Xerosis cutis
Xerosis cutis is a medical term for dry skin, a condition of rough dry skin with fine scaling of skin and occasionally with small cracks in the skin 1. Xerosis cutis is also known as winter itch, xerosis, xeroderma or asteatosis (lack of fat). Xerosis cutis develops due to a decrease in the natural oils in the outer layer of skin, which makes the skin lose water or lacking moisture in the outer horny cell layer (stratum corneum) and this results in cracks in the skin surface and inflammation 2. This is often accompanied by itch (pruritus) and risks for secondary infections 3, 4. While any part of the body can be affected, dry skin is particularly common on the shins and the arms.
Both men and women of all ages can be affected by xerosis cutis. There is some racial variability in water and lipid content of the skin.
By 60 years of age nearly everyone has xerosis cutis (dry skin). If you also take certain medication, undergo cancer treatment, or receive dialysis, you can develop excessively dry skin.
When the dry skin of an elderly person is itchy without a visible rash, it is sometimes called winter itch, 7th age itch, senile pruritus or chronic pruritus of the elderly.
Dry skin is also commonly seen in people with atopic dermatitis (also known as atopic eczema). Atopic dermatitis is a disorder characterized by inflammation of the skin (dermatitis). The condition usually begins in early infancy, and it often disappears before adolescence. However, in some affected individuals the condition continues into adulthood; in others, it does not begin until adulthood. Up to 60 percent of people with atopic dermatitis develop asthma or hay fever (allergic rhinitis) later in life, and up to 30 percent have food allergies 5. Individuals with atopic dermatitis also have an increased risk of developing other conditions related to inflammation, such as inflammatory bowel disease, rheumatoid arthritis, and hair loss caused by a malfunctioning immune reaction (alopecia areata) 5. They also have an increased risk of having a behavioral or psychiatric disorder, such as attention-deficit/hyperactivity disorder (ADHD) or depression 5. Hallmarks of atopic dermatitis include dry, itchy skin and red rashes that come and go. The rashes can occur on any part of the body, although the pattern tends to be different at different ages. In affected infants, the rashes commonly occur on the face, scalp, hands, and feet. In children, the rashes are usually found in the bend of the elbows and knees and on the front of the neck. In adolescents and adults, the rashes typically occur on the wrists, ankles, and eyelids in addition to the bend of the elbows and knees. Scratching the itchy skin can lead to oozing and crusting of the rashes and thickening and hardening (lichenification) of the skin. The itchiness can be so severe as to disturb sleep and impair a person’s quality of life.
Dry skin that starts in early childhood may be one of about 20 types of serious dry skin conditions called ichthyosis (fish-scale skin). Ichthyosis can sometimes be disfiguring and upsetting. Most people inherit ichthyosis (also called inherited ichthyosis) from their parents through a mutated (changed) gene. However, some people develop a form of acquired (nongenetic) ichthyosis from another medical disorder or certain medications (e.g., nicotinic acid, kava, hydroxyurea). People with ichthyosis may have a systemic disease, such as Hodgkin lymphoma, underactive thyroid (hypothyroidism), sarcoidosis, cancer (ichthyosis may be a cutaneous marker of internal malignancy) and HIV infection. While there is currently no cure for ichthyosis, research is ongoing and treatments are available to help manage the symptoms.
Xerosis cutis (dry skin) that begins later in life may be seen in people with certain diseases and conditions 6:
- Postmenopausal women
- Hypothyroidism (underactive thyroid)
- Chronic kidney disease
- Malnutrition and weight loss
- Subclinical dermatitis
- Treatment with certain drugs such as oral retinoids, diuretics and epidermal growth factor receptor inhibitors
People exposed to a dry environment may experience xerosis cutis 6:
- Low humidity: in desert climates or cool, windy conditions
- Excessive air conditioning
- Direct heat from a fire or fan heater
- Excessive bathing
- Contact with soap, laundry detergents and solvents
- Inappropriate topical agents such as alcohol
- Frictional irritation from rough clothing or abrasives
Xerosis cutis is often temporary — you get it only in winter, for example — but it may be a lifelong condition.
Xerosis cutis isn’t usually serious, but it can be uncomfortable and unsightly. Your skin can itch most of the time. Xerosis cutis is one of the most common causes of chronic itch 7, 8. Long-term scratching can cause thick patches of permanently itchy skin.
If you have excessively dry skin, you can do a lot on your own to improve your skin, including using moisturizers and avoiding harsh, drying soaps. Chronic or severe dry skin problems may require evaluation by a doctor who specializes in skin (dermatologist).
Without treatment, you have a greater risk of developing another skin condition, such as a skin infection. Some people develop food allergies. It’s also possible to develop irritated skin every time you touch certain objects.
Dry skin often responds well to lifestyle measures, such as using moisturizers and avoiding long, hot showers and baths. If you have very dry skin, your doctor may recommend a moisturizing product formulated for your needs.
If you have a serious skin disease, a doctor may want to treat it with a prescription cream or ointment. If your dry skin becomes itchy, you may use a lotion with hydrocortisone in it. If your skin cracks open, your doctor may prescribe wet dressings to help prevent infection.
Figure 1. Xerosis cutis face
Figure 2. Xerosis cutis feet
What is skin?
