Gingival hypertrophy
Gingival hypertrophy also known as gingival hyperplasia, gum hypertrophy or gingival enlargement, refers to excessive growth of the gums or gingiva around the necks of the teeth. The hypertrophic gingival tissue may be inflamed (gingivitis), in which case the gums are red, soft, shiny and bleed easily.
Gingival overgrowth can be caused by several mechanisms but will have very similar appearances. A study in the journal histopathology describes the condition as “a small papillary or velvety bright red gingival overgrowth that bleeds easily.” However, the overgrowth can be extensive and round in appearance. It is usually found on the front of the teeth and can be on the tongue side in some cases.
One of the causes is inflammation. The inflammation can be induced by poor oral hygiene or from a dental appliance like orthodontic braces. Other factors include systemic conditions like hormonal imbalances or leukemia, medications or heredity conditions. Also, localized overgrowth can be a benign or malignant lesion.
Once gingival hypertrophy has started, it is difficult to maintain good oral hygiene. Poor oral hygiene also can increase inflammation that can be a factor in gum hypertrophy. If you think you have an area of gum hypertrophy, visit your dentist for an evaluation of your condition. If you are now taking medications that can cause overgrowth consult your physician and dentist.
In general, your ability to practice effective oral hygiene measures on a daily basis helps to reduce the risk of developing gingival enlargement. Your dentist is available to monitor your oral hygiene measures and assist you as necessary. For example, you may need to undergo more frequent professional cleanings or may be instructed on ways to improve your brushing technique. Effective oral hygiene is especially important for managing gum hypertrophy caused by chronic inflammation and cyclosporine. For medication-induced gingival enlargement, your physician may be able to substitute the medication to reduce your risk of developing gingival enlargement. For gingival enlargement associated with a systemic condition, management of the underlying systemic condition usually results in partial or complete resolution of gingival enlargement.
Figure 1. Inflammatory-induced gingival hypertrophy
Figure 2. Drug-induced gum hypertrophy
Is gingival hypertrophy associated with the dose of my medication?
The dose of the medication appears to be less of an issue than having good oral hygiene (less plaque present on your teeth).
Is gingival hypertrophy contagious?
No, gum hypertrophy are not infectious. You did not catch it from anyone and cannot pass it on.
Gingival hypertrophy causes
There are several causes of gingival enlargement and they can be grouped into four categories: 1) inflammatory gingival enlargement, 2) medication-induced gingival enlargement, 3) hereditary gingival fibromatosis, and 4) systemic causes of gingival enlargement. In many gum hypertrophy cases the cause is unknown.
Specific causes of gingivitis include:
- Poor dental hygiene resulting in bacterial plaque, gingivitis and periodontitis
- Smoking, mouth breathing and overcrowded teeth
- Systemic diseases especially diabetes, HIV infection
Inflammatory gingival hypertrophy
The gingival enlargement observed may be localized or generalized and is an inflammatory response that occurs when plaque (collection of food debris and bacteria) accumulates on the teeth. This is a result of the patient not accomplishing effective oral hygiene. An example is noted to the right. Gums affected by this condition are often tender, soft, red, and bleed easily. Fortunately, this condition usually resolves with effective oral hygiene practices (tooth brushing, flossing) to remove the plaque and irritants on the teeth.
Medication-induced gingival hypertrophy
Patients who take certain medications may develop gingival enlargement. In contrast to inflammatory gingival enlargement, the gum tissues in such cases are typically firm, non-tender, pale pink in color, and do not bleed easily. In severe cases, the gingiva may completely cover the crowns of the teeth causing periodontal (gum) disease (due to difficulty in keeping the teeth clean) as well as problems with tooth eruption and alignment. Medication-induced gingival enlargement may resolve either partially or completely when the medication is discontinued. If the medication cannot be discontinued, surgical removal of the excess gingiva (gingivectomy) may be performed but the condition will likely recur. As this condition is somewhat worsen by the level of plaque accumulation on the teeth, effective oral hygiene measures will reduce the severity.
