What is vocal cord dysfunction
Vocal cord dysfunction is also called inducible laryngeal obstruction, is an abnormal narrowing or abnormal closing of the vocal cords when you breathe in or out. Vocal cord dysfunction is also called laryngeal dysfunction, paradoxical vocal cord movement disorder or paradoxical vocal cord motion. Vocal cord dysfunction occurs in some people during high intensity exercise or exposure to certain irritants. This leaves only a small opening for air to flow through the windpipe which can feel like you can’t get enough air into your lungs. Vocal cord dysfunction can cause signs and symptoms that mimic asthma. Like asthma, vocal cord dysfunction can be triggered by breathing in lung irritants, having an upper respiratory infection or exercising. However, unlike asthma, vocal cord dysfunction isn’t an immune system reaction and doesn’t involve the lower airways. Treatment for the two conditions also is different.
When vocal cord dysfunction is not correctly identified, it is often treated with asthma medicines. Vocal cord dysfunction is a separate diagnosis from asthma. Vocal cord dysfunction symptoms do not improve with asthma treatments.
Incorrect diagnosis and treatment may lead to frequent emergency room visits. It may also lead to using oral steroid medicine. Sometimes the wrong diagnosis leads to hospitalization.
There are side effects of taking asthma medicine when you don’t have asthma. If you have both asthma and vocal cord dysfunction, you will need to be treated appropriately for both conditions.
Your doctor needs to make sure that you do NOT have vocal cord damage, damaged vocal cord nerves, a vocal cord growth or other problems that are different than vocal cord dysfunction. Vocal cord dysfunction can be very hard to prove. Your doctor can find out if you have vocal cord dysfunction by testing your breathing and looking at your vocal cords.
Treatment for vocal cord dysfunction may involve special breathing exercises called panting maneuvers, speech therapy, biofeedback and avoidance of irritants.
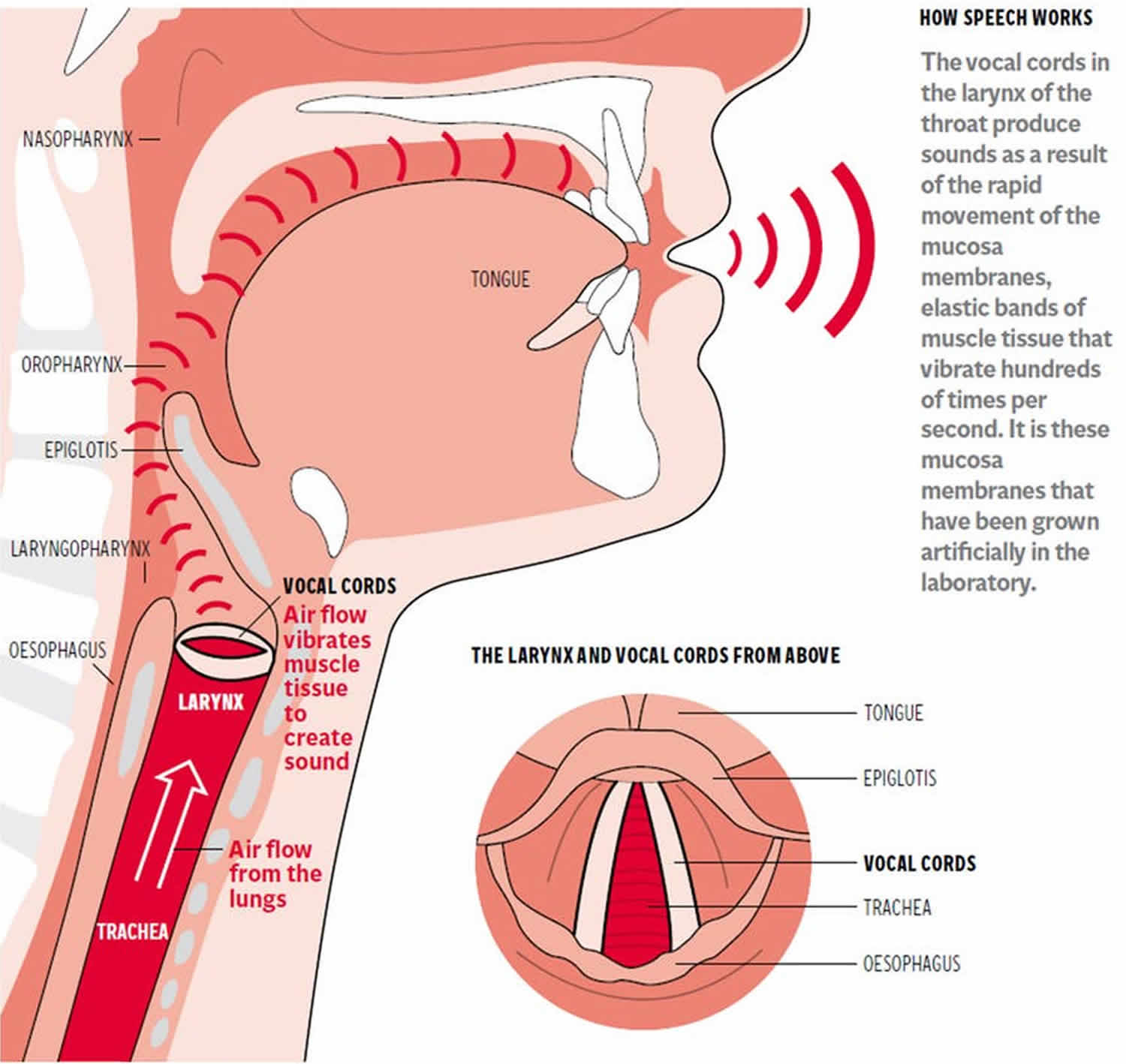
What are vocal cords and what do vocal cords do?