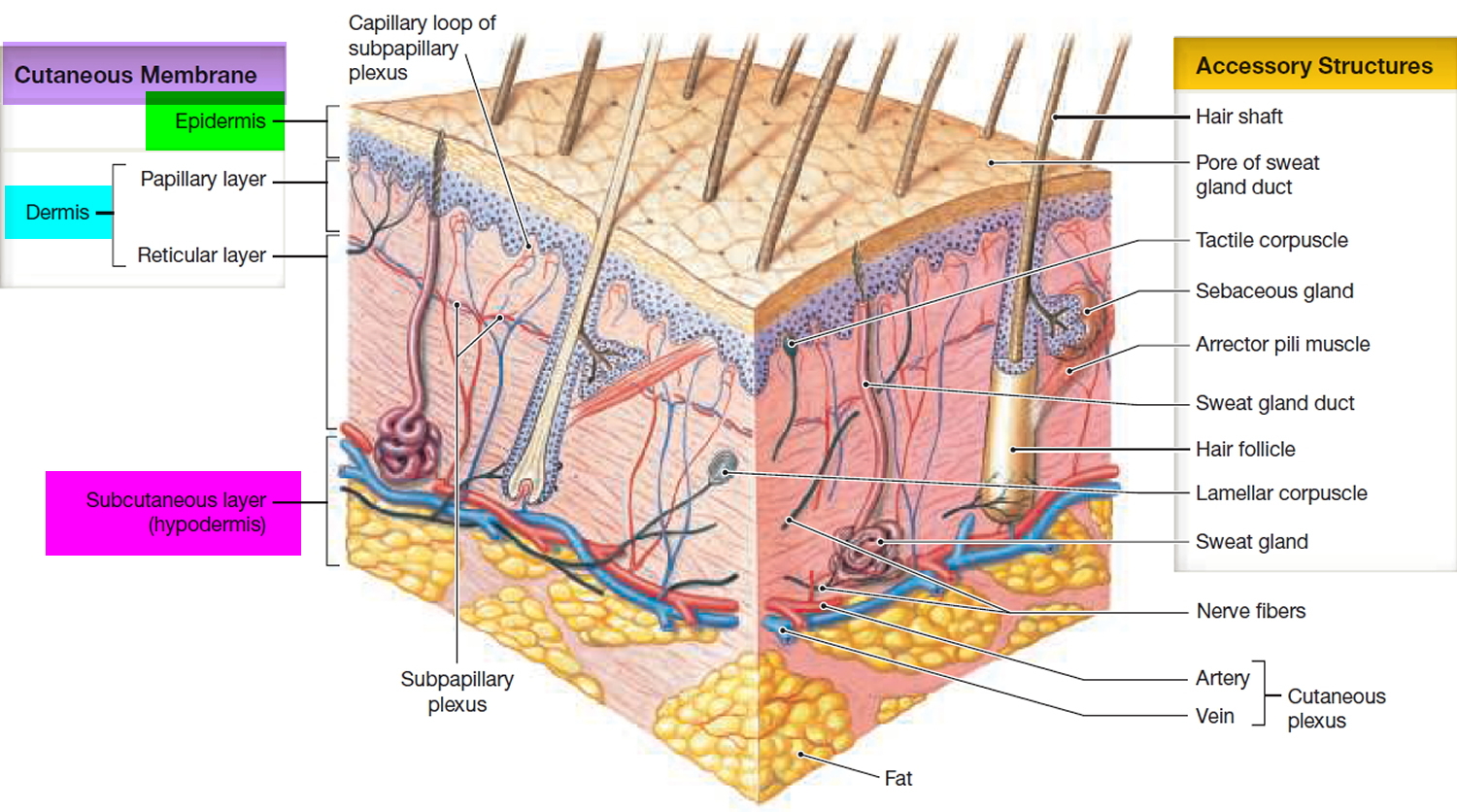
Your skin is your largest organ. Skin covers your entire body and has three layers:
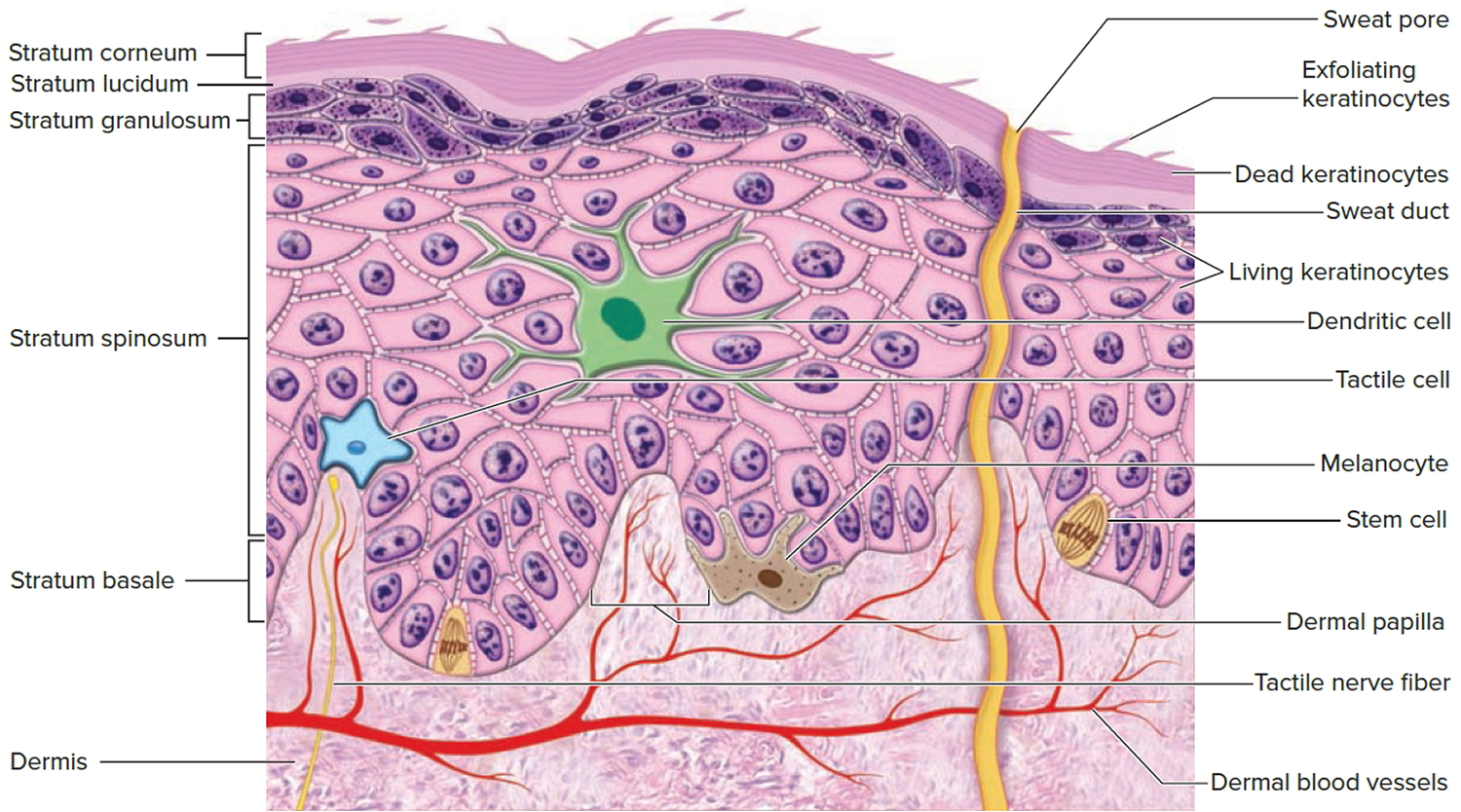
- The top layer is the epidermis (outer layer). This is a thin layer. It provides a waterproof barrier for your body. It also contains cells (melanocytes) that gives your skin colour.
- The dermis is the middle layer of skin. It is much thicker than your epidermis. It contains tough connective tissue, blood vessels, nerves, hair follicles and sweat glands.
- Beneath the dermis is the subcutaneous layer. This layer contains fat and large blood vessels.
As you age, your skin changes. Most notably there are less elastic and collagen fibers and more obvious wrinkles. These changes can be increased by too much sun exposure.
Your skin also becomes dryer as you age due to less sebum (oil) being made.
Your hair will thin as you age. This is because you have fewer active hair follicles.
Your ability to regulate your temperature through your skin also decreases as you get older. This means you are more likely to get heatstroke or hypothermia than a younger person. You are also more likely to become sunburnt.
Figure 3. Skin structure
Figure 4. Structure and skin cells of the Epidermis
Functions of skin
Your skin has many purposes:
- Skin is water-resistant and protects you from the weather.
- Skin allows you to feel things – heat, cold, touch, pain, and vibration.
- Skin protects you against infection, and is part of the body’s immune system.
- Skin helps control your body temperature. When blood flow to your skin increases is helps to release heat from your body. When blood flow to your skin decreases it helps to keep warmth in. How much moisture evaporates from your skin, also affects your body’s temperature.
- Skin absorbs ultraviolet light from the sun, which is needed to make vitamin D. Vitamin D is important for good bone health. Most Australians can get enough vitamin D through safe exposure to the sun. The Sunshine Map tells you how much sunlight you need depending on where you live.
Xerosis cutis causes
When skin loses water too quickly, it becomes dry. Dry skin is due to water loss from the outer layer of skin. This can happen for many reasons.