Hereditary gingival fibromatosis
Hereditary gingival fibromatosis is a rare hereditary condition that usually develops during childhood, although some cases may not become evident until adulthood. The condition presents as a slowgrowing generalized or occasionally localized non-tender, firm, pale pink enlargement of the gingival. Surgical removal of excess gingival is often necessary to avoid impaction and displacement of teeth. Repeated surgical removals may be required because of the recurrent nature of this condition.
Non-inflamed gingival hypertrophy tends to be a darker red or purple. It may be soft, which bleeds easily, or firm and fibrous. It is also more likely to occur in those with poor dental hygiene. Causes include:
- Hormonal states: pregnancy, puberty;
- Nutritional deficiency: scurvy (vitamin C deficiency);
- Medications, most often ciclosporin, phenytoin and other anticonvulsants, calcium channel blockers. Uncommonly, it may be due to antibiotics, antidepressants and other medications.
- Genetic conditions, often present at birth (all rare conditions): hereditary fibromatosis, I-cell disease, mucopolysaccharidoses, fucosidosis, aspartyl glycosaminuria, Pfeiffer syndrome, infantile systemic hyalinosis and primary amyloidosis. Localised gingival enlargement may be seen in Fabry disease, Cowden syndrome, tuberous sclerosis, Sturge-Weber angiomatosis and gingival granular cell tumour.
- Blood conditions such as acute leukaemia, lymphoma or aplastic anaemia;
- Systemic diseases most often granulomatosis with polyangiitis, sarcoidosis, Crohn disease, Type 1 neurofibromatosis, primary amyloidosis, Kaposi sarcoma and acromegaly.
Systemic causes of gum hypertrophy
There are numerous physiologic and systemic conditions that may promote localized and/or generalized gingival enlargement such as pregnancy, hormonal imbalances, and leukemia. Gingival enlargement associated with systemic conditions usually resolves when the underlying condition is treated or in the case of pregnancy, delivery of the child. As with medication-induced gingival enlargement, effective oral hygiene measures will reduce the risk of developing gingival enlargement.
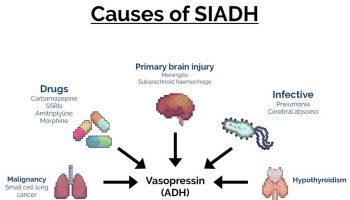
Drugs causing gum hypertrophy
Drugs are the commonest reason behind gum hypertrophy 1. Drug-induced gingival overgrowth also called drug-induced gingival enlargement, was previously referred to as drug-induced gingival hyperplasia. It is a noted side-effect of certain drugs given for non-dental uses where the gingival tissue is not the intended target organ. The drugs that cause gum hypertrophy are mainly the anticonvulsants, immunosuppressants, and the calcium channel blockers 2. Studies have shown that it is more commonly seen in male children and adolescents. Genetic heterogeneity also plays a vital role and the extent and the degree of overgrowth depends on the drugs 1. Hereditary gingival fibromatosis is the most common type of gingival enlargement seen in children usually seen during the eruption of the permanent dentition. Neurofibromatosis type 1 causes plexiform neurofibromas in the connective tissue in the gingiva and is most commonly seen in mentally handicapped patients. This type of gingival overgrowth consists of hypertrophic nerves arranged in a lobulated form in the connective tissue of the gingiva 3.
This is of great importance as gingival overgrowth impedes proper dental hygiene and apart from the cosmetic disfigurement, causes painful chewing and eating.
Anticonvulsants
Phenytoin (5,5-diphenylhydantoin), sodium valproate, phenobarbitone, vigabatrin, primidone, mephenytoin, and ethosuximide are some of the drugs that cause gingival hypertrophy 1. At times, multiple drugs are given together which could act synergistically and aggravate the condition. Drugs like phenytoin, phenobarbitone, and primidone are metabolized to 5-(4-hydroxyphenyl)5-phenyl hydantoin(4-HPPH) which is responsible for the overgrowth of gingival tissue.
