What is Zygoma
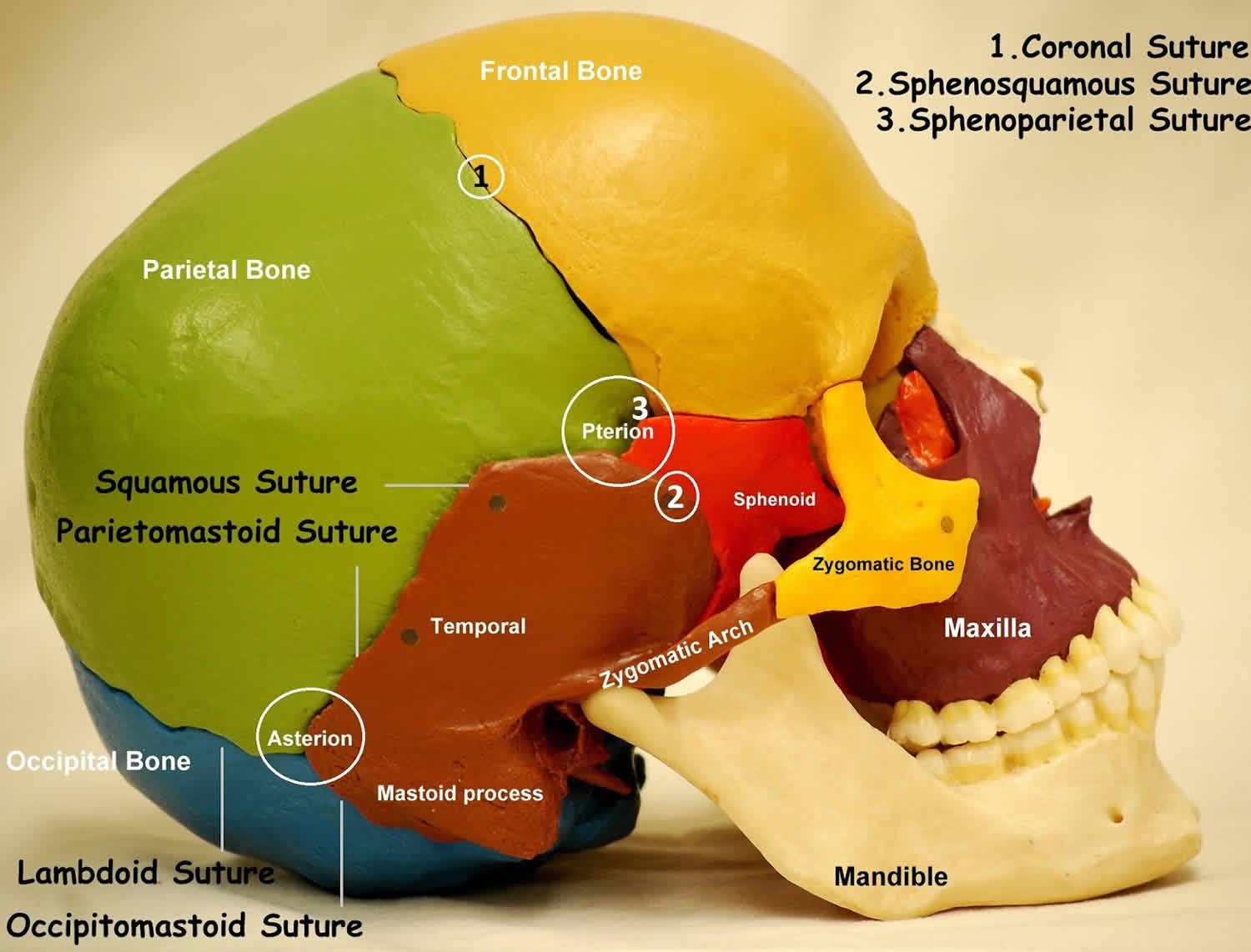
Zygoma or the irregularly shaped zygomatic bones are commonly called the cheekbones. The zygomatic bones form the prominences of the cheeks and define part of the margin of each orbit. The zygoma forms a significant portion of the floor and lateral wall of the orbit and forms a portion of the zygomatic arch, otherwise known as the malar eminence, which plays a key role in the determination of facial morphology. Each joins the zygomatic process of a temporal bone posteriorly, the zygomatic process of the frontal bone superiorly, and the zygomatic process of the maxilla anteriorly (Figure 1).
