What is vaginismus
Vaginismus is defined as recurrent or persistent involuntary spasm of the muscles of the outer third of the vagina, which interferes with sexual intercourse and causes distress and interpersonal difficulty 1, 2. Vaginismus causes the muscles around your vagina to tighten involuntarily. This makes your vagina very narrow and can prevent sexual activity and medical exams 3. Vaginismus is a subset of the penetration disorder or genito-pelvic pain and is currently defined as a penetration disorder in which any form of vaginal penetration such as tampons, digit, vaginal dilators, gynecologic examinations, and intercourse is often painful or impossible 2. The Diagnostic and Statistical Manual of Mental Disorders, 5th ed., (DSM-5) now addresses painful intercourse (dyspareunia – defined as persistent or recurrent genital pain that occurs just before, during or after sex) and vaginismus as one entity, characterized by pain, anxiety, problems with penetration, or a combination of these, rather than as separate conditions 4, 5. Vaginismus is thought to be one of the most common female psychosexual dysfunctions 6. Based on data that spasm of the muscles is not always present in vaginismus 7, Basson et al 8 proposed an alternative definition of persistent or recurrent difficulties in vaginal entry of a penis, finger, or other object despite the desire to do so.
Vaginismus has been associated with a high risk of disruption of marital relationships, anxiety, depression and low self esteem 6.
Vaginismus is a psychologic disorder manifested by fear and anxiety to penetration 9 and a physical disorder as noted by vaginal spasm 10 and is distinct from other sexual pain disorders such as vulvodynia (pain disorder of the vulva – the outside area of a woman’s genitals) or vestibulodynia (also known as vulvar vestibulitis syndrome, which causes pain only when pressure is applied to the area surrounding the entrance to your vagina [the vestibule, which is the tissue surrounding the vaginal opening]) 11. The diagnosis of vaginismus is made by history 11.
Vaginismus can occur whether you have had sex or not. Vaginismus usually occurs when the genital area is touched. This can be before sexual intercourse, before attempting to insert a tampon, or during a gynecological examination, for example.
Vaginismus doesn’t necessarily affect your ability to get aroused and enjoy other types of sexual contact. Many women with vaginismus can have orgasms when the clitoris is stimulated.
Vaginismus is an uncommon condition. Vaginismus seems to be quite uncommon when looking at its prevalence in the general population. However, because of the shame and secrecy associated with the condition it may be underreported and on the basis of clinic samples, it would appear that vaginismus is not that uncommon after all. Vaginismus is also believed to be a leading cause of the nonconsummation of marriage 12.
In the general population, the prevalence of vaginismus is 1–6%, and this ratio between 5% to 17% in sexual dysfunction clinics 13. A study of 301 randomly selected women in Ghana found that 205 (68.1%) reported symptoms of vaginismus 14. Among Italian women phoning a helpline for sexual concerns 9% were enquiring about vaginismus 15. A study of women attending a family planning clinic in Iran found that 12% of women suffered vaginismus at least 50% of the time with 4% always suffering vaginismus 16. A study of 54 women attending a psychiatric outpatient department in Turkey found that 41 (75.9%) reported vaginismus, of which 36 reported a lifelong problem 17. A case‐control study in Mexico found that 35 women (9.1%) had vaginismus which met the DSM‐4‐TR criteria 18. A survey of 49 gynaecologists in Holland found that vaginismus accounted for 4.2% of all sexual problems or concerns seen over a one‐week period 19. Studies of referrals to sexual dysfunction clinics in the UK and the USA indicate a prevalence rate of between 5% and 17% of female patients 20, 21, 22. The lowest estimate (5%) comes from Renshaw 21 who used the most stringent criteria and excluded patients who had vaginismus together with another sexual dysfunction. Is important to mention that the variety in the figures for the prevalence of vaginismus is possibly due to the unclear and differing definitions used in the studies.
There are several reasons why someone may experience vaginismus. These include physical and psychological factors, like:
- childbirth
- medical conditions like urinary tract infections (UTIs), yeast infections (thrush), chronic pain syndromes
- rape, sexual abuse or assault in the past 23
- a painful examination in the past
- unpleasant sexual intercourse
- fear of getting pregnant
- fear the vagina may be too small for any penetration
Other things that can cause women pain during sex include:
- vulvodynia
- thrush
- sexually transmitted infections (STIs)
- menopause
- a bad reaction to condoms, soap or shampoo
- pelvic inflammatory disease
- endometriosis
As with other sexual dysfunctions, vaginismus can lead to marital and interpersonal problems 24 and it is likely to result in infertility 6.
The main vaginismus symptoms are:
- Difficult or painful vaginal penetration during sex. Vaginal penetration may not be possible.
- Vaginal pain during sexual intercourse or a pelvic exam.
Symptoms of vaginismus vary according to the severity of vaginismus. Symptoms include fear, anxiety, and pain of vaginal penetration; inability to use a tampon (often noted at a young age); inability to remove a tampon that gets “stuck” (the proximal portion of the tampon swells with blood and cannot be extracted through the area of opening of the vagina spasm, at times necessitating removal under anesthesia); severe pain with penetration; complaints that attempted intercourse is like “hitting a wall”; and an inability to tolerate a gynecologic examination 25. These symptoms help differentiate vaginismus from vulvodynia and provoked vestibulodynia and are suggestive of spasm at the level of the introitus (opening of the vagina) 26.
The diagnosis of vaginismus is made by history 26. Women who cannot tolerate a gynecologic examination might have an examination under anesthesia during which any vaginal spasm disappears 25. Then, the patient is told that the examination was “normal.”
A health care team made up of a gynecologist, physical therapist, and sexual counselor can help with vaginismus treatment. Treatment of vaginismus depends on what is causing it. Vaginismus treatments include the widespread use of vaginal dilators, physical therapy with or without biofeedback, biofeedback, sex therapy and relationship counseling, psychotherapy, cognitive behavioral therapy, therapist-aided exposure, hypnotherapy, and lubricants 26. Sex therapy may involve relaxation techniques and gradually inserting a dilator or finger into the vagina (this may be called systematic desensitisation) 6.
See a doctor or go to a sexual health clinic if:
- you find it hard inserting a tampon into your vagina
- you struggle with vaginal penetration during sex
- you feel burning or stinging pain during sex
These are common signs of vaginismus.
Types of vaginismus
There are 2 types of vaginismus:
- Primary Vaginismus occurs where a woman has never, at any time, been able to have pain-free sexual intercourse.
- Secondary Vaginismus occurs when a woman develops vaginismus after having been able to engage in pleasurable pain free intercourse previously; this is usually due to trauma or surgery 27.
Vaginismus grades
Vaginismus was divided into 4 grades by Lamont based on the gynecological examination and the patient’s history (see Table 1) 28. The most severe vaginismus, grade 5, was defined by Pacik 29 as the form in which bodily reactions such as tremors, hyperventilation, palpitations, crying attacks, fainting spells, nausea, vomiting, running away from the table, attacking a doctor due to intense fear experienced during gynecological examination.
Table 1. Vaginismus Grade – Lamont Classification
| Grade 1 | It is the mildest form. These patients can control the contraction of their vaginal muscles with the suggestions given during the examination. |
| Grade 2 | Despite the suggestions given to the patient, they continue to contract the pelvic floor muscles throughout the examination. |
| Grade 3 | Throughout the examination, the patient raises or pulls her hip to the side, thus trying to prevent the gynecological examination. |
| Grade 4 | During the examination, the patient lifts her hips, pulls herself back, closes her legs, and thus prevents the examination. |
Vaginismus causes
Vaginismus is a sexual problem. Vaginismus has several possible causes, including:
- Past sexual trauma or abuse
- Mental health factors
- A response that develops due to physical pain
- Intercourse
- Fear that your vagina is too small
- A bad first sexual experience
- An unpleasant medical examination
- A belief that sex is shameful or wrong
- A painful medical condition, like thrush
Sometimes no cause can be found.