Vocal cords are folds of tissue in your voice box (larynx) at the top of the trachea (windpipe). They protect the airway by coughing and throat clearing. Vocal cords open during breathing, close during swallowing, and vibrate for speaking, singing and making sounds. Normally, when you breathe in (inhale), your vocal cords open. This allows air to go into your windpipe (trachea) and lungs. When you breathe out (exhale), your vocal cords open and let the air out of your lungs. Breathing out can cause your the vocal cords to vibrate and lets you produce sounds for speaking.
Figure 1. Vocal cords
Can you die from vocal cord dysfunction?
No. However, vocal cord dysfunction can be very hard to prove, because vocal cord dysfunction and asthma have similar triggers and symptoms, it’s common for vocal cord dysfunction to be misdiagnosed as asthma. Your doctor can find out if you have vocal cord dysfunction by testing your breathing and looking at your vocal cords.
Many people who have a diagnosis of vocal cord dysfunction or exercise-induced laryngeal obstruction may have problems with:
- Asthma
- Upper respiratory infections
- Post nasal drip
- Gastroesophageal reflux or gastroesophageal reflux disease (GERD)
- Laryngopharyngeal reflux
- Exposure to airborne irritants (e.g., pollution, chemicals, allergens)
- Strong odors, fumes or inhaled chemical exposure
- Exercise/exertion
- Stress or anxiety.
Exposure to irritants such as postnasal drainage associated with nasal and sinus congestion and/or reflux associated with gastroesophageal reflux or gastroesophageal reflux disease (GERD) and laryngopharyngeal reflux can lead to chronic irritation of the throat.
Vocal cord dysfunction can also be aggravated by increased chest, shoulder and neck tension.
Chronic cough and frequent throat clearing can further irritate vocal cords contributing to hypersensitivity.
Vocal cord dysfunction triggers
There are many different possible triggers of vocal cord dysfunction. Often no trigger can be found.
Possible triggers of vocal cord dysfunction and are often similar to asthma triggers. However, it is important to know that not all people who experience vocal cord dysfunction have asthma.
Vocal cord dysfunction may be triggered by:
- Acid reflux (GERD)
- Post-nasal drip
- Upper respiratory infection (cold)
- Exercise
- Strong odors, fragrances or fumes
- Tobacco smoke
- Strong emotions
- Stress and anxiety
- Coughing, laughing or singing
- Changes in temperature and humidity
Vocal cord dysfunction causes
Top three triggers that cause vocal cord dysfunction are:
- Exercise
- Post-nasal drip
- Gastroesophageal reflux disease (GERD) or acid reflux
Vocal cord dysfunction symptoms
Vocal cord dysfunction signs and symptoms include:
- Shortness of breath
- Intermittent hoarseness or hoarse voice
- A feeling of choking or suffocation
- Noisy breathing (stridor, gasping, raspy sounds or wheezing)
- Frequent cough and/or throat clearing
- Chest and/or throat tightness
- Difficulty getting air into or out of your lungs
Vocal cord dysfunction can come on suddenly and may be mild or sometimes severe and make you go to the emergency room. Even if an attack is severe, the oxygen level in your blood is usually normal. Vocal cord dysfunction symptoms do not usually occur during sleep.
Vocal cord dysfunction diagnosis
A respiratory doctor will evaluate your breathing and determine what things make your symptoms worse. A detailed evaluation is needed to correctly diagnose vocal cord dysfunction.