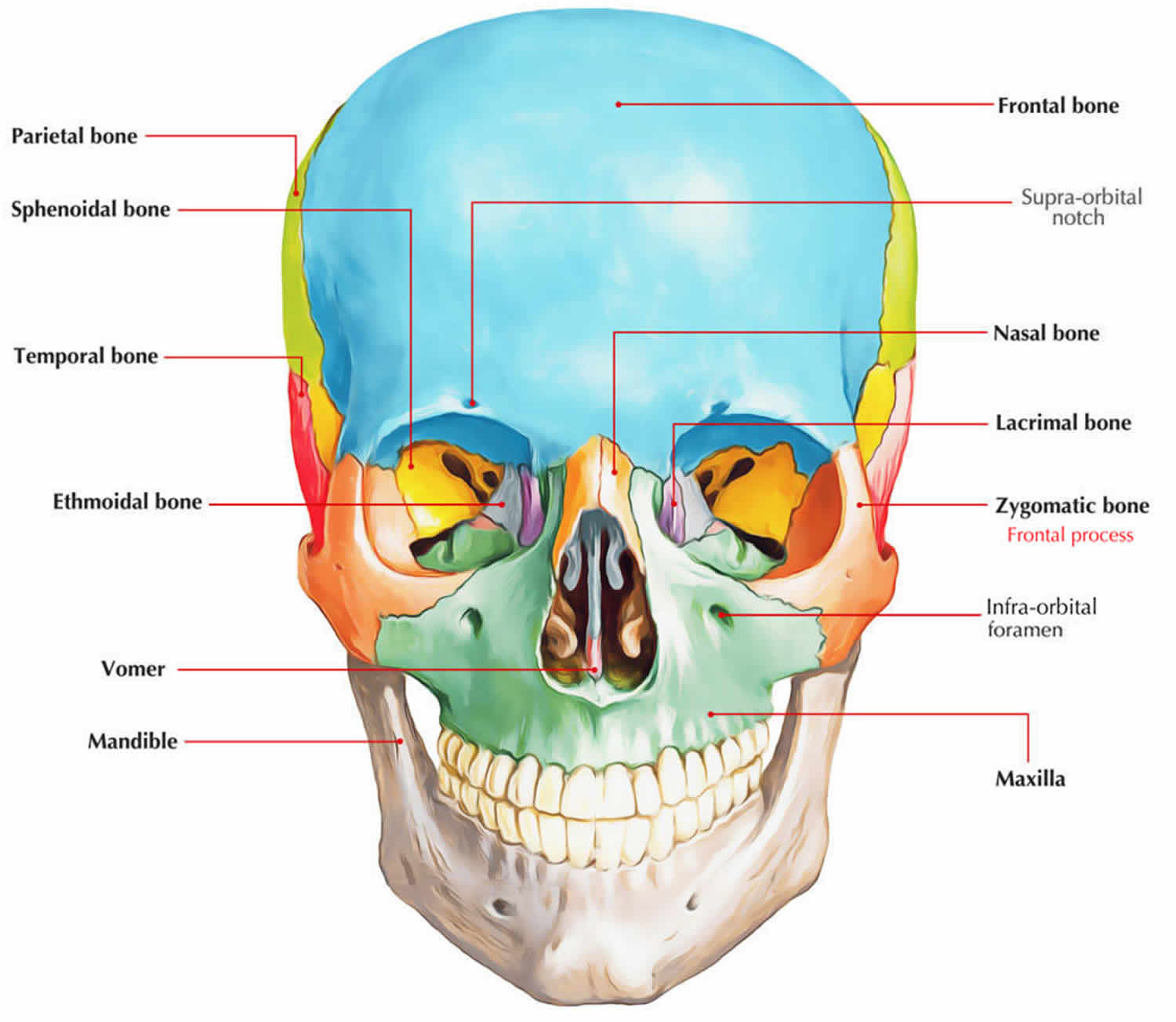
Fourteen facial bones form the face: two nasal bones, two maxillae (or maxillas), two zygomatic bones, the mandible, two lacrimal bones, two palatine bones, two inferior nasal conchae, and the vomer. The zygoma and maxilla play an important role in the facial contour for both cosmetic and functional reasons and their symmetry is cosmetically important; therefore zygomatic bone injuries should be properly diagnosed and adequately treated.