Classical psychoanalytic theory conceptualized vaginismus as a conversion disorder caused by unresolved psychosexual conflicts in early childhood 30. Vaginismic women have been characterized as fixated or regressed to the pre-oedipal or oedipal stages 31. Vaginismus is believed to be a psycho-physiologic disorder due to fear from actual or imagined negative experiences with penetration and/or organic pathology. Women with vaginismus have also been noted to have a lack of sex education 31.
Contributing factors of vaginismus
Vaginismus is due to involuntary tightening of the muscles in the vagina, these women have no control over it and also do not realise that this is happening. Therefore, for most women, vaginismus comes completely unexpected. It is like an automatic reflex, similar to the fact that when blowing into someone’s eyes, it causes the eyelids to shut.
All the muscles in the human body learn progressively how to behave appropriately. For example, when babies learn to walk it requires attention focus and effort, however slowly it becomes an automatic response, which does not require any conscious focus. Similarly, the muscles in the vagina of a woman with Vaginismus have unconsciously learned an automatic response to penetration, which is to spasm. So these muscles have, for some reason, developed a memory that penetration is not desirable and should not be allowed.
It is important to remember that vaginismus is not due to a physical abnormality of the genitals. Woman with vaginismus have normal vaginas and they are not too small to fit a penis.
Generally woman with vaginismus seem to have some unhealthy sexual messages that result in the reflex of these muscles. These messages can be conscious or unconscious.
Potential contributing factors are:
- Fear of penetration, which can rise to levels of a phobia
- Fear of pregnancy
- Fear of pain
- Lack of sex education
- Past sexual abuse
- Past sexual trauma
- Negative sexual attitudes
- Parental fears
- High anxiety
- Religious background
- Violence
- Abusive partner
- Difficulty to trust
- Fear of commitment
Vaginismus can co-exist with various medical conditions. Vaginismus can also continue to be present even after a medical condition has been treated. It is important to rule out any of these medical conditions.
Some of these medical conditions or additional causes of sexual pain, dyspareunia, are:
- Ovarian Cysts
- Urinary Tract Infection (UTI)/Interstitial Cystitis
- Vulvodynia
- Pelvic Inflammatory Disease
- Genital/Pelvic Tumors
- Vaginal Atrophy
- Vaginal Dryness/ Inadequate Lubrication
- Childbirth trauma
- Vulvar Cancer
- Vaginal Infections
- Sexually transmitted infections (STIs)
- Skin conditions, such as Eczema/Psoriasis
Negative sexual attitudes and lack of sexual education
The associations between negative sexual attitudes, sexual ignorance and vaginismus have been frequently mentioned in the vaginismus literature 32, 33, 34. Ellison claimed that vaginismus primarily resulted from: a lack of sexual knowledge and the presence of sexual guilt both leading to a fear of engaging in intercourse 12. These are consistent with Silverstein 33, Ward et al. 35 and Basson’s conclusion that women suffering from vaginismus hold negative views about sexuality in general and about sex before marriage 36. However, all these studies suffer from a number of important methodological limitations such as small sample sizes (n = 22–89), lack of appropriate statistical analyses and control groups, as well as absence of standardized measurement instruments and a standardized protocol to diagnose vaginismus 32. There are only two causal studies of vaginismus that have included a standard statistical analysis or a control group 37, 38 and only one that used a standardized measurement instrument 39; their results do not support the notions that women with vaginismus hold negative sexual attitudes and/or have lower levels of sexual knowledge and education 32.
Relationship factors
Vaginismus has frequently been reported to result from a dysfunctional couple relationship 40, 39. The available empirical evidence is controversial. For example, Tugrul and Kabakçi’s (n = 40) uncontrolled study demonstrated that 85% of vaginismic women who applied for the treatment of vaginismus and 90% of their husbands evaluated their marriages as satisfactory 41. Hawton and Catalan (n = 30) found that couples suffering from vaginismus have a significantly better relationship and communication when compared with 76 couples presenting other types of female sexual dysfunctions 42. Although relationship factors have not been empirically demonstrated to play a significant role in the etiology of vaginismus, women who suffer from vaginismus do have fewer sexual relations and avoid more sexual contact when compared with healthy controls 41, 38. It remains unclear, however, whether these are causes or consequences of vaginismus 32.
Partners of women with vaginismus have been reported in clinical reports to suffer from sexual dysfunction as well as to display passive and unassertive personalities 43, 44, 45, 33.
Controlled empirical findings using standardized instruments evaluating type of personalities and male sexual dysfunction, however, have not supported this view 46, 47, 37. For example, when the personality characteristics of male partners of women with vaginismus are compared with controls or norms, no differences were demonstrated. Moreover, the few studies that investigated the chronology of sexual dysfunction in partners of women with vaginismus concluded that sexual dysfunction such as erectile and premature ejaculation are generally the result rather than the cause of vaginismus 48, 49, 50, 51.
Sexual and/or physical abuse
Although the experience of sexual and/or physical abuse is generally considered an important causal factor in vaginismus, the empirical evidence is less conclusive 52, 53. Five out of six studies 42, 54, 55, 53, 56 found no evidence of a higher prevalence of sexual and physical abuse. The sixth study found only weak evidence since women with vaginismus were twice as likely to report a history of childhood sexual interference (attempts at sexual abuse and sexual abuse involving touching) as compared with a ‘no pain’ group 38. Larger studies with matched control groups and well-validated definitions of abuse are required to resolve this issue 32.
Organic pathology
A number of organic pathologies (e.g., hymeneal and congenital abnormalities, infections, vestibulodynia, trauma associated with genital surgery or radiotherapy, vaginal atrophy, pelvic congestion, endometriosis, vaginal lesions and tumors, scars in the vagina from injury, childbirth or surgery, and irritation caused by douches, spermicides or latex in condoms) resulting in painful/difficult/impossible vaginal penetration have been suggested as causal factors 51, 57. There have been no controlled studies evaluating this possibility 32.
Pelvic floor dysfunction
Pelvic floor muscle dysfunction (e.g., hypertonicity and reduced muscle control) has been suggested as a predisposing factor in the development of vaginismus 58, 59. Barnes et al.’s 60 uncontrolled study (n = 5) argued that vaginismic women had difficulty evaluating vaginal muscle tone and as a result experienced problems distinguishing between a relaxed state and a spasm. It remains unclear, however, whether pelvic floor dysfunction is a predisposing factor or the defining symptom. To date, no controlled longitudinal studies have investigated the role of pelvic floor muscle dysfunction in the cause of vaginismus 32.
Vaginismus symptoms
Symptoms of vaginismus vary according to the severity of vaginismus 61. Symptoms include fear, anxiety, and pain of vaginal penetration; inability to use a tampon (often noted at a young age); inability to remove a tampon that gets “stuck” (the proximal portion of the tampon swells with blood and cannot be extracted through the area of introital spasm, at times necessitating removal under anesthesia); severe pain with penetration; complaints that attempted intercourse is like “hitting a wall”; and an inability to tolerate a gynecologic examination. These symptoms help differentiate vaginismus from vulvodynia and provoked vestibulodynia and are suggestive of spasm at the level of the introitus 11.
The main vaginismus symptoms are:
- Difficult or painful vaginal penetration during sex. Vaginal penetration may not be possible.
- Vaginal pain during sexual intercourse or a pelvic exam.
Women with vaginismus often become anxious about sexual intercourse. This does not mean they cannot become sexually aroused. Many women with this problem can have orgasms when the clitoris is stimulated.
Consequences of vaginismus
Emotional hardship
Vaginimus is an extremely distressing condition. It is experienced slightly differently for each vaginismus sufferer, however common feelings may include:
- Confused
- Frustrated
- Feeling lonely/isolated
- Angry
- Sad/Depressed
- Shame/Embarrassment
- Scared to start a new relationship
- Worried about partner’s feelings/thoughts
Most women with vaginismus feel confused about what is happening to them and are not sure where to go for support. They may feel as if they are the only one suffering from vaginismus and may not understand why or what to do. When in a relationship they may feel they are a disappointment to their partner. When not in a relationship, they may feel embarrassed or scared to approach a new partner or start a new relationship and therefore it is common for them to isolate themselves.
