Acinetobacter
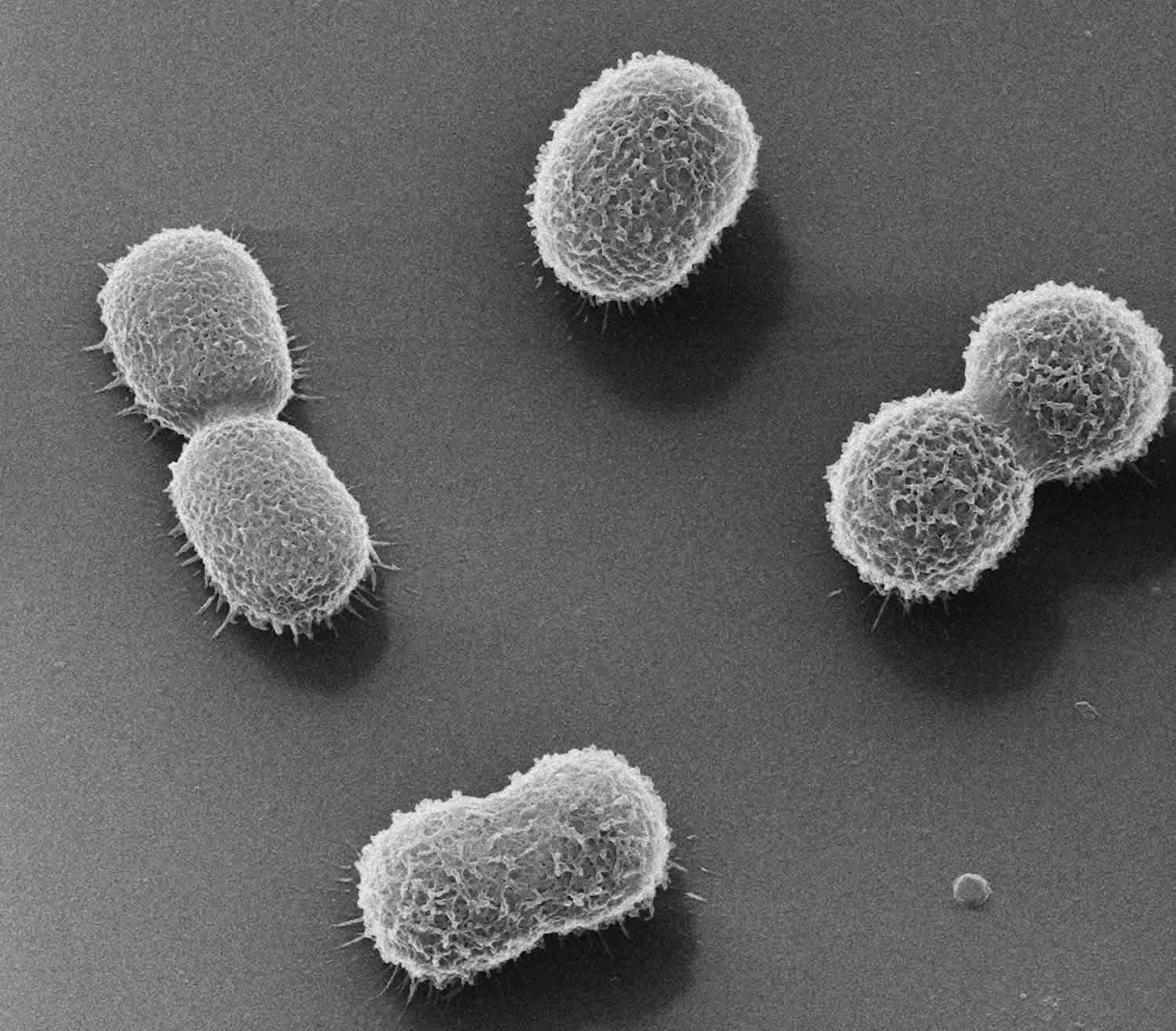
Acinetobacter is a gram-negative, aerobic, non-fermentative, oxidase negative and non-motile paired coccobacillus that are widely distributed in nature and can cause severe primary infections in immunocompromised hosts 1. Acinteobacter has several different species but Acinetobacter baumannii has the greatest known clinical significance. Acinetobacter can be found in soil and water.In patients, they are frequently cultured from the urine, saliva, respiratory secretions and open wounds. Acinetobacter is also known to colonize intravenous fluids and other irrigation solutions 2.