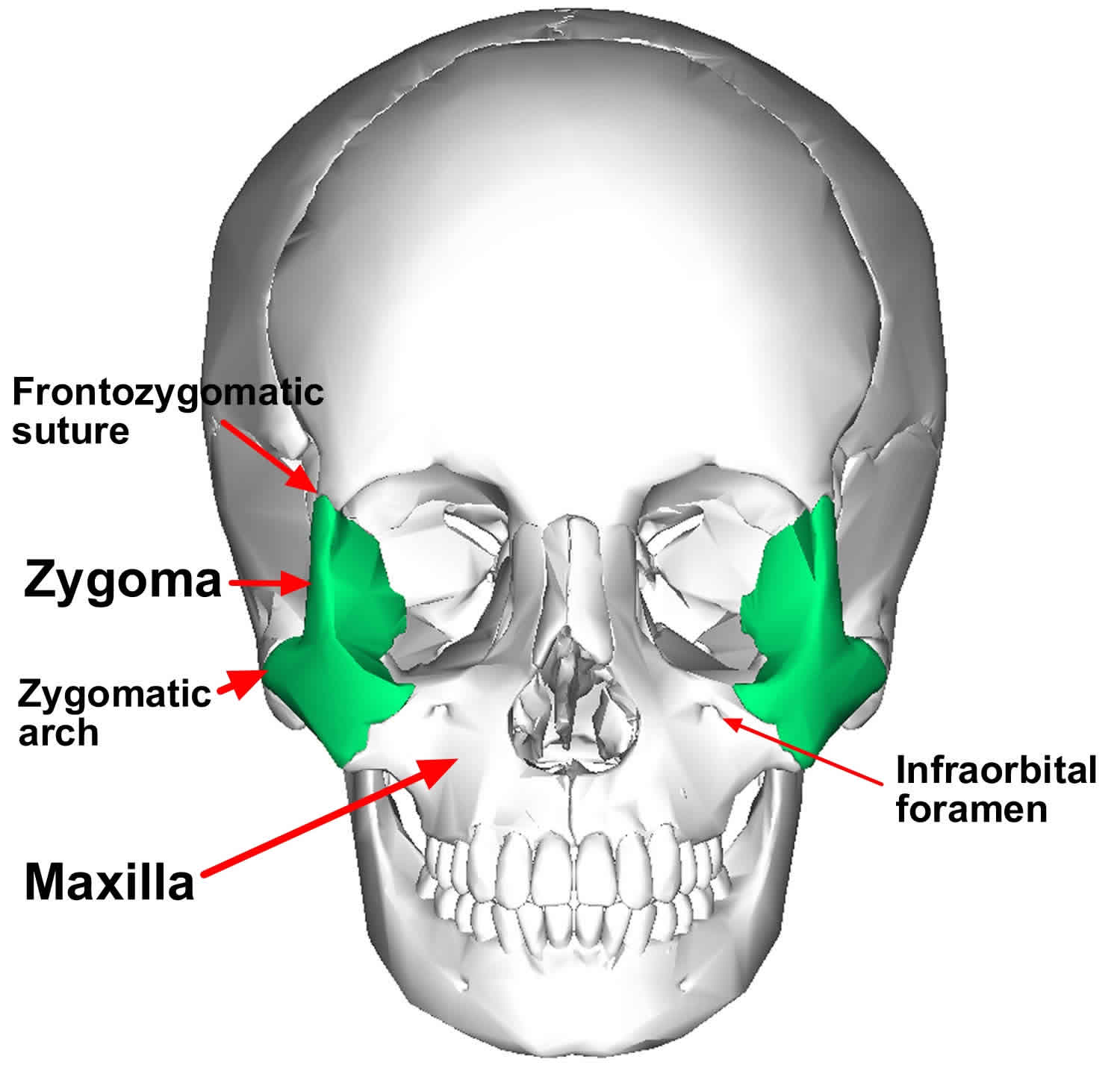
From a frontal view, the zygoma can be seen to articulate with 3 bones: medially by the maxilla, superiorly by the frontal bone, and posteriorly by the greater wing of the sphenoid bone within the orbit (see Figures 1 and 2). From a lateral view, you clearly can see the temporal process of the zygoma join the zygomatic process of the temporal bone to form the zygomatic arch (Figure 3). Attached to the zygoma anteriorly are the zygomaticus minor and major muscles, as well as part of the orbicularis oculi muscle. Laterally, the masseter muscle from below attaches to the zygomatic arch and produces displacing forces on the zygoma.
