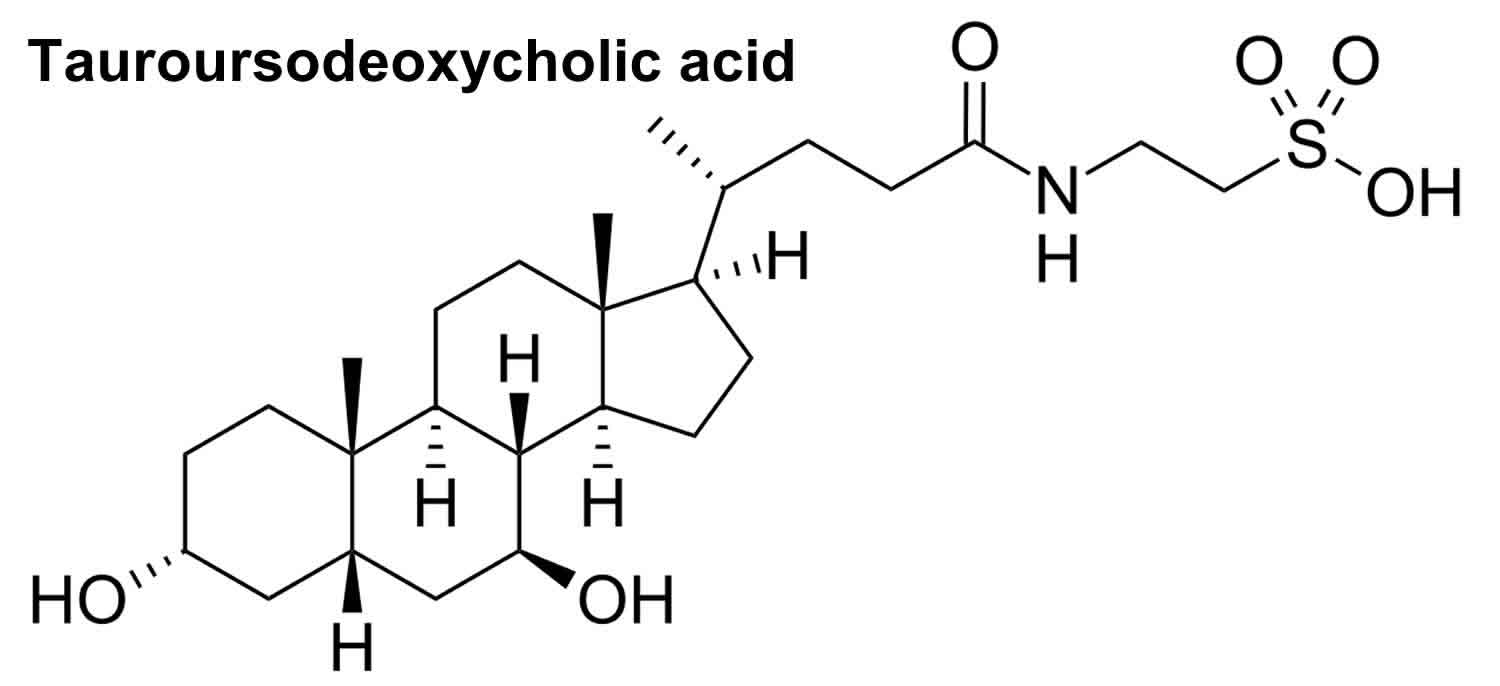
What is TUDCA
TUDCA is short for tauroursodeoxycholic acid, is a taurine-conjugated bile acid derived from ursoodeoxycholic acid (UDCA) that is produced in the human liver and is presented at a very low level in human bile (but at a high level in bear bile) and is used in traditional Chinese medicine for treatment of chronic cholestatic liver disease (a condition in which bile fails to flow from the liver to the duodenum) and cholesterol gallstones (dissolving gallstones to a size in which they may be passed) 1. When bile salts reach the intestines, they can be metabolized by bacteria into ursodeoxycholic acid (UDCA). TUDCA (tauroursodeoxycholic acid) is formed when taurine binds to ursoodeoxycholic acid (UDCA). TUDCA is not approved by the U.S. Food and Drug Administration (FDA), while UDCA (ursodeoxycholic acid) is approved in the United States for the treatment of primary biliary cirrhosis (previously primary biliary cihrrosis) 2. In addition, some studies have found that TUDCA can inhibit the inflammatory response of cells and block oxidative stress and caspase-1 activation, thus inhibiting the apoptosis of hepatocytes and liver injury 3. Previous studies have showed that TUDCA can significantly reduce brain injury and improve neurological function associated with acute hemorrhagic stroke or acute ischemic stroke in rats through inhibiting neuronal apoptosis 4.