Relationship Issues
Currently in a relationship:
There is no doubt that Vaginismus has a significant impact on sexual relationships.
Although Vaginismus is often considered a women’s problem, it is essentially a couple’s problem and it may even be a relationship deal-breaker.
It is commonly seen that couples seek therapy because vaginismus has become highly problematic or when they want to have children.
Partners of women with vaginismus
Partners of women with vaginismis may feel confused as to what is happening exactly and may not understand why sexual intercourse is being avoided.
Partners may:
- Feel concerned about their partner’s interest in them/physical attraction to them
- Be worried about doing something wrong sexually and not being able to get their partner aroused enough to enjoy sexual pleasure
- Be worried about hurting their partner
- Are distressed about their partner’s wellbeing
- Feel frustrated about not being able to be intimate with their partner
- Be confused about where to go for support
Currently NOT in a Relationship
When not in a relationship, vaginismus may prevent a woman from approaching new partners or starting a new relationship. They may feel ashamed and embarrassed and therefore isolate themselves.
It is important to remember that vaginismus can be worked on without having a partner. This may increase your confidence and your self-esteem to feel empowered to enter in a new relationship or to start meeting people again.
Vaginismus diagnosis
You can ask to be seen by a female doctor and you can bring someone you trust along for support. Your doctor will ask you about your symptoms and may ask to examine your vagina. A pelvic exam can confirm the diagnosis. A medical history and complete physical exam are needed to look for other causes of pain with sexual intercourse (dyspareunia).
The examination is usually very quick. Your doctor will take a quick look to rule out other conditions, like an infection.
It’s unlikely they’ll need to perform an internal examination of your vagina.
If your doctor thinks you have vaginismus, you may be referred to a specialist, such as a sex therapist.
Vaginismus is diagnosed by experiencing one or more of the specified following criteria continuously and/or repeatedly for at least 6 months 62:
- Significant difficulty during vaginal intercourse and/or penetration,
- Prominent vulvovaginal or pelvic pain during vaginal intercourse and/or penetration,
- Prominent fear or anxiety about vulvovaginal or pelvic pain during vaginal penetration,
- Prominent contraction and/or stretching of the pelvic muscles during vaginal penetration attempt.
Vaginismus treatment
A health care team made up of a gynecologist, physical therapist, sex therapist and sexual counselor can help with treatment.
Vaginismus does not get better on its own. It requires some commitment from you.
Overall the management of vaginismus involves having the woman learn to control her pelvic floor muscles.
Treatment usually focuses on:
- managing your feelings around penetration
- exercises to gradually get you used to penetration
Treatment involves a combination of physical therapy, education, counseling, and exercises such as pelvic floor muscle contraction and relaxation (Kegel exercises). It has been recognized that most women or couples dealing with vaginismus will benefit from counseling.
Treatment is initially done under the guidance of specialized therapists. You’ll then usually be expected to practise some of the exercises at home.
Table 2. Vaginismus treatment
| Possible treatments | Details |
|---|---|
| Psychosexual therapy | a type of talking therapy that aims to help you understand and change your feelings about your body and sex |
| Relaxation techniques | mindfulness, breathing and gentle touching exercises to help you learn to relax the vaginal muscles |
| Pelvic floor exercises | squeezing and releasing exercises to gain control of the vaginal muscles |
| Sensate focus | exercises to help with your relaxation during sex and increase your sex drive (libido) |
| Vaginal trainers | smooth tampon-shaped objects in different sizes to help you gradually get used to having something inserted into your vagina |
Vaginal dilation exercises using plastic dilators are recommended. This method helps to make the person less sensitive to vaginal penetration. These exercises should be done under the direction of a sex therapist, physical therapist, or other health care provider. Therapy should involve the partner and can slowly lead to more intimate contact. Intercourse may ultimately be possible.
Treatment is usually effective and you may see progress in a matter of weeks.
You will get information from your provider. Topics may include:
- Sexual anatomy
- Sexual response cycle
- Common myths about sex
Vaginismus self care
There are a number of self care techniques that can help treat vaginismus.
Get to know your body. Have some time to yourself to explore your body and what feels good for you. Make sure you are relaxed, and start feeling yourself around the genital area.
Get used to what it feels like in and around the outer part of your vagina before trying to penetrate yourself. Once you are comfortable and relaxed with that, try inserting your finger gently inside your vagina. It may take days or weeks to get to a stage where you feel comfortable enough to do this. Once you can do this, feel around inside your vagina with your finger, pushing further in very gently.
You may want to try inserting a lubricated tampon instead. Use the same method, making sure you’re calm and relaxed before inserting anything.
If you have a sexual partner, you may want to ask them to touch your genitals gently, to try and get used to them being around your vagina. Again, this will probably take time before you feel comfortable enough to be penetrated with a finger.
When you reach a stage where you want to try sexual intercourse, take things slowly and don’t rush anything.
If these methods do not help, contact your doctor who may be able to refer you to a sexual health specialist.
If you are in pain, get advice on medicines you can take.
Vaginismus physical therapy
Some women with Vaginismus may benefit from physical therapy. Physical therapy for Vaginismus does include musculoskeletal, vulvar and pelvic floor assessments via physical examinations and includes manual therapy of various hands-on techniques to treat musculoskeletal abnormalities, postural and skeletal asymmetries and soft tissue immobility. One common technique used is the application of trigger point massage in the pelvic area and transvaginal.
Vaginismus exercises
Kegel exercises also called pelvic floor muscle training exercises, are exercises to make your pelvic floor muscles stronger. The pelvic floor are the muscles that hold up your bladder, rectum and uterus (womb) and help keep them from prolapsing (a condition where organs fall down or slip out of place), resulting in urinary or fecal leakage (incontinence).
Kegel exercises (pelvic floor muscle training exercises) can help both men and women who have problems with urine leakage or bowel control. Kegel exercises (pelvic floor muscle training exercises) can also make sex better.
Building up your pelvic muscles with Kegel exercises (pelvic floor muscle training exercises) can help with your bladder and bowel control. Kegel exercises strengthen the pelvic muscles — the muscles under the uterus, bladder, and bowel (large intestine) and don’t require any equipment. Once you learn how to do “Kegel exercises” you can Kegel anywhere. You can do Kegel exercises while lying down, sitting at a desk, or standing up.