Anatomically, the zygomatic bone contains foramina that allow for the passage of the zygomaticofacial and zygomaticotemporal arteries and corresponding nerves of the second division of the trigeminal nerve that supply sensation to cheek and anterior temple. Similarly, the infraorbital nerve courses the floor of the orbit and exits the infraorbital foramen or notch. Consequently, fractures of the zygomatic arch can lead to hypoesthesia in the corresponding dermatome. Muscle attachments along the zygomatic arch include the origin of the masseter, the zygomaticus major, and some fibers of the temporalis fascia. The Whitnall tubercle, which serves a critical role in the maintenance of eyelid contour as the attachment site for the lateral canthal tendon, is located on the zygomatic bone 2 mm behind the lateral orbital rim 1.
Figure 1. Zygoma
Figure 2. Zygomatic bones
Zygoma reduction
Many surgical approaches have been introduced for the reduction of zygomatic complex fractures, including the intraoral (Keen), temporal (Gillies), brow incision, and bicoronal approaches 2. Fractures of the zygomatic complex occur because of the rotation of the zygoma associated with the disarticulation of the zygomatic bone at the zygomaticofrontal suture (along the lateral orbital rim), the zygomaticomaxillary suture (medially), and along the zygomatic arch to the temporal bone (see below) 3.
The zygoma is the main buttress between the maxilla and the skull, but, in spite of its sturdiness, its prominent location makes it prone to fracture. The mechanism of injury usually involves a blow to the side of the face from a fist, from an object, or secondary to motor vehicle accidents. Moderate force may result in minimally or nondisplaced fractures at the suture lines. More severe blows frequently result in inferior, medial, and posterior displacement of the zygoma. Comminuted fractures of the body with separation at the suture lines are most often the result of high-velocity motor vehicle accidents. Patients with zygomatic fractures frequently have associated ophthalmic injuries, especially in the setting of combined zygomatic and orbital floor fractures 4.
Most cases of zygomatic complex fractures occur in young patients in their second to third decades of life, with the exception of fractures due to accidental falls, which are mainly seen in older patients 5.
In the United States, zygomatic fractures are the second most common fracture of the facial bones following nasal bone fractures 6. Studies from countries outside the United States found zygomatic complex fractures to be the most common fracture site in patients with maxillofacial trauma 7.
In general, displaced fractures involve the inferior orbital rim and orbital floor, the zygomaticofrontal suture, the zygomaticomaxillary buttress, and the zygomatic arch. However, occasionally, a direct blow to the arch results in an isolated depressed fracture of the arch only 1. Displaced zygoma fractures can lead to changes in globe position and facial contour if not properly realigned. Associated ophthalmic and intracranial injuries may occur and may carry separate prognostic considerations.
Manson and colleagues have proposed a more modern classification system in which CT scan is used to assess and classify zygomatic fractures 8. CT provides information about facial structures, including both bone segmentation and displacement, allowing for complete repair of the fractures. This system divides fractures into low-energy, medium-energy, and high-energy injuries.
Low-energy zygoma fractures result in minimal or no displacement. These types of fractures often are seen at the zygomaticofrontal suture, and inherent stability usually obviates reduction.
Middle-energy zygoma fractures result in fractures of all buttresses, mild-to-moderate displacement, and comminution. Often, an eyelid and intraoral exposure is necessary for adequate reduction and fixation.
High-energy zygoma fractures frequently occur with Le Fort or panfacial fractures. The zygomatic fractures often extend through the glenoid fossa and permit extensive posterior dislocation of the arch and malar eminence. A coronal exposure, in addition to the oral and eyelid incisions, usually is necessary to properly reposition the malar eminence.