In general, Acinetobacter has low virulence but is capable of causing infection in immunocompromised and neutropenic patients 1. Most of the Acinetobacter infections are a result of nosocomial (originating in a hospital) spread and colonization rather than de novo infections. Thus, great care is required when Acinetobacter is isolated – whether it is an actual infection or just colonization. Risk factors for Acinetobacter infection include:
- Prolonged stay in the intensive care until
- Prior antibiotic exposure
- Mechanical ventilation
- Use of a central venous catheter
- Hemodialysis
Most acinetobacter infections are group outbreaks, and isolated cases are rare. Infections may complicate intravenous (IV) catheter treatment, mechanical ventilation and even peritoneal dialysis. In most cases, the presence of Acinetobacter in respiratory secretions of ventilated patients represents colonization.
Patients in the intensive care unit are the most difficult to treat as colonization is common and it is difficult to distinguish this from an infection. All patients who are noted to have colonization with Acinetobacter should be isolated from other patients to prevent further colonization.Once an infection is treated, the patient’s clinical course must be followed rather than cultures, because colonization may offer a falsely positive diagnosis.
The morbidity of Acinetobacter is related to the patient’s underlying medical condition and immune status. Acinetobacter bacterium is not very virulent but due to various innate mechanisms it has the capacity to acquire resistance. Multidrug-resistant , extensively drug resistant and pan-drug resistant isolates of Acinetobacter have been described as non-susceptible to at least one agent in three or more antibiotic classes, non-susceptible to at least one agent in all but two or fewer antibiotic classes and non-susceptible to all antibiotic classes. Multi-drug resistant Acinetobacter was designated a threat category of ‘Serious’ Center of disease Control Antimicrobial resistance report published in 2013. Though not virulent by itself, the morbidity and mortality of Acinetobacter are high in sick patients with multiorgan disease. In the case of infections being caused by resistant strains of Acinetobacter baumanii, mortality rates of up to 70% have been reported 3.
Acinetobacter infection causes
Even though Acinetobacter is mostly a nosocomial (originating in a hospital) pathogen and is isolated from hospitalized patients, care should be exercised in determining if the isolate is a cause or simply a result of colonization. Acinetobacter is a water-loving organism and has the propensity to colonize body organs that contain fluid. Thus, in hospitalized patients, Acinetobacter is often found in the peritoneal fluid, cerebrospinal fluid (CSF), saliva, respiratory secretions and urinary tract 4.
Acinetobacter gained clinical significance in the 1960s with the increasing growth of intensive care units at hospitals 3. Though Acinetobacter is an organism of low virulence, its ability to survive dessication and persist in the environment for extended duration of time makes it easily transmissible in the healthcare setting. Nosocomial spread by healthcare personnel, respiratory equipment like ventilators and other devices has been reported frequently. It can be found in all types of secretions such as wounds, saliva, urine, and blood. Acinetobacter bacterium has low virulence but is still capable of causing infections in patients with febrile neutropenia and those who have received organ transplants 5.
Acinetobacter symptoms
Prolonged hospitalization or antibiotic therapy predisposes to Acinetobacter colonization, and because colonization is the rule and infection is the exception, colonized patients have no physical findings 1. Patients with Acinetobacter colonization often have a history of prolonged hospitalization or antimicrobial therapy (with antibiotics that have little or no activity against Acinetobacter).
Most patients are in hospital when infected with Acinetobacter. The one organ most commonly involved is the lung, primarily because of colonization of the airways and respiratory equipment used for mechanical ventilation.
Patients with Acinetobacter pneumonias occurring in the context of an outbreak in the intensive care unit (ICU) generally have a history of preceding contact with respiratory support monitors or equipment.
Pneumonia, wound infection, catheter-associated bacteremia or nosocomial meningitis have all been described by Acinetobacter.
There are no pathognomic findings in Acinetobacter infections, and they need to be differentiated from other gram-negative infections like Enterobacter, Burkholderia, Pseudomonas, and Serratia. Since Acinetobacter is chiefly a colonizing organism, the physician has the onus to prove that it is causing the pathology in any given clinical scenario.
Acinetobacter diagnosis
Acinetobacter is a common colonizer of patients in the intensive care unit and those who have multiple comorbid disorders. It is most likely to cause infections in patients who are immunocompromised and those with a compromise of their cardiopulmonary system. The organism can readily be cultured, but the findings need to be correlated to the clinical picture.
Laboratory studies
There may be leucocytosis, with a left shift. However, the findings are nonspecific and do not always indicate the presence of a bacterial infection. When there is an outbreak of Acinetobacter, the organism is usually readily isolated and cultured from body fluids. More important, the outbreak usually involves multiple patients.
Imaging studies
A chest x-ray is required if pneumonia is suspected. Other imaging tests depend on the signs and symptoms.
Procedures
If meningitis is suspected, then CSF needs to be analyzed and cultured.