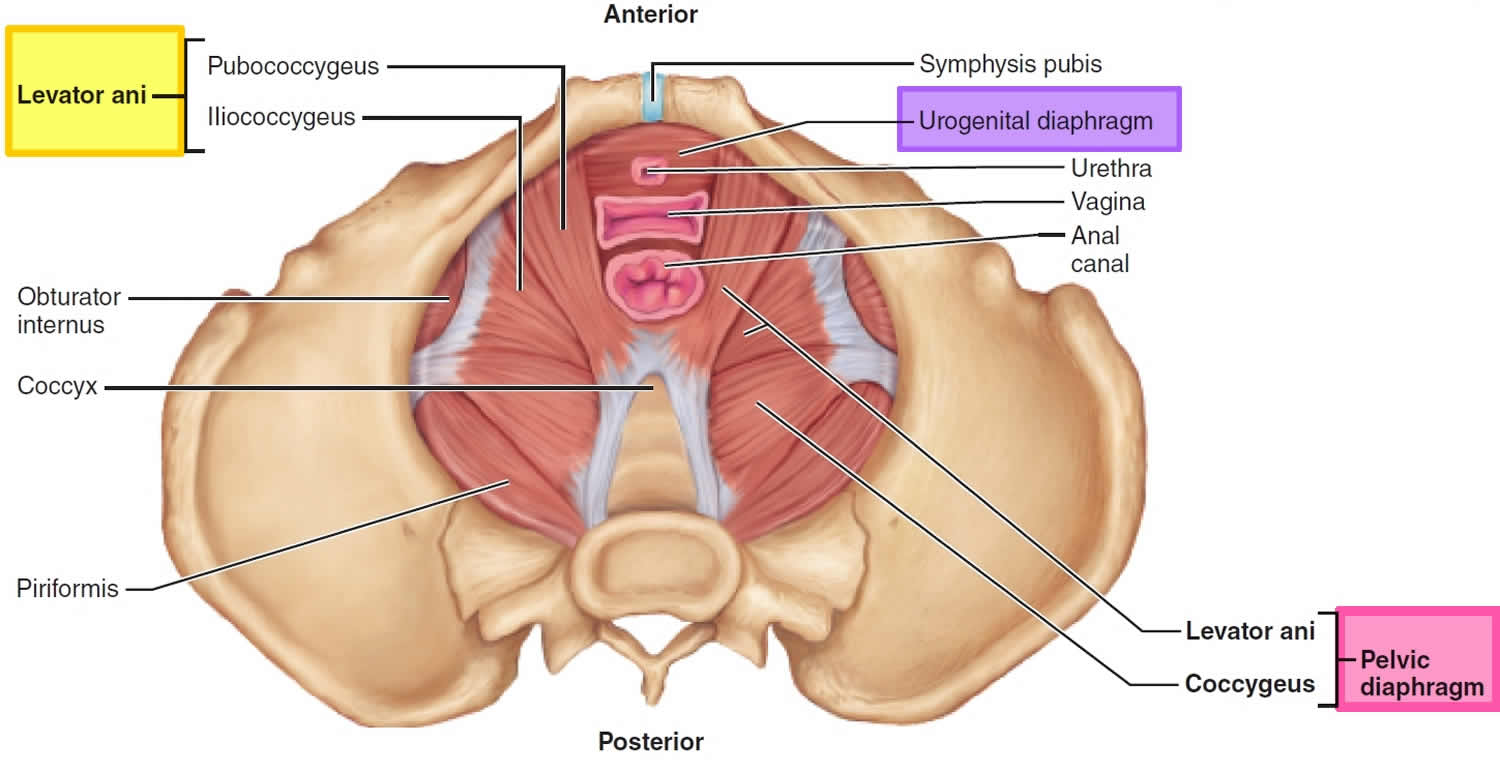
The trick is finding the right muscles to squeeze (see Figures 1 and 2 for reference). Your doctor or nurse can help make sure you are squeezing the right muscles. Your doctor may refer you to a specially trained physical therapist who will teach you to find and strengthen the sphincter muscles. Learning when to squeeze these muscles can also help stop the bladder spasms that cause urge incontinence. After about 6 to 8 weeks, you should notice that you have fewer leaks and more bladder control.
To do Kegel exercises, you just squeeze your pelvic floor muscles. The part of your body including your hip bones is the pelvic area. At the bottom of the pelvis, several layers of muscle stretch between your legs. The muscles attach to the front, back, and sides of the pelvic bone (see Figures 1 and 2).
The pelvic floor has several functions:
- it supports your pelvic and abdominal organs, especially when you are standing or straining;
- it helps your urethra stay closed when you cough, sneeze or strain;
- it controls leakage of wind or motions from your lower bowel;
- it helps to heighten sexual awareness by tightening during intercourse.
A weak pelvic floor gives you less control so that you may have urinary stress incontinence (urine leakage) or fecal incontinence (fecal leakage) when you exercise, lift, cough, laugh hard or sneeze.
Often women leak urine when they are pregnant or after they have given birth.
Female athletes of all ages sometimes have urine leakage during strenuous sports activities.
A man’s pelvic floor muscles support the bladder and bowel and affect sexual function. Kegel exercises can help strengthen these muscles.
The pelvic floor muscles can be weakened by:
- pregnancy and childbirth (in women);
- operations on other organs within the pelvis (e.g. the bowel);
- damage to the nerves of your pelvic floor muscles (by disease, injury, surgery or radiotherapy);
- repeated straining to empty your bowels, usually due to constipation;
- a chronic cough such as a smoker’s cough, chronic bronchitis or asthma;
- being overweight;
- lack of general fitness;
- ageing;
- lack of exercise and the menopause.
Muscles of the pelvic floor
The pelvic floor also called the pelvic diaphragm (Figure 1), is a complex layer of muscles and ligaments which stretches like a hammock from the pubic bone at the front of your pelvis to the coccyx at the bottom your spine.
The pelvic floor is a sheet consisting of two muscles, the levator ani and the small coccygeus (ischiococcygeus). The pelvic floor supports the pelvic organs, seals the inferior opening of the bony pelvis, and lifts superiorly to help release feces during defecation. The pelvic floor is pierced by the rectum and urethra (the tube for urine) and (in females) by the vagina.
The muscles of the pelvic floor are the levator ani and ischiococcygeus. Along with the fascia covering their internal and external surfaces, these muscles are referred to as the pelvic diaphragm, which stretches from the pubis anteriorly to the coccyx posteriorly, and from one lateral wall of the pelvis to the other. This arrangement gives the pelvic diaphragm the appearance of a funnel suspended from its attachments. The pelvic diaphragm separates the pelvic cavity above from the perineum below. The anal canal and urethra pierce the pelvic diaphragm in both sexes, and the vagina also goes through it in females. The three components of the levator ani muscle are the pubococcygeus, puborectalis, and iliococcygeus. Figure 1 shows these muscles in the female and Figure 2 illustrates them in the male. The levator ani is the largest and most important muscle of the pelvic floor. It supports the pelvic viscera and resists the inferior thrust that accompanies increases in intraabdominal pressure during functions such as forced exhalation, coughing, vomiting, urination, and defecation. The muscle also functions as a sphincter at the anorectal junction, urethra, and vagina. In addition to assisting the levator ani, the ischiococcygeus pulls the coccyx anteriorly after it has been pushed posteriorly during defecation or childbirth.
The body region inferior to the pelvic floor is the perineum. In the anterior half of the perineum is a triangular sheet of muscle called the urogenital diaphragm. It contains the external urethral sphincter muscle, which surrounds the urethra. You use this muscle voluntarily to prevent urination. Just inferior to the urogenital diaphragm is the superficial perineal space, which contains muscles (bulbospongiosus, ischiocavernosus) that help maintain erection of the penis and clitoris. In the posterior half of the perineum, circling the anus, lies the external anal sphincter. This muscle is used voluntarily to prevent defecation. Just anterior to this sphincter, at the exact midpoint of the perineum, is the central tendon. Many perineal muscles insert on this strong tendon and, in so doing, are able to support the heavy organs in the pelvis.
Figure 1. Pelvic floor female
How do you do Kegel exercises
To do Kegel exercises, you just squeeze your pelvic floor muscles. The part of your body including your hip bones is the pelvic area. At the bottom of the pelvis, several layers of muscle stretch between your legs. The muscles attach to the front, back, and sides of the pelvic bone. Kegel exercises are designed to make your pelvic floor muscles stronger. These are the muscles that hold up your bladder and help keep it from leaking.
A pelvic floor muscle training exercise is like pretending that you have to urinate, and then holding it. You relax and tighten the muscles that control urine flow. It is important to find the right muscles to tighten.
Find the right muscles. Try one of the following ways to find the right muscles to squeeze.
- Imagine that you are trying to stop passing gas. Squeeze the muscles you would use. If you sense a “pulling” feeling, you are squeezing the right muscles for pelvic exercises.
- Imagine that you are sitting on a marble and want to pick up the marble with your vagina. Imagine “sucking” the marble into your vagina.
- Lie down and put your finger inside your vagina. Squeeze as if you were trying to stop urine from coming out. If you feel tightness on your finger, you are squeezing the right pelvic muscles.