The diagnosis will also help determine the most effective treatment of vocal cord dysfunction or inducible laryngeal obstruction.
Your doctor may suspect vocal cord dysfunction rather than asthma if:
- It’s harder to breathe in than breathe out when symptoms flare up.
- Asthma medications don’t seem to ease your symptoms.
- Results of breathing (pulmonary function) tests or other tests for asthma are normal or only show mild changes.
Because they have similar triggers and symptoms, it’s common for vocal cord dysfunction to be misdiagnosed as asthma. This can lead to use of asthma medications (bronchodilators like albuterol) that don’t help and cause side effects. Some people have both vocal cord dysfunction and asthma, and require treatment for both conditions.
When a person with both vocal cord dysfunction and asthma starts to cough, wheeze or have trouble breathing, it can be difficult to tell if the symptoms are from asthma, vocal cord dysfunction, or both at the same time.
Common tests for vocal cord dysfunction
Vocal cord dysfunction diagnosis usually includes:
- Lung function (breathing) test called spirometry looks at how well air moves in and out of your lungs. It also includes a flow-volume loop to show how the air flows into your lungs. If you are having vocal cord dysfunction symptoms during the test, the test will sometimes, but not always, show blockage mainly of the air flowing into the lungs. Breathing test results are usually normal if your vocal cord dysfunction is not active at the time of testing. This is one reason why determining if you have vocal cord dysfunction can be so hard.
- Laryngoscopy is the best way to tell if you have vocal cord dysfunction. A healthcare worker will look at your vocal cords when you are having difficulty breathing. To look at your vocal cords, a small, flexible tube with a camera (laryngoscope) is passed through your nose to the back of your throat where your vocal cords can be seen. Before the laryngoscope is put into your nose, medicine to numb your nose and throat is used. The test is usually done as an outpatient. You are awake for this test and during the test you may be asked to talk, to see if your vocal cords work normally. Laryngoscopy can help show that you do NOT have vocal cord damage or other vocal cord problems besides vocal cord dysfunction.
- Challenge study. A challenge study may be done with lung function testing after you exercise on a treadmill or cycle or inhale a medicine called methacholine or histamine to try to bring on vocal cord dysfunction symptoms. If symptoms develop, a breathing test or laryngoscopy will be done to confirm the abnormal closure of the vocal cords. A challenge study may be combined with laryngoscopy called continuous laryngoscopy during exercise (CLE).
- Continuous laryngoscopy during exercise. Continuous laryngoscopy during exercise (CLE) enables your doctor to see what is happening in the upper airway during intense exercise. This test is used to evaluate vocal cord dysfunction and exercise-induced laryngeal obstruction.
- Speech consultation: Speech therapy can also be useful in diagnosing vocal cord dysfunction. As symptoms must be present during laryngoscopy or spirometry to accurately diagnose vocal cord dysfunction, sometimes the inappropriate airway restriction is missed during testing because it wasn’t provoked. A speech-language pathologist who specializes in vocal cord dysfunction can assess your medical history, symptoms and treatment response to determine whether vocal cord dysfunction is present, while concurrently beginning therapy.
Vocal cord dysfunction treatment
Vocal cord dysfunction is different than many other breathing problems because medicines are not the main treatment to control or prevent vocal cord dysfunction. Treatment for patients diagnosed with vocal cord dysfunction or inducible laryngeal obstruction, includes medical and behavioral care. The main treatment for vocal cord dysfunction is learning techniques that help you control your vocal cords. These techniques are usually taught by a speech therapist or psychologist who is trained and experienced in treating vocal cord dysfunction.
Behavioral Treatment
Speech therapy is the basis of treatment. Individualized exercises and techniques are taught to help you:
- Learn and feel comfortable using different breathing techniques. National Jewish Health invented the latest breathing methods
- Increase awareness of body posture
- Encourage throat muscles to relax
- Decrease vocal cord sensitivity to odors, temperature changes, exercise and other triggers.
The goal of therapy is to teach you techniques to prevent, and ultimately eliminate vocal cord dysfunction or inducible laryngeal obstruction.
Supportive counseling is an important part of treatment. It can help people adjust to a new diagnosis and a new treatment program. Counseling can also help identify and deal positively with stress. Stress may be an underlying factor in vocal cord dysfunction. Most people with vocal cord dysfunction find counseling to be very beneficial. Sometimes performance psychologists can be helpful for people with exercise-induced laryngeal obstruction.
Treating other symptoms
- Allergies
- Infection
- Acid reflux
- Other health conditions
If you have asthma and vocal cord dysfunction, it is important that you take actions to keep both under good control.
