Yellow nail syndrome
Yellow nail syndrome is a very rare disorder characterized by three features: yellow nail discoloration affecting the fingernails and toenails, abnormalities affecting the lungs and the airways (respiratory tract) and swelling or puffiness in different parts of the body because of the accumulation of protein-rich fluid (lymph) in the soft layers of tissue under the skin (lymphedema) 1. Yellow nail syndrome usually occurs in older adults with most cases occurring in individuals over 50 years of age, but can also occur in children 2. In addition to being yellow, nails may lack a cuticle, grow very slowly, and become detached (onycholysis) 1. Respiratory problems may include chronic cough, bronchiectasis, and pleural effusion 2. Chronic sinusitis may also occur 2. The cause of yellow nail syndrome remains unknown. It usually occurs on its own, but is sometimes associated with autoimmune disease, lymphatic diseases, or cancers. Some researchers have hypothesized that titanium may play a role in the development of yellow nail syndrome (for example, in dental or joint implants or other environmental exposures).
Yellow nail syndrome affects males and females in equal numbers. More than 100 cases have been reported in the medical literature.
Yellow nail syndrome management aims to address each of the symptoms. Treatment for nail discoloration may include oral vitamin E and/or triazole antifungals. Pleural effusion may be treated with surgery. Antibiotic prophylaxis may be prescribed for bronchiectasia with chronic mucus production. Lymphedema treatment may involve low-stretch bandages and elastic compression garments combined with skin care, exercises and manual lymph drainage as needed 2.
In some cases, yellow nail syndrome goes away on its own or when an underlying, associated condition is treated 2.
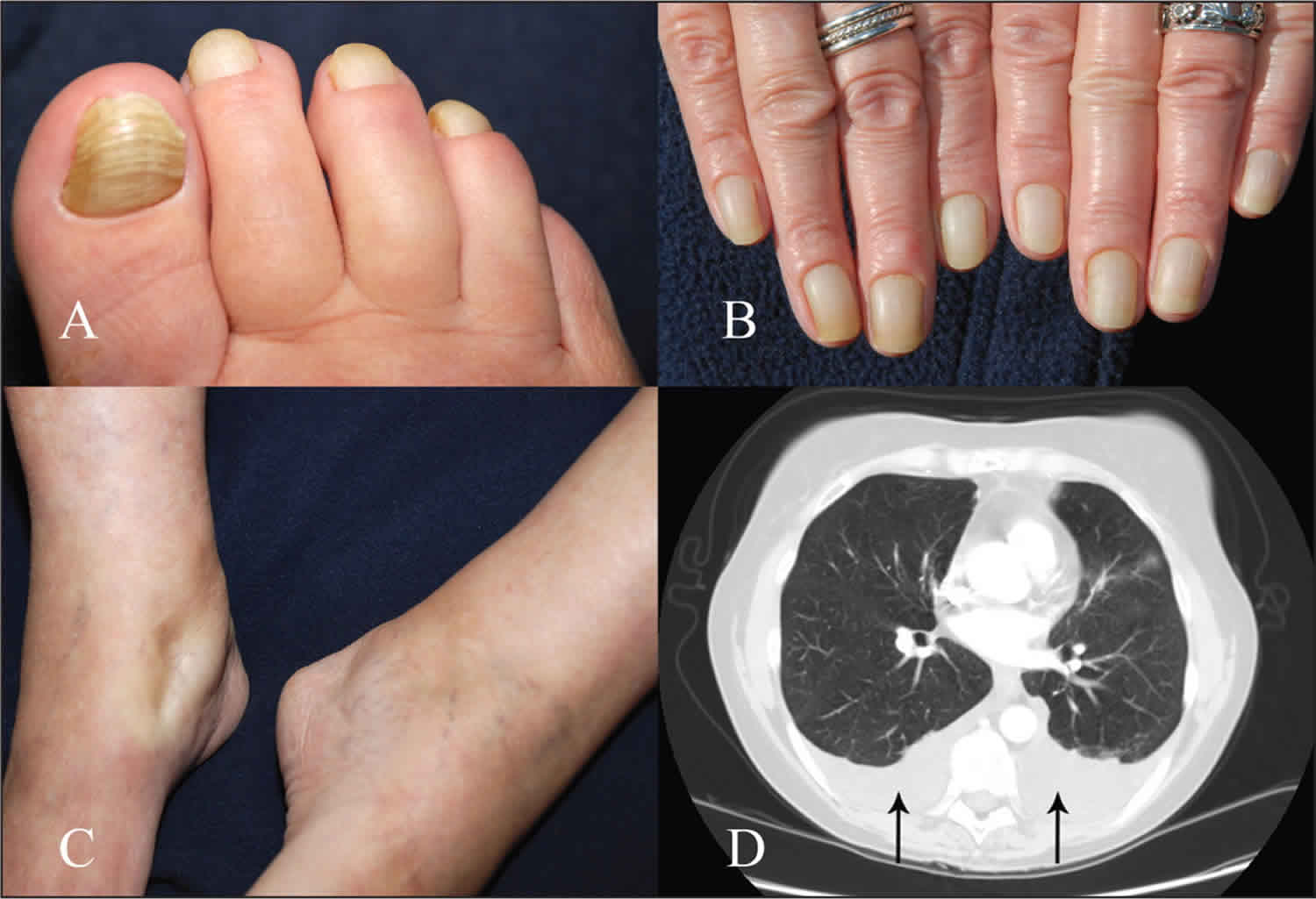
Figure 1. Yellow nail syndrome
Footnote: The toenails (A) and fingernails (B) of a 58-year-old woman with yellow nail syndrome. All nails are brownish yellow, thickened and curved sideways with transverse ridging. (C) Pitting edema of the patient’s ankles. (D) A contrast-enhanced computed tomography scan of the chest shows bilateral pleural effusions (arrows).