Some of the main causes of dry skin are:
- Low humidity weather (e.g. during winter, living in cold, windy conditions or low-humidity climates)
- Heat. Central heating, wood-burning stoves, space heaters and fireplaces all reduce humidity in the room.
- Too much bathing or scrubbing. Taking long, hot showers or baths or scrubbing your skin too much can dry your skin. Bathing more than once a day can remove the natural oils from your skin too.
- Harsh soaps and detergents (especially those that are heavily perfumed, or antibacterial). Many popular soaps, detergents and shampoos strip moisture from your skin because they are formulated to remove oil.
- Other skin conditions. People with skin conditions such as atopic dermatitis (eczema) or psoriasis are more likely to have dry skin.
- Medical treatments. Some people develop dry, thick skin after undergoing treatment for cancer, receiving dialysis or taking certain medications.
- Aging. As people age, the skin thins and produces less of the oils needed for the skin to retain water.
- Sleeping with an electric blanket turned on
- Exposing your skin to the sun
- Putting drying chemicals on your skin, such as alcohol
Xerosis cutis (dry skin) is due to abnormalities in the integrity of the barrier function of the stratum corneum, which is made up of corneocytes.
- There is an overall reduction in the lipids in the stratum corneum.
- The ratio of ceramides, cholesterol and free fatty acids may be normal or altered.
- There may be a reduction in the proliferation of keratinocytes.
- Keratinocyte subtypes change in affected skin with a decrease in keratins K1, K10 and increase in K5, K14.
- Involucrin (a protein) may be expressed early, increasing cell stiffness.
- The result is the retention of corneocytes and reduced water-holding capacity.
Ichthyosis is a disorder of cornification, characterized by persistently dry, thickened, ‘fish scale’ skin. There are at least 20 varieties of ichthyosis, including inherited and acquired forms.
The inherited forms of ichthyosis are due to loss of function mutations in various genes (listed in parentheses below).
- Ichthyosis vulgaris (FLG).
