Tzanck test
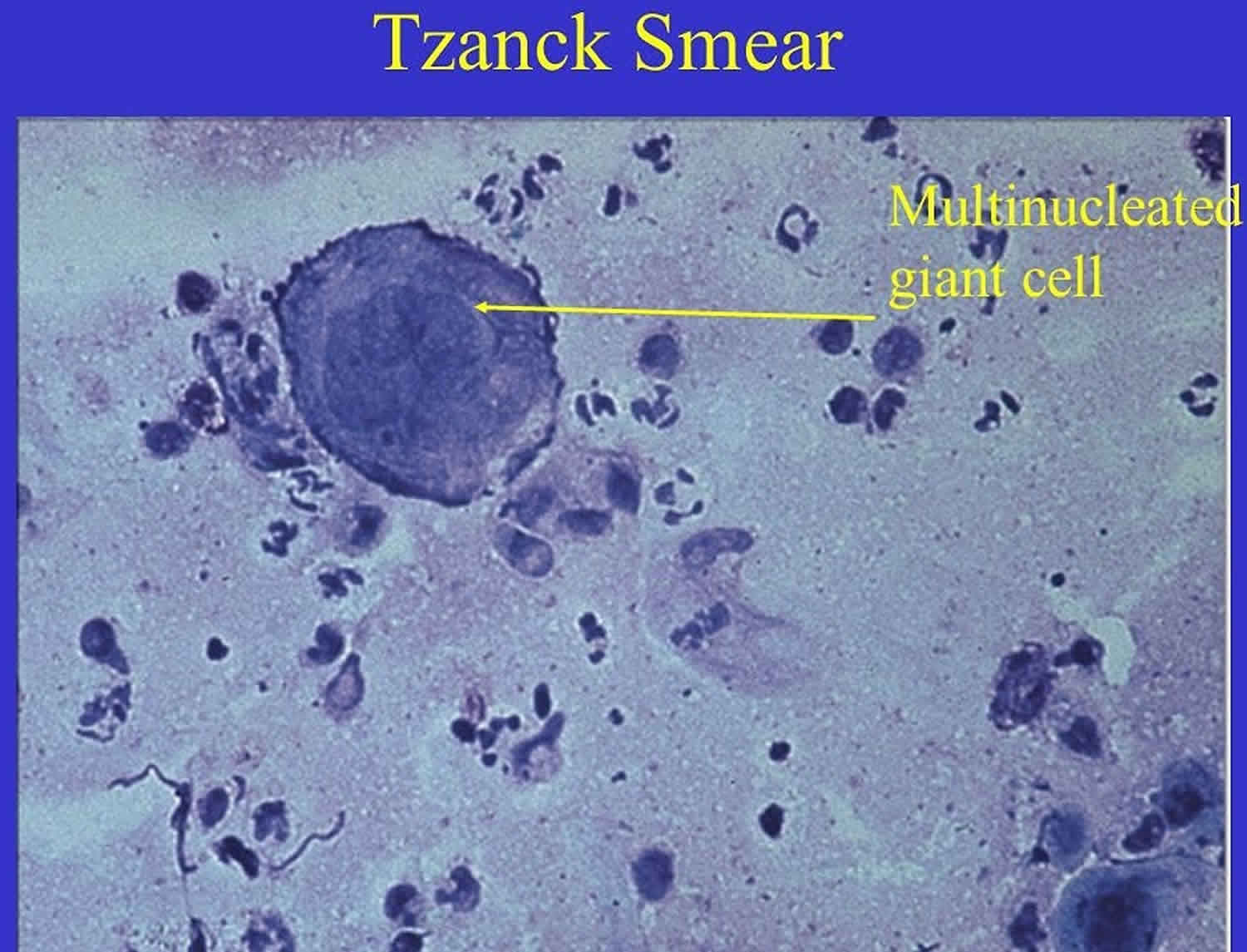
Tzanck test also Tzanck smear, is scraping of an ulcer base to look for Tzanck cells. Tzanck test is sometimes also called the Chickenpox skin test and the herpes skin test. The Tzanck test is named after Arnault Tzanck, a French dermatologist who described the technique in 1947 to distinguish various blistering conditions, especially herpes simplex 1. Atypical Tzanck cell is a large round keratinocyte with a hypertrophic nucleus, hazy or absent nucleoli, and abundant basophilic cytoplasm. The basophilic staining is deeper peripherally on the cell membrane due to the cytoplasm’s tendency to get condensed at the periphery, leading to a perinuclear halo. Tzanck cells commonly are found in: herpes simplex, varicella, herpes zoster and pemphigus vulgaris 2. The Tzanck smear is mainly used in an acute setting to rapidly detect a herpes infection or to distinguish Stevens- Johnson syndrome or toxic epidermal necrolysis from staphylococcal scalded skin syndrome. However, it can be used to diagnose a variety cutaneous infections and blistering diseases.