[Source 3 ]How is yellow nail syndrome treated?
Yellow nail syndrome management aims to address each of the symptoms. Treatment for nail discoloration may include oral vitamin E and/or triazole antifungals. Pleural effusion may be treated with surgery. Antibiotic prophylaxis may be prescribed for bronchiectasia with chronic mucus production. Lymphedema treatment may involve low-stretch bandages and elastic compression garments combined with skin care, exercises and manual lymph drainage as needed 2.
In some cases, yellow nail syndrome goes away on its own or when an underlying, associated condition is treated 2.
What lung conditions are commonly associated with yellow nail syndrome?
Lung conditions commonly associated with yellow nail syndrome, include 4:
- Pleural effusions
- Recurrent attack of bronchitis
- Chronic sinusitis
- Recurrent pneumonia
Has a genetic cause of familial yellow nail syndrome been discovered?
The exact cause of yellow nail syndrome remains unclear. There have been reports of several members in the same family being affected with this condition and also reports of children being affected at young ages. These reports have been used to suggest the possibility a genetic component to yellow nail syndrome 5. However, the possibility of a genetic cause for yellow nail syndrome remains a subject of debate, as most cases of yellow nail syndrome occur by chance in individuals who do not have a family history of this condition 6. Unfortunately, because there are so few cases of familial yellow nail syndrome, there is limited information and currently no known research about possible genetic causes.
Yellow nail syndrome causes
The exact cause of yellow nail syndrome is unknown. Most cases seem to occur randomly, for no apparent reason (sporadically). Some researchers believe that yellow nail syndrome is a sporadic, acquired condition. However, some sources in the medical literature currently classify yellow nail syndrome as a primary genetic disorder.
Some cases of yellow nail syndrome have run in families suggesting that, in these cases, genetic factors may play a role in the development of the disorder. Some researchers have speculated that yellow nail syndrome is inherited in an autosomal dominant pattern, although the evidence for this remains scarce. Dominant genetic disorders occur when only a single copy of an abnormal gene is necessary for the appearance of the disease. The abnormal gene can be inherited from either parent, or can be the result of a new mutation (gene change) in the affected individual. The risk of passing the abnormal gene from affected parent to offspring is 50 percent for each pregnancy. The risk is the same for males and females.
Some reports in the medical literature have linked some cases of yellow nail syndrome to mutations of the FOXC2 gene. This gene is known to cause a similar disorder called lymphedema-distichiasis syndrome. Some researchers believe that the only primary lymphedema disorder caused by mutation of this gene is lymphedema-distichiasis syndrome and that individuals with yellow nail syndrome linked to this gene may have been misdiagnosed.
Yellow nail syndrome has occurred with greater frequency than would be expected in individuals with certain forms of cancer, immunodeficiency syndromes, nephrotic syndrome, thyroid disease, and rheumatoid arthritis. In individuals with rheumatoid arthritis and yellow nail syndrome, researchers believe certain drugs used to treat the arthritis (thiol drugs) play a role in the development of yellow nail syndrome. Recent reports have suggested the possibility of titanium toxicity as a potential cause of the syndrome, prompting some physicians to recommend removal of titanium prostheses or dental implants on occasions. It should be emphasized that due to the rarity of the syndrome, this association remains entirely speculative. In addition, symptoms do not seem to improve significantly after removal. Accordingly, removal of titanium-based medical devices cannot be recommended.
Many of the symptoms of yellow nail syndrome are commonly associated with malfunction of the lymphatic system including yellow nails, lymphedema, and breathing (respiratory abnormalities). The lymphatic system is a circulatory network of vessels, ducts, and nodes that filter and distribute certain protein-rich fluid (lymph) and blood cells throughout the body. Researchers believe that in yellow nail syndrome, lymphatic fluid collects in the soft tissues in and under the skin (subcutaneous) due to obstruction, malformation, or underdevelopment (hypoplasia) of various lymphatic vessels. Researchers have also speculated that abnormal of leakage of fluid through very tiny vessels (microvascular permeability) may also contribute to the development of lymphedema in yellow nail syndrome.