The literature indicates that 10-50% of all zygomaticomaxillary complex fractures require no surgical intervention 9. This is suitable for zygoma fractures that are nondisplaced or minimally displaced or where systemic status precludes operative intervention.
Stable, nondisplaced fractures may be observed weekly for healing.
Avoidance of nose blowing is mandatory in the medical care of these patients. It is essential to instruct patients to avoid forceful nose blowing. The disrupted orbital walls can allow air to be forced into the retrobulbar space, causing orbital emphysema, which may lead to pain and visual loss. Advise patients to call the surgeon at any time if orbital bleeding is suspected.
Intermittent application of ice packs to the area of the fracture in the first 3-4 days after injury may aid in alleviating pain and edema.
The routine use of systemic antibiotics for isolated zygomatic arch fractures generally is not recommended.
Indicators of favorable outcome include bony union, absence of skeletal or soft tissue deformity, and a normal range of mandibular movement.
Generally, it is suggested to avoid surgery during times of maximum edema but prior to the adhesion of displaced bony fragments and scarring of soft tissues into bony defects. Most surgeons advise surgical intervention prior to the formation of dense scar tissue. As a general guideline, surgery should be undertaken within 3 weeks from the time of injury 10.
The treatment of zygomatic complex fractures is frequently a challenge for plastic surgeons 2. Traditionally, closed-reduction techniques were the method of choice for nearly all zygomatic fractures. In the past, simple techniques, such as exerting pressure under the zygomatic arch and resetting the bones in their anatomic position (eg, Gilles approach), were hindered by unsatisfactory cosmetic results and persistent diplopia. Although open techniques currently are favored, closed-reduction techniques may be suitable for isolated arch fractures and minimally displaced noncomminuted fractures 11. A more aggressive approach using open-reduction techniques and rigid stabilization with plating systems (eg, Synthes or Leibinger) is the standard of care today, particularly for unstable or potentially unstable fractures 12. This approach provides direct access to the frontozygomatic suture, orbital floor, and infraorbital rims.
Many surgical approaches have been introduced for the reduction of zygomatic complex fractures, including the intraoral (Keen), temporal (Gillies), brow incision, and bicoronal approaches 13. The generally preferred approach consists of three incisions, including lateral brow and intraoral incisions 2. Although the subciliary incision, lateral brow incision, bicoronal approaches provide good exposure and direct visualization, they leave conspicuous external scars on the face. The temporal approach leaves no facial scars, but it cannot provide direct visualization, which may result in incomplete surgical reduction 13.
The intraoral approach also has the advantages of leaving no facial scars and being simple to use. Limited reductions are popular today; for example, the intraoral approach alone can be used for about 50% to 75% of all zygomatic complex fractures 14. This type of limited approach can be used for fractures that are greensticked or minimal at the zygomaticofrontal suture, or include a minimal or linear orbital floor fracture that can be repaired by zygoma reduction. In most cases, however, one cannot fully assess the degree of reduction based on the intraoral approach alone, and further exposure is indicated 15.
The orbital floor and rim are usually approached by a subciliary or infrapalpebral incision 13. However, these incisions leave a visible scar and have a risk of lower eyelid deformity. In particular, a subciliary incision can injure the orbicularis oculi muscle of the lower lid and decrease pretarsal fullness or cause aesthetically unfavorable results, such as lower eyelid retraction, both transient and permanent 16.
The extended transconjunctival approach is usually used in ophthalmology, and little information is available about treating zygoma complex fractures using the extended transconjunctival approach approach; as such, its technical details and limitations are not well defined 17. Lee et al. 18 reported 53 cases treated using the transconjunctival approach with a lateral canthal incision and 2-point fixations in all cases.
Postoperative complications include ectropion, epiphora 19, plate exposure, and wound infections, potentially requiring removal of implanted material 20. Case reports have also described postoperative orbital hemorrhage, which can lead to permanent blindness in the affected eye 21.