Histologic findings
There are no specific histopathological features of an Acinetobacter infection that can differentiate it from any other gram-negative bacilli
Acinetobacter treatment
Being a gram-negative organism, the drugs used to treat Acinetobacter infections include the aminoglycosides, fourth-generation cephalosporins, tigecycline, and rifampin 1. Acinetobacter will not respond to macrolides, third-generation cephalosporins, and penicillin 1. When an infection is suspected in the presence of a long-term catheter or a pacemaker, it should be removed 3.
Any external device, infected line, shunt or drain must be removed to obtain a cure. If the patient has a collection of an abscess or necrotic tissue, it needs to be debrided thoroughly.
One should avoid treating colonization as it only leads to more antibiotic resistance.
Over the last few years, drug resistance has become a common problem in the United States. Anti-microbials which may be used in Acinetobacter infections include colistin, carbapenems, tigecycline, polymyxin, amikacin, and beta-lactam/beta-lactamase combinations. But, there have been more recent outbreaks with extensively drug resistant Acinetobacter which makes the management of these infections much more complicated. The duration of therapy is from 7 to 10 days, depending on the patient illness.
Acinetobacter prognosis
The prognosis of Acinetobacter infection depends on the underlying health of the host and the extent of organ involvement; it is the same as for other aerobic gram-negative bacillary infections. The prognosis of an isolated Acinetobacter infection is excellent in patients who are otherwise healthy. Patients who are immunosuppressed tend to have a poor outcome.
Acinetobacter baumannii
Acinetobacter baumannii is a Gram-negative bacillus that is aerobic, pleomorphic and non-motile 6. Acinetobacter baumannii is named in honor of American bacteriologists Paul and Linda Baumann, is an opportunistic nosocomial (hospital-acquired) pathogen with acquired multidrug resistance that is emerging as a major concern worldwide 7. Acinetobacter baumannii has a high incidence among immunocompromised individuals, particularly those who have experienced a prolonged (> 90 days) hospital stay 8. Acinetobacter baumannii is commonly associated with aquatic environments 9, Acinetobacter baumannii is has been shown to colonize the skin as well as being isolated in high numbers from the respiratory and oropharynx secretions of infected individuals 10. In recent years, it has been designated as a “red alert” human pathogen, generating alarm among the medical fraternity, arising largely from its extensive antibiotic resistance spectrum 11.
Acinetobacter baumannii had been regarded as a low-grade pathogen, but it is a successful pathogen responsible for opportunistic infections of the skin, bloodstream, urinary tract, and other soft tissues 12. Because many Acinetobacter baumannii infections have suddenly been reported among veterans and soldiers who served in Iraq and Afghanistan 13, Acinetobacter baumannii is referred to as “Iraqibacter.” Multidrug-resistant Acinetobacter baumannii has spread to civilian hospitals in part by cross-infection of injured military patients repatriated from war zones 12. Most Acinetobacter baumannii infections occur in critically ill patients in the intensive care unit (ICU) setting 14 and account for up to 20% of infections in ICUs worldwide 15. Furthermore, the frequency of community-acquired Acinetobacter baumannii infections has been increasing gradually 7. Several virulence factors have been identified by genomic and phenotypic analyses, including outer membrane porins, phospholipases, proteases, lipopolysaccharides, capsular polysaccharides, protein secretion systems, and iron-chelating systems 16.
Many reports have shown that Acinetobacter baumannii rapidly develops resistance to antimicrobials, and multidrug-resistant strains have been isolated 16. The World Health Organization (WHO) declared that Acinetobacter baumannii is one of the most serious ESKAPE organisms (Enterococcus faecium, Staphylococcus aureus, Klebsiella pneumoniae, Acinetobacter baumannii, Pseudomonas aeruginosa, and Enterobacter species) that effectively escape the effects of antibacterial drugs 17. A number of Acinetobacter baumannii resistance mechanisms are known, including enzymatic degradation of drugs, target modifications, multidrug efflux pumps, and permeability defects 7.
Acinetobacter baumannii symptoms
Acinetobacter baumannii causes a range of infections in both the hospital and community, including skin and soft tissue, urinary tract infections, meningitis, bacteremia, and pneumonia, with the latter being the most frequently reported infection in both settings 18. Hospital-acquired infections are most commonly seen in critically ill patients; specific risk factors for developing an Acinetobacter baumannii infection include prolonged hospital stays, immune suppression, advanced age, presence of comorbid diseases, major trauma or burns, previous antibiotic use, invasive procedures, and presence of indwelling catheters or mechanical ventilation 19. Due to the already poor prognosis of critically ill patients who acquire Acinetobacter baumannii infections, it is difficult to attribute a definitive mortality rate 20; however crude morality rates have ranged from 23 to 68% 21.