The next time you have to urinate, start to go and then stop. Feel the muscles in your vagina, bladder, or anus get tight and move up. These are the pelvic floor muscles. If you feel them tighten, you have done the exercise right.
If you are still not sure whether you are tightening the right muscles, keep in mind that all of the muscles of the pelvic floor relax and contract at the same time. Because these muscles control the bladder, rectum, and vagina, the following tips may help:
- Women: Insert a finger into your vagina. Tighten the muscles as if you are holding in your urine, then let go. You should feel the muscles tighten and move up and down.
It is very important that you keep the following muscles relaxed while doing pelvic floor muscle training exercises:
- Abdominal
- Buttocks (the deeper, anal sphincter muscle should contract)
- Thigh
If you’re having trouble doing Kegel exercises, don’t be embarrassed to ask for help. Your doctor or other health care provider can give you important feedback so that you learn to isolate and exercise the correct muscles.
In some cases, vaginal weighted cones or biofeedback might help. A woman can also strengthen these muscles by using a vaginal cone, which is a weighted device that is inserted into the vagina. To use a vaginal cone, you insert it into your vagina and use pelvic muscle contractions to hold it in place during your daily activities. During a biofeedback session, your doctor or other health care provider inserts a pressure sensor into your vagina or rectum. As you relax and contract your pelvic floor muscles, a monitor will measure and display your pelvic floor activity.
If you are unsure whether you are doing the pelvic floor muscle training correctly, you can use biofeedback and electrical stimulation to help find the correct muscle group to work.
- Biofeedback is a method of positive reinforcement. Electrodes are placed on the abdomen and along the anal area. Some therapists place a sensor in the vagina in women or anus in men to monitor the contraction of pelvic floor muscles.
- A monitor will display a graph showing which muscles are contracting and which are at rest. The therapist can help find the right muscles for performing pelvic floor muscle training exercises.
Let your doctor, nurse, or therapist help you. Many people have trouble finding the right muscles. Your doctor, nurse, or therapist can check to make sure you are doing the exercises correctly. You can also exercise by using special weights or biofeedback. Ask your health care team about these exercise aids.
Don’t squeeze other muscles at the same time. Be careful not to tighten your stomach, legs, or other muscles. Squeezing the wrong muscles can put more pressure on your bladder control muscles. Just squeeze the pelvic muscle. Don’t hold your breath.
Repeat, but don’t overdo it. At first, find a quiet spot to practice—your bathroom or bedroom—so you can concentrate. Lie on the floor. Pull in the pelvic muscles and hold for a count of 3. Then relax for a count of 3. Work up to 10 to 15 repeats each time you exercise. Use the Exercise Log below to keep track of your sessions.
Do your pelvic exercises at least three times a day. Every day, use three positions: lying down, sitting, and standing. You can exercise while lying on the floor, sitting at a desk, or standing in the kitchen. Using all three positions makes the muscles strongest.
Be patient. Don’t give up. It’s just 5 minutes, three times a day. You may not feel your bladder control improve until after 3 to 6 weeks. Still, most women do notice an improvement after a few weeks.
Performing Kegel Exercises/Pelvic Floor Exercises
- Begin by emptying your bladder.
- Tighten the pelvic floor muscles and hold for a count of 10.
- Relax the muscles completely for a count of 10.
- Do 10 repetitions, 3 to 5 times a day (morning, afternoon, and night).
You can do these exercises at any time and place. Most people prefer to do the exercises while lying down or sitting in a chair. After 4 to 6 weeks, most people notice some improvement. It may take as long as 3 months to see a major change.
After a couple of weeks, you can also try doing a single pelvic floor contraction at times when you are likely to leak (for example, while getting out of a chair).
A word of caution: Some people feel that they can speed up the progress by increasing the number of repetitions and the frequency of exercises. However, over-exercising can instead cause muscle fatigue and increase urine leakage.
If you feel any discomfort in your abdomen or back while doing these exercises, you are probably doing them wrong. Breathe deeply and relax your body when you do these exercises. Make sure you are not tightening your stomach, thigh, buttock, or chest muscles.
When done the right way, pelvic floor muscle exercises have been shown to be very effective at improving urinary continence.
There are physical therapists specially trained in pelvic floor muscle training. Many people benefit from formal physical therapy.
Kegel Exercise Log
Week: ______________
My Pelvic Muscle Exercise Log
Sunday
- I exercised my pelvic muscles ____ times.
- I spent ____ minutes exercising.
- At each exercise session, I squeezed my pelvic muscles ____ times.
Monday
- I exercised my pelvic muscles ____ times.
- I spent ____ minutes exercising.
- At each exercise session, I squeezed my pelvic muscles ____ times.
Tuesday
- I exercised my pelvic muscles ____ times.
- I spent ____ minutes exercising.
- At each exercise session, I squeezed my pelvic muscles ____ times.
Wednesday
- I exercised my pelvic muscles ____ times.
- I spent ____ minutes exercising.
- At each exercise session, I squeezed my pelvic muscles ____ times.
Thursday
- I exercised my pelvic muscles ____ times.
- I spent ____ minutes exercising.
- At each exercise session, I squeezed my pelvic muscles ____ times.
Friday
- I exercised my pelvic muscles ____ times.
- I spent ____ minutes exercising.
- At each exercise session, I squeezed my pelvic muscles ____ times.
Saturday
- I exercised my pelvic muscles ____ times.
- I spent ____ minutes exercising.
- At each exercise session, I squeezed my pelvic muscles ____ times.
Use this sheet as a master for making copies that you can use to record your exercises week after week.
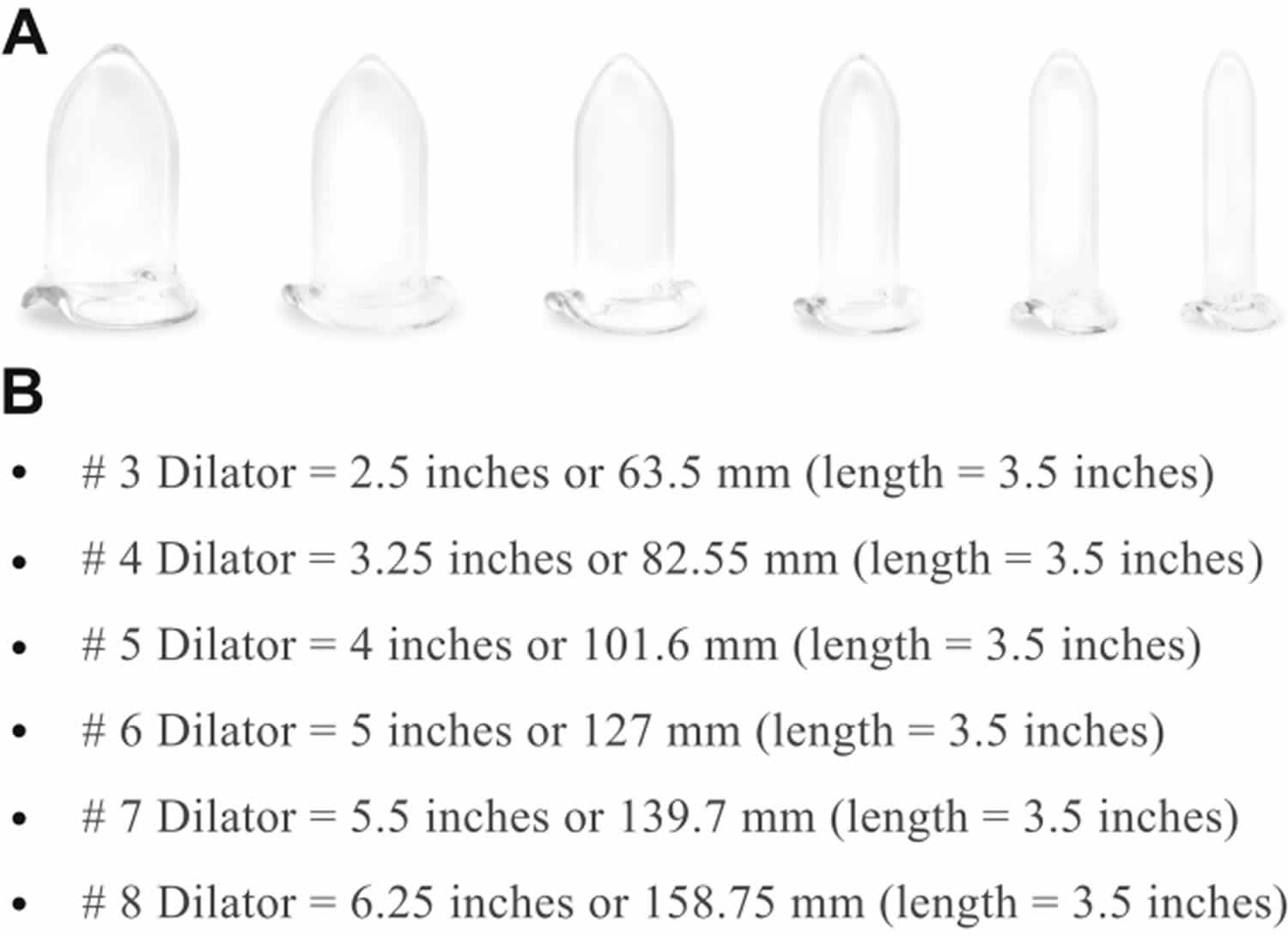
Dilation, Dilators and Home Care
Many protocols exist regarding dilation recommendations to overcome vaginismus. More than 50% of women attempted the use of dilators and were unable to progress to comfortable penetration because, too often, not enough time was spent dilating. Regardless of the type of treatment, dilation is an important part of the recovery process. Women have mentioned repeatedly that they hate to dilate and even patients who went through this rigorous program sometimes failed to dilate for long enough periods. The dilation instructions are summarized as follows.