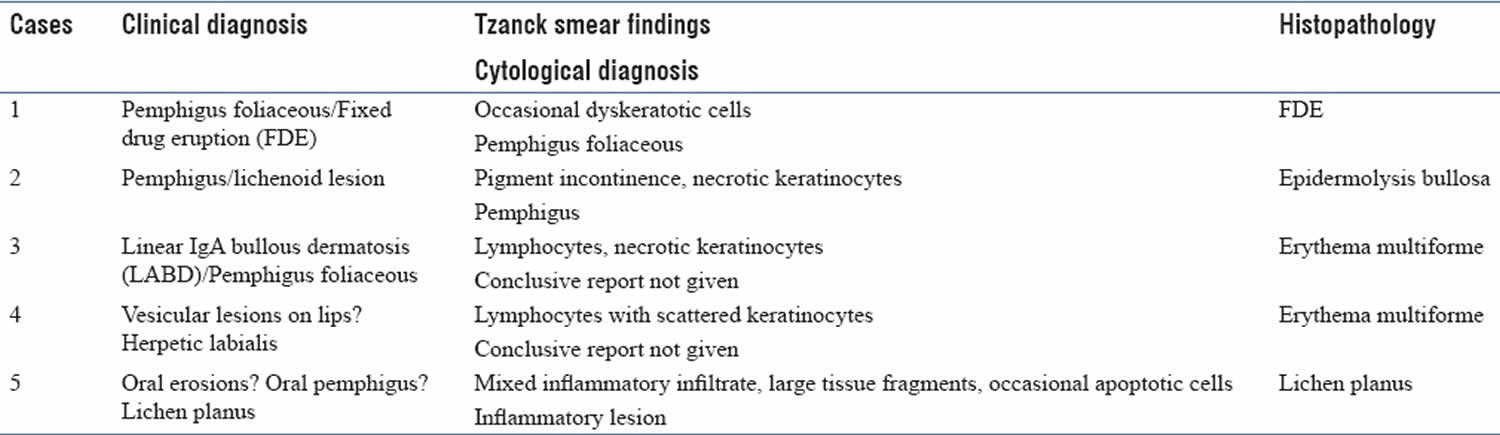
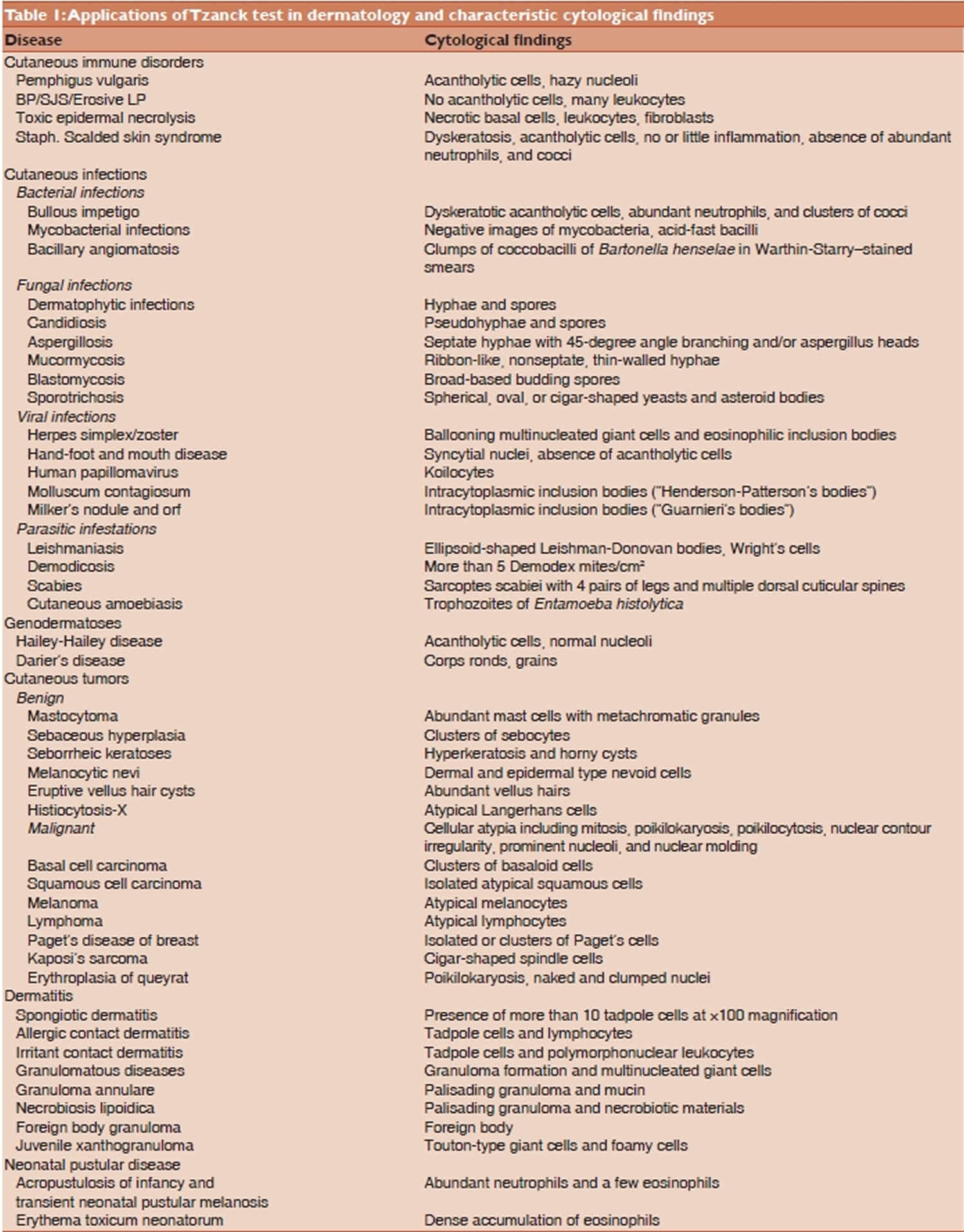
With time Tzanck test evolved and Tzanck smear findings for several other dermatological conditions like immunobullous disorders, genodermatosis, cutaneous infections, and cutaneous tumors have also been described 3. Tzanck test offers the advantage of being a simple, fast, and inexpensive diagnostic test but it requires certain amount of skill and experience for accurate interpretation 4. The technique of this test is simple that can be performed with minimal patient discomfort or cost. It provides a helpful aid for corroboration or exclusion of a clinically suspected diagnosis. A positive Tzanck smear result can lead to rapid confirmation of the diagnosis of herpetic infection, even when viral culture fails. Presence of acantholytic cells or typical Tzanck-like cells in Tzanck smears can suggest a diagnosis of pemphigus group of diseases. Skin is the largest desquamating organ and though exfoliative cytology is routinely used for diagnosis in other medical and surgical specialties, but studies on cutaneous cytology remain limited. Certain studies have been published in Western literature regarding the accuracy and diagnostic reliability of Tzanck smear 5.
The Tzanck test is not often performed, due to the development of histology, virological culture, polymerase chain reaction (PCR) and electron microscopy 6.
Figure 1. Tzanck smear test pitfalls
[Source 7 ]Advantages and disadvantages of Tzanck smear test
Initial results from a Tzanck smear should normally be confirmed by other techniques, such as biopsy or PCR.
Advantages
Tzanck smear has the following benefits:
- It is inexpensive
- It results in minimal discomfort to patients
- It is quick: useful for initial evaluation, or when rapid diagnosis required or in recurrences of disease. Faster diagnosis leads to early initiation of treatment.
Disadvantages
Tzanck smear requires expertise 4:
- In preparing the slide
- In interpreting cytology
False negatives may occur in early or late disease.
Tzanck smear procedure
- Select a fresh blister on the patient.
- Using a blunt scalpel blade, gently deroof the lesion
- Scrape the base of the lesion
- Smear the tissue onto a clean microscope slide
- Allow it to dry in the air
- Fix the specimen with preservative
In the laboratory
The slide is stained. The choice of stain depends on the sample and diagnostic possibilities.
Giemsa stain
Giemsa stain is poured over the slide. After 15 minutes, the slide is washed with sterile water.