TUDCA can be taken orally or injected intraperitoneally and intravenously 5. In a multicenter study, TUDCA was as safe and efficacious as ursodeoxycholic acid (UDCA) in Chinese patients with primary biliary cholangitis and it was better for relieving symptoms than UDCA 6. Studies have reported that TUDCA could have a crucial role in preventing apoptosis 7, suppressing adipogenesis of adipose-derived mesenchymal stem cells 8, promoting angiogenesis 9 and enhancing osteogenic differentiation of bone marrow-derived mesenchymal stem cells 10. In recent years, experimental studies found TUDCA to have important anti-apoptosis effects and potential neuroprotective activity. For example, studies have confirmed that TUDCA has excellent effects on nervous system diseases by reducing the apoptosis of nerve cells 11. Yanguas-Casás et al. 12 found that TUDCA had significant anti-inflammatory effect and could effectively inhibit the inflammation of neuron and the over-activation of microglia in acute neuritis model of mice. Dionísio et al. 13 showed that TUDCA inhibited inflammation and over-deposition of beta-amyloid protein in Alzheimer’s disease in mice, which is a promising strategy in Alzheimer’s disease treatment. In addition, in the study of spinal cord injury, Zhang et al. 14 found that TUDCA could reduce the damage by inhibiting the up-regulation of CIBZ gene, suppressing oxidative stress and reducing neuronal apoptosis. All the above animal studies have proven the excellent neuro-protective effect of TUDCA in spinal cord injury. Similarly, another study involving rats also confirmed that TUDCA could improve Basso Beattie Bresnahan scores and pathologic injury of spinal cord, and reduce apoptosis of spinal cord tissue 5.
TUDCA benefits
TUDCA effects in healthy adults are unknown, but TUDCA increases insulin sensitivity, decreases total (and HDL) cholesterol, and reduces inflammation.
Liver disease
Randomized controlled trials have shown that TUDCA treatment improves liver function in patients with liver cirrhosis 15, hepatitis C virus (HCV)-related chronic hepatitis 16, and cholestasis 17, a condition in which bile fails to flow from the liver to the duodenum. These studies have shown that TUDCA drastically lowers serum liver enzymes that are markers of liver inflammation (ALT, AST, and ALP). TUDCA effects on cholestasis are strong and it is used as a reference drug for these effects.
Insulin sensitivity
In a randomized controlled trial of 20 obese men and women with insulin resistance, TUDCA treatment (1750 mg/day) for 4 weeks resulted in a 30% increase in insulin sensitivity in the liver and muscle 18. Although TUDCA is reported to decrease endoplasmic reticulum (ER) stress, markers of ER stress were not altered in these subjects (from adipose tissue biopsy). Thus, the specific cellular mechanisms responsible for the increased insulin sensitivity are unclear. It is also unknown whether TUDCA is protective in healthy adults without insulin resistance.
High cholesterol
In a small dose-response study in 24 primary biliary cirrhosis patients, higher doses of TUDCA treatment (1000 or 1500 mg/day) for 6 months decreased both total cholesterol and high-density lipoprotein (HDL or “good”) cholesterol compared to baseline, while the low dose (500 mg/day) showed no change 19. Change ratios for total cholesterol were 1.01, 0.94, and 0.89 for 500, 1000, and 1500 mg, respectively. Change ratios for HDL cholesterol were 1.04, 0.81, and 0.81 for 500, 1000, and 1500 mg, respectively. There were no placebo controls in this study. The changes in cholesterol levels may be explained by the improvement of cholestasis and also by a decrease in cholesterol absorption. It is unknown whether TUDCA would have similar effects in people without liver disease.