The Procedure
The procedure involves Botox injections plus separate injections of 0.25% bupivacaine 18 mL with 1:400,000 epinephrine divided into 1-mL increments along the length of the right and left submucosal lateral vaginal walls (9 mL per side) from the level of the cervix to the introitus, to allow patients to wake up pain free with a large dilator in place. No injections were delivered anteriorly or posteriorly to help avoid urinary and rectal incontinence. Conscious sedation was needed during vaginal injections and dilation, although, rarely, women with less severe vaginismus tolerated the procedure with no sedation. The patient was progressively dilated with the #4 dilator (3-inch circumference), the #5 dilator (4-inch circumference), and then, when possible, the #6 dilator (5-inch circumference) and reassessed with digital examination. Sometimes it was physically impossible to insert the #6 dilator. Approximately 10% to 15% of women required release of a constricting hymenal ring noted to be present around the circumference of the introitus (not to be confused with an intact hymen) with a small snip or the removal of a small triangular wedge on the left and right lateral sides of the ring. This procedure results in a small amount of bleeding that can be controlled with pressure. Hymenectomy was not needed in any of the patients. The procedure was concluded with bimanual examination and reinsertion of a #5 or #6 indwelling dilator, and the patient was awakened and transported to the recovery area (Figure 2). Operative time was approximately 30 minutes.
First Month After Procedure
- Dilate 2 hours a day, 1 hour in the morning and 1 hour in the evening, or 2 hours at any one sitting. Advance to larger dilators as able until the #5 or #6 dilator becomes comfortable.
Second Month After Procedure
- Decrease dilation to 1 hour a day and advance to larger sizes.
Third Month After Procedure
- Dilate 15 to 30 minutes a day.
One Year After Procedure
Women with severe vaginismus had a higher rate of recurrence if they stopped dilating by approximately 6 months. For this reason, even 10 to 15 minutes of dilation every day or two is of value.
It is helpful for the partner to assist with dilation to help transition to intercourse physically and psychologically.
Advancing to Intercourse
Postprocedure counseling includes a discussion of the following items. Attempts at intercourse should be delayed until at least the #5 dilator can be inserted easily. It is helpful to dilate with the #5 or #6 dilator for approximately 1 hour before to attempting first-time intercourse. For partners who have larger penises, #7 (6-inch circumference) and #8 (7-inch circumference) dilators are available. During these first attempts at intercourse, patients and their partners are taught to penetrate with no more than the penile tip because women with severe vaginismus are fragile at this juncture and often have considerable fear. Men also are vulnerable in that erectile dysfunction might be noted including loss of erection and premature ejaculation. Everything possible is done to help remove the pressure of this moment. Once penile tip penetration is achieved comfortably, the couple can advance to full penetration; however, thrusting is discouraged because this can be a setback for the woman. Women with severe vaginismus might note “leg lock,” the involuntary closure of the thighs in anticipation of penetration. The “spooning position” with entry from behind has been found to be helpful in overcoming leg lock. Women are encouraged to try different positions during their dilation and attempts at coitus to find their comfort zone.
Figure 2. Vaginismus vaginal dilators
Footnote: Panel A shows Pacik borosilicate glass dilators sizes 3 to 8 (right to left). Panel B shows circumferences and lengths of Pacik borosilicate glass dilators.
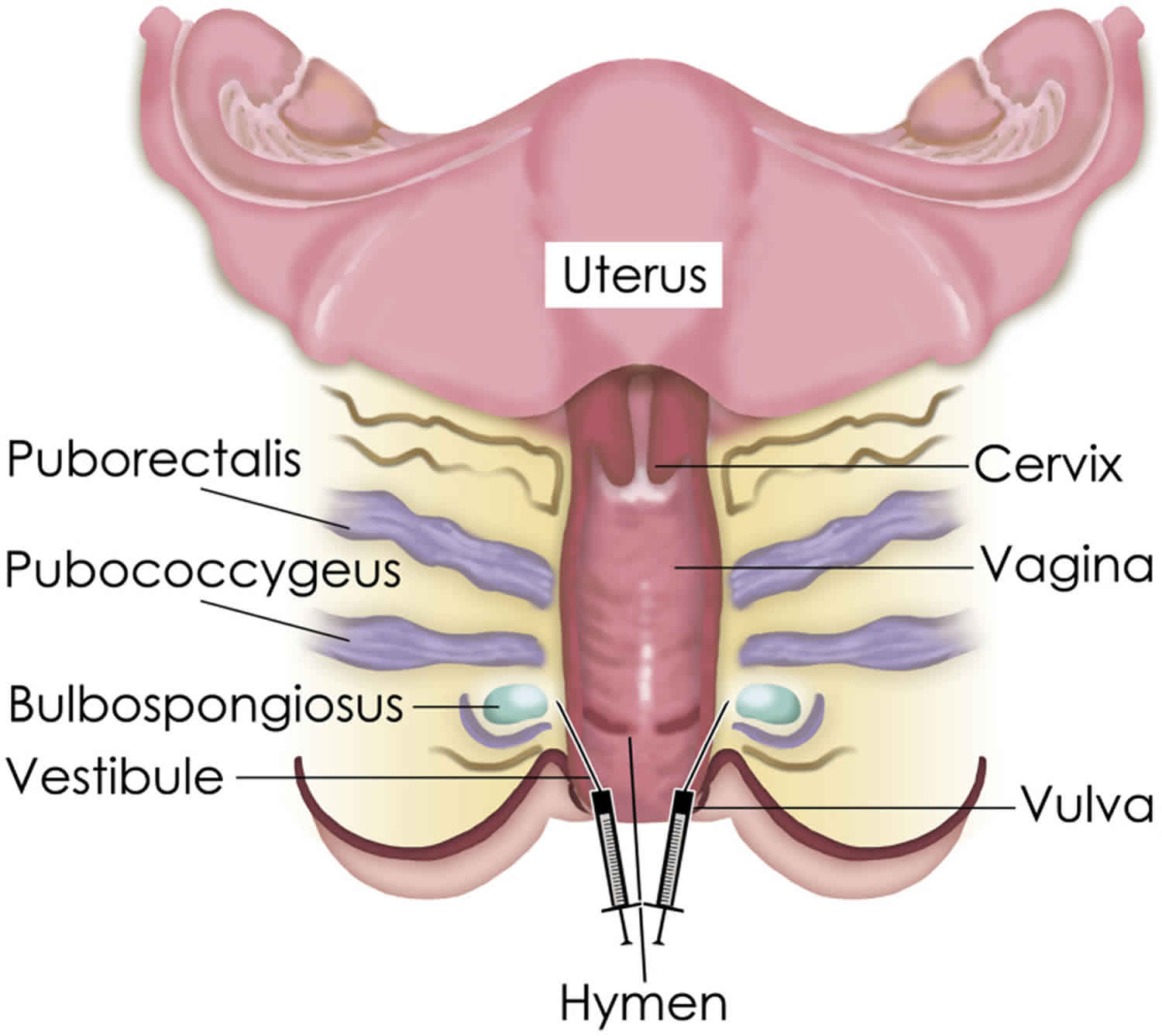
[Source 61 ]Vaginismus Botox injections therapy
The successful use of Botox (onabotulinumtoxinA) injections to treat secondary vaginismus was first described as a case report in 1997 11 and later developed by different investigators 11. Abbott et al. 63 using a placebo-controlled study of onabotulinumtoxinA showed that all eight women who had onabotulinumtoxinA 25 U injected into the bulbospongiosum achieved intercourse compared with none of the five women in the placebo group, with no recurrence or reinjection in the follow-up period of 8 to 14 months. Ghazizadeh and Nikzad 64 used Dysport (abobotulinumtoxinA) to treat 23 women with Lamont grade 3 and 4 refractory vaginismus 65 and reported a 75% success rate of pain-free intercourse in these women were followed for a mean of 12.3 months (range = 2–24)
Figure 3. Vaginismus Botox injections therapy
Footnote: Submucosal injections of Botox to the bulbospongiosum, on each side, using hymenal fragments as a landmark. The needle is bent 30° at the hub for ease of injections. Bupivacaine injections are not shown.