Community-acquired infections present as a distinct and severe clinical syndrome in countries with hot and humid climates. These infections typically occur in individuals with underlying health conditions, including diabetes mellitus and chronic obstructive pulmonary disease, or in those that are heavy smokers or drink alcohol in excess 18. Mortality rates for community-acquired Acinetobacter baumannii infections have been reported as high as 64% 22; however, it is currently unknown as to whether host or bacterial factors are responsible for the difference in disease presentation between community and hospital infections.
Acinetobacter baumannii treatment
The optimal treatment for multidrug-resistant Acinetobacter baumannii nosocomial infections has not been established. There are no compelling data to recommend combination therapy for severe Acinetobacter baumannii infections. Carbapenems have been considered the treatment of choice for infections caused by multidrug-resistant Acinetobacter baumannii 23. In the last years, many Acinetobacter baumannii isolates exhibit carbapenem resistance, which is strongly associated with prior use of carbapenems.
Meropenem has a lower affinity for certain oxacillinase enzymes than imipenem 24. Its stability in extended infusion and a comparatively lower seizure threshold than imipenem makes meropenem a rational choice for Acinetobacter baumannii. Unfortunately, rising minimum inhibitory concentrations (MIC) of meropenem substantially decrease the probability of achieving the relevant pharmacokinetic/pharmacodynamic index with the routine dosing regimens of 1 g every 8 hour. A 2-g 8 hour regimen in extended infusion is more likely to achieve the required %T more than MIC target. Nevertheless, these carbapenem-resistant-Acinetobacter baumannii strains exhibit high MIC levels (>32 mg/l) making necessary the use of other antimicrobials. Therefore, carbapenems cannot be used empirically, at least in monotherapy, for severe infections in areas with a high rate of resistance to carbapenems.
Sulbactam is a penicillanic acid sulfone which, as well as being a β-lactamases inhibitor, with intrinsic activity against Acinetobacter baumannii. A pharmacokinetic/pharmacodynamic study performed in healthy volunteers concluded that a 4-hour infusion of 3 g of sulbactam every 8 h constitutes the best treatment option for less susceptible isolates 25. Multiple clinical studies corroborate that high-dose sulbactam (9 g/day) is a valid option in the management of severe Acinetobacter infections. In a retrospective study analyzing infections caused by carbapenem-resistant-Acinetobacter baumannii, polymyxin (colistin or polymyxin B) treatment was significantly associated with higher mortality than sulbactam. The use of a polymyxin was identified as an independent risk factor for mortality 26.
Unfortunately, nowadays the percentage of resistance to sulbactam has reached such a high level 27 that its use as empirical therapy against infections caused by Acinetobacter baumannii is discouraged 28.
Polymyxins are a group of polypeptide cationic antibiotics. Only polymyxin B and polymyxin E (colistin) are used in clinical practice. Colistin is by far the most extensively used polymyxin. It is administered as colistimethate (CMS), a prodrug that needs to be hydrolyzed to its active form (colistin).
Colistimethate is mostly excreted unchanged in urine (70%) and is partly transformed to colistin (30%), whereas renal excretion of colistin is negligible (1–2%). As renal function decreases, a progressively larger fraction of a dose of colistimethate will be converted to colistin. The elimination of colistin is nonrenal because it undergoes extensive renal tubular reabsorption, and nonbiliary by unknown mechanism. In the last years, our knowledge on the clinical pharmacokinetic of colistin has increased substantially. The ratio of the area under the curve (AUC) to the MIC (AUC/MIC ratio) is the best pharmacokinetic–pharmacodynamic index to describe its efficacy profile. A dosing regimen should allow for colistin plasma concentrations of about 2 mg/l to assure the efficacy against colistin susceptible Acinetobacter baumannii. A meta-analysis of 32 studies confirmed the clinical benefit of high doses of colistin (MIC ≤ 2 mg/l) 29. The risk of nephrotoxicity increases as plasma colistin concentration exceeds 2.5 mg/l 30. This problem of heteroresistance to colistin can be overcome with high doses of colistin or with the use of another active agent 31.
Polymyxin B is available for direct intravenous administration. Polymyxin B dosages should be calculated based on body weight and the plasma concentration is not influenced by renal function 32. Of note, the incidence of renal failure seems to be lower with polymyxin B than with colistin 33.
Minocycline exhibits bactericidal activity against Acinetobacter baumannii as well as synergistic effects with different antimicrobials. In retrospective studies, the use of intravenous minocycline provided high rates of clinical success or improvement and was generally well tolerated among patients with multidrug-resistant or carbapenem-resistant-Acinetobacter baumannii infections 34.