- Cell cytoplasm stains blue
- Nuclei stain purple/red/pinkish
Toluidine blue
Toluidine blue is more rapid, as it only requires staining for 60 seconds 8.
Tzanck smear interpretation
Characteristic cytological findings of Tzanck smears follow 9.
[Source 9 ]Cutaneous infections
- Bacterial infections
- Bullous impetigo: dyskeratosis, acantholytic cells, clusters of cocci, abundant neutrophils
- Staphylococcal scalded skin syndrome: dyskeratosis, acantholytic cells, no or little inflammation, cocci, absence of abundant neutrophils
- Viral infections
- Herpes simplex and herpes zoster: Ballooning multinucleated giant cells and eosinophilic inclusion bodies
- Viral warts: koilocytes
- Molluscum contagiosum: intracytoplasmic inclusion bodies (“Henderson-Patterson’s bodies”)
- Hand foot and mouth disease: syncytial nuclei, absence of acantholytic cells
- Fungal infections
- Candidiasis: pseudohyphae and spores
- Histoplasmosis
- Cryptococcosis
- Sporotrichosis: spherical, oval or cigar-shaped yeasts and asteroid bodies
- Parasites
- Scabies: Sarcoptes scabiei (4 pairs of legs and multiple dorsal cuticular spines)
- Leishmaniasis: ellipsoid-shaped Leishman-Donovan bodies, Wright’s cells
Blistering diseases
- Pustular disease of the newborn: exclude infection, neutrophils observed in toxic erythema of the newborn
- Pemphigus vulgaris: acantholytic cells
- Stevens- Johnson syndrome / toxic epidermal necrolysis (necrotic basal cells, leukocytes, fibroblasts
Cutaneous neoplasms
- Melanoma: atypical melanocytes
- Basal cell carcinoma: clusters of basaloid cells.
- Seborrheic keratosis: hyperkeratosis, horny cysts
The Tzanck smear test was found to have similar diagnostic accuracy to dermatoscopy in pigmented skin lesions 10.
Inflammatory skin diseases
- Allergic contact dermatitis: tadpole cells, lymphoctyes
- Irritant contact dermatitis: tadpole cells, polymorphonuclear leukocytes
- Necrobiosis lipoidica: palisading granuloma, necrobiotic material
- Foreign body granuloma: foreign body.
- Tzanck A. Le cytodiagnostic immediate en dermatology. Ann Dermatol Syphiligr 1947;7:68.[↩]
- Schneider WH (2010). “Arnault Tzanck, MD (1886-1954)”. Transfus Med Rev. 24 (2): 147–50. doi:10.1016/j.tmrv.2009.11.006[↩]
- Gupta LK, Singhi MK. Tzanck smear: A useful diagnostic tool. Indian J Dermatol Venereol Leprol 2005;71:295-9.[↩]
- Grossman MC, Silvers DN. The Tzanck smear: Can dermatologists accurately interpret it? J Am Acad Dermatol 1992;27:403-5.[↩][↩]
- Eryılmaz A, Durdu M, Baba M, Yıldırım FE. Diagnostic reliability of the Tzanck smear in dermatologic diseases. Int J Dermatol 2014;53:178-86.[↩]
- Weller, Richard; Hunter, Hamish; Mann, Margaret W. Clinical Dermatology.[Internet] 5th Ed. Wiley, 11 January 2014 p39[↩]
- Panwar H, Joshi D, Goel G, Asati D, Majumdar K, Kapoor N. Diagnostic utility and pitfalls of Tzanck smear cytology in diagnosis of various cutaneous lesions. J Cytol 2017;34:179-82 http://www.jcytol.org/text.asp?2017/34/4/179/216133[↩]
- Kelly B, Shimoni T Reintroducing the Tzanck Smear, Am J Clin Dermatology 2009; 10 (3): 141-152.[↩]
- Dey VK, Thawani M, Dubey N. Accuracy and reliability of Tzanck test compared to histopathology for diagnosis of basal cell carcinoma. Indian J Dermatopathol Diagn Dermatol 2015;2:8-13 http://www.ijdpdd.com/temp/IndianJDermatopatholDiagnDermatol218-4298559_115625.pdf[↩][↩]
- Durdu M, Baba M, Seçkin D. Dermatoscopy versus Tzanck smear test: a comparison of the value of two tests in the diagnosis of pigmented skin lesions. J Am Acad Dermatol. 2011 Nov;65(5):972-82. doi: 10.1016/j.jaad.2010.08.019[↩]