- Recessive X-linked ichthyosis (STS)
- Autosomal recessive congenital ichthyosis (ABCA12, TGM1, ALOXE3)
- Keratinopathic ichthyoses (KRT1, KRT10, KRT2)
Acquired ichthyosis may be due to:
- Metabolic factors: thyroid deficiency
- Illness: lymphoma, internal malignancy, sarcoidosis, HIV infection
- Drugs: nicotinic acid, kava, protein kinase inhibitors (eg EGFR inhibitors), hydroxyurea.
Table 1. External causes and environmental triggers of xerosis cutis
| Environmental factors | Cold; low humidity/dry indoor heat; intense exposure to sunlight |
|---|---|
| Occupational factors/hobbies | “Wet” work or contact with irritant occupational substances (e.g., hairdressers, construction and metal workers, nursing staff); housekeeping |
| Skin cleansing/washing | Frequently taking long hot showers or baths. Use of alkaline soaps and cleansing agents |
Table 2. Endogenous causes (dermatological, internal and psychiatric diseases, diet, drugs) associated with xerosis cutis
| Category | Examples of diseases/triggers |
|---|---|
| Dermatological diseases | |
| Inflammatory skin disorders | Atopic dermatitis, allergic contact eczema, irritant contact dermatitis, dyshidrotic eczema, nummular eczema, drug eruption, psoriasis, seborrheic dermatitis, perioral dermatitis |
| Genodermatoses | Ichthyoses |
| Infectious dermatoses (chronic stage) | Fungal and bacterial infections, pediculosis, scabies |
| Neoplasms | Cutaneous lymphoma (e.g., mycosis fungoides) |
| Internal diseases | |
| Endocrine and metabolic disorders | Chronic kidney disease, diabetes mellitus, hepatopathies (e.g., primary biliary cholangitis, primary sclerotic cholangitis, drug-induced cholestasis, extrahepatic cholestasis), hyperparathyroidism, hypothyroidism, malabsorption |
| Inflammatory diseases | Chronic inflammatory bowel disease (gluten-sensitive enteropathy), rheumatic disease |
| Infections | Diarrheal diseases, helminths, hepatitis B and C virus, HIV |
| Hormonal changes | Menopause, andropause, pregnancy |
| Hematological and lymphoproliferative diseases | Myeloproliferative disorders (e.g., polycythemia vera, essential thrombocytosis), Hodgkin’s disease, non-Hodgkin’s lymphoma, multiple myeloma |
| Psychiatric causes | |
| Obsessive-compulsive disorders | Obsessive skin cleansing/washing |
| Eating disorders | Anorexia |
| Addictions | Alcohol and drug abuse |
| Dietary causes | |
| Dehydration | Insufficient fluid intake, excessive perspiration |
| Malnutrition | Hypovitaminosis (vitamin D, vitamin A, niacin deficiency), zinc or iron deficiency |
| Drug-related causes | |
| Pharmaceutical drugs (not including erythema) | Retinoids, topical corticosteroids (prolonged use), diuretics, lipid-lowering agents, calcium antagonists, beta blockers, antirheumatic drugs, contraceptives/antiandrogens, cytostatic agents, radiation dermatitis (following radiation therapy), possibly immunomodulators |
Xerosis cutis risk factors
Anyone can develop dry skin. But you’re more likely to develop xerosis cutis if you:
- Are over 40, as the skin’s ability to retain moisture diminishes with age. With age, your skin produces less sebum, an oil that keeps skin soft and youthful. By your 40s, the amount of sebum your body makes drops dramatically. After 40, the amount of sebum your skin contains continues to drop.
- Live in cold, windy conditions or low-humidity climates
- Low outdoor temperature: When outdoor temperatures fall, the air holds less moisture. Research shows that this can lead to excessively dry skin.
- Wet work: A job that requires you to frequently put your hands in water throughout the day or use harsh chemicals can strip your skin of its protective layer. Hairdressers, nurses, housekeepers, construction workers, cooks, florists, and metal workers often develop excessively dry skin.
- Use your hands to work with cement, clay or soil
- Swim frequently in chlorinated pools
- Have certain diseases or conditions, such as hypothyroidism, diabetes, kidney disease or malnutrition. These conditions are known to cause excessively dry skin.
- Dialysis: Kidney disease increases your risk of developing extremely dry skin. When you receive dialysis, you have an even greater risk because dialysis removes water from your body. People receiving dialysis treatments also need to limit how much fluid they drink, consuming only 32 ounces a day. This can further dry your skin.
- Anorexia: If you’re not eating enough, you’re not getting the nutrients your skin needs to stay hydrated.
- Vitamin or mineral deficiency: Skin requires nutrients to keep it healthy. If you’re not getting enough vitamin D, vitamin A, niacin, zinc, or iron, you can develop excessively dry skin.
- Black, brown, or fair skin: Research shows that people who have brown, black, or fair skin are more likely to develop very dry skin than people who have a medium complexion, such as people who have Mediterranean ancestry.
- Use certain medications: Extremely dry skin is a possible side effect of several medications, including statins and diuretics.
- Smoking: Cigarettes contain harmful chemicals that speed up how quickly your skin ages, so skin becomes drier.
- Condition that affects the skin: Some conditions that affect the skin, including atopic dermatitis, ichthyosis, perioral dermatitis, psoriasis, and seborrheic dermatitis, can cause excessively dry skin.
- Itchy skin condition: If you’ve had a skin condition that caused itchiness at some time in your life, you have a greater risk of developing excessively dry skin. Many adults who had atopic dermatitis as a child live with extremely dry skin.
- HIV positive: Excessively dry skin is common in people who are HIV positive, even those on antiretroviral treatment (ART).
- Cancer treatment (current and past): If you’ve ever had chemotherapy, are receiving a cancer treatment called targeted therapy, or getting radiation treatments, you can develop extremely dry skin.