Serious doubts exist about the role of tigecycline in monotherapy for multidrug-resistant-Acinetobacter baumannii infections. The currently approved dosage is a 100-mg loading dose followed by a 50-mg dose administered twice daily. Tigecycline possesses a large distribution volume but Cmax in the serum does not exceed 0.87 mg/l with the standard regimen; treatment of intravascular/bacteremic infections by Acinetobacter baumannii seems impossible with the approved regimen 35. Similarly, tigecycline concentrations in pulmonary endothelial lining fluid with conventional dosing are insufficient (0.01–0.02 mg/l) to treat Acinetobacter baumannii pneumonia 36.
A matched cohort analysis concluded that the tigecycline-based therapy resulted in higher in-hospital mortality than the colistin-based therapy (61 vs. 44%, respectively) in critically ill patients with pneumonia caused by multidrug-resistant Acinetobacter baumannii. This lower efficacy of tigecycline might be because of Acinetobacter baumannii isolates with MIC more than 2 mg/l 37. Two meta-analyses discourage the use of a tigecycline for the treatment of multidrug-resistant-Acinetobacter baumannii infections because, compared with other active antimicrobials, the use of tigecycline was associated with higher in-hospital mortality, lower microbial eradication rate and longer length of stay 38. Nevertheless, a high-dose regimen (200 mg/day), usually in combination with another antimicrobial, may be an effective and well-tolerated alternative for severe Acinetobacter baumannii infections including hospital acquired pneumonia 39.
A recent observational study that evaluated multiple combinations (colistin and tigecycline followed by carbapenem and tigecycline were the most common combinations) compared with monotherapy (colistin and carbapenems were the most common drugs used in monotherapy) failed to demonstrate any benefits in term of mortality in patients with sepsis because of multidrug-resistant Acinetobacter baumannii. Various observational studies evaluating different colistin-based combination therapy against monotherapy with colistin have reported a higher eradication rate but no impact on mortality with the used of combination therapy 40. It is worth mentioning a retrospective study that compared monotherapy with colistin with patients that received combination therapy (colistin and carbapenem, sulbactam, tigecycline, or other agents) in multidrug-resistant-Acinetobacter baumannii bloodstream infection. Rates of 14-day survival and microbiological eradication were significantly higher in the combination group but without differences in hospital mortality 40.
Several in-vitro studies have documented the existence of a potent synergism of the combination of colistin with anti-gram-positive antibiotics 41. In a retrospective series, clinical benefit of the combination of colistin and vancomycin was not documented in patients with Acinetobacter baumannii ventilator-associated pneumoni and bloodstream infection. In addition, the rate of renal failure was significantly higher in patients on combination therapy compared with those on monotherapy with colistin 42. Conversely, a multicenter study that included a heterogeneous group of infections caused by different gram-negative bacilli concluded that therapy with colistin and a glycopeptide at least five days was a protective factor for 30-day mortality 43.
- Colistin and rifampicin. A randomized, open label trial found no difference in mortality or length of hospitalization between a colistin-rifampicin group and colistin monotherapy in serious multidrug-resistant-Acinetobacter baumannii infections. However, an increased rate of Acinetobacter baumannii eradication with combination therapy was observed 44. The results were identical in another clinical trial that compared colistin and rifampicin with colistin in 43 patients with ventilator-associated pneumonia caused by carbapenem-resistant-Acinetobacter baumannii 45.
- Colistin and fosfomycin. A recent randomized open-trial evaluated monotherapy with colistin compared with the combination of colistin and fosfomycin for 7–14 days in patients infected with carbapenem-resistant Acinetobacter baumannii. Microbiological response at the first 72 hours and at the end of treatment were significantly higher in the combination group but without differences in clinical cure rate or 28-day mortality 46.
- Colistin and meropenem. Experimental studies suggest that for Acinetobacter baumannii infections, polymyxin–carbapenem combinations are synergistic and increased bactericidal activity compared with polymyxins alone. A recent randomized controlled trial that enrolled 406 patients with severe infections caused by carbapenem-resistant gram-negative bacteria concluded that combination therapy (colistin and meropenem) did not result in better outcomes compared with colistin monotherapy. Specifically, for Acinetobacter baumannii infections, no differences existed between monotherapy and combination therapy for clinical failure (primary outcome), or 14-day and 28-day mortality 47.