[Source 61 ]Vaginismus prognosis
Women who are treated by a sex therapy specialist can very often overcome this problem.
- Lahaie MA, Boyer SC, Amsel R, Khalifé S, Binik YM. Vaginismus: a review of the literature on the classification/diagnosis, etiology and treatment. Womens Health (Lond). 2010 Sep;6(5):705-19. doi: 10.2217/whe.10.46[↩]
- American Psychiatric Association . 5th ed. American Psychiatric Association; Washington, DC: 2013. Diagnostic and statistical manual of mental disorders.[↩][↩]
- Vaginismus. https://medlineplus.gov/ency/article/001487.htm[↩]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 5th ed. Arlington, Va.: American Psychiatric Association; 2013.[↩]
- Binik YM. The DSM diagnostic criteria for vaginismus. Arch Sex Behav. 2010 Apr;39(2):278-91. doi: 10.1007/s10508-009-9560-0[↩]
- Melnik T, Hawton K, McGuire H. Interventions for vaginismus. Cochrane Database Syst Rev. 2012 Dec 12;12(12):CD001760. doi: 10.1002/14651858.CD001760.pub2[↩][↩][↩][↩]
- Reissing ED, Binik YM, Khalifé S, Cohen D, Amsel R. Vaginal spasm, pain, and behavior: an empirical investigation of the diagnosis of vaginismus. Arch Sex Behav. 2004 Feb;33(1):5-17. doi: 10.1023/B:ASEB.0000007458.32852.c8[↩]
- Basson R, Althof S, Davis S, Fugl-Meyer K, Goldstein I, Leiblum S, Meston C, Rosen R, Wagner G. Summary of the recommendations on sexual dysfunctions in women. J Sex Med. 2004 Jul;1(1):24-34. doi: 10.1111/j.1743-6109.2004.10105.x[↩]
- Rosenbaum T. An integrated mindfulness-based approach to the treatment of women with sexual pain and anxiety: promoting autonomy and mind/body connection. Sex Relatsh Ther. 2013;28, 1–2[↩]
- Pacik P.T. Vaginismus: review of current concepts and treatment using Botox injections, bupivacaine injections, and progressive dilation with the patient under anesthesia. Aesthetic Plast Surg. 2011;35:1160–1164.[↩]
- Pacik P.T. Understanding and treating vaginismus: a multimodal approach. Int Urogynecol J. 2014;25:1613–1620.[↩][↩][↩][↩][↩]
- Ellison C. Psychosomatic factors in the unconsummated marriage. J Psychosom Res. 1968 Jun;12(1):61-5. doi: 10.1016/0022-3999(68)90009-3[↩][↩]
- Konkan R, Bayrak M, Gonullu GO. Sexual function and satisfaction of women with vaginismus. J Psychiatry Neurol Sci. 2012;25:305–311.[↩]
- Amidu N, Owiredu WK, Woode E, Addai-Mensah O, Quaye L, Alhassan A, Tagoe EA. Incidence of sexual dysfunction: a prospective survey in Ghanaian females. Reprod Biol Endocrinol. 2010 Sep 1;8:106. doi: 10.1186/1477-7827-8-106[↩]
- Simonelli C, Tripodi F, Cosmi V, Rossi R, Fabrizi A, Silvaggi C, Di Pomponio I. What do men and women ask a helpline on sexual concerns? Results of an Italian telephone counselling service. Int J Clin Pract. 2010 Feb;64(3):360-70. doi: 10.1111/j.1742-1241.2009.02269.x[↩]
- Shokrollahi P, Mirmohamadi M, Mehrabi F, Babaei G. Prevalence of sexual dysfunction in women seeking services at family planning centers in Tehran. J Sex Marital Ther. 1999 Jul-Sep;25(3):211-5. doi: 10.1080/00926239908403995[↩]
- Dogan S. Vaginismus and accompanying sexual dysfunctions in a Turkish clinical sample. J Sex Med. 2009 Jan;6(1):184-92. doi: 10.1111/j.1743-6109.2008.01048.x[↩]
- Bravo CS, Melendez JC, Ramirez SM, Lopez ME. Feminine and masculine sexual dysfunctions: gender comparison in a Mexico City sample [Disfunciones sexuales femininas y masculinas: Comparacion de genero en una muestra de la Ciudad de Mexico]. Salud Mental 2005;28(4):74‐80.[↩]
- Frenken J, Tol P. Sexual problems in gynaecological practice. Journal of Psychosomatics Obstetrics & Gynecology 1987;6:143‐55.[↩]
- Hirst JF, Baggaley MR, Watson JP. A four year survey of an inner city psychosexual problems clinic. Sexual & Marital Therapy 1996;11:19‐36.[↩]
- Renshaw DC. Profile of 2376 patients treated at Loyola Sex Clinic between 1972 and 1987. Sexual and Marital Therapy 1988;3:111‐7.[↩][↩]
- Catalan J, Hawton K, Day A. Couples referred to a sexual dysfunction clinic. Psychological and physical morbidity. Br J Psychiatry. 1990 Jan;156:61-7. doi: 10.1192/bjp.156.1.61[↩]
- Tetik S, Yalçınkaya Alkar Ö. Vaginismus, Dyspareunia and Abuse History: A Systematic Review and Meta-analysis. J Sex Med. 2021 Sep;18(9):1555-1570. doi: 10.1016/j.jsxm.2021.07.004[↩]
- Catalan J, Bradley M, Gallwey J, Hawton K. Sexual dysfunction and psychiatric morbidity in patients attending a clinic for sexually transmitted diseases. Br J Psychiatry. 1981 Apr;138:292-6. doi: 10.1192/bjp.138.4.292[↩]
- Pacik PT, Geletta S. Vaginismus Treatment: Clinical Trials Follow Up 241 Patients. Sex Med. 2017 Jun;5(2):e114-e123. doi: 10.1016/j.esxm.2017.02.002[↩][↩]
- Pacik PT. Understanding and treating vaginismus: a multimodal approach. Int Urogynecol J. 2014 Dec;25(12):1613-20. doi: 10.1007/s00192-014-2421-y[↩][↩][↩]
- Crowley T., Goldmeier D., Hiller J. Diagnosing and managing vaginismus. BMJ. 2009;338:b2284.[↩]
- Lamont JA. Vaginismus. Am J Obstet Gynecol. 1978 Jul 15;131(6):633-6.[↩][↩]
- Pacik PT. Vaginismus: The Lamont classification revisited. Poster presentation at the ISSWSH Annual Meeting; Scottsdale; 2011.[↩]
- Successful management of vaginismus: An eclectic approach. Indian J Psychiatry. 2011 Apr-Jun; 53(2): 154–155. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3136020/[↩]
