What is tinea nigra
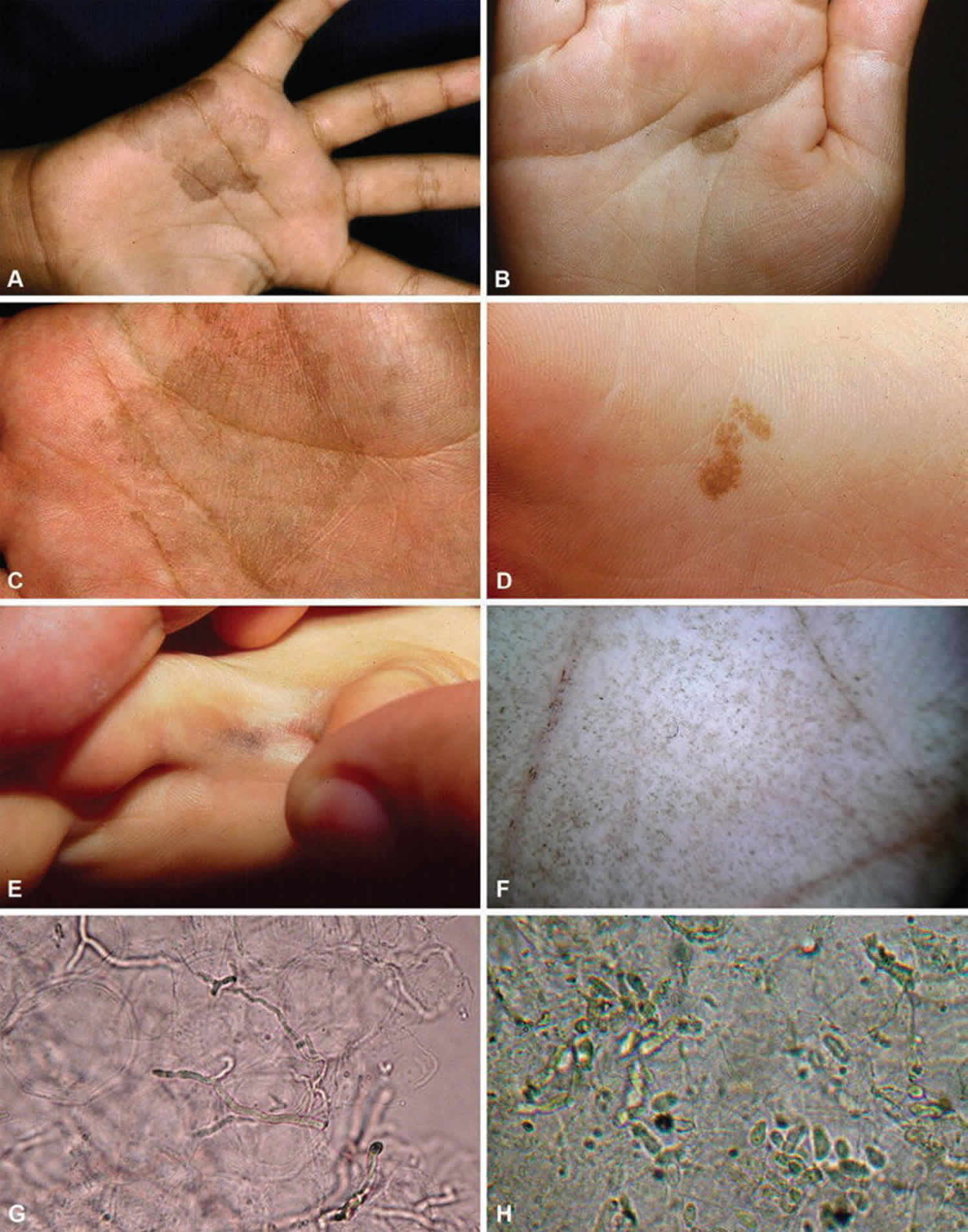
Tinea nigra is a brown fungus (Exophiala phaeoannellomyces) skin infection. This mold (dermatophyte) usually inhabits soil. Tinea nigra affects the skin of the palm and/or sole with persistent slowly growing brown or black patches. Tinea nigra appears as a hyperpigmented macule, which usually occurs on the palms. The soles and, more rarely, other areas of the body, can also be affected. They are slightly scaly and do not itch or sting. Tinea nigra is most common in tropical regions and often infects those with a tendency to excessive sweating (hyperhidrosis).
The brown mold, Exophiala phaeoannellomyces, other names include:
- Hortaea werneckii
- Phaeoannellomyces werneckii
- Exophiala werneckii
- Cladosporium werneckii
Tinea nigra skin infection is sometimes confused with other skin conditions such as:
- Melanoma
- Benign moles (nevi)
- Stains
- Pigmentation arising after a dermatitis or other skin inflammation
Tinea nigra usually clears with topical antifungal applied for 2 -4 weeks.
Is tinea nigra contagious?
Tinea nigra is a superficial fungal infection of the stratum corneum. Tinea nigra infection is believed to occur as a result of inoculation from a contamination source such as soil, sewage, wood, or compost subsequent to trauma in the affected area.
Tinea nigra causes
Tinea nigra is due to infection by the fungus, Hortaea werneckii or Exophiala phaeoannellomyces, which is classified in the family Dematiaceae, class Hyphomycetes, phylum Deuteromycota. Infection occurs after inoculation subsequent to trauma. The dermatomycosis tends to occur in areas with an increased concentration of eccrine sweat glands. Hyperhidrosis appears to be a risk factor for this disease.