Neuroinflammation
In a mouse model of neuroinflammation (lipopolysaccharide [LPS] injection), TUDCA treatment reduced the production of nitrites by microglial cells and astrocytes by inhibiting the NFkB pathway 20. A triple anti-inflammatory effect on glial cells was observed: 1) reduced glial cell activation, 2) reduced microglial cell migratory capacity, and 3) reduced expression of chemoattractants (e.g., MCP1) and vascular adhesion proteins (e.g., VCAM1) that are required for microglial migration and blood monocyteinvasion to the brain inflammation site.
Neuroprotective benefit
Promising for neuroprotection and potentially for Alzheimer’s disease therapy, but all evidence is currently based on animal studies. The most compelling study for neuroprotection is one in an Alzheimer’s disease mouse model (APP/PS1) where the treatment was started after pathology was present (7 months old). TUDCA treatment (500 mg/kg intraperitoneal, every 3 days) for 3 months significantly decreased Aβ deposition (Aβ40 and Aβ42) in the frontal cortex and hippocampus 21. The amyloidogenic processing of amyloid precursor protein was also reduced, indicating that TUDCA interferes with Aβ production. TUDCA also decreased glial activation and proinflammatory cytokine RNA expression (TNFα), while partially rescuing synaptic loss. Thus, even when started after disease onset, TUDCA was able to attenuate Aβ production and deposition, tau pathology, glial activation, and loss of synaptic function. Most of these effects are likely related to the activation of the Akt/GSK3β signaling pathway. Only a trend to improved spatial memory was found in TUDCA-treated APP/PS1 mice, likely because these mice already had extensive cognitive deficits. Several studies have shown in the same mouse model that when TUDCA diet (0.4% mixed in food) is started at 2 months of age (before significant amyloid deposits) and continued for 6 months, deficits in spatial, recognition, and contextual memory can be prevented 22. These actions were mediated in part through modulation of the gamma-secretase activity. This same treatment paradigm also prevented the decrease in PSD95 expression, suggesting a neuroprotective role of TUDCA at the synaptic level 23.
Other potential mechanisms of action for neuroprotection have been reported. A test tube study has shown that TUDCA can directly suppress Aβ-induced disruption of the mitochondrial membrane structure, which correlates with mitochondrial health 24. A study from a cell culture model of Alzheimer’s reported that TUDCA reduces p53-induced apoptosis and modulates expression of the anti-apoptotic Bcl2 family 25. TUDCA also downregulates the expression of connective tissue growth factor (CTGF), which is present in the vicinity of Aβplaques and neurofibrillary tangles and influences γ-secretase activity 22.
Studies in mouse models of Huntington’s disease also reported neuroprotection with TUDCA. TUDCA increased neuronal survival, preserved mitochondria, and decreased huntingtin inclusions in the mouse striatum while reducing cognitive and sensorimotor deficits 26. The authors noted that“TUDCA can be administered orally or i.v., are accessible to the brain and other organs, and exhibit essentially no toxicity” 26.
A double-blind placebo controlled clinical trial was performed with a 54-week treatment with TUDCA at a dose of 2 g daily oral in 34 amyotrophic lateral sclerosis (ALS) patients currently taking riluzole as an add-on regimen 1. The treatment was well tolerated in all patients without any severe adverse effects beyond common gastrointestinal symptoms. TUDCA treatment for 1 year has potential neuroprotective effects with slowed deterioration of function in ALS patients, with a 15% increase in ALS functional rating scale (ALSFRS-R) scoring 1. Due to the aggressive nature of ALS, studies that improve deterioration rates or increase neuronal growth show a promising future for ALS research.