Diverse meta-analyses have assessed the use of combination therapy in severe Acinetobacter baumannii infections. A meta-analysis 48 that included five observational studies and two randomized controlled trials concluded that the combination of colistin and rifampicin compared with colistin alone did not impact on mortality rate or length of hospitalization although microbiological eradication rate was significantly higher in the combination group. The use of rifampicin was associated with a nonsignificant trend toward a higher incidence of liver toxicity. However, the variability in the doses administered including the low doses of colistin used in these studies and the lack of colistin loading dose warrant further investigation of this antimicrobial combination. Another meta-analysis 49 concluded that the combination of polymyxins with other antibiotics achieved similar hospital mortality and clinical response rates than monotherapy.
It is worth mentioning a recent meta-analysis that concluded that colistin in combination with sulbactam was associated with a significantly higher microbiological cure rate compared with colistin in combination with tigecycline and colistin monotherapy although mortality rates were unaffected. As expected by its pharmacokinetic properties, tigecycline-based therapy was significantly less effective for achieving a microbiological cure in bloodstream infections 38. Finally, a Bayesian network meta-analysis analyzed the comparative effectiveness of different antimicrobials in monotherapy or combined for multidrug-resistant-Acinetobacter baumannii hospital acquired pneumonia in critically ill patients. Intravenous colistin monotherapy was chosen as comparator. For survival benefit, sulbactam appears to be the best treatment option. Among combinations, colistin and fosfomycin achieved the highest survival benefit 50.
References- Brady MF, Pervin N. Acinetobacter. [Updated 2018 Dec 28]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK430784
- Munier AL, Biard L, Legrand M, Rousseau C, Lafaurie M, Donay JL, Flicoteaux R, Mebazaa A, Mimoun M, Molina JM. Incidence, risk factors and outcome of multi-drug resistant Acinetobacter baumannii nosocomial infections during an outbreak in a burn unit. Int. J. Infect. Dis. 2019 Feb;79:179-184.
- Wong D, Nielsen TB, Bonomo RA, Pantapalangkoor P, Luna B, Spellberg B. Clinical and Pathophysiological Overview of Acinetobacter Infections: a Century of Challenges. Clin. Microbiol. Rev. 2017 Jan;30(1):409-447.
- Garnacho-Montero J, Timsit JF. Managing Acinetobacter baumannii infections. Curr. Opin. Infect. Dis. 2019 Feb;32(1):69-76.
- de Azevedo FKSF, Dutra V, Nakazato L, Mello CM, Pepato MA, de Sousa ATHI, Takahara DT, Hahn RC, Souto FJD. Molecular epidemiology of multidrug-resistant Acinetobacter baumannii infection in two hospitals in Central Brazil: the role of ST730 and ST162 in clinical outcomes. J. Med. Microbiol. 2019 Jan;68(1):31-40.
- Howard A, O’Donoghue M, Feeney A, Sleator RD. Acinetobacter baumannii: an emerging opportunistic pathogen. Virulence. 2012;3(3):243–250. doi:10.4161/viru.19700 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3442836
- Lin M. F., Lan C. Y. (2014). Antimicrobial resistance in Acinetobacter baumannii: from bench to bedside. World J. Clin. Cases. 2, 787–814. 10.12998/wjcc.v2.i12.787
- Montefour K, Frieden J, Hurst S, Helmich C, Headley D, Martin M, et al. Acinetobacter baumannii: an emerging multidrug-resistant pathogen in critical care. Crit Care Nurse. 2008;28:15–25, quiz 26.
- Turton JF, Kaufmann ME, Gill MJ, Pike R, Scott PT, Fishbain J, et al. Comparison of Acinetobacter baumannii isolates from the United Kingdom and the United States that were associated with repatriated casualties of the Iraq conflict. J Clin Microbiol. 2006;44:2630–4. doi: 10.1128/JCM.00547-06
- Sebeny PJ, Riddle MS, Petersen K. Acinetobacter baumannii skin and soft-tissue infection associated with war trauma. Clin Infect Dis. 2008;47:444–9. doi: 10.1086/590568
- Cerqueira GM, Peleg AY. Insights into Acinetobacter baumannii pathogenicity. IUBMB Life. 2011;63:1055–60. doi: 10.1002/iub.533
- Peleg A. Y., Seifert H., Paterson D. L. (2008). Acinetobacter baumannii: emergence of a successful pathogen. Clin. Microbiol. Rev. 21, 538–582. 10.1128/CMR.00058-07
- Centers for Disease Prevention (2004). Acinetobacter baumannii infections among patients at military medical facilities treating injured U.S. service members, 2002–2004. MMWR Morb. Mortal. Wkly. Rep. 53, 1063–1066.
