiodine therapy is indicated in the following cases 14:
- Patients with tumor >2 cm and one of the following risk factors: gross extra-thyroidal extension, age >45 years, lymph node and distant metastases
- Patients with tumor <2 cm and distant metastasis
Thyroid Hormone Treatment
After surgery or radioiodine therapy, you will need to take medicine called levothyroxine for the rest of your life. This replaces the hormone the thyroid would normally make. Since TSH (thyrotropin) can promote the growth of remaining papillary carcinoma cells, the dosage of l-thyroxine (levothyroxine) should initially be high enough to achieve a suppression of thyrotropin (TSH).
Your doctor will likely have you take a blood test every 6 to 8 weeks to check your thyroid hormone levels. Depending on the result, the dosage should be adjusted; the use of TSH suppressive therapy should merit careful consideration since it carries an increased risk of complications 15.
Other follow-up tests that may be done after treatment for thyroid cancer include:
- Ultrasound of the thyroid
- An imaging test called a radioactive iodine (I 131) uptake scan
- Repeat fine needle aspiration biopsy (FNAB)
Papillary thyroid cancer prognosis
The prognosis in patients with papillary thyroid cancer is related to age, sex, and stage. In general, if the cancer does not extend beyond the capsule of the gland, life expectancy is minimally affected. Prognosis is better in females and in patients younger than 40 years. The survival rate is at least 95% with appropriate treatments. More than 90% of adults with this cancer survive at least 10 to 20 years. The prognosis is better for people who are younger than 40 and for those with smaller tumors.
The following factors may decrease the survival rate:
- Older than 55
- Cancer that has spread to distant parts of the body
- Cancer that has spread to soft tissue
- Large tumor size
- Male sex
- Less differentiated or solid areas, vascular invasion, and aneuploid cell population
- Subtypes of papillary carcinoma that associate with a more aggressive clinical behavior: tall cell variant, diffuse sclerosis variant, solid variant, and follicular variant
If neglected, any thyroid cancer may result in symptoms because of compression and/or infiltration of the cancer mass into the surrounding tissues, and the cancer may metastasize to lung and bone. Metastases, in descending order of frequency, are most common in the neck lymph nodes and lung, followed by the bone, brain, liver, and other sites. Metastatic potential seems to be a function of the primary tumor size. Metastases in the absence of thyroid pathology in the physical examination findings are rare in patients with microscopic papillary carcinoma (occult carcinomas).
In a long-term follow-up study of children and adolescents with papillary thyroid cancer, Hay et al 16 found that all-causes mortality rates did not exceed expectation through 20 years after treatment, but the number of deaths was significantly higher than predicted from 30 through 50 years afterward. Nonthyroid malignancy accounted for 68% of deaths, and, of that group, 73% had received postoperative therapeutic irradiation.
A study by Yu et al 17 found that papillary thyroid microcarcinomas are generally associated with an excellent prognosis; however, 0.5% of patients may die. Risk factors for overall survival include the following:
- Age older than 45 years
- Male sex
- Minority race
- Node metastases
- Extrathyroidal invasion
- Distant metastases
If two or more risk factors are present, patients should be considered for more aggressive management.
A study by Miyauchi et al 18 found that serum thyroglobulin doubling time was a significant prognostic predictor in patients with papillary thyroid carcinoma. The authors concluded that this finding was superior to classical prognostic factors, including TNM stage, age, and gender.
In a study of 39,562 patients with papillary thyroid carcinoma from the National Cancer Data Base, risk factors for central lymph node metastasis included the following 19:
- Age ≤45 years
- Male sex
- Asian race
- Tumor >1 cm
A family history of papillary thyroid carcinoma is an independent risk factor for disease recurrence in patients with papillary thyroid microcarcinoma 20.
For patients found to be at intermediate risk on the basis of established prognostic factors, Brennan and colleagues 21 report that gene expression signatures may permit classification into intermediate-good prognosis and intermediate-poor prognosis groups. The authors note that their findings require validation, but they observe that tests that routinely measure expression of hundreds of genes are already commercially available.
A retrospective study 22 of clinicopathological outcomes of 6282 patients with papillary carcinoma demonstrated significant differences in recurrence and disease-specific patient survival with three histologic variants of papillary carcinoma. Particularly in patients at least 45 years old, patients with tall-cell papillary carcinoma had the worse prognosis; those with conventional papillary carcinoma had an intermediate prognosis, and those with follicular-variant papillary carcinoma had the best prognosis.
Indeed, the American Thyroid Association has recommended that the encapsulated follicular variant of papillary carcinoma without capsular or vascular invasion be reclassified as noninvasive follicular thyroid neoplasm with papillary-like nuclear features 23. Recurrence of noninvasive follicular thyroid neoplasm with papillary-like nuclear features is extremely rare, even in patients treated with surgery alone, without radioactive iodine therapy, and ceasing to classify it as a cancer may help clinicians avoid unnecessary aggressive treatment 24.
Diffuse sclerosing papillary thyroid carcinoma is an uncommon variant of papillary thyroid carcinoma. A systematic review and meta-analysis by Vuong et al 25 concluded that DSpapillary carcinoma should be considered a high-risk condition, because it has a high propensity for tumor invasion, metastasis, relapse, and mortality, compared with classic papillary thyroid carcinoma.
References- Thyroid cancer – papillary carcinoma. https://medlineplus.gov/ency/article/000331.htm
- Limaiem F, Mazzoni T. Cancer, Papillary Thyroid Carcinoma (PTC) [Updated 2019 Jan 15]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK536943
- Lim H, Devesa SS, Sosa JA, Check D, Kitahara CM. Trends in Thyroid Cancer Incidence and Mortality in the United States, 1974-2013. JAMA. 2017 Apr 04;317(13):1338-1348.
