Torus palatinus
Torus palatinus is a harmless and painless bony exostosis (bony growth) occurring in the midline of the hard palate of the maxilla that affects 20 to 30% of people in the United States 1. The word “palatinus” refers to the roof of the mouth. Torus (meaning “to stand out” or “lump” in Latin) 2 is an exostosis (also called osteoma, is a benign growth of new bone on top of existing bone) that are formed by a dense cortical and limited amount of bone marrow, and they are covered with a thin and poorly vascularized mucosa 3. These bony growths are covered by a thin mucosa that is susceptible to lacerations 4, which could cause perioperative bleeding and swelling if traumatized. Torus palatinus is more common in women and in people of Asian and Inuit ancestry 4.
Tori can be unilobular or multilobulated and pedunculated or flat. Large tori that protrude more than 5 mm from the maxilla comprise less than 5% of tori 3.
Torus palatinus are usually located at the longitudinal ridge of the half palatine, on the union of the palatine apophysis of the maxillae or on the internal side of the horizontal branch of the jaw, above the mylohyoid line and at the level of the premolar area 5 and canine area 6, presenting a very slow 7 and progressive growth that can stop spontaneously 2. This slowly growing benign lesion can take decades to grow into a noticeable size and patients generally do not report them as they are asymptomatic 8. In the cases in which a torus interferes with dental work, such as fitting dentures or prosthetic devices, or in the process of mastication, surgical removal might be warranted 4.
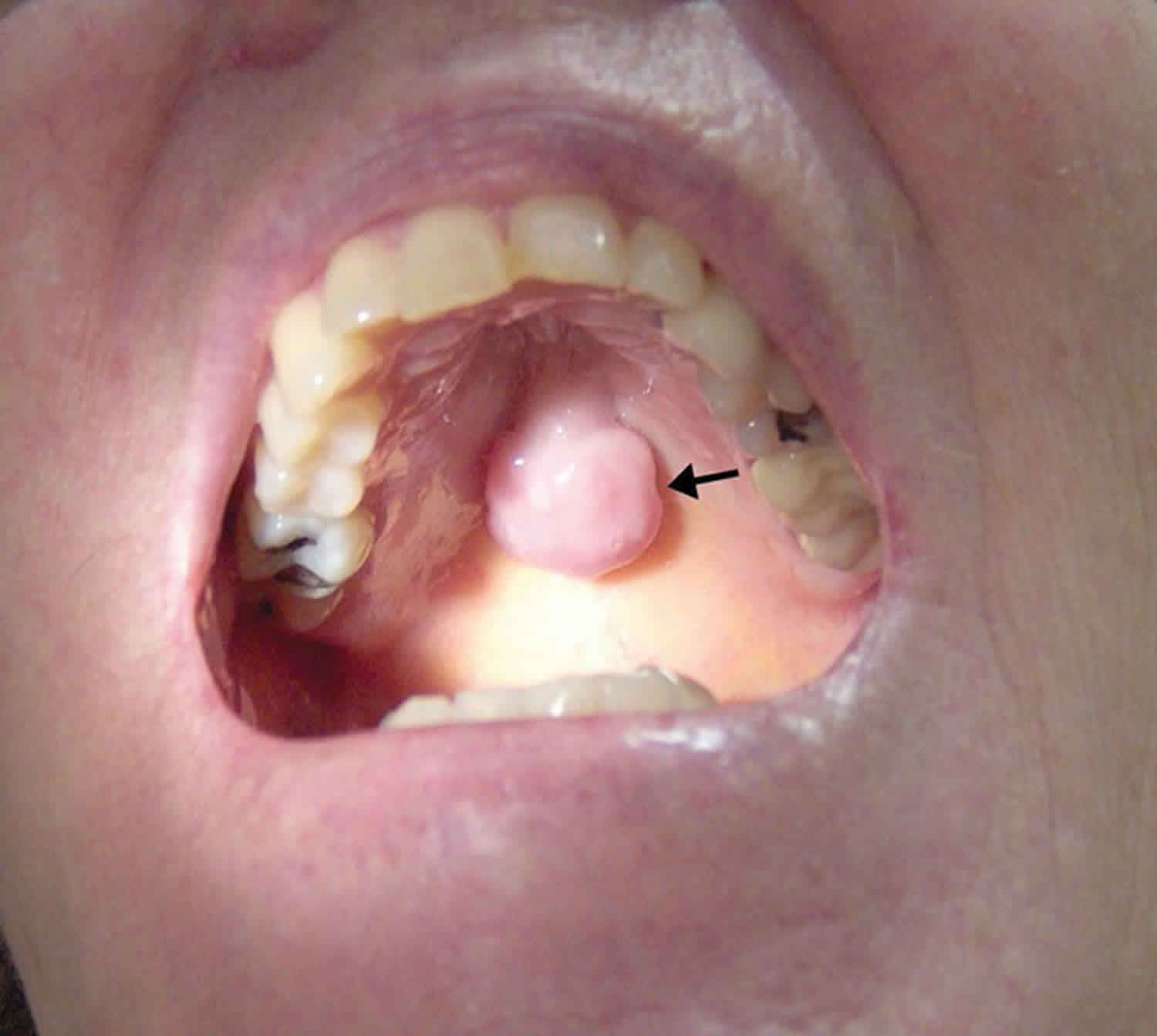
Large tori can develop sites that trap food 3, shown in the photograph (Figure 1) with a potential cavity between the base of the lesion and the hard palate (arrow), thus posing an aspiration risk if any trapped food material is dislodged while establishing an airway.