- Fournier P. E., Richet H. (2006). The epidemiology and control of Acinetobacter baumannii in health care facilities. Clin. Infect. Dis. 42, 692–699. 10.1086/500202
- Vincent J. L., Rello J., Marshall J., Silva E., Anzueto A., Martin C. D., et al. . (2009). International study of the prevalence and outcomes of infection in intensive care units. JAMA 302, 2323–2329. 10.1001/jama.2009.1754
- McConnell M. J., Actis L., Pachon J. (2013). Acinetobacter baumannii: human infections, factors contributing to pathogenesis and animal models. FEMS Microbiol. Rev. 37, 130–155. 10.1111/j.1574-6976.2012.00344.x
- Boucher H. W., Talbot G. H., Bradley J. S., Edwards J. E., Gilbert D., Rice L. B., et al. . (2009). Bad bugs, no drugs: no ESKAPE! An update from the Infectious Diseases Society of America. Clin. Infect. Dis. 48, 1–12. 10.1086/595011
- Dexter C., Murray G. L., Paulsen I. T., Peleg A. Y. (2015). Community-acquired Acinetobacter baumannii: clinical characteristics, epidemiology and pathogenesis. Expert Rev. Anti-Infect. Ther. 13, 567–573. 10.1586/14787210.2015.1025055
- Wong D., Nielsen T. B., Bonomo R. A., Pantapalangkoor P., Luna B., Spellberg B. (2017). Clinical and pathophysiological overview of Acinetobacter infections: a century of challenges. Clin. Microbiol. Rev. 30, 409–447. 10.1128/CMR.00058-16
- Freire M. P., De Oliveira Garcia D., Garcia C. P., Campagnari Bueno M. F., Camargo C. H., Kono Magri A. S. G., et al. . (2016). Bloodstream infection caused by extensively drug-resistant Acinetobacter baumannii in cancer patients: high mortality associated with delayed treatment rather than with the degree of neutropenia. Clin. Microbiol. Infect. 22, 352–358. 10.1016/j.cmi.2015.12.010
- Eliopoulos G. M., Maragakis L. L., Perl T. M. (2008). Acinetobacter baumannii: epidemiology, antimicrobial resistance, and treatment options. Clin. Infect. Dis. 46, 1254–1263. 10.1086/529198
- Patamatamkul S., Klungboonkrong V., Praisarnti P., Jirakiat K. (2017). A case-control study of community-acquired Acinetobacter baumannii pneumonia and melioidosis pneumonia in Northeast Thailand: an emerging fatal disease with unique clinical features. Diagn. Microbiol. Infect. Dis. 87, 79–86. 10.1016/j.diagmicrobio.2016.10.014
- Managing Acinetobacter Baumannii Infections. Curr Opin Infect Dis. 2019;32(1):69-76.
- Roca I, Espinal P, Vila-Farrés X, Vila J. The Acinetobacter baumannii oxymoron: commensal hospital dweller turned pan-drug-resistant menace. Front Microbiol 2012; 3:148.
- Jaruratanasirikul S, Wongpoowarak W, Aeinlang N, Jullangkoon M. Pharmacodynamics modeling to optimize dosage regimens of sulbactam. Antimicrob Agents Chemother 2013; 57:3441–3444.
- Oliveira MS, Prado GV, Costa SF, et al. Ampicillin/sulbactam compared with polymyxins for the treatment of infections caused by carbapenem-resistant Acinetobacter spp. J Antimicrob Chemother 2008; 61:1369–1375.
- Yang Y, Fu Y, Lan P, et al. Molecular epidemiology and mechanism of sulbactam resistance in Acinetobacter baumannii isolates with diverse genetic backgrounds in China. Antimicrob Agents Chemother 2018; 62: doi: 10.1128/AAC.01947–17.
- Garnacho-Montero J, Dimopoulos G, Poulakou G, et al. Task force on management and prevention of Acinetobacter baumannii infections in the ICU. Intensive Care Med 2015; 41:2057–2075.
- Vardakas KZ, Mavroudis AD, Georgiou M, Falagas ME. Intravenous colistin combination antimicrobial treatment vs. monotherapy: a systematic review and meta-analysis. Int J Antimicrob Agents 2018; 51:535–547.
- Horcajada JP, Sorli L, Luque S, et al. Validation of a colistin plasma concentration breakpoint as a predictor of nephrotoxicity in patients treated with colistin methanesulfonate. Int J Antimicrob Agents 2016; 48:725–727.
- Srinivas P, Hunt LN, Pouch SM, et al. Detection of colistin heteroresistance in Acinetobacter baumannii from blood and respiratory isolates. Diagn Microbiol Infect Dis 2018; 91:194–198.