If your vocal cord dysfunction is triggered by post-nasal drip or acid reflux disease (GERD), it is important to talk to your healthcare provider about what you can to do control these.
Strong emotions and stress can trigger vocal cord dysfunction so it is important to learn to manage your stress. Relaxation techniques, biofeedback, and psychotherapy have been shown to be helpful in controlling vocal cord dysfunction.
Speech therapy
- Breathing techniques
- Cough suppression
- Throat clearing techniques
- Voice therapy
A speech-language pathologist can provide treatment for vocal cord dysfunction.
Initial Consult
A speech-language pathologist will:
- Assist in the identification of triggers
- Provide education on anatomy and function of the throat, larynx and vocal cords
- Provide education on techniques to prevent and eliminate vocal cord dysfunction and regain control
- Provide techniques to minimize abusive behaviors such as chronic coughing and frequent throat clearing
Follow-up Visits
A speech-language pathologist will:
- Review and reinforce techniques
- Provide support and encouragement for consistent application
Irritant Challenge
A speech-language pathologist will:
- Provide education/support for implementation of techniques to de-escalate vocal cord dysfunction when exposed to triggers
Exercise Challenge
A speech-language pathologist will:
- Provide education/support for implementation of techniques to de-escalate vocal cord dysfunction when triggered with exercise
- Common challenges include walking, running, sprinting, biking, skating, swimming, dancing/cheering, wrestling, basketball and baseball
Breathing Technique
The techniques you will learn will help to improve your ability to relax your throat muscles which allows your vocal cords to behave normally. You may have to meet with a therapist at least 2–3 times to learn these techniques. Learning these techniques takes regular practice. You will need to practice them even when you are not having vocal cord dysfunction, so you can be ready to control the symptoms before they become severe.
Breathing technique 1
There are 3 steps to this particular method.
- As soon as one feels an attack coming, SLOWLY breath in through your NOSE. DO NOT BREATH IN THROUGH THE MOUTH! Sometimes deliberately holding breath for 5 seconds prior to nasal inhalation helps.
- More quickly exhale out the mouth with pursed lips.
- Continue slow nasal inhalation and quick mouth exhalation with pursed lips until the episode passes.
Why does this work?
For some reason, nasal breathing reinforces the brain to keep the vocal cords apart when inhaling. Quick inhalation through the mouth seems to do the opposite and encourage the vocal cords to close which exacerbates the problem. Also, quick inhalation reinforces the Bernoulli Principle that as a fluid (air in this case) passes through a pipe that suddenly narrows (the vocal cords), the pressure actually decreases which encourages further narrowing (or vocal cord closure). Therefore, SLOW breathing helps keep the vocal cords apart! You can test this principle yourself by sucking air on a narrow short straw slowly and than quickly. You will find that the straw will tend to collapse when sucking in quickly.
Straw Breathing
This method essentially forces a person to decrease the speed of breathing allowing for vocal cord relaxation. In essence, cut a regular drinking straw to half its length. When an attack occurs, place the straw in your mouth and make a tight seal. Breath thru the straw (via mouth) until attack passes. Patients with recurrent laryngospasm attacks typically keep a straw in their pocket or purse to have immediately on hand.