Beyond the interference with dental work, complications of oral tori are rare, and generally at the case report level. Oral tori have also been linked to low bone mineral density, but are felt to be secondary to the underlying process 9. This may explain why torus palatinus is found more commonly in women than men. Tori have been reported to be subject to bisphosphonate-induced osteonecrosis, so this should be included in the differential of oral pain in the appropriate population 10.
Figure 1. Torus palatinus
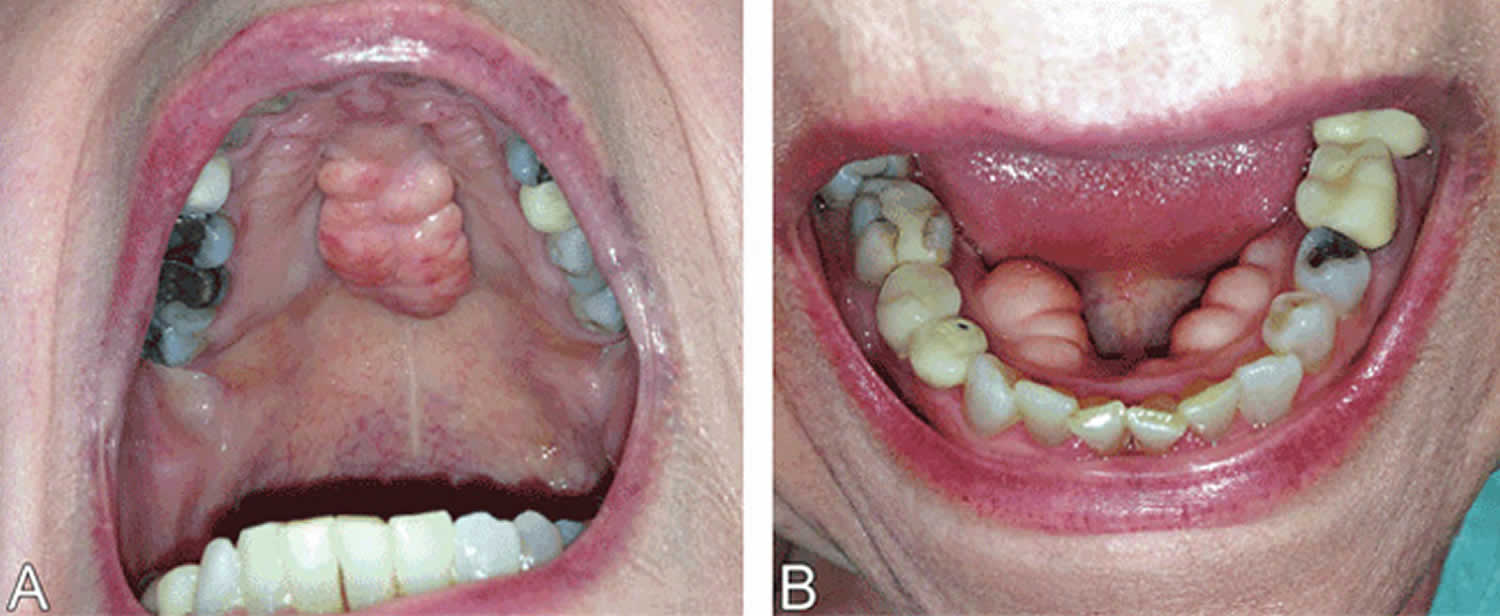
Figure 2. Torus palatinus (palatine torus) and torus mandibularis (mandibular torus)
Footnote: Torus palatinus (left, A) is an exostosis arising from the median raphe of the palatine bone, whereas torus mandibularis (right, B) arises in the premolar area of the lingual surface of the mandible. These bony excrescences are benign, are usually asymptomatic, and require no treatment.