Xerosis cutis symptoms
The signs and symptoms of xerosis cutis (dry skin) depend on many factors, including the cause, your age, and your general health.
The most common locations for xerosis of skin include:
- Legs, especially the fronts of the lower legs (shins)
- Arms
- Trunk, especially the side areas between the bottom rib and the hip (flanks)
- Backs of the hands
Although any site can be dry, affected skin tends to involve the shins more than any other site.
If you have xerosis cutis (dry skin), you may notice your skin:
- looks dull (not shiny)
- has small lines or cracks in it
- feels rough and dry to touch
- feels tight (especially after its been wet)
- looks scaly
- flakes off in tiny bits.
Dry skin has a dull surface with a rough, scaly quality. The skin is less pliable and cracked. When dryness is severe, the skin may become inflamed and fissured.
Xerosis can be completely without symptoms (asymptomatic), though more inflamed skin tends to be mildly to severely itchy.
The clinical features of ichthyosis depend on the specific type of ichthyosis 10.
- Ichthyosis vulgaris (95% of all ichthyosis cases)
- The skin may appear normal at birth
- By the age of 5, the skin is dry with fine white scale
- Affects abdomen, arms and legs, sparing creases of arms and legs
- Causes keratosis pilaris
- Palms are excessively lined
- Associated with atopic eczema in 50%
- Recessive X-linked ichthyosis
- Generalized fine or rhomboid grey/brown scale is present at or within six months of birth
- Scaling is most prominent over the extremities, neck, trunk, and buttocks
- Palms are normal
- Corneal opacities in 50%
- Only affects males
- Undescended testicles in 5–20%
- Autosomal recessive congenital ichthyosis-1 (ARCI1)
- The baby is encased by collodion membrane at birth, which cracks and is then shed; 10% are self-healing
- Harlequin ichthyosis: severe collodion membrane, ectropion (drooping lower eyelids), eclabium (out-turned lips) and contractures
- Lamellar ichthyosis: plate-like dark scaling over the whole body, including creases of arms and legs
- Bathing suit variant: localised to scalp and trunk (warmer sites of the body)
- Nonbullous congenital ichthyosiform erythroderma (NCIE): erythroderma and fine white, superficial, semiadherent scales
- Palmoplantar keratoderma varies with affected gene
- Keratinopathic ichthyoses
- Skin is moist, red, and tender at birth
- Fluid-filled blisters may occur which may become infected and give rise to a foul skin odor
- Thick, generalised white to brown scaling occurs within a few weeks especially over extensor joints
- Epidermolytic ichthyosis may cause slowly extending annular polycyclic erythematous plaques
- Porcupine or spiky appearance in ichthyosis Curth-Macklin, due to a varied thickness of scale
- KT-1 mutation causes palmoplantar keratoderma (KRT-10 does not)
- Growth failure may occur
- Mosaic form causes epidermal naevus
- Acquired ichthyosis
- Resembles ichthyosis vulgaris but develops in adult life
- May have an underlying disease
- The patient may be taking a drug known to cause dry skin
- Ichthyosis syndromes. Ichthyosis is a component of several rare congenital syndromes. These include:
- KID GJB2, GJB6 (keratitis, ichthyosis, and deafness)
- CHIME PIGL (colobomas of the eye, heart defects, ichthyosis, mental retardation, and ear defects)
- Netherton syndrome SPINK5 (ichthyosis, erythroderma, hair shaft defects, atopic features)
- Sjögren-Larsson ALDH3A2 (ichthyosis, spastic diplegia, pigmentary retinopathy, and mental retardation)
- Refsum disease PHYH/PEX7 (ichthyosis and pigmentary retinopathy).
Xerosis cutis complications
Dry skin is usually harmless. But when it’s not cared for, dry areas of skin may become itchy, indicating a form of eczema or dermatitis has developed.
- Atopic eczema (atopic dermatitis) — If you’re prone to develop this condition, excessive dryness can lead to activation of the disease, causing a rash and cracking skin, especially in people with ichthyosis vulgaris
- Eczema craquelé also called asteatotic eczema — especially in older people.
- A dry form of nummular dermatitis or discoid eczema — especially in people that wash their skin excessively
- Infections. Dry skin may crack, allowing bacteria to enter, causing infections.
When the skin of an older person is dry and itchy without a visible rash, it is sometimes called winter itch, 7th age itch, senile pruritus or chronic pruritus of the elderly.
Other complications may include:
- Flaky skin or itchy skin (pruritus)
- Skin infection when bacteria or viruses penetrate a break in the skin surface
- Overheating, especially in some forms of ichthyosis
- Food allergy, eg, to peanuts, has been associated with filaggrin mutations
- Contact allergy, eg, to nickel, has also been correlated with barrier function defects.
These complications are most likely to occur when your skin’s protective mechanisms are severely compromised. For example, severely dry skin can cause deep cracks or fissures, which can open and bleed, providing an avenue for invading bacteria.
Xerosis cutis prevention
Try these tips to help your skin retain moisture:
- Moisturize. Moisturizer seals in water to help keep your skin’s protective barrier healthy. Use moisturizer throughout the day, especially on the hands. And before going outdoors, use a moisturizer that contains sunblock or a broad-spectrum sunscreen with an SPF of at least 30, even on cloudy days. Apply sunscreen generously and reapply every two hours — or more often if you’re swimming or sweating.
- Apply an emollient liberally and often, particularly shortly after bathing, and when itchy. The drier the skin, the thicker this should be, especially on the hands.
- Limit water exposure. Keep bath and shower time to 10 minutes or less. Use lukewarm water, not hot water. Rinse and pat dry. Try to bathe no more than once a day.