Immunosuppressants
Cyclosporin, tacrolimus, and sirolimus are some of the immunosuppressants that cause gingival hypertrophy. The commonest one is Cyclosporin, the indications for use being autoimmune diseases and after organ transplantation like post renal transplants 4. Highly toxic, one study found the incidence of gingival overgrowth apart from other side effects to be nearly 53% in patients of renal transplant on cyclosporin 5. Tacrolimus is another immunosuppressant sometimes used in place of cyclosporin. It is less toxic than cyclosporin, causing less hepatotoxicity and renal toxicity and less severe gingival overgrowth than cyclosporin 6. Sirolimus is another immunosuppressant that has shown to predispose to gingival hypertrophy 7.
Calcium channel blockers
Calcium channel blockers include nifedipine, nitrendipine, felodipine, amlodipine, nisoldipine, verapamil, and diltiazem. The calcium channel blocker that is most commonly associated with gingival hypertrophy is nifedipine, with a reported incidence of approximately 38% 8. Other agents that have been found to have an association with gingival overgrowth include diltiazem, incidence of 20% 9; verapamil, incidence of 4 to 19% 10; and amlodipine, incidence of 3% 11. Seymour et al. 12 reported the first case of gingival overgrowth attributed to the use of amlodipine in 1994. Lafzi et al 13 reported gingival hypertrophy in patients receiving 10 mg of amlodipine daily within 2 months of onset of treatment. Case reports have indicated that gingival overgrowth can also occur with the use of felodipine 14 and nitrendipine 15.
The indications for use are hypertension, angina pectoris or peripheral vascular disease 4. Renal transplant patients who are on immunosuppressants like cyclosporin show a greater propensity to develop gingival hypertrophy when put on nifedipine or diltiazem, though the extent of hypertrophy is greater with the former 4. Combinations of these drugs could act synergistically, causing exaggerated hypertrophy of gingival tissue.
Gingival hypertrophy differential diagnosis
- False enlargement of gingival tissue: This is pseudo-enlargement of the gingiva, which is actually because of enlarged underlying bony tissue. The gingiva here has no abnormality.
- Inflammation: An abscess presents as a localized painful swelling which is tender. Chronically inflamed gingival tissue is red or violaceous smooth and bleeds on touch.
- Familial or hereditary: The tendency runs in the family. The gingiva is pink, non-tender, involves the attached gingiva, the gingival margin and the interdental papillae, and has a firm and leathery consistency.
- Tumors: These are localized, hard in consistency, wart-like, friable and bleed on touch.
- Physiological states: Puberty and pregnancy are at times associated with gingival enlargement.
- Scurvy: Vitamin C deficiency can produce very tender bleeding gingiva.
- Systemic diseases: Leukemias, tuberculosis, sarcoidosis. Can be corroborated hematologically to confirm the diagnosis.
In all these conditions, a thorough history, physical examination, and investigations including a biopsy may be required to confirm the cause.
Conditions similar to gingival hypertrophy:
- Fibrous epulis/peripheral fibroma
- Angiogranuloma/Pyogenic granuloma
- Gingival cysts
- Neoplasms: They can be benign or malignant. Benign are fibroma, peripheral and central giant cell granuloma, papilloma, leukoplakia, nevus, hemangioma, leukoplakia, nevus, myoblastoma, hemangioma, neurilemoma, neurofibroma, ameloblastoma. Malignant tumors are squamous cell carcinoma, Kaposi’s sarcoma, etc.
- Others like palatal mucocele or lateral periodontal cyst 16
Gingival hypertrophy symptoms
Gum hypertrophy may cause discomfort, interfere with speech or chewing, result in halitosis (bad odor to the breath) and it may look unsightly.
Gingival hypertrophy diagnosis
As there can be several reasons for gingival hypertrophy, it is important to receive the right diagnosis. A biopsy may be necessary to rule out pathological conditions. If the cause is gingival inflammation (gingivitis), then periodontal therapy and improved oral hygiene will be needed. If the cause is a medication, then your physician may need to be consulted. Stopping or changing the medication can help limit the overgrowth, but never stop a medication on your own. Just stopping the medication will not reverse the overgrowth, so additional treatment is usually required.
