What is tibial plateau fracture
Tibial plateau fractures occur below your knee joint and disrupts the smooth gliding surface of your knee joint. This can lead to permanent cartilage damage and lead to osteoarthritis of the knee. Tibial plateau fractures may be associated with injury to nearby structures including vasculature, nerves, ligaments, menisci, and adjacent compartments. While minimal tibial plateau fractures with no associated injuries can be safely managed non-operatively, typically this injury requires orthopedic consultation and operative management.
Tibial plateau fractures account for 1% of all fractures and are typically sustained with high-energy mechanisms. The incidence of tibial plateau fractures is 10.3 per 100,000 people annually 1. Tibial plateau fractures were originally termed a bumper or fender fracture but only 25% of tibial plateau fractures result from impact with automobile bumpers. The tibial plateau is one of the most critical loadbearing areas in the human body; tibial plateau fractures affect knee alignment, stability, and motion. Early detection and appropriate treatment of tibial plateau fractures are critical for minimizing patient disability and reducing the risk of documented complications, particularly posttraumatic arthritis 2.
Tibial plateau fractures may be lateral, medial, or bicondylar. Injuries to the lateral part of the tibial plateau are most common, and typically involve a blow to the lateral knee 1. Injuries to the medial plateau require more force and are sustained from high energy mechanisms including axial load from falling from a height and landing on the feet, motor vehicle collisions, and other sources of direct trauma. With high-energy mechanisms such as these, bicondylar fractures are more common than isolated medial plateau fractures. Tibial plateau fractures as a result of low energy mechanisms are more likely to occur in the elderly, or other populations with osteoporotic disease.
Tibia anatomy
The tibia is the weight-bearing bone of the lower leg, located medially to the fibula. The proximal part of the bone compromises the distal part of the knee joint. The tibial plateau has two articular surfaces, the medial and lateral tibial condyles, also called the medial and lateral plateaus. The medial tibial condyle bears 60% of the knee’s weight and is a thicker structure. It is concave in shape and located slightly more distally compared to the lateral tibial condyle. The lateral tibial condyle is convex in shape, thinner, weaker, and more proximal than the medial tibial condyle. The intercondylar eminence is a bony structure between the two condyles that serves as an attachment point for the anterior cruciate ligament.
Fascia separates the lower leg into four compartments containing muscle, vessels, and nerves. The anterior, posterior and deep compartments border the tibia and are at risk for compartment syndrome with tibial fractures.
The ligaments and menisci of the knee joint are also in contact with the proximal tibia and are at risk for injury associated with tibial fractures.
Vascular injury is also a complication of proximal tibial fractures; the popliteal artery runs posterior to the knee, and branches into the anterior and posterior tibial artery.
Tibial plateau fracture causes
The most common mechanism resulting in a tibial plateau fracture is a valgus force with axial loading. Of these fractures, 80% are motor vehicle–related injuries, and the remainder are sports-related injuries. Bumper- or fender-related injuries from a vehicle-pedestrian collision constitute more than 25% of tibial plateau fractures. Trauma can be direct or can be related to a fall from a height, an industrial accident, or a sports injury.