Torus palatinus causes
The exact cause of torus palatinus is not well-understood, and appears to be a complex interplay of occlusive (biting) forces 11, genetics 12 and environmental factors 13. Medical conditions associated with bone disruption, e.g., hyperparathyroidism (of any type), have also been found to be associated with torus development 14.
Tori are more common in females and in specific ethnic and racial groups, especially Asians 15.
The most widely accepted theory today is genetics 3, but it has not always been
possible to show the autosomal dominant nature of its appearance 16. In the three clinical cases analyzed by Curran et al. 17, in which a daughter, mother and grandmother had autosomal dominant osteosclerosis, torus mandibularis and torus palatinus were found to be present in all three women. In the study by Eggen 18, it was only possible to estimate the genetic origin
of the torus mandibularis in 29.5% of the cases; as for the rest of the cases, approximately 70%, the origin was attributed to environmental factors, mainly related to occlusal stress.
Another cause is superficial injuries 7 or its occurrence as a functional response in individuals with well developed chewing muscles 19 or in patients with abraded teeth due to occlusion 20. In the study conducted by Reichart et al. 21, they found a significant correlation between the incidence of torus and the presence of abraded teeth in Thais, but not in Germans. In studies conducted by Sirirungrojying et al. 22, Clifford et al. 23 and Kerdpon et al. 24, they found a large relationship between the torus mandibularis and parafunctional habits, which they did not find with the torus palatinus. Thus, Sirirungrojying et al. 22, Clifford et al. 23 determined that torus mandibularis can be used to indicate the risk of appearance of temporomandibular disorders.
As possible causes, other authors mention eating habits 11, states of vitamin deficiency or supplements rich in calcium 19 and also diet 25. In the studies conducted by Eggen et al. 26 and Al-Bayaty et al. 25, they associate the consumption of fish with the presence of tori, because fish contains omega-3 unsaturated fatty acids and vitamin D, encourages bone growth.
Sasaki et al. 27 tried to draw a relationship between the occurrence of tori and the prolonged use of phenytoin, but were unable to conclude that it was what caused the appearance of the tori. However, they did determine that it is a factor that leads to an increase in size, because it induces an increase in calcium homeostasis, functioning as an osteogenic agent.
Lastly, and possibly maintaining a certain relationship with the aforementioned injuries, Sonnier et al. 28 associate the presence of teeth at the mandibular level with the presence torus. To further support this, in the study conducted by Eggen et al. 29, they found a relationship
between the presence of torus and the number of teeth present in the mouth. In addition, among adolescents with mandibular tori, the ratio of non-erupted canines was much smaller than those who did not have any tori. Furthermore, in another study, Eggen 30 found a relationship between the presence of mandibular tori and a normal bone height around the teeth.
Torus palatinus symptoms
Torus palatinus is usually asymptomatic and is found an incidental finding during a routine clinical exam. In cases of significant growth or in edentulous patients, in which case torus palatinus may hinder the construction of the prosthesis.
Sometimes patients may present phonatory disturbances, limitation of masticatory mechanics, ulcerations of the mucosa, food deposits, prosthetic instability, and some patients may experience cancerophobia, and consult a professional in order to look for a solution 19.
Torus palatinus signs and symptoms:
- Hard lump protruding from the midline hard palate into the mouth covered with normal mucous membrane.
- Small size (<2 mm) appear most frequent (70% to 91%).
- Shapes include flat, nodular, lobular, or spindle-shaped; nodular appear most common.
Torus palatinus complications
Torus palatinus usually don’t cause any complications, and many medical experts advise against having them removed in most cases. However, certain situations may call for surgical removal, such as when a person needs to be fitted for dental prosthetics. Your dentist can explain if you’re a good candidate for removal.
