Nocardia infection
Nocardia is partially acid-fast, aerobic, gram-positive, branching filamentous bacillus bacterium that is found ubiquitously in soil, fresh and salt water, decomposing vegetation, other organic matter and marine water 1. There are more than 100 Nocardia species defined. However, approximately 30 of these carry significance to human disease. Nocardia species cause serious pulmonary infections (with occasional brain abscesses) in immunocompromised patients, primarily those with cell-mediated immunity abnormalities 2. Nocardiosis is a rare infection caused by several species of Nocardia bacteria and have two main clinical forms, disseminated and/or pulmonary infection and cutaneous infection. Nocardiosis most commonly occurs after Nocardia bacterium has been introduced into the respiratory tract, but it may be acquired through direct inoculation into the skin 3. Classically, Nocardia manifests as an opportunistic infection in immunocompromised hosts and can impact nearly every part of the human body including skin and skin structures, the pleural or pulmonary system, or it can be a disseminated disease impacting other organ systems 4. However, Nocardia bacteremia is rarely reported, even for severely immunocompromised patients with underlying malignancies 5.
Disseminated and/or pulmonary nocardiosis
Disseminated and/or pulmonary nocardiosis is the most common form of nocardiosis and the responsible bacteria are usually Nocardia asteroides. Humans become infected by breathing in the Nocardia bacterium. Many patients with disseminated and/or pulmonary nocardiosis have immunodeficiency, such as chronic (long-term) lung disease, HIV infection, or long-term use of immunosuppressant medications. The disease often begins in the lungs but can spread to involve any organ, most commonly the brain (causing brain abscesses), and skin in 10 to 30% of cases.
Nocardia skin infection
Cutaneous nocardiosis is usually caused by Nocardia brasiliensis and primarily affects individuals who are otherwise healthy. The bacteria enter the body via a skin wound, such as a cat scratch or a puncture wound from a thorn. Three types of primary cutaneous nocardiosis have been described:
- Superficial skin infection
- Lymphocutaneous infection
- Mycetoma (click on the link for details)
Disseminated and/or pulmonary nocardiosis can also spread to involve the skin; in these cases Nocardia asteroides is often responsible. Conversely, primary cutaneous disease can rarely spread to involve the lungs, brain, and other organs.
In the United States, an estimated 500-1000 new cases of Nocardia infection occur each year. Worldwide rates of nocardiosis vary by country. Middle-aged men performing outdoor labour are at highest risk of infection. Other species of Nocardia less commonly cause infection, such as Nocardia farcinica, Nocardia nova, Nocardia transvalensis, and Nocardia pseudobrasiliensis. There is no racial predilection; however, it has been observed that males are at a higher risk for infection than females with an incidence of 3:1. There is no age predilection for infection; however, those impacted are, on average, in their 40s 6.
Given the severity and rarity of nocardial infections in immunocompromised patients and the high rate of dissemination and abscess formation of the bacterium, it is essential to utilize a multidisciplinary approach toward evaluation and treatment to yield the best results. Some examples of specialties that should be involved in the decision-making process to determine optimal treatment include primary care physicians, infectious diseases specialists, general, neurological, and/or cardiothoracic surgeons, pulmonologists, neurologists, critical care physicians, and/or ophthalmologists.
Some data indicate that prophylaxis with trimethoprim-sulfamethoxazole in AIDS patients with a low CD 4 count may decrease the risk of nocardiosis 7.
There are only small cases series on outcomes of Nocardia treatment. Individuals with intact immunity usually have a good outcome, but transplant patients or those with HIV who are immunosuppressed have a guarded prognosis. The management of a transplant patient requires an interdisciplinary approach if high morbidity and mortality is to be avoided 8.
Nocardiosis causes
Pulmonary nocardiosis and disseminated forms of the infection are opportunistic diseases occurring mainly in patients deficient in T cell-mediated immunity 6. Patients with the greatest susceptibility to this include those with solid organ transplant and hematopoietic stem cell transplant recipients, HIV-infected patients, patients taking corticosteroids chronically, or patients with ongoing malignant processes. Primary cutaneous nocardiosis may occur in immunocompetent patients who have experienced a direct inoculation of the microorganism into the skin structures from a traumatic event. This is seen most commonly in those working in rural areas involving in agricultural activities