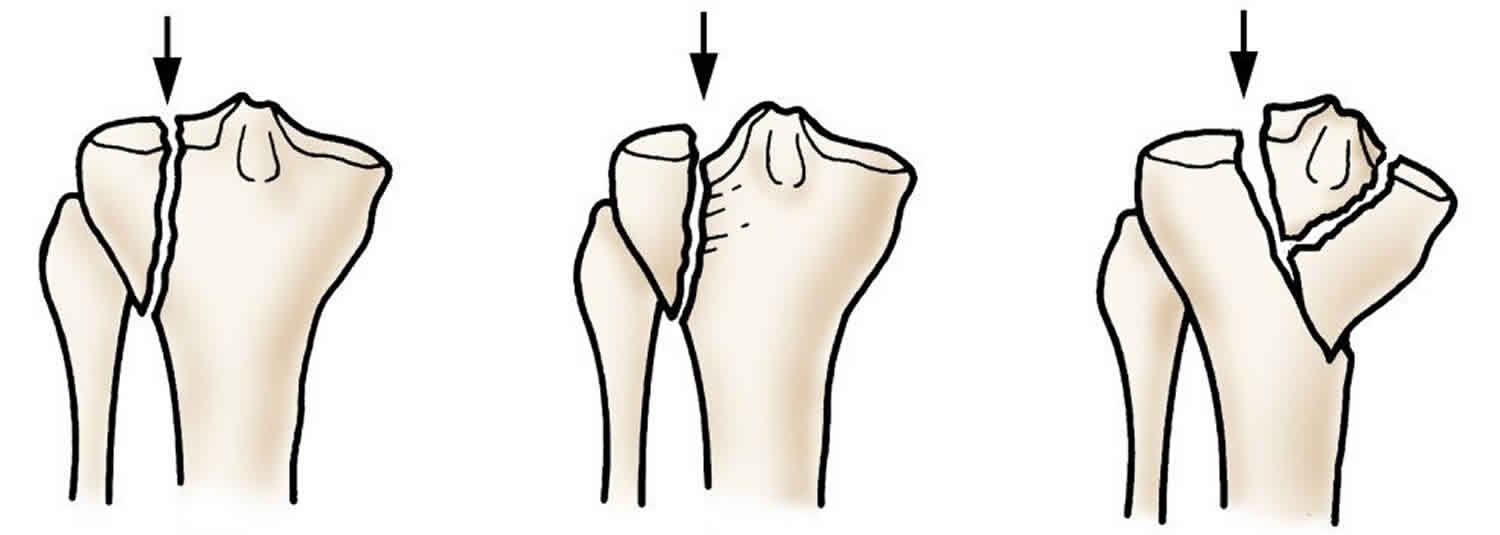
Tibial plateau fractures may be either low-energy or high-energy. Low-energy fractures occur in osteoporotic bone and typically are depressed fractures. High-energy fractures are often a result of motor vehicle–related trauma, and the most common pattern of fracture in this group is a splitting fracture.
Approximately 50% of knees with closed tibial plateau fractures have injuries of the menisci and cruciate ligaments that usually necessitate surgical repair. Because of the valgus stress at the moment of impact, the medial collateral ligament is at greater risk than the lateral collateral ligament; however, disruption of the lateral collateral ligament is of grave concern because of possible injuries to the peroneal nerve and the popliteal vessels. Dislocation-relocation injuries are more common with medial plateau injuries and carry an increased risk of peroneal nerve damage.
Tibial plateau fracture symptoms
Tibial plateau fracture symptoms can include any of the following:
- Pain on weight bearing
- Leg swelling
- Leg weakness
- Tenseness around the knee or leg with limited bending
- Deformity around the knee
- Pale and cool foot
- Numbness around the foot
Tibial plateau fracture complications
Tibial plateau fracture complications can be divided into early (eg, loss of reduction, deep vein thrombosis, infection) or late (eg, nonunion, implant breakage, posttraumatic arthritis). Most early complications can be viewed as biologic failures, whereas late complications are often associated with mechanical problems 3.
Early complications include the following:
- Compartment syndrome
- Vascular injuries
- Swelling and wound-healing problems
- Infections
- Deep vein thrombosis
- Nerve injuries
Late complications include the following:
- Knee stiffness
- Knee instability
- Angular deformities
- Late collapse
- Malunion
- Osteoarthrosis 4
Tibia plateau fracture diagnosis
Tibial plateau fractures should be suspected in patients presenting with knee pain, possible deformity, edema, and a significant mechanism of injury or risk factors that predispose to orthopedic injuries.
Patients with very high energy mechanisms of injury may present to the trauma bay and undergo complete advanced trauma life support evaluation, and prioritization should always be given to evaluating ABCs (Airway, Breathing, Circulation) and stabilizing the patient. A pulseless distal extremity is an orthopedic emergency. Complete physical exam of a potential tibial fracture should include an examination of the entire knee, comparison to the contralateral (presumably uninjured) knee, with special attention to the following:
- Skin: The skin should be examined circumferentially to evaluate for an open fracture, lacerations, or puncture wounds.
- Knee effusion: If there is a significant effusion, the knee may be aspirated to evaluate for hemarthrosis, and for the presence of lipids or bone marrow elements, suggesting intraarticular fracture.
- Neurovascular exam: Sensation, motor function, and distal pulses should be assessed. There should be a low threshold to measure Ankle-brachial indices should there be a difference in pulses between extremities.
- Compartments: All compartments should be palpated; a firm, tense compartment suggests compartment syndrome, which can be further evaluated by measuring intracompartmental pressure.
- Laxity tests: More than 10 degrees of laxity at the joint line with varus/valgus stress testing suggests a tear of the collateral ligaments. Laxity below the joint line is indicative of a displaced fracture.
- The range of motion: Range of motion and strength may be very difficult to assess secondary to pain.