Torus palatinus diagnosis
In most torus palatinus cases, the finding is usually incidental and observed during clinical examination at the dental office. This is because they are asymptomatic for the most part, and those who have torus are not aware of it 25.
Torus palatinus are diagnosed by clinical examination:
- The torus palatinus can be unilobular, polylobulated, flat and spindle-shaped, located at the midline of the hard palate 19.
- The torus mandibularis are usually symmetrical and bilateral 2, but can also be unilateral 31, located on the lingual side of the mandible, above the mylohyoid line and at the level of the premolars 25.
- X-rays taken reveal radiodense images with a slightly higher density than that of the surrounding bone 31.
- Carrying out X-rays (periapical, occlusal, and panoramic) is not very useful, given the simplicity of the diagnosis during clinical examination 19.
Histopathological examination reveals that torus palatinus is similar to the compact structure of the normal bone, having a slightly spongy structure with marrow spaces 31.
Torus palatinus differential diagnosis
Oral torus must be differentiated from other growths in the mouth including fibromas, mucoceles, osteomas, osteochondromas, and osteoid osteomas. However, oral tori can usually be distinguished from other conditions on the basis of clinical findings alone. Biopsy may be warranted if there is doubt. Tori tend to grow gradually throughout life and do not have potential for malignant transformation. Although they are typically asymptomatic, removal is sometimes warranted for proper fitting of prostheses or for use in autogenous cortical bone grafting.
Torus palatinus treatment
Torus palatinus has a benign natural history and is slow growing and noninvasive. Removal of the tori is not always necessary. Removal is required only if they are symptomatically burdensome or interfere with denture placement in edentate individuals.
The most frequent cause of extirpation continues to be the need for prosthetic treatment 7 or that of being a potential source of autogenous cortical bone for grafts in periodontal surgery, cyst surgery or implant surgery 32, although long-term stability of the grafts is uncertain.
Other authors do not recommend the removal of tori except in very extreme cases, and they recommended the removal of the prosthesis in these areas 7 or the use of soft acrylics on the edges of the prosthesis 33.
Barker et al. 5 used the bone obtained from the torus mandibularis of a patient in order to increase the thickness of his upper jaw and allow the placement of implants, in order to replace the lateral incisors and absent canines. They determined that the torus mandibularis provided a useful and local source of bone in procedures for increasing bone thickness. Proussaefs 32 discusses three clinical cases in which he makes a clinical and histological evaluation of the use of mandibular tori as grafts in order to place implants, in which he obtained up to a 4.33 mm increase in thickness and an absorption rate similar to the grafts that are made with bone from other donor areas of the oral cavity.
Torus palatinus surgery
Reasons for torus palatinus removal:
- Disturbances of phonation
- Limitation of masticatory mechanics
- Sensitivity due to the thin mucosa layer
- Traumatic inflammation
- Ulcer of a traumatic origin
- Retention of food remains
- Esthetic reasons
- Prosthetic instability
- Patients with cancerophobia
- Prosthetic treatment
- Source of autogenous cortical bone for grafts 28
The use of general anesthesia is not indicated for this type of surgery, given that it poses a risk to the patient, and based on the fact that its systematic use is not justified 2.
For the removal of the torus palatinus, the nasopalatine nerve must be anesthetized at its exit through the anterior palatine foramen, and the anterior palatine nerves must be anesthetized through the posterior palatine foramen. In addition, the anesthesia will be administered by perilesional infiltration in order to facilitate the detachment of the palatine fibromucosa 31.
Different incisions can be made in order to perform the removal of the torus palatinus. The most common type of incision used is the double-Y incision, because it prevents injury of the nasopalatine and anterior palatine blocks 2. The incision will be a total thickness 2.
Periostotomes will be used for the detachment, and separate the fibromucosa until the lesion is exposed 2. As mentioned earlier, the mucosa that covers the torus is very thin, which makes it tear easily if you are not careful 2. The flaps can be anchored by suturing to the teeth, or by separating them using Farabeuf in order to avoid damaging them while performing the operation 2.
Initially, the excision will be performed using a fissure bur, which the maxillofacial surgeon wiil use to divide the torus; then they will use a chisel to cut into each of the divisions, or alternatively, a large burr or a file may be used to reshape the bone or to even it out 7. If the torus is not very large, it is not necessary to divide it; it can be removed directly with a burr. Castro Reino et al. 2 advocate the use of a high speed turbine cooled with normal saline solution, given that they consider the use of a chisel and hammer involves a greater risk of iatrogenic injury, and also to avoid the bumping the patient with the chisel; however, we must take into account the risk that this may cause emphysema.