TUDCA dosage
TUDCA is available as a dietary supplement in capsule form. No studies or websites have directly compared efficacy, purity, or safety of the different brands. TUDCA doses used in clinical studies vary widely. As low as 10-13 mg per day has been shown to improve liver regenesis rates in people with chronic liver disease 27. Doses of 750 mg daily have been used in patients with liver cirrhosis 17. The dose used in mouse models of Alzheimer’s disease and Huntington’s disease that provided neuroprotection was 500 mg/kg (intraperitoneal) every 3 days, or a diet containing 0.4% TUDCA (roughly estimated at 12 mg/day, or 400 mg/kg/day) 21, 22. The human equivalent oral dose after taking into account differential body surface area is 32.5 mg/kg/day (or 1951 mg daily for a person weighing 60 kg).
TUDCA side effects
Gastrointestinal symptoms are a common side effects of TUDCA. In the TUDCA study group involving 129 Chinese patients with primary biliary cholangitis only 5 patients (3.8%) were considered to be study drug related: diarrhea in 1 case, itch in 2 cases, rash in 1 case and dysmenorrhea (period pain) in 1 case 6. TUDCA is safe and well-tolerated in patients with liver transplants, liver cirrhosis, and other diseases, but no clinical data exist for treatments longer than 1 year.
A Cochrane meta-analysis of 7 randomized controlled trials in liver-transplanted patients reported that bile acids including TUDCA were safe and well-tolerated 28. Of the 4 trials that reported adverse events, diarrhea was the only adverse event reported and occurred in only 2 trials.
There were no significant differences in adverse events between those receiving standard immunosuppressants versus those receiving bile acids in addition. Other trials in liver cirrhosis (up to 6 months) 15 and ALS (1 year) 29 have also reported that TUDCA is well-tolerated with diarrhea being the only side effect 17, 19.
References- Elia, A. E., Lalli, S., Monsurrò, M. R., Sagnelli, A., Taiello, A. C., Reggiori, B., La Bella, V., Tedeschi, G., & Albanese, A. (2016). Tauroursodeoxycholic acid in the treatment of patients with amyotrophic lateral sclerosis. European journal of neurology, 23(1), 45–52. https://doi.org/10.1111/ene.12664
- Kusaczuk M. (2019). Tauroursodeoxycholate-Bile Acid with Chaperoning Activity: Molecular and Cellular Effects and Therapeutic Perspectives. Cells, 8(12), 1471. https://doi.org/10.3390/cells8121471
- Paridaens A, Raevens S, Colle I, Bogaerts E, Vandewynckel YP, Verhelst X, Hoorens A, van Grunsven LA, Van Vlierberghe H, Geerts A, Devisscher L. Combination of tauroursodeoxycholic acid and N-acetylcysteine exceeds standard treatment for acetaminophen intoxication. Liver Int. 2017;37:748–756.
- Rodrigues CM, Sola S, Nan Z, et al. Tauroursodeoxycholic acid reduces apoptosis and protects against neurological injury after acute hemorrhagic stroke in rats. Proc Natl Acad Sci USA. 2003;100:6087–92.
- Dong, Y., Yang, S., Fu, B., Liu, F., Zhou, S., Ding, H., & Ma, W. (2020). Mechanism of tauroursodeoxycholic acid-mediated neuronal protection after acute spinal cord injury through AKT signaling pathway in rats. International journal of clinical and experimental pathology, 13(9), 2218–2227.