Plain radiographs should include anterior-posterior (AP), lateral, and intercondylar notch views. However, tibial plateau fractures can be difficult to see on plain films. These injuries are associated with significant morbidity, and frequently require operation management, therefore if there is a high degree of suspicion for tibial plateau fractures and negative plain radiographs, CT or MRI should be used. The knee joint should be evaluated for fracture lines, displacement, depression of the tibial plateau, and associated ligamentous or meniscal injury. Either CT or MRI can better demonstrate the extent of plateau depression and comminution than plain radiographs, and may be helpful in surgical planning should this management be indicated. CT scans are typically faster and easier to obtain in an acute setting. However, MRI can identify meniscal and ligamentous injury while CT cannot.
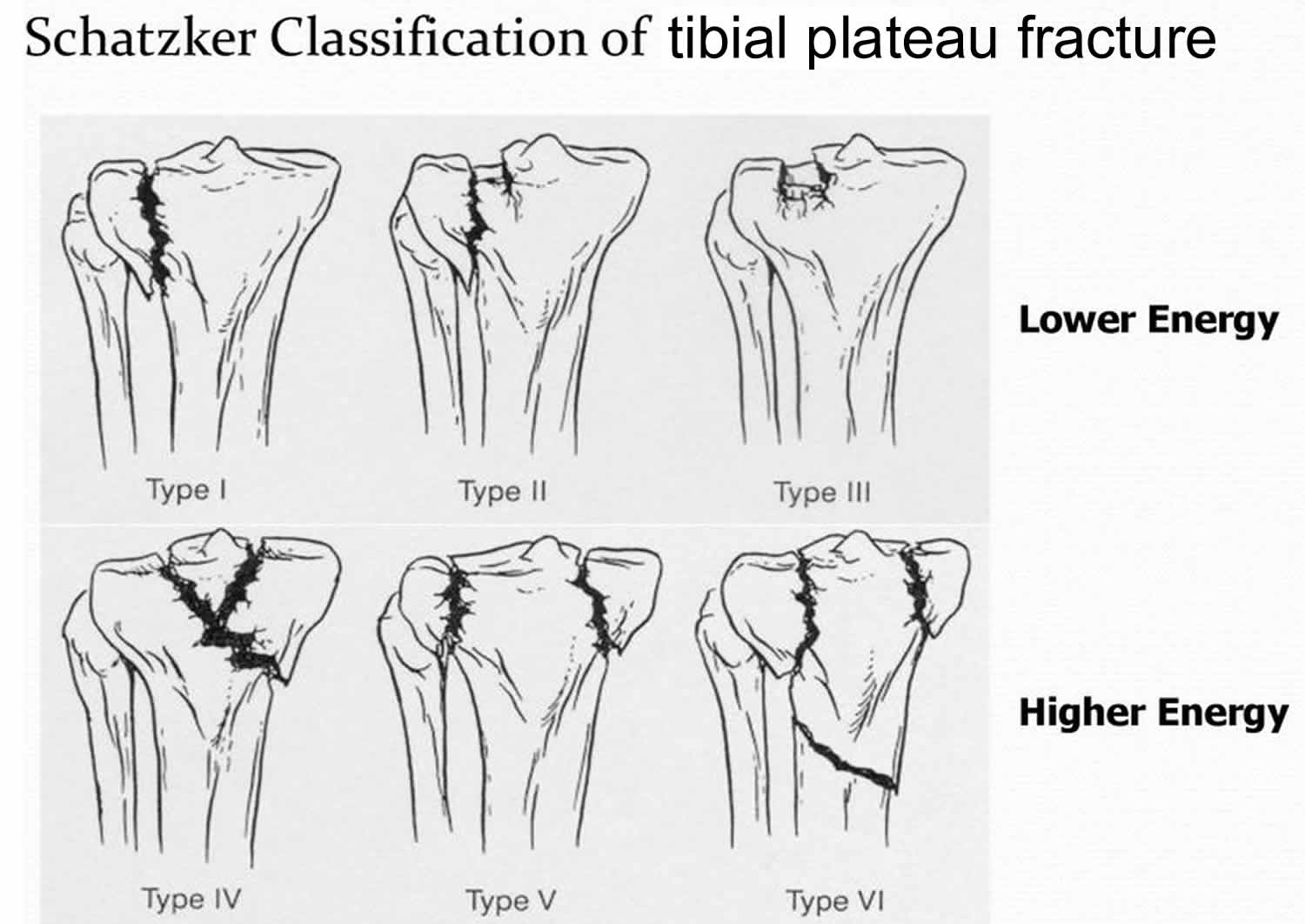
Once the extent of the injury has been visualized, tibial plateau fractures are classified based on the Schatzker Classification system, summarized below 5:
- Schatzker I: Lateral split fracture, wedge-shaped pure cleavage fracture of the lateral tibial plateau, originally defined as having less than 4 mm of depression or displacement
- Schatzker II: Lateral split-depressed fracture – splitting and depression of the lateral tibial plateau; namely, type I fracture with a depressed component
- Schatzker III: Lateral pure depression fracture – pure depression of the lateral tibial plateau; divided into two subtypes:
- Schatzker IIIa: with lateral depression
- Schatzker IIIb: with central depression
- Schatzker IV: Medial tibial plateau fracture with a split or depressed component
- Schatzker V: Bicondylar plateau fracture (wedge fracture of both lateral and medial tibial plateau)
- Schatzker VI: Metaphyseal-diaphyseal dissociation – transverse tibial metadiaphyseal fracture, along with any type of tibial plateau fracture (metaphyseal-diaphyseal discontinuity)
Figure 1. Schatzker Classification of tibial plateau fracture
Tibial plateau fracture treatment
Non-surgical management
Tibial plateau fractures most commonly require orthopedic consultation. These injuries may be managed non-operatively only if there is absolutely no displacement, depression of the tibial plateau, comminution, or associated ligamentous or meniscal injury. These typically occur with low energy mechanisms. Fractures appropriate for non-operative management may be placed in a hinged knee brace and made non-weight bearing. The patient should be re-evaluated weekly with plain radiographs for 3 weeks following injury, and assuming there is no further injury or displacement, may be transitioned to imaging biweekly or every three weeks. Typically patients will be non-weight bearing for 6 weeks, with partial weight bearing permitted after bony callus is demonstrated on radiographs. The patient should remain in the brace until radiographic healing is complete, which may take up to 12 weeks. Physical therapy may begin at this time, and patients may not regain full function until 16 to 20 weeks or longer. Return to activities requiring prolonged weight bearing and stress such as certain sports should not occur until healing is nearly complete, with the affected extremity demonstrating more than 90% of the strength of the unaffected extremity.