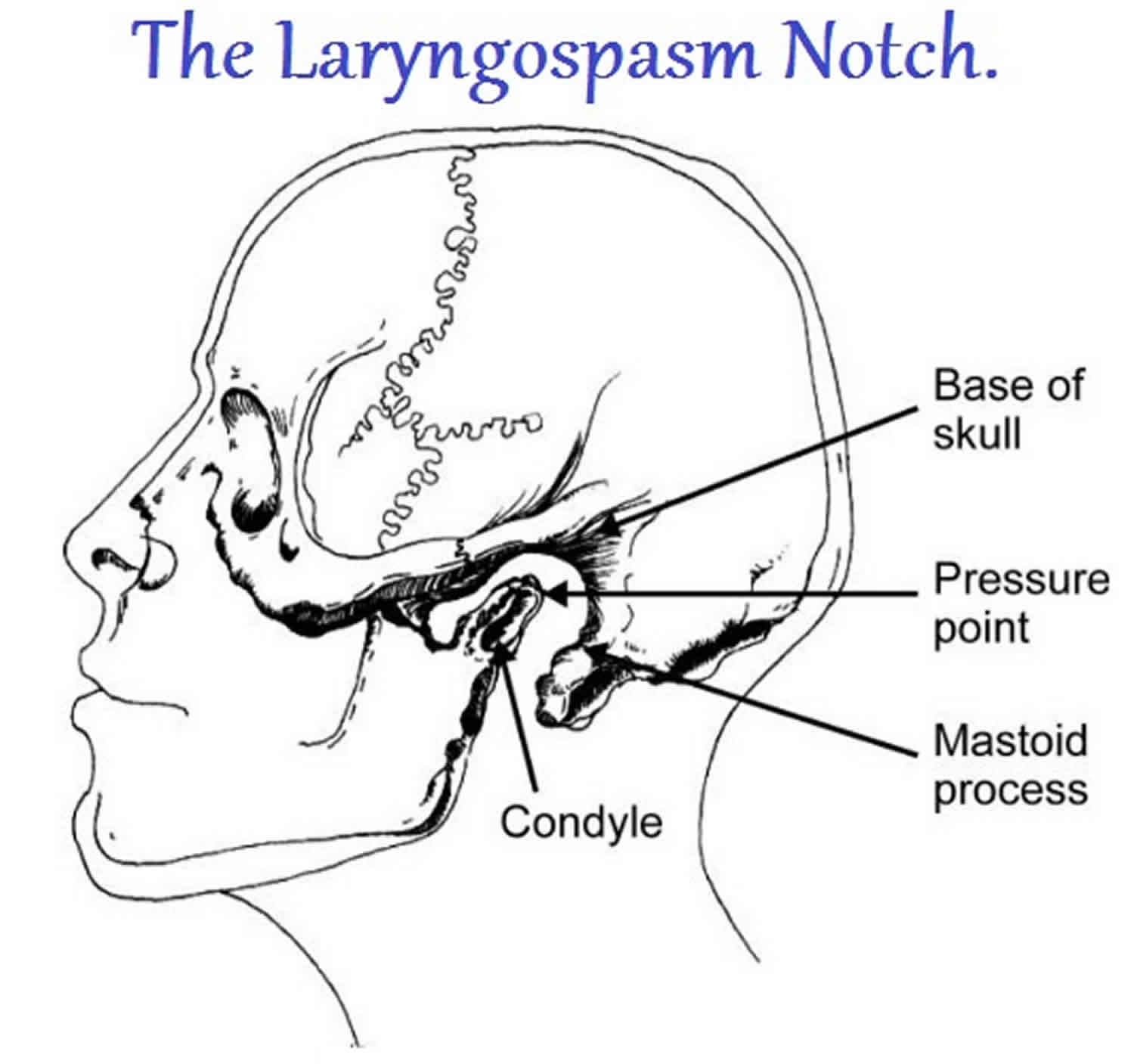
Pressure Point
Another manuever called the Larson maneuver that may work is firm pressure in the “laryngospasm notch”. Basically, with an attack, quickly with your (or somebody else’s) index fingers, press very firmly just behind both your earlobes where there is a notch between the bone of your mastoid process and ear. Press deep and forward towards the nose. It should hurt. If it doesn’t hurt, you are not pressing hard enough. The attack should resolve within 10 seconds. Below is a video describing this method (the Larson maneuver).
Figure 2. Laryngospasm notch
CPAP
This particular method applies only if laryngospasm attacks occur mainly at night while sleeping. Essentially, one uses a continuous positive airway pressure (CPAP) machine which blows air into your lungs while you sleep. This treatment helps by preventing the body from believing it is "drowning" which would result in vocal cord adduction. By having a persistent positive airflow from the CPAP device, it also reinforces to the brain to keep the vocal cords apart. At worst case, if an attack occurs, the CPAP machine helps push air into your lungs past the vocal cords. Indeed… if you ask any anesthesiologist what they do when a laryngospasm attack occurs during intubation, they’ll say apply strong positive pressure by mask (along with other things of course). Make sure you use heated humidification. Please be aware that the air pressure being applied MAY actually cause laryngospasm due to direct vocal cord irritation of the forced air. Unfortunately, there’s no way to predict someone who will respond vs someone who will do worse with this treatment method.
Botox injection
In rare cases, doctor will consider injecting Botox into the vocal cords which will physically prevent the vocal cords from coming together and as such, prevent the difficulty in breathing should an attack occur. In some people, it decreases not only the severity, but also the frequency of attacks. The way Botox is injected into the vocal cords is shown here for spasmodic dysphonia. Dystonia encompasses a broad and complex spectrum of clinical presentations that occur as a result of opposite muscles contracting (muscle co-contraction), involuntarily causing the muscle to spasm. Spasmodic dysphonia (SD) is a rare form of dystonia that affects the laryngeal muscles (vocal cords). It is also known as laryngeal dystonia.