- Use a gentle cleanser or allergen-free soap. Try a nonsoap cleansing cream or shower gel. Or use fragrance-free moisturizing soap with no alcohol or allergy-causing substances (hypoallergenic soap), especially if you handwash often. Rinse thoroughly and pat dry. Apply a moisturizing cream while your skin is still damp.
- Replace standard soap with a substitute such as a synthetic detergent cleanser, water-miscible emollient, bath oil, anti-pruritic tar oil, colloidal oatmeal etc.
- Shave with care. Shaving can be drying. If you shave, use a lubricating agent before you start. Shave in the direction of hair growth, unless that irritates your skin. Use a sharp blade and rinse it with warm water after each stroke. When done, apply moisturizer.
- Cover as much skin as possible in cold or windy weather. Harsh weather can be especially drying to skin. Scarves, hats, and gloves or mittens help protect your skin when you’re outdoors.
- Use a humidifier in winter and air conditioner in summer.
- Wear gloves. Protect your hands with suitable gloves when gardening, using harsh cleansers and doing other skin-drying activities.
- Rinse and moisturize after swimming. This is especially important if you’ve been swimming in a heavily chlorinated pool.
- Ensure good hydration by drinking plenty of water. Drink noncaffeinated beverages each day to help keep all your body’s tissues, including your skin, well hydrated.
- Bathe babies with care. For babies, using a cleanser every 1-2 weeks for bathing usually is enough. Otherwise, bathe them in just water. However, clean their diaper area with each diaper change. Apply a thin layer of petroleum jelly (Vaseline, Aquaphor, others) while the skin is still damp.
Xerosis cutis diagnosis
To diagnose dry skin, your doctor is likely to examine you by looking at your skin and ask about your medical history. You might discuss when your dry skin started, what factors make it better or worse, what your bathing habits are, and how you care for your skin.
Before your appointment, it’s helpful to make sure that you can answer the following questions:
- Have you (or any close blood relatives) had atopic dermatitis, asthma, hay fever, or food allergies?
- How long have you had the excessively dry skin?
- What worsens your dry skin?
- What treatments have you tried?
This will help your skin doctor (dermatologist) uncover what’s causing your excessively dry skin.
Your doctor may suggest that you have some tests to see if your dry skin is being caused by a medical condition, such as an underactive thyroid (hypothyroidism). Often, dry skin is a symptom of another skin condition, such as dermatitis or psoriasis.
In children
- Family history
- Age of onset
- Appearance at birth, if known
- Distribution of xerosis cutis
- Other features, e.g., eczema, abnormal nails, hair, dentition, sight, hearing.
In adults
- Medical history
- Medications and topical preparations
- Bathing frequency and use of soap
- Evaluation of environmental factors that may contribute to xerosis cutis.
Sometimes a skin biopsy may be requested. There may be additional tests requested to diagnose some types of ichthyosis. Your doctor may also suggest certain diagnostic tests to check whether your dry skin is the result of an underlying medical condition, such as an underactive thyroid (hypothyroidism).
Xerosis cutis treatment
Xerosis cutis often responds well to lifestyle measures, such as using moisturizers and avoiding long, hot showers and baths. If your doctor suspects that a medical condition is causing your dry skin, then he or she may do blood tests or other diagnostic procedures. The best treatment for dry skin caused by a medical problem is to treat the medical problem.
The mainstay of treatment of xerosis cutis (dry skin) and ichthyosis is moisturizers or emollients by applying a cream or ointment throughout the day. Emollients are products used to soften your skin. Moisturizers are products used to add moisture to your skin. Creams and ointments tend to be more effective than lotion. They should be applied liberally and often enough to:
- Reduce itch
- Improve the skin barrier function
- Prevent entry of irritants, bacteria
- Reduce transepidermal water loss.
When considering which emollient is most suitable, consider:
- Severity of the dryness
- Tolerance
- Personal preference
- Cost and availability.
Emollients generally work best if applied to damp skin, if pH is below 7 (acidic), and if containing humectants such as urea or propylene glycol.
Active ingredients of emollients and moisturizers are occlusives and humectants. They often include other ingredients, such as surfactants (non-soap cleansers), fragrances and preservatives. Occlusives are oils of non-human origin, often mixed with water and an emulsifier to form a lotion or cream. They provide a layer of oil on the surface of the skin to reduce water loss from the stratum corneum.
Note: Creams and lotions are prone to microbial contamination and preservatives are added to improve shelf life. Preservatives in moisturizers can lead to contact allergic dermatitis in sensitive individuals.
If you have a serious skin disease, a doctor may want to treat it with a prescription cream or ointment. If your dry skin becomes itchy, you may use a lotion with hydrocortisone in it. If your skin cracks open, your doctor may prescribe wet dressings to help prevent infection.