By removing the torus and relocating the flaps, you will end up with too much soft tissue, which can be removed with scissors. The suture may be made by simple points, mattress sutures, etc., provided they are not too tight 2
Surgical cement is used to protect the wound from traumatic and mechanical force during the healing process, so as to achieve a bacteriostatic or bactericidal action if it contains an agent with these properties, and to prevent the accumulation of food remains 2
In the torus palatinus, a surgical splint should be placed over the surgical cement for a period of 48 hours, and is removed when reviewing the wound. The patient’s former relined and adjusted prosthesis can also be reseated 2.
Torus palatinus surgery complications
Although it is uncommon, complications can occur:
- Perforation of the nasal cavities
- Secondary anesthesia due to palatine nerve damage
- Bone necrosis due to poor refrigeration during surgical drilling
- Hemorrhage due to section of palatine arteries
- Dilaceration of the palatine mucosa
- Fracture of the palatine bone
Post-operative care
The patient must be informed that the signs and symptoms that may occur during the postoperative period will be those that are most commonly associated with this type of surgical procedure, such as edema, hematoma, mild pain, etc. Postoperative medication will consist of antibiotics, analgesics and anti-inflammatory medicine, as well as stressing that it is important for the patient to continue with appropriate personal hygiene so that the wound may heal properly 2.
- Loukas M, Hulsberg P, Tubbs RS, et al. The tori of the mouth and ear: a review. Clin Anat. 2013;26(8):953–960. doi:10.1002/ca.22264 https://doi.org/10.1002/ca.22264[↩]
- Castro Reino O, Perez Galera J, Perez Cosio Martin J, Urbon Caba-llero J. Surgical techniques for the exeresis of torus, both palatal and mandibular. We observe indications, contraindications and compli-cations as well as enumerate all the right events to realize correctly the said techniques. [Surgery of palatal and mandibular torus]. Rev Actual Odontoestomatol Esp. 1990;50:47-50, 53-6.[↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩]
- García-García AS, Martínez-González JM, Gómez-Font R, Soto-Rivadeneira A, Oviedo-Roldán L. Current status of the torus palatinus and torus mandibularis. Med Oral Patol Oral Cir Bucal. 2010;15(2):e353–e360. Published 2010 Mar 1. http://www.medicinaoral.com/pubmed/medoralv15_i2_pe353.pdf[↩][↩][↩][↩]
- Loukas M, Hulsberg P, Tubbs RS, et al. The tori of the mouth and ear: a review. Clin Anat. 2013. November;26(8):953–960.[↩][↩][↩]
- Barker D, Walls AW, Meechan JG. Ridge augmentation using mandibular tori. Br Dent J. 2001;190:474-6.[↩][↩]
- Jainkittivong A, Langlais RP. Buccal and palatal exostoses: pre-valence and concurrence with tori. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2000;90:48-53.[↩]
- Donado M. Pre-prosthetic Surgery. In: Donado M, ed. Cirugía bu-cal. Patología y técnica. [Oral Surgery. Pathology and Technique] 2th ed. Barcelona: Masson; 1998. p. 481-510.[↩][↩][↩][↩][↩]
- Komori T, Takato T. Time-related changes in a case of torus palatinus. JOMOS. 1998;56(4):492–494.[↩]
- Lo JC, O’Ryan F, Yang J, et al. Oral Health Considerations in Older Women Receiving Oral Bisphosphonate Therapy. J Am Geriatr Soc. 2011;59(5):916–922.[↩]
- Goldman ML, Denduluri N, Berman AW, et al. A Novel Case of Bisphosphonate-Related Osteonecrosis of the Torus Palatinus in a Patient with Metastatic Breast Cancer. Oncology. 2006;71:306–308.[↩]
- Al-Bayaty HF, Murti PR, Matthews R, Gupta PC. An epidemiolo-gical study of tori among 667 dental outpatients in Trinidad & Toba-go, West Indies. Int Dent J. 2001;51:300-4[↩][↩]