Indications for nonoperative treatment are as follows:
- Nondisplaced stable split fractures
- Minimally displaced or depressed fractures
- Submeniscal rim fractures
- Fractures in elderly, low-demand, or osteoporotic patients
Advantages of nonoperative treatment are as follows:
- Simple technique
- No surgical trauma or risk for sepsis
- Shorter hospital stay
- Early joint mobilization (only if functional cast brace is used) and delayed weight-bearing
Disadvantages of nonoperative treatment are as follows:
- Risk of displacement and need for surgery (follow-up with imaging studies every 2 weeks for 6 weeks; activity restriction for 4-6 months)
- Prolonged immobilization and related complications – If traction is used, good motion is obtained at the cost of a lengthy hospital stay and the risk of pin-tract infection 6; related complications of recumbency can include pulmonary embolism or phlebitis
- Joint stiffness (if immobilization >2-3 weeks)
- Instability and posttraumatic arthritis in the long term
Tibial plateau fracture surgery
Fracture displacement ranging from 4-10 mm can be treated nonoperatively; however, a depressed fragment greater than 5 mm should be elevated and grafted 7.
The following are absolute indications for surgery:
- Open plateau fractures
- Fractures with an associated compartment syndrome
- Fractures associated with a vascular injury
The following are relative indications for surgery:
- Most displaced bicondylar fractures
- Displaced medial condylar fractures
- Lateral plateau fractures that result in joint instability
Contraindications for surgical treatment include the following:
- Presence of a compromised soft-tissue envelope (for immediate open reduction)
- Fractures that do not result in joint instability or deformity and can therefore be treated with nonoperative modalities
Open or arthroscopic-assisted techniques are considered for fractures with displacement, depression of the condylar surfaces, or both 8. Open surgical therapy can be immediate or staged.
Open reduction with internal fixation (ORIF) is recommended for tibial fractures with significant articular step-off, condylar widening, ligamentous instability, and for Schatzer IV to VI injuries. If the injury is too comminuted for internal fixation, external fixation with limited open/percutaneous fixation of the articular segment may be performed. If there is significant soft tissue injury, or if the patient has sustained other serious injuries that require more immediate attention, open reduction with internal fixation (ORIF) may be delayed and bridging external fixation may be performed as a temporizing measure.
Internal fixation can be accomplished by means of the following:
- Biologic fixation – Screw fixation, minimally invasive plate osteosynthesis, least invasive stabilization system 9
- Arthroscopic-assisted fixation
- Conventional double-plating
External fixation can be accomplished with the following:
- Ilizarov fixator 10
- Hybrid fixator
Combination devices may also be employed.
Some promising results have been achieved with balloon tibioplasty for depression fractures of the tibial plateau, but long-term results remain to be determined 11.