- Ma, H., Zeng, M., Han, Y., Yan, H., Tang, H., Sheng, J., Hu, H., Cheng, L., Xie, Q., Zhu, Y., Chen, G., Gao, Z., Xie, W., Wang, J., Wu, S., Wang, G., Miao, X., Fu, X., Duan, L., Xu, J., … Jia, J. (2016). A multicenter, randomized, double-blind trial comparing the efficacy and safety of TUDCA and UDCA in Chinese patients with primary biliary cholangitis. Medicine, 95(47), e5391. https://doi.org/10.1097/MD.0000000000005391
- Keene CD, Rodrigues CM, Eich T, Chhabra MS, Steer CJ, Low WC. Tauroursodeoxycholic acid, a bile acid, is neuroprotective in a transgenic animal model of Huntington’s disease. Proc Natl Acad Sci U S A. 2002 Aug 6;99(16):10671-6. doi: 10.1073/pnas.162362299
- Guo Q, Shi Q, Li H, Liu J, Wu S, Sun H, Zhou B. Glycolipid Metabolism Disorder in the Liver of Obese Mice Is Improved by TUDCA via the Restoration of Defective Hepatic Autophagy. Int J Endocrinol. 2015;2015:687938. doi: 10.1155/2015/687938. Epub 2015 Nov 19. Retraction in: Int J Endocrinol. 2020 Nov 28;2020:2138532
- Vettorazzi JF, Ribeiro RA, Borck PC, Branco RC, Soriano S, Merino B, Boschero AC, Nadal A, Quesada I, Carneiro EM. The bile acid TUDCA increases glucose-induced insulin secretion via the cAMP/PKA pathway in pancreatic beta cells. Metabolism. 2016 Mar;65(3):54-63. doi: 10.1016/j.metabol.2015.10.021
- Cha BH, Jung MJ, Moon BK, Kim JS, Ma Y, Arai Y, Noh M, Shin JY, Kim BS, Lee SH. Administration of tauroursodeoxycholic acid enhances osteogenic differentiation of bone marrow-derived mesenchymal stem cells and bone regeneration. Bone. 2016 Feb;83:73-81. doi: 10.1016/j.bone.2015.10.011
- Gronbeck KR, Rodrigues CM, Mahmoudi J, Bershad EM, Ling G, Bachour SP, Divani AA. Application of tauroursodeoxycholic acid for treatment of neurological and non-neurological diseases: is there a potential for treating traumatic brain injury? Neurocrit Care. 2016;25:153–166.
- Yanguas-Casás N, Barreda-Manso MA, Nieto-Sampedro M, Romero-Ramírez L. TUDCA: an agonist of the bile acid receptor GPBAR1/TGR5 with anti-inflammatory effects in microglial cells. J Cell Physiol. 2017;232:2231–2245.
- Dionísio PA, Amaral JD, Ribeiro MF, Lo AC, D’Hooge R, Rodrigues CM. Amyloid-β pathology is attenuated by tauroursodeoxycholic acid treatment in APP/PS1 mice after disease onset. Neurobiol Aging. 2015;36:228–240.
- Zhang ZM, Chen J, Chen FH, Yu DL, Li R, Lv CL, Wang HS, Li HL, Li J, Cai YF. Tauroursodeoxycholic acid alleviates secondary injury in the spinal cord via up-regulation of CIBZ gene. Cell Stress Chaperones. 2018;23:551–560.
- Pan XL, Zhao L, Li L, Li AH, Ye J, Yang L, Xu KS, Hou XH. Efficacy and safety of tauroursodeoxycholic acid in the treatment of liver cirrhosis: a double-blind randomized controlled trial. J Huazhong Univ Sci Technolog Med Sci. 2013 Apr;33(2):189-194. doi: 10.1007/s11596-013-1095-x
- Crosignani A, Budillon G, Cimino L, Del Vecchio Blanco C, Loguercio C, Ideo G, Raimondo G, Stabilini R, Podda M. Tauroursodeoxycholic acid for the treatment of HCV-related chronic hepatitis: a multicenter placebo-controlled study. Hepatogastroenterology. 1998 Sep-Oct;45(23):1624-9.