Tinea nigra symptoms
Tinea nigra is characterized by the presence of a painless brown-to-black macule. Generally, patients with tinea nigra are asymptomatic. Rarely, itch may be reported. The absence of any discomfort often delays the patient’s decision to seek medical advice.
Patients who live in the inland areas of the United States generally report a history of foreign travel, most often to the Caribbean islands. In addition, patients may have acquired this infection while visiting the tropical regions of Asia or Africa. Those who reside in the coastal regions do not necessarily report any travel outside of the United States.
Uezato et al 1 reported a case of tinea nigra palmaris from Okinawa, Japan on the left palm of a 13-year-old girl, who had noticed the pigmented, asymptomatic macule on her left palm approximately 4-5 years prior to presentation. She stated the lesion became lighter after a bath and darkened some time later. Physical examination revealed a 4 X 5-cm, dark brown, and irregularly shaped macule.
Histological findings were reported as follows: “Direct potassium hydroxide (KOH) microscopic examination from skin scrapings revealed branched brown hyphae with light brown septa. A fungal culture on Sabouraud’s agar media produced wet, medium brown, yeast-like colonies, the surface of which later became black and shiny. A slide culture disclosed light brown, elliptic or peanut-shaped conidia comprised of one to two ampullaceous cells. Scanning electron microscopic examination of the conidia showed both annellation [sic] conidia with lunate bud scars and sympodial conidiogenesis.”
DNA was extracted from separately cultured fungi, and polymerase chain reaction with primers specific to Hortaea werneckii or Exophiala phaeoannellomyces was performed; results showed positive bands. Direct sequencing was performed with the DNA segments from the positive bands. Type C Hortaea werneckii was determined to be the causative fungus, based on the base sequences obtained, and tinea nigra due to Hortaea werneckii was diagnosed.
Tinea nigra diagnosis
Microscopic examination of skin scrapings treated with 20% potassium hydroxide (KOH) reveals thick, septate, branching hyphae that contain a dark pigment in their walls. Blastospores or chlamydoconidia may also be present. The hyphae can be clear in color, yellow or brown and are septate (this means they are divided into compartments by thick walls).
Culture grows black colonies of Phaeoannellomyces wernekii within a week. Culture of skin scrapings on Sabouraud agar at 25°C yields growth in approximately 1 week. Initially, yeastlike colonies that are shiny, black, and mucoid are present. Subsequently, the colonies become olivaceous brown and develop aerial mycelia in 2-3 weeks. Microscopic examination of the colonies reveals dematiaceous 2-celled yeast that produce annelloconidia in addition to dematiaceous, septate hyphae with conidia on intercalary annelides.
The diagnosis may also be made on skin biopsy because of characteristic histopathological features of tinea nigra.
Tinea nigra treatment
After tinea nigra is diagnosed on the basis of the findings from the patient’s history, physical examination, and appropriate laboratory test, a topical antifungal medication designed to eradicate the fungal infection should be applied to the respective area. Topical application of antifungal agents usually resolves tinea nigra within 2-4 weeks. Topical ketoconazole cream may be a good choice 2, as well other antifungals 3. Prolonged therapy may be necessary to prevent relapse. Repeated vigorous scrubbing or topical application of keratolytic agents can reduce pigmentation 4.
Spontaneous healing has been described but is rare 5.
A topical antifungal medication is a cream, solution, lotion, powder, gel, spray or lacquer applied to the skin surface to treat a fungal infection.
Topical antifungals can be obtained over the counter without a doctor’s prescription. They are generally applied to the affected area twice daily for two to four weeks, including a margin of several centimetres of normal skin. Treatment should continue for one or two weeks after the last visible rash has cleared. They can often cure a localized infection, although recurrence is common so repeated treatment is often necessary.
Many antifungal medications are suitable for both dermatophyte and yeast infections. Others are more specific to one or the other type of fungus.
- Whitfield ointment (3% salicylic acid, 6% benzoic acid in petrolatum)
- Undecylenic alkanolamide
- Ciclopirox olamine
- Imidazoles
- Bifonazole
- Clotrimazole
- Econazole
- Efinaconazole
- Ketoconazole
- Luliconazole
- Miconazole
- Sulconazole
- Tioconazole
- Allylamine
- Terbinafine
- Thiocarbamates
- Tolciclate
- Tolnaftate
- Benzoxaborole
- Tavaborole
Because tinea nigra infection is believed to occur after inoculation subsequent to trauma, patients should avoid potentially contaminated sources, such as soil, sewage, compost, and decaying wood.
Tinea nigra prognosis
Although the appearance of tinea nigra may be alarming because of its uncommon occurrence and its potential confusion with a more serious medical disorder (eg, malignant melanoma), tinea nigra is a benign disease that is easily curable.
- Uezato H, Gushi M, Hagiwara K, Kayo S, Hosokawa A, Nonaka S. A case of tinea nigra palmaris in Okinawa, Japan. J Dermatol. 2006 Jan. 33(1):23-9.[↩]
- Noguchi H, Hiruma M, Inoue Y, Miyata K, Tanaka M, Ihn H. Tinea nigra showing a parallel ridge pattern on dermoscopy. J Dermatol. 2015 May. 42 (5):518-20.[↩]
- Rossetto AL, Cruz RC. Tinea nigra: successful treatment with topical butenafine. An Bras Dermatol. 2012 Nov-Dec. 87(6):939-41.[↩]
- Tilak R, Singh S, Prakash P, Singh DP, Gulati AK. A case report of tinea nigra from North India. Indian J Dermatol Venereol Leprol. 2009 Sep-Oct. 75(5):538-9.[↩]
- Rossetto AL, Cruz RC. Spontaneous cure in a case of Tinea nigra. An Bras Dermatol. 2012 Feb. 87(1):160-2.[↩]