The patient of gingival enlargement is typically one with hypertension or angina or an epileptic or a renal transplant recipient, on medication from any of the drug-induced gingival overgrowth inducing drugs, reporting with hypertrophy of the gums since a variable period (which is generally a few weeks from the start of medication) and complaining of pain during mastication or cosmetic disfigurement.
Possible findings
- Firm, painless, nodular enlargement of the interdental papilla, limited to the keratinized portions of the gingiva and extending to the facial and lingual gingival margins.
- In severe cases, a huge fold of hypertrophied gingival tissue is observed covering the crowns.
- At times, it appears firm and pale pink with minute lobulations, pouting from underneath the gingival margin, delineated by a groove of tissue which does not bleed on touch.
- If secondary inflammation exists, the gingiva appears smooth, and The enlargement is greater in the maxillary and anterior mandibular regions. Typically, it is not seen in edentulous areas of the gingiva.
The following tests should be done to evaluate this condition:
- A complete blood count (CBC) is indicated in patients with gingival enlargement if there is a presence of profuse gingival bleeding even if it is drug induced to rule out anemia and leukemia.
- Full mouth periapical radiographs or OPG (orthopantomograph) are to be taken before beginning any treatment to rule out periodontal disease or dental disease.
- Candidiasis and other infections must be ruled out by taking a culture.
- Tissue biopsy should be carried out in case the presentation of the disease is unusual.
- A periodontal examination is necessary to evaluate for the presence of periodontal disease.
- The removal of dental plaque maintains oral hygiene.
- Scaling and root planning must be carried out.
Gingival hypertrophy treatment
Gingival hypertrophy treatment depends on treating the underlying cause. Gingivitis may improve with the following measures:
- Removal of bacterial plaque by thorough tooth brushing and flossing
- Antiseptic mouthwashes such as chlorhexidine
- Ultrasonic treatments
- Courses of antibiotics to reduce oral bacterial load (e.g. erythromycin or azithromycin)
Drugs that are known to cause gum hypertrophy should be discontinued or switching over to another drug without the same side-effects can be considered 17. The aim of treatment in drug-induced gingival overgrowth is to alleviate the discomfort and make simple acts like eating and chewing pain-free, to treat the inflammation and reduce the swelling, and also give a better cosmetic appearance to the gingiva.
The modalities of treatment are medical and surgical.
Medical management is the first line of treatment, and surgery is reserved for recurrences or cases that persist despite good medical treatment.
Plaque removal including periodic scaling, tooth surface cleaning 18.
Control of inflammation including non-steroidal anti-inflammatory agents (NSAIDs), antibiotics to control infection and topical application of antifungal medication like nystatin 19.
Folate supplementation to be started.
Surgical treatment is to be considered in patients not responding to medical management, or cases that recur despite adequate plaque control. An adequate period should be allowed to elapse after medical therapy or discontinuation of the inducing drug before surgery is considered.
The surgical methods include traditional scalpel gingivectomy (surgical removal of the overgrown gum tissue) and periodontal flap surgery. Gingivectomy may be repeated if necessary.
Electrocautery may be used in difficult cases, children, or where the gingiva is fragile and likely to bleed.
CO2 Laser has a wavelength of 10600 nm; hence, it is readily absorbed by water and therefore is very effective in surgery of soft tissues with high water content like the gingiva. Blood vessels up to a diameter of 0.5 mm can be sealed effectively and provides a dry field for better visibility of the surgical field. A laser is preferred over the scalpel as it has strong bactericidal and hemostatic effects 20.
References- Tungare S, Paranjpe AG. Drug Induced Gingival Overgrowth (DIGO) [Updated 2020 Aug 27]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2020 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK538518
- Marshall RI, Bartold PM. Medication induced gingival overgrowth. Oral Dis. 1998 Jun;4(2):130-51.
- Doufexi A, Mina M, Ioannidou E. Gingival overgrowth in children: epidemiology, pathogenesis, and complications. A literature review. J. Periodontol. 2005 Jan;76(1):3-10.