- What Is Thyroid Cancer? https://www.cancer.org/cancer/thyroid-cancer/about/what-is-thyroid-cancer.html
- Mileva M, Stoilovska B, Jovanovska A, Ugrinska A, Petrushevska G, Kostadinova-Kunovska S, Miladinova D, Majstorov V. Thyroid cancer detection rate and associated risk factors in patients with thyroid nodules classified as Bethesda category III. Radiol Oncol. 2018 Sep 27;52(4):370-376.
- Mao XC, Yu WQ, Shang JB, Wang KJ. Clinical characteristics and treatment of thyroid cancer in children and adolescents: a retrospective analysis of 83 patients. J Zhejiang Univ Sci B. 2017 May;18(5):430-436.
- Limaiem F, Mazzoni T. Cancer, Papillary Thyroid Carcinoma (PTC) [Updated 2019 Jan 15]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK536943
- Rahmat F, Kumar Marutha Muthu A, S Raja Gopal N, Jo Han S, Yahaya AS. Papillary Thyroid Carcinoma as a Lateral Neck Cyst: A Cystic Metastatic Node versus an Ectopic Thyroid Tissue. Case Rep Endocrinol. 2018;2018:5198297
- Sebastian SO, Gonzalez JM, Paricio PP, Perez JS, Flores DP, Madrona AP, Romero PR, Tebar FJ. Papillary thyroid carcinoma: prognostic index for survival including the histological variety. Arch Surg. 2000 Mar;135(3):272-7
- Mazzaferri EL, Jhiang SM. Long-term impact of initial surgical and medical therapy on papillary and follicular thyroid cancer. Am. J. Med. 1994 Nov;97(5):418-28.
- DeGroot LJ, Kaplan EL, McCormick M, Straus FH. Natural history, treatment, and course of papillary thyroid carcinoma. J. Clin. Endocrinol. Metab. 1990 Aug;71(2):414-24.
- Ng CM, Choi CH, Tiu SC. False-negatives in thyroid nodule aspiration cytology. Hong Kong Med J. 2007 Apr. 13(2):168-9.
- Haugen BR. 2015 American Thyroid Association Management Guidelines for Adult Patients with Thyroid Nodules and Differentiated Thyroid Cancer: What is new and what has changed? Cancer. 2017 Feb 01;123(3):372-381.
- Tang J, Kong D, Cui Q, Wang K, Zhang D, Liao X, Gong Y, Wu G. The role of radioactive iodine therapy in papillary thyroid cancer: an observational study based on SEER. Onco Targets Ther. 2018;11:3551-3560.
- Haugen BR. 2015 American Thyroid Association Management Guidelines for Adult Patients with Thyroid Nodules and Differentiated Thyroid Cancer: What is new and what has changed? Cancer. 2017 Feb 01;123(3):372-381
- Hay ID, Gonzalez-Losada T, Reinalda MS, Honetschlager JA, Richards ML, Thompson GB. Long-term outcome in 215 children and adolescents with papillary thyroid cancer treated during 1940 through 2008. World J Surg. 2010 Jun. 34(6):1192-202.
- Yu XM, Wan Y, Sippel RS, Chen H. Should all papillary thyroid microcarcinomas be aggressively treated? An analysis of 18,445 cases. Ann Surg. 2011 Oct. 254(4):653-60.
- Miyauchi A, Kudo T, Miya A, et al. Prognostic impact of serum thyroglobulin doubling-time under thyrotropin suppression in patients with papillary thyroid carcinoma who underwent total thyroidectomy. Thyroid. 2011 Jul. 21(7):707-16.
- Suman P, Wang CH, Abadin SS, Moo-Young TA, Prinz RA, Winchester DJ. Risk factors for central lymph node metastasis in papillary thyroid carcinoma: A National Cancer Data Base (NCDB) study. Surgery. 2015 Oct 1.
- Cao J, Chen C, Chen C, Wang QL, Ge MH. Clinicopathological features and prognosis of familial papillary thyroid carcinoma – a large-scale, matched, case-control study. Clin Endocrinol (Oxf). 2015 Jul 20.
- Brennan K, Holsinger C, Dosiou C, Sunwoo JB, Akatsu H, Haile R, et al. Development of prognostic signatures for intermediate-risk papillary thyroid cancer. BMC Cancer. 2016 Sep 15. 16 (1):736.
- Shi X, Liu R, Basolo F, Giannini R, Shen X, et al. Differential Clinicopathological Risk and Prognosis of Major Papillary Thyroid Cancer Variants. J Clin Endocrinol Metab. 2016 Jan. 101 (1):264-74.
- Haugen BR, Sawka AM, Alexander EK, Bible KC, Caturegli P, Doherty GM, et al. American Thyroid Association Guidelines on the Management of Thyroid Nodules and Differentiated Thyroid Cancer Task Force Review and Recommendation on the Proposed Renaming of Encapsulated Follicular Variant Papillary Thyroid Carcinoma Without Invasion to Noninvasive Follicular Thyroid Neoplasm with Papillary-Like Nuclear Features. Thyroid. 2017 Apr. 27 (4):481-483.
- Tallini G, Tuttle RM, Ghossein RA. The History of the Follicular Variant of Papillary Thyroid Carcinoma. J Clin Endocrinol Metab. 2017 Jan 1. 102 (1):15-22.
- Vuong HG, Kondo T, Pham TQ, Oishi N, Mochizuki K, Nakazawa T, et al. Prognostic significance of diffuse sclerosing variant papillary thyroid carcinoma: a systematic review and meta-analysis. Eur J Endocrinol. 2017 Apr. 176 (4):431-439.