Table 3. Classification of commonly used active ingredients for basic skin care in patients with xerosis cutis
| Class | Mode of action | Active ingredients (examples) |
|---|---|---|
| Remoisturizing | ||
| Natural moisturizing factor | Physiologically formed by the breakdown of filaggrin in the skin; occurs in sweat; binds water in the skin. | Urea, lactic acid derivatives, pyrrolidine carboxylic acid (PCA), amino acids (alanine, arginine, citrulline, glycine, histidine, leucine, lysine, serine, threonine), inorganic salts |
| Other moisturizing factors (humectants) and swelling agents | Hydrophilic and hygroscopic substances that reduce transepidermal water loss and/or improve water distribution. | Glycerol, glyceryl glucoside (GG), hyaluronic acid, glycosaminoglycans, glycols (propylene glycol, polyethylene glycol/macrogols (PEG), butylene glycol), various sugars and sugar alcohols** |
| Film forming | ||
| Hydrocarbon mixtures based on mineral oil | Form a hydrophobic film on the surface of the skin, thus reducing water loss. | Vaseline (petroleum jelly), liquid paraffin, wax, microcrystalline ozokerite |
| Silicone oils | Form a thin hydrophobic, semi-occlusive (permeable to water vapor) film on the surface of the skin; positive effects on spreadability | Dimethicone, methicone, polysiloxane, cyclomethicone |
| Lipid replenishing | ||
| Physiological barrier lipids | Replenish the intercellular lipid matrix | Ceramides, sterols, cholesterol derivatives, squalenes, triglycerides, free fatty acids |
| Naturally occurring oils, fats and waxes | Provide numerous polyunsaturated omega-6 fatty acids (linoleic acid, γ-linolenic acid), phytosterols and sterols for the formation of skin barrier lipids; form a hydrophobic film on the surface of the skin. | e.g., evening primrose oil, grape seed oil, safflower oil, canola oil, sunflower oil, flaxseed oil, almond oil, borage oil, jojoba oil, shea butter, lanolin#, beeswax# |
| Skin soothing | ||
| Inhibit, for example, the secretion of mediators of inflammation; capture free radicals and/or promote wound healing | Licochalcone A, glycyrrhizic acid, dexpanthenol, oat extract# bisabolol#, vitamins A, E, B (niacinamide), witch hazel | |
| Antipruritic | ||
| Act as local anesthetic, relieve pain and/or activate cold receptors | Polidocanol, menthol, menthoxypropanediol, N-palmitoylethanolamide, camphor, tannins |
Footnotes: The drier the skin, the more lipids the base should contain. For acute, inflammatory disease stages, vehicles with a higher water content are preferable. Skin-soothing and antipruritic substances can be added. Pure fats/oils are generally NOT suited for long-term basic skin care.
** Fructose, glucose, inositol, mannitol, sorbitol, butylene.
# Sensitization potential.
Occlusive moisturizers
The choice of occlusive emollient depends upon the area of the body and the degree of dryness and scaling of the skin.
- Bath oil deposits a thin layer of oil on the skin upon rising from the water.
- Lotions are more occlusive than oils. Lotions are used for the scalp and other hairy areas and for mild dryness elsewhere
- Creams are more occlusive again. Thicker barrier creams containing dimethicone are particularly useful for hand dermatitis. Creams are used when more emollience is required.
- Ointments are the most occlusive and include pure oil preparations such as equal parts of white soft and liquid paraffin or petroleum jelly. Ointments are prescribed for dry, thick, scaly areas, but many patients find them too greasy.
Sorbolene and glycerine cream is a general-purpose moisturizer that is non-greasy, cheap and available in bulk without prescription.
The minimum quantity for an occlusive emollient is 250 g (or ml) and often 500 g or 1 kg is needed: liberal and regular usage is to be encouraged. How frequently it is applied depends on how dry your skin is: very dry skin may benefit from a greasy emollient every couple of hours, but slightly dry skin may only need a light moisturizer at night.
Humectants
Humectants increase the water holding capacity of the stratum corneum. They include:
- Glycerine
- Urea
- Alpha hydroxy acids such as lactic acid or glycolic acid.
- Salicylic acid
Urea and the acidic preparations often sting if applied to scratched or fissured skin. They are also keratolytic, ie they have a descaling or peeling effect, important in the management of ichthyosis.
Additional treatments
Additional treatments include:
- Topical steroid if itchy or there is dermatitis — choose an emollient base
- Topical calcineurin inhibitors if topical steroids are unsuitable.
Home remedies
Many people can heal dry skin at home on their own.
The following measures can help keep your skin moist and healthy:
- Gently wash your face at least twice a day. Use a gentle, alcohol-free, nonfoaming cleanser on your face twice a day and after sweating. Products with stearic acid (found in shea butter) or linoleic acid (found in argan oil and others) can help repair your skin. If you have sensitive skin, wash with a cleanser in the evening and just rinse with water other times. While your skin is still damp, apply any topical medication you’re using, wait a few minutes (see medication packaging for specifics), then apply your moisturizer. If you use cosmetics, consider selecting products with a cream or oil base. Use a moisturizer that contains sunblock or a broad-spectrum sunscreen with an SPF of at least 30, even on cloudy days. Apply sunscreen generously and reapply every two hours — or more often if you’re swimming or sweating.
- Moisturize. Apply moisturizer several times a day, especially when your skin feels dry and after handwashing or bathing, while your skin is still moist. Ask your doctor about the pros and cons of various products for your skin and condition. You may need to try several products before you find those you like, that help you and that you’ll use regularly. Look for healing ingredients such as urea, ceramides, fatty acids and glycerol (also known as glycerin), shea butter, and cocoa butter. Look for fragrance-free products that don’t cause acne (noncomedogenic) and don’t contain allergy-causing substances (hypoallergenic). Avoid products that contain sodium lauryl sulfate, which is drying. For the face and neck, you might want to use a cream. Choose something that’s easy to apply and leaves no visible residue. If you are acne-prone, avoid products on your face that contain petroleum jelly, cocoa butter or coconut oil. If you skin is very oily, try using a sunscreen instead of a moisturizer. If you have mature skin, you might prevent scaly, flaky skin by using products that contain antioxidants or alpha hydroxy acid. Moisturizers often form the basis for wrinkle creams, with added retinoids, antioxidants, peptides and other ingredients. If nonfacial skin is very dry, you might want to use a thicker moisturizer (Eucerin, Cetaphil, others) or an oil, such as baby oil. Oil has more staying power than do lotions and prevents the evaporation of water from the skin’s surface. Another possibility is a petrolatum-based product (Vaseline, Aquaphor, others). If it feels too greasy, use it only at bedtime or just on tiny cracks in your skin. For very dry hands, apply petroleum jelly liberally at bedtime and put on plain cotton socks or gloves.