- Sandri AM, Landersdorfer CB, Jacob J, et al. Population pharmacokinetics of intravenous polymyxin B in critically ill patients: implications for selection of dosage regimens. Clin Infect Dis 2013; 57:524–531.
- Akajagbor DS, Wilson SL, Shere-Wolfe KD, et al. Higher incidence of acute kidney injury with intravenous colistimethate sodium compared with polymyxin B in critically ill patients at a tertiary care medical center. Clin Infect Dis 2013; 57:1300–1303.
- Greig SL, Scott LJ. Intravenous minocycline: a review in Acinetobacter infections. Drugs 2016; 76:1467–1476.
- Meagher AK, Ambrose PG, Grasela TH, et al. Pharmacokinetic/pharmacodynamics profile for tigecycline: a new glycylcycline antimicrobial agent. Diagn Microbiol Infect Dis 2005; 52:165–171.
- Burkhardt O, Rauch K, Kaever V, et al. Tigecycline possibly underdosed for the treatment of pneumonia: a pharmacokinetic viewpoint. Int J Antimicrob Agents 2009; 34:101–102.
- Chuang YC, Cheng CY, Sheng WH, et al. Effectiveness of tigecycline-based versus colistin-based therapy for treatment of pneumonia caused by multidrug-resistant Acinetobacter baumannii in a critical setting: a matched cohort analysis. BMC Infect Dis 2014; 14:102.
- Kengkla K, Kongpakwattana K, Saokaew S, et al. Comparative efficacy and safety of treatment options for MDR and XDR Acinetobacter baumannii infections: a systematic review and network meta-analysis. J Antimicrob Chemother 2018; 73:22–32.
- De Pascale G, Montini L, Pennisi M, et al. High dose tigecycline in critically ill patients with severe infections due to multidrug-resistant bacteria. Crit Care 2014; 18:R90.
- Batirel A, Balkan II, Karabay O, et al. Comparison of colistin-carbapenem, colistin-sulbactam, and colistin plus other antibacterial agents for the treatment of extremely drug-resistant Acinetobacter baumannii bloodstream infections. Eur J Clin Microbiol Infect Dis 2014; 33:1311–1322.
- Galani I, Orlandou K, Moraitou H, et al. Colistin/daptomycin: an unconventional antimicrobial combination synergistic in vitro against multidrug-resistant Acinetobacter baumannii. Int J Antimicrob Agents 2014; 43:370–374.
- Garnacho-Montero J, Amaya-Villar R, Gutiérrez-Pizarraya A, et al. Clinical efficacy and safety of the combination of colistin plus vancomycin for the treatment of severe infections caused by carbapenem-resistant A. baumannii. Chemotherapy 2013; 59:225–231.
- Petrosillo N, Giannella M, Antonelli M, et al. Colistinglycopeptide combination in critically ill patients with Gram-negative infection: the clinical experience. Antimicrob Agents Chemother 2014; 58:851–858.
- Durante-Mangoni E, Signoriello G, Andini R, et al. Colistin and rifampicin compared with colistin alone for the treatment of serious infections due to extensively drug-resistant Acinetobacter baumannii: a multicenter, randomized clinical trial. Clin Infect Dis 2013; 57:349–358.
- Aydemir H, Akduman D, Piskin N, et al. Colistin vs. the combination of colistin and rifampicin for the treatment of carbapenem-resistant Acinetobacter baumanniiventilator-associated pneumonia. Epidemiol Infect 2013; 141:1214–1222.
- Sirijatuphat R, Thamlikitkul V. Colistin versus colistin plus fosfomycin for treatment of carbapenem-resistant Acinetobacter baumannii infections: a preliminary study. Antimicrob Agents Chemother 2014; 58:5598–5601.
- Paul M, Daikos GL, Durante-Mangoni E, et al. Colistin alone versus colistin plus meropenem for treatment of severe infections caused by carbapenem-resistant Gram-negative bacteria: an open-label, randomised controlled trial. Lancet Infect Dis 2018; 18:391–400.
- Mohammadi M, Khayat H, Sayehmiri K, et al. Synergistic effect of colistin and rifampin against multidrug resistant Acinetobacter baumannii: a systematic review and meta-analysis. Open Microbiol J 2017; 11:63–71.
- Liu Q, Li W, Feng Y, Tao C. Efficacy and safety of polymyxins for the treatment of Acinectobacter baumannii infection: a systematic review and meta-analysis. PLoS One 2014; 9:e98091.
- Jung SY, Lee SH, Lee SY, et al. Antimicrobials for the treatment of drug-resistant Acinetobacter baumannii pneumonia in critically ill patients: a systemic review and Bayesian network meta-analysis. Crit Care 2017; 21:319.