- Gorsky M, Bukai A, Shohat M. Genetic influence on the prevalence of torus palatinus. Am J Med Genet. 1998;75(2):138–140.[↩]
- Morrison MD, Tamimi F. Oral tori are associated with local mechanical and systemic factors: A case-control study. JOMOS. 2013;71(1):14–22.[↩]
- Padbury AD, Tözüm TF, Taba M, et al. The Impact of primary hyperparathyroidism on the oral cavity. J Clin Endocrinol Metab. 2006;91(9):3439–3445.[↩]
- Chohayeb AA, Volpe AR. Occurrence of torus palatinus and mandibularis among women of different ethnic groups. Am J Dent. 2001;14(5):278–280.[↩]
- Bruce I, Ndanu TA, Addo ME. Epidemiological aspects of oral tori in a Ghanaian community. Int Dent J. 2004;54:78-82.[↩]
- Curran AE, Pfeffle RC, Miller E. Autosomal dominant osteos-clerosis: report of a kindred. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1999;87:600-4.[↩]
- Eggen S. Torus mandibularis: an estimation of the degree of ge-netic determination. Acta Odontol Scand. 1989;47:409-15.[↩]
- Martínez-González JM. Tumores benignos de los maxilares [Be-nign tumors of the maxilla]. In: Donado M, ed. Cirugía Bucal. Pato-logía y Técnica. 2th ed. Barcelona: Masson; 1998. p. 627-639.[↩][↩][↩][↩][↩]
- Eggen S, Natvig B. Variation in torus mandibularis prevalence in Norway. A statistical analysis using logistic regression. Community Dent Oral Epidemiol. 1991;19:32-5.[↩]
- Reichart PA, Neuhaus F, Sookasem M. Prevalence of torus palati-nus and torus mandibularis in Germans and Thai. Community Dent Oral Epidemiol. 1988;16:61-4.[↩]
- Sirirungrojying S, Kerdpon D. Relationship between oral tori and temporomandibular disorders. Int Dent J. 1999;49:101-4.[↩][↩]
- Clifford T, Lamey PJ, Fartash L. Mandibular tori, migraine and temporomandibular disorders. Br Dent J. 1996;180:382-4.[↩][↩]
- Kerdpon D, Sirirungrojying S. A clinical study of oral tori in southern Thailand: prevalence and the relation to parafunctional ac-tivity. Eur J Oral Sci. 1999;107:9-13.[↩]
- Al-Bayaty HF, Murti PR, Matthews R, Gupta PC. An epidemiolo-gical study of tori among 667 dental outpatients in Trinidad & Toba-go, West Indies. Int Dent J. 2001;51:300-4.[↩][↩][↩][↩]
- Eggen S, Natvig B, Gåsemyr J. Variation in torus palatinus preva-lence in Norway. Scand J Dent Res. 1994;102:54-9.[↩]
- Sasaki H, Ikedo D, Kataoka M, Kido J, Kitamura S, Nagata T. Pro-nounced palatal and mandibular tori observed in a patient with chro-nic phenytoin therapy: a case report. J Periodontol. 1999;70:445-8.[↩]
- Sonnier KE, Horning GM, Cohen ME. Palatal tubercles, palatal tori, and mandibular tori: prevalence and anatomical features in a U.S. population. J Periodontol. 1999;70:329-36.[↩][↩]
- Eggen S, Natvig B. Relationship between torus mandibularis and number of present teeth. Scand J Dent Res. 1986;94:233-40.[↩]
- Eggen S. Correlated characteristics of the jaws: association bet-ween torus mandibularis and marginal alveolar bone height. Acta Odontol Scand. 1992;50:1-6.[↩]
- Castro Reino O, Perez Galera J, Perez Cosio Martin J, Urbon Caba-llero J. Surgical techniques for the exeresis of torus, both palatal and mandibular. We observe indications, contraindications and complications as well as enumerate all the right events to realize correctly the said techniques. [Surgery of palatal and mandibular torus]. Rev Actual Odontoestomatol Esp. 1990;50:47-50, 53-6.[↩][↩][↩][↩]
- Proussaefs P. Clinical and histologic evaluation of the use of mandibular tori as donor site for mandibular block autografts: report of three cases. Int J Periodontics Restorative Dent. 2006;26:43-51.[↩][↩]
- Abrams S. Complete denture covering mandibular tori using three base materials: a case report. J Can Dent Assoc. 2000;66:494-6.[↩]