- Dongari-Bagtzoglou A., Research, Science and Therapy Committee, American Academy of Periodontology. Drug-associated gingival enlargement. J. Periodontol. 2004 Oct;75(10):1424-31.
- Greenberg KV, Armitage GC, Shiboski CH. Gingival enlargement among renal transplant recipients in the era of new-generation immunosuppressants. J. Periodontol. 2008 Mar;79(3):453-60.
- Sekiguchi RT, Paixão CG, Saraiva L, Romito GA, Pannuti CM, Lotufo RF. Incidence of tacrolimus-induced gingival overgrowth in the absence of calcium channel blockers: a short-term study. J. Clin. Periodontol. 2007 Jul;34(7):545-50.
- Cota LO, Viana MB, Moreira PR, Gomez RS, Cortelli JR, Cortelli SC, Costa FO. Gingival overgrowth in cyclosporine, tacrolimus, or sirolimus-based immunosuppressive regimens and the single nucleotide IL-6 (-174 G/C) gene polymorphism. Arch. Oral Biol. 2010 Jul;55(7):494-501.
- Steele RM, Schuna AA, Schreiber RT. Calcium antagonist-induced gingival hyperplasia. Ann Intern Med. 1994 Apr 15;120(8):663-4. doi: 10.7326/0003-4819-120-8-199404150-00006
- Fattore L, Stablein M, Bredfeldt G, Semla T, Moran M, Doherty-Greenberg JM. Gingival hyperplasia: a side effect of nifedipine and diltiazem. Spec Care Dentist. 1991 May-Jun;11(3):107-9. doi: 10.1111/j.1754-4505.1991.tb00828.x
- Miller CS, Damm DD. Incidence of verapamil-induced gingival hyperplasia in a dental population. J Periodontol. 1992 May;63(5):453-6. doi: 10.1902/jop.1992.63.5.453
- Leknes KN, Lie T, Böe OE, Selvig KA. A correlation study of inflammatory cell mobilization in response to subgingival microbial colonization. J Periodontol. 1997 Jan;68(1):67-72. doi: 10.1902/jop.1997.68.1.67
- Seymour RA, Thomason JM, Ellis JS. The pathogenesis of drug-induced gingival overgrowth. J. Clin. Periodontol. 1996 Mar;23(3 Pt 1):165-75.
- Lafzi A, Farahani RM, Shoja MA. Amlodipine-induced gingival hyperplasia. Med Oral Patol Oral Cir Bucal. 2006 Nov 01;11(6):E480-2.
- Lombardi T, Fiore-Donno G, Belter U & Dl Felice R. Felodipine-induced gingival hyperplasia: a clinical and histologie study. J Oral Pathol Med. 1991; 20: 8992
- Brown RS, Sein P, Corio R, Bottomley WK. Nitrendipine-induced gingival hyperplasia. First case report. Oral Surg Oral Med Oral Pathol. 1990 Nov;70(5):593-6. doi: 10.1016/0030-4220(90)90406-i
- Agrawal AA. Gingival enlargements: Differential diagnosis and review of literature. World J Clin Cases. 2015 Sep 16;3(9):779-88.
- de la Rosa García E, Mondragón Padilla A. [The effect of mycophenolate mofetil and azathioprine on gingival enlargement associated with cyclosporin A use in kidney transplant patients]. Nefrologia. 2009;29(5):474-8.
- Srivastava AK, Kundu D, Bandyopadhyay P, Pal AK. Management of amlodipine-induced gingival enlargement: Series of three cases. J Indian Soc Periodontol. 2010 Oct;14(4):279-81.
- Lu HK, Tseng CC, Lee YH, Li CL, Wang LF. Flutamide inhibits nifedipine- and interleukin-1 beta-induced collagen overproduction in gingival fibroblasts. J. Periodont. Res. 2010 Aug;45(4):451-7.
- Mavrogiannis M, Ellis JS, Thomason JM, Seymour RA. The management of drug-induced gingival overgrowth. J. Clin. Periodontol. 2006 Jun;33(6):434-9.