- Does vaginismus exist? A critical review of the literature. Reissing ED, Binik YM, Khalifé S. J Nerv Ment Dis. 1999 May; 187(5):261-74.[↩][↩]
- Lahaie M-A, Boyer SC, Amsel R, Khalifé S, Binik YM. Vaginismus: A Review of the Literature on the Classification/Diagnosis, Etiology and Treatment. Women’s Health. 2010;6(5):705-719. doi:10.2217/WHE.10.46[↩][↩][↩][↩][↩][↩][↩]
- Silverstein JL. Origins of psychogenic vaginismus. Psychother Psychosom. 1989;52(4):197-204. doi: 10.1159/000288324[↩][↩][↩]
- Audibert C, Kahn-Nathan J: Le vaginisme. Contracept. Fertil. Sex 8, 257–263 (1980).[↩]
- Ward E, Ogden J: Experiencing vaginismus sufferers’ beliefs about causes and effects. Sex Marital Ther. 9, 33–45 (1994).[↩]
- Basson R: Lifelong vaginismus: a clinical study of 60 consecutive cases. J. SOGC 18, 551–561 (1996).[↩]
- Duddle M. Etiological factors in the unconsummated marriage. J Psychosom Res. 1977;21(2):157-60. doi: 10.1016/0022-3999(77)90083-6[↩][↩]
- Reissing ED, Binik YM, Khalifé S, Cohen D, Amsel R. Etiological correlates of vaginismus: sexual and physical abuse, sexual knowledge, sexual self-schema, and relationship adjustment. J Sex Marital Ther. 2003 Jan-Feb;29(1):47-59. doi: 10.1080/713847095[↩][↩][↩]
- Biswas A, Ratnam SS. Vaginismus and outcome of treatment. Ann Acad Med Singap. 1995 Sep;24(5):755-8.[↩][↩]
- Van de Wiel HB: Treatment of vaginismus: a review of concepts and treatment modalities. J. Psychosom. Obstet. Gynaecol. 11, 1–18 (1990).[↩]
- Tugrul C, Kabakçi E: Vaginismus and its correlates. Sex Marital Ther. 12(1), 23–34 (1997).[↩][↩]
- Hawton K, Catalan J: Sex therapy for vaginismus: characteristics of couples and treatment outcome. Sex Marital Ther. 5, 39–48 (1990).[↩][↩]
- Van Lankveld JJ, Brewaeys AM, Ter Kuile MM, Weijenborg PT: Difficulties in the differential diagnosis of vaginismus, dyspareunia and mixed sexual pain disorder. J. Psychosom. Obstet. Gynaecol. 16, 201–209 (1995).[↩]
- Masters WH, Johnson VE: Human Sexual Inadequacy. Little, Brown, Boston, USA (1970).[↩]
- Ellison C: Vaginismus. Med. Aspects Hum. Sex 6, 34–54 (1972).[↩]
- Engman M, Lindehammar H, Wijma B. Surface electromyography diagnostics in women with partial vaginismus with or without vulvar vestibulitis and in asymptomatic women. J Psychosom Obstet Gynaecol. 2004 Sep-Dec;25(3-4):281-94. doi: 10.1080/01674820400017921[↩]
- Kennedy P, Doherty N, Barnes J: Primary vaginismus: a psychometric study of both partners. J. Sex Marital Ther. 10, 9–22 (1995).[↩]
- Lamont J: Vaginismus: a reflex response out of control. Contemp. Rev. Obstet. Gynaecol. 3, 30–32 (1994).[↩]
- Friedman LJ: Virgin Wives: a Study of Unconsummated Marriages. Tavistock Publications, London, UK (1962).[↩]
- Barnes J. Primary vaginismus (Part 1): Social and clinical features. Ir Med J. 1986 Mar;79(3):59-62. [↩]
- Leiblum SR: Vaginismus: a most perplexing problem. In: Principles and Pactice of Sex Therapy. Leiblum SR, Rosen RC (Eds). Guilford Press, NY, USA 181–202 (2000).[↩][↩]
- Biswas A, Ratnam SS. Vaginismus and outcome of treatment. Ann Acad Med Singap. 1995 Sep;24(5):755-8. [↩]
- van Lankveld JJ, Brewaeys AM, Ter Kuile MM, Weijenborg PT. Difficulties in the differential diagnosis of vaginismus, dyspareunia and mixed sexual pain disorder. J Psychosom Obstet Gynaecol. 1995 Dec;16(4):201-9. doi: 10.3109/01674829509024470[↩][↩]
- O’Sullivan K. Observations on vaginismus in Irish women. Arch Gen Psychiatry. 1979 Jul;36(7):824-6. doi: 10.1001/archpsyc.1979.01780070102012[↩]
- Barnes J. Primary vaginismus (Part 1): Social and clinical features. Ir Med J. 1986 Mar;79(3):59-62.[↩]
- Van Lankveld JJ, ter Kuile MM, de Groot HE, Melles R, Nefs J, Zandbergen M: Cognitive–behavioral therapy for women with lifelong vaginismus: a randomized waiting-list controlled trial of efficacy. J. Consult. Psychol. 74 (1), 168–178 (2006).[↩]
- Abramov L, Wolman I, David MP. Vaginismus: an important factor in the evaluation and management of vulvar vestibulitis syndrome. Gynecol Obstet Invest. 1994;38(3):194-7. doi: 10.1159/000292478[↩]
- Meana M, Binik YM, Khalifé S, Cohen D. Dyspareunia: sexual dysfunction or pain syndrome? J Nerv Ment Dis. 1997 Sep;185(9):561-9. doi: 10.1097/00005053-199709000-00005[↩]
- Rosenbaum TY. Physiotherapy treatment of sexual pain disorders. J Sex Marital Ther. 2005 Jul-Sep;31(4):329-40. doi: 10.1080/00926230590950235[↩]
- Barnes J, Bowman EP, Cullen J. Biofeedback as an adjunct to psychotherapy in the treatment of vaginismus. Biofeedback Self Regul. 1984 Sep;9(3):281-9. doi: 10.1007/BF00998972[↩]
- Vaginismus Treatment: Clinical Trials Follow Up 241 Patients. Sex Med. 2017 Jun; 5(2): e114–e123. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5440634/[↩][↩][↩]
- American Psychiatric Association . 5th ed. American Psychiatric Press; USA: 2013. DSM-5: Diagnostic and Statistical Manual for Mental Disorders.[↩]
- Abbott J.A., Jarvis S.K., Lyons S.D. Botulinum toxin type A for chronic pain and pelvic floor spasm in women: a randomized controlled trial. Obstet Gynecol. 2006;108:915–923.[↩]
- Ghazizadeh S., Nikzad M. Botulinum toxin in the treatment of refractory vaginismus. Obstet Gynecol. 2004;104:922–925.[↩]
- Lamont J.A. Vaginismus. Am J Obstet Gynecol. 1978;131:633–636.[↩]