- Zingg M, Laedrach K, Chen J, et al. Classification and treatment of zygomatic fractures: a review of 1,025 cases. J Oral Maxillofac Surg. 1992 Aug. 50(8):778-90[↩][↩]
- Song SH, Kwon H, Oh SH, Kim SJ, Park J, Kim SI. Open reduction of zygoma fractures with the extended transconjunctival approach and T-bar screw reduction. Arch Plast Surg. 2018;45(4):325–332. doi:10.5999/aps.2018.00311 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6062705[↩][↩][↩]
- Song WC, Choi HG, Kim SH, et al. Topographic anatomy of the zygomatic arch and temporal fossa: A cadaveric study. J Plast Reconstr Aesthet Surg. 2008 Oct 21.[↩]
- Michelet FX, Deymes J, Dessus B. Osteosynthesis with miniaturized screwed plates in maxillo-facial surgery. J Maxillofac Surg. 1973 Jun. 1(2):79-84[↩]
- Manson PN, Markowitz B, Mirvis S, et al. Toward CT-based facial fracture treatment. Plast Reconstr Surg. 1990 Feb. 85(2):202-12; discussion 213-4.[↩]
- Covington DS, Wainwright DJ, Teichgraeber JF, et al. Changing patterns in the epidemiology and treatment of zygoma fractures: 10-year review. J Trauma. 1994 Aug. 37(2):243-8.[↩]
- Rallis G, Stathopoulos P, Igoumenakis D, Krasadakis C, Mourouzis C, Mezitis M. Treating maxillofacial trauma for over half a century: how can we interpret the changing patterns in etiology and management?. Oral Surg Oral Med Oral Pathol Oral Radiol. 2015 Jun. 119 (6):614-8.[↩]
- Septa D, Newaskar VP, Agrawal D, Tibra S. Etiology, incidence and patterns of mid-face fractures and associated ocular injuries. J Maxillofac Oral Surg. 2014 Jun. 13 (2):115-9.[↩]
- Salentijn EG, Boffano P, Boverhoff J, van den Bergh B, Forouzanfar T. The epidemiological characteristics of zygomatic complex fractures: A comparison between the surgically and non-surgically treated patients. Natl J Maxillofac Surg. 2013 Jul. 4 (2):214-8.[↩]
- Randall DA, Bernstein PE. Epistaxis balloon catheter stabilization of zygomatic arch fractures. Ann Otol Rhinol Laryngol. 1996 Jan. 105(1):68-9.[↩]
- af Geijerstam B, Hultman G, Bergstrom J, et al. Zygomatic fractures managed by closed reduction: an analysis with postoperative computed tomography follow-up evaluating the degree of reduction and remaining dislocation. J Oral Maxillofac Surg. 2008 Nov. 66(11):2302-7.[↩]
- Smyth AG. A modified miniplate for use in malar complex fractures. Br J Oral Maxillofac Surg. 1995 Jun. 33(3):169-70[↩]
- Lee PK, Lee JH, Choi YS, et al. Single transconjunctival incision and two-point fixation for the treatment of noncomminuted zygomatic complex fracture. J Korean Med Sci. 2006;21:1080–5.[↩][↩][↩]
- Rodriguez ED, Dorafshar AH, Manson PN. Facial fraactures. In: Neligan PC, editor. Plastic surgery. 3rd ed. Vol. 3. Philadelphia: Saunders Elsevier; 2013. pp. 49–88[↩]
- Kaufman Y, Stal D, Cole P, et al. Orbitozygomatic fracture management. Plast Reconstr Surg. 2008;121:1370–4.[↩]
- Werther JR. Cutaneous approaches to the lower lid and orbit. J Oral Maxillofac Surg. 1998;56:60–5.[↩]
- Chang EL, Hatton MP, Bernardino CR, et al. Simplified repair of zygomatic fractures through a transconjunctival approach. Ophthalmology. 2005;112:1302–9.[↩]
- Lee PK, Lee JH, Choi YS, et al. Single transconjunctival incision and two-point fixation for the treatment of noncomminuted zygomatic complex fracture. J Korean Med Sci. 2006;21:1080–5[↩]
- Knight JS, North JF. The classification of malar fractures: An analysis of displacement as a guide to treatment. Br J Plast Surg. 1961. 13:325.[↩]
- Pozatek ZW, Kaban LB, Guralnick WC. Fractures of the zygomatic complex: an evaluation of surgical management with special emphasis on the eyebrow approach. J Oral Surg. 1973 Feb. 31(2):141-8.[↩]
- Lund K. Fractures of the zygoma: a follow-up study on 62 patients. J Oral Surg. 1971 Aug. 29(8):557-60.[↩]