- Use warm water and limit bath time. Long showers or baths and hot water remove your skin’s natural oils. Limit bathing to no more than once a day and no longer than 5-10 minutes. Use warm, not hot, water.
- Avoid harsh, drying soaps. It’s best to use cleansing creams or gentle skin cleansers and bath or shower gels with added moisturizers. Choose mild soaps that have added oils and fats. Avoid deodorant and antibacterial detergents, fragrance, and alcohol.
- Use allergen-free moisturizing soap. For handwashing, use fragrance-free (hypoallergenic) moisturizing soap. Then apply a moisturizing cream while your hands are still damp. In the shower or bath, try a nonsoap cleansing cream or shower gel, and use soap only in areas where needed, such as the armpits and groin. Avoid loofahs and pumice stones. Rinse thoroughly and pat dry.
- Use a humidifier. Hot, dry, indoor air can parch sensitive skin and worsen itching and flaking. A portable home humidifier or one attached to your furnace adds moisture to the air inside your home. Be sure to keep your humidifier clean to ward off bacteria and fungi.
- Choose fabrics that are kind to your skin. Natural fibers, such as cotton, allow your skin to breathe. Wool, although natural, sometimes irritates even healthy skin. For laundry, use detergents without dyes or perfumes, both of which can irritate your skin. These types of products usually have the word “free” in their names.
- Relieve itchiness. If dry skin causes itchiness, apply a clean, cool, damp cloth to the affected area. You might also apply an anti-itch cream or ointment, containing at least 1% hydrocortisone.
If these measures don’t relieve your symptoms or if your symptoms worsen, see your doctor or consult a dermatologist about creating a personalized skin care plan based on your skin type and any skin condition you may have.
Xerosis cutis prognosis
Researchers have found that when patients follow the prescribed treatment plan, most people see their skin heal.
If you have trouble following your treatment plan, be sure to tell your doctor or dermatologist. To get relief and prevent worsening, it’s essential to follow the treatment plan.
Let your doctor or dermatologist know if you:
- Find it difficult to apply the moisturizer as often as necessary
- Cannot reach areas where you need to apply your moisturizer
- Have problems protecting your skin at work
Your doctor or dermatologist can work with you to develop a plan that you can follow. That’s important. To get relief, you need to treat excessively dry skin.
- Amin R, Lechner A, Vogt A, Blume-Peytavi U, Kottner J. Molecular characterization of xerosis cutis: A systematic review. PLoS One. 2021 Dec 16;16(12):e0261253. doi: 10.1371/journal.pone.0261253[↩]
- White-Chu EF, Reddy M. Dry skin in the elderly: complexities of a common problem. Clin Dermatol. 2011 Jan-Feb;29(1):37-42. doi: 10.1016/j.clindermatol.2010.07.005[↩]
- Lichterfeld-Kottner A, Lahmann N, Blume-Peytavi U, Mueller-Werdan U, Kottner J. Dry skin in home care: A representative prevalence study. Journal of Tissue Viability. 2018;27(4):226–31. doi: 10.1016/j.jtv.2018.07.001[↩]
- Lechner A, Lahmann N, Neumann K, Blume-Peytavi U, Kottner J. Dry skin and pressure ulcer risk: A multi-center cross-sectional prevalence study in German hospitals and nursing homes. International Journal of Nursing Studies. 2017;73:63–9. doi: 10.1016/j.ijnurstu.2017.05.011[↩]
- Atopic dermatitis. https://medlineplus.gov/genetics/condition/atopic-dermatitis[↩][↩][↩]
- Dry skin. https://dermnetnz.org/topics/dry-skin[↩][↩]
- Yosipovitch G, Bernhard JD. Clinical practice. Chronic pruritus. N Engl J Med. 2013 Apr 25;368(17):1625-34. doi: 10.1056/NEJMcp1208814[↩]
- Valdes-Rodriguez R, Stull C, Yosipovitch G. Chronic pruritus in the elderly: pathophysiology, diagnosis and management. Drugs Aging. 2015 Mar;32(3):201-15. doi: 10.1007/s40266-015-0246-0[↩]
- Augustin, M., Wilsmann-Theis, D., Körber, A., Kerscher, M., Itschert, G., Dippel, M. and Staubach, P. (2019), Diagnosis and treatment of xerosis cutis – a position paper. JDDG: Journal der Deutschen Dermatologischen Gesellschaft, 17: 3-33. https://doi.org/10.1111/ddg.13906[↩][↩][↩]
- Oji V, Tadini G, Akiyama M, Blanchet Bardon C, Bodemer C, Bourrat E, Coudiere P, DiGiovanna JJ, Elias P, Fischer J, Fleckman P, Gina M, Harper J, Hashimoto T, Hausser I, Hennies HC, Hohl D, Hovnanian A, Ishida-Yamamoto A, Jacyk WK, Leachman S, Leigh I, Mazereeuw-Hautier J, Milstone L, Morice-Picard F, Paller AS, Richard G, Schmuth M, Shimizu H, Sprecher E, Van Steensel M, Taïeb A, Toro JR, Vabres P, Vahlquist A, Williams M, Traupe H. Revised nomenclature and classification of inherited ichthyoses: results of the First Ichthyosis Consensus Conference in Sorèze 2009. J Am Acad Dermatol. 2010 Oct;63(4):607-41. doi: 10.1016/j.jaad.2009.11.020[↩]