- Ma H, Zeng M, Han Y, Yan H, Tang H, Sheng J, Hu H, Cheng L, Xie Q, Zhu Y, Chen G, Gao Z, Xie W, Wang J, Wu S, Wang G, Miao X, Fu X, Duan L, Xu J, Wei L, Shi G, Chen C, Chen M, Ning Q, Yao C, Jia J. A multicenter, randomized, double-blind trial comparing the efficacy and safety of TUDCA and UDCA in Chinese patients with primary biliary cholangitis. Medicine (Baltimore). 2016 Nov;95(47):e5391. doi: 10.1097/MD.0000000000005391
- Kars M, Yang L, Gregor MF, Mohammed BS, Pietka TA, Finck BN, Patterson BW, Horton JD, Mittendorfer B, Hotamisligil GS, Klein S. Tauroursodeoxycholic Acid may improve liver and muscle but not adipose tissue insulin sensitivity in obese men and women. Diabetes. 2010 Aug;59(8):1899-905. doi: 10.2337/db10-0308
- Crosignani A, Battezzati PM, Setchell KD, Invernizzi P, Covini G, Zuin M, Podda M. Tauroursodeoxycholic acid for treatment of primary biliary cirrhosis. A dose-response study. Dig Dis Sci. 1996 Apr;41(4):809-15. doi: 10.1007/BF02213140
- Yanguas-Casás, N., Barreda-Manso, M. A., Nieto-Sampedro, M., & Romero-Ramírez, L. (2014). Tauroursodeoxycholic acid reduces glial cell activation in an animal model of acute neuroinflammation. Journal of neuroinflammation, 11, 50. https://doi.org/10.1186/1742-2094-11-50
- Dionísio PA, Amaral JD, Ribeiro MF, Lo AC, D’Hooge R, Rodrigues CM. Amyloid-β pathology is attenuated by tauroursodeoxycholic acid treatment in APP/PS1 mice after disease onset. Neurobiol Aging. 2015 Jan;36(1):228-40. doi: 10.1016/j.neurobiolaging.2014.08.034
- Lo AC, Callaerts-Vegh Z, Nunes AF, Rodrigues CM, D’Hooge R. Tauroursodeoxycholic acid (TUDCA) supplementation prevents cognitive impairment and amyloid deposition in APP/PS1 mice. Neurobiol Dis. 2013 Feb;50:21-9. doi: 10.1016/j.nbd.2012.09.003
- Ramalho RM, Nunes AF, Dias RB, Amaral JD, Lo AC, D’Hooge R, Sebastião AM, Rodrigues CM. Tauroursodeoxycholic acid suppresses amyloid β-induced synaptic toxicity in vitro and in APP/PS1 mice. Neurobiol Aging. 2013 Feb;34(2):551-61. doi: 10.1016/j.neurobiolaging.2012.04.018
- Rodrigues CM, Solá S, Brito MA, Brondino CD, Brites D, Moura JJ. Amyloid beta-peptide disrupts mitochondrial membrane lipid and protein structure: protective role of tauroursodeoxycholate. Biochem Biophys Res Commun. 2001 Feb 23;281(2):468-74. doi: 10.1006/bbrc.2001.4370
- Ramalho RM, Borralho PM, Castro RE, Solá S, Steer CJ, Rodrigues CM. Tauroursodeoxycholic acid modulates p53-mediated apoptosis in Alzheimer’s disease mutant neuroblastoma cells. J Neurochem. 2006 Sep;98(5):1610-8. doi: 10.1111/j.1471-4159.2006.04007.x
- Keene CD, Rodrigues CM, Eich T, Linehan-Stieers C, Abt A, Kren BT, Steer CJ, Low WC. A bile acid protects against motor and cognitive deficits and reduces striatal degeneration in the 3-nitropropionic acid model of Huntington’s disease. Exp Neurol. 2001 Oct;171(2):351-60. doi: 10.1006/exnr.2001.7755
- Panella C, Ierardi E, De Marco MF, Barone M, Guglielmi FW, Polimeno L, Francavilla A. Does tauroursodeoxycholic acid (TUDCA) treatment increase hepatocyte proliferation in patients with chronic liver disease? Ital J Gastroenterol. 1995 Jun;27(5):256-8.
- Chen W, Gluud C. Bile acids for liver-transplanted patients. Cochrane Database Syst Rev. 2005 Jul 20;(3):CD005442. doi: 10.1002/14651858.CD005442. Update in: Cochrane Database Syst Rev. 2010;(3):CD005442.
- Elia AE, Lalli S, Monsurrò MR, Sagnelli A, Taiello AC, Reggiori B, La Bella V, Tedeschi G, Albanese A. Tauroursodeoxycholic acid in the treatment of patients with amyotrophic lateral sclerosis. Eur J Neurol. 2016 Jan;23(1):45-52. doi: 10.1111/ene.12664. Epub 2015 Feb 9. Erratum in: Eur J Neurol. 2017 Apr;24(4):659.