Tibial plateau fracture recovery
Recovering range of motion is a challenge for patients such as the following:
- Those who cannot actively participate in rehabilitation
- Those who may have soft-tissue injuries that preclude immediate range of motion
- Those who have had external-fixation pins inserted near their quadriceps
Because of the potential disability associated with chronic flexion contracture, after surgery, these patients should be placed in a hinged knee brace that is locked in extension. A padded bump under the heel is used both in the hospital bed and at home after discharge to maximize knee extension.
Motion is restricted until surgical and traumatic wounds are dry. Continuous passive motion begins when wounds are dry; the goal is full extension and 90° of flexion within 5-7 days. If other injuries allow, the patient is mobilized with a hinged brace locked in extension for 6 weeks 12.
Nonweightbearing precautions generally continue for 12 weeks. Active flexion and passive extension are encouraged for 6 weeks, after which period active knee extension is started. Active knee extension is delayed if ORIF of a tibial tubercle avulsion was required.
A study by Garner et al found that elective removal of implants after ORIF for tibial plateau fracture led to improved clinical outcomes at 12 months 13.
Tibial plateau fracture prognosis
Higher energy mechanisms of trauma are associated with poor outcomes. Long-term complications of tibial plateau fractures include an inability to regain normal gait, osteoarthritis of the knee, ankle osteoarthritis secondary to an abnormal gait, and chronic pain. These problems may affect the quality of life profoundly. For patients whose jobs require a high degree of mobility, a tibial plateau fracture may significantly delay return to employment.
- Malik S, Rosenberg N. Tibial Plateau Fractures. [Updated 2019 Jan 20]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK470593[↩][↩]
- Agnew SG. Tibial plateau fractures. Oper Tech Orthoped. 1999. 9(3):197-205.[↩]
- Papagelopoulos PJ, Partsinevelos AA, Themistocleous GS, et al. Complications after tibia plateau fracture surgery. Injury. 2006 Jun. 37(6):475-84.[↩]
- Mehin R, O’Brien P, Broekhuyse H, Blachut P, Guy P. Endstage arthritis following tibia plateau fractures: average 10-year follow up. Can J Surg. 2012 Feb 1. 55(1):003111-3111.[↩]
- The tibial plateau fracture. The Toronto experience 1968–1975. Schatzker J, McBroom R, Bruce D. Clin Orthop Relat Res. 1979 Jan-Feb;(138):94-104. https://www.ncbi.nlm.nih.gov/pubmed/445923[↩]
- Laible C, Earl-Royal E, Davidovitch R, Walsh M, Egol KA. Infection after spanning external fixation for high-energy tibial plateau fractures: is pin site-plate overlap a problem?. J Orthop Trauma. 2012 Feb. 26(2):92-7[↩]
- Pernaa K, Koski I, Mattila K, Gullichsen E, Heikkila J, Aho A, et al. Bioactive Glass S53P4 and Autograft Bone in Treatment of Depressed Tibial Plateau Fractures – A Prospective Randomized 11-year Follow-Up. J Long Term Eff Med Implants. 2011. 21(2):139-48.[↩]
- Chen XZ, Liu CG, Chen Y, Wang LQ, Zhu QZ, Lin P. Arthroscopy-assisted surgery for tibial plateau fractures. Arthroscopy. 2015 Jan. 31 (1):143-53.[↩]
- Kayali C, Oztürk H, Altay T, Reisoglu A, Agus H. Arthroscopically assisted percutaneous osteosynthesis of lateral tibial plateau fractures. Can J Surg. 2008 Oct. 51(5):378-82.[↩]
- Kumar P, Singh GK, Bajracharya S. Treatment of grade IIIB opens tibial fracture by ilizarov hybrid external fixator. Kathmandu Univ Med J (KUMJ). 2007 Apr-Jun. 5(2):177-80.[↩]
- Craiovan BS, Keshmiri A, Springorum R, Grifka J, Renkawitz T. [Minimally invasive treatment of depression fractures of the tibial plateau using balloon repositioning and tibioplasty : Video article]. Orthopade. 2014 Oct. 43(10):930-3.[↩]
- Chan YS, Chiu CH, Lo YP, Chen AC, Hsu KY, Wang CJ, et al. Arthroscopy-assisted surgery for tibial plateau fractures: 2- to 10-year follow-up results. Arthroscopy. 2008 Jul. 24(7):760-8.[↩]
- Garner MR, Thacher RR, Ni A, Berkes MB, Lorich DG. Elective removal of implants after open reduction and internal fixation of Tibial Plateau fractures improves clinical outcomes. Arch Orthop Trauma Surg. 2015 Nov. 135 (11):1491-6.[↩]