Yellow nail syndrome symptoms
Yellow nail syndrome most often starts in middle age, although a similar condition has been described in younger children.
The yellow nail syndrome triad are described in the following table.
| Feature | Characteristics |
|---|---|
| Nail changes |
|
| Lymphoedema |
|
| Respiratory signs |
|
The characteristic finding associated with yellow nail syndrome is the development of yellow, thickened, and excessively curved nails with almost complete stoppage of nail growth. Loss of the strip of hardened skin at the base and sides of a fingernail (cuticles) may also occur. Separation of the nails from the nail bed (onycholysis) may cause the nails to fall out. Some individuals may develop infection of the soft tissue around edge of the nails (paronychia). Any nail (both toenails and fingernails) may be affected. Unlike the nails in similar, related disorders, the nails of individuals with yellow nail syndrome generally remain clear (translucent) and smooth as opposed to not transparent (opaque) and rough.
Yellow nail syndrome is occasionally associated with the accumulation of fluid in the membranes surrounding the lungs and lining the chest cavity (pleural effusion). Pleural effusions can cause shortness of breath, chest pain and a cough. Additional respiratory problems may occur in yellow nail syndrome such as chronic infection and inflammation of the main air passages (bronchial tubes) out of the lungs (bronchitis), destruction and widening of the small air passages out of the lung (bronchiectasis), ongoing inflammation of the membranes that line the sinus cavities (sinusitis) and/or chronic inflammation or infection of the lungs (recurrent pneumonias). Individuals with yellow nail syndrome may have a history of respiratory problems before developing characteristic nail findings.
Individuals with yellow nail syndrome often have swelling of the arms and legs due to the accumulation of a fluid known as lymph (peripheral lymphedema). The legs are especially affected in yellow nail syndrome. The onset of lymphedema may occur around puberty. Areas affected by lymphedema may feel heavy or tight. Decreased flexibility may develop in the hands, feet, wrists or ankles if lymphedema is present in the corresponding arm or leg. The skin on areas affected by lymphedema may become hardened or thickened.
Yellow nail syndrome diagnosis
A diagnosis of yellow nail syndrome is made based upon a thorough clinical evaluation, a detailed patient history and identification of characteristic findings. The nail changes in yellow nail syndrome are distinct from the nail changes that occur in most other lymphedema syndromes.
Yellow nail syndrome treatment
The treatment of yellow nail syndrome is geared toward the symptoms present in each individual. Treatment may include antibiotic therapy for repeated respiratory infections. The yellowed, malformed nails may improve without therapy. In some cases, the changes may be permanent. Topical vitamin E solution and oral itraconazole have been used to treat nail changes. Itraconazole and fluconazole are oral antifungal agents. It has been noted that they appear to speed up the rate of growth of nails, which may be of benefit in yellow nail syndrome even though it is not caused by fungal infection. Some studies have shown that nutritional supplementation with vitamin E appears to be effective in controlling yellow nail syndrome, for unknown reasons. Zinc supplements have also been used but it is unclear whether they are effective.
Corticosteroids have also been used to treat individuals with yellow nail syndrome. Surgical management of respiratory problems such as pleural effusions has been used in some cases. Removal of titanium prostheses or dental implants is not recommended, as the evidence for a causal relationship between titanium and yellow nail syndrome is at best speculative, and symptoms do not appear dramatically improved after these interventions.
Genetic counseling may be helpful for affected individuals and their families. Other treatment is symptomatic and supportive.
Yellow nail syndrome prognosis
The long-term outcome for yellow nail syndrome is variable and related to the type and severity of associated conditions. Yellow nail syndrome is associated with reduced survival compared with the general population, and remissions and relapses can occur 3. Treatment is symptomatic 7.
- Yellow Nail syndrome. https://rarediseases.org/rare-diseases/yellow-nail-syndrome[↩][↩]
- Vignes, S., Baran, R. Yellow nail syndrome: a review. Orphanet J Rare Dis 12, 42 (2017). https://doi.org/10.1186/s13023-017-0594-4[↩][↩][↩][↩][↩][↩][↩]
- Yellow nail syndrome. CMAJ October 27, 2009 181 (9) 614; https://doi.org/10.1503/cmaj.080255[↩][↩]
- Yellow nail syndrome. https://dermnetnz.org/topics/yellow-nail-syndrome/[↩]
- Nanda A, Al-Essa FH, El-Shafei WM, Alsaleh QA. Congenital yellow nail syndrome: a case report and its relationship to nonimmune fetal hydrops. Pediatric Dermatology. 2010; 27:533-534. http://www.ncbi.nlm.nih.gov/pubmed/20807364[↩]
- Maldonado F, Ryu JH. Yellow Nail Syndrome. Current Opinions in Pulmonary Medicine. 2009; 15:371-375. http://www.ncbi.nlm.nih.gov/pubmed/19373089[↩]
- Maldonado F, Tazelaar HD, Wang CW, et al. Yellow nail syndrome: analysis of 41 consecutive patients. Chest 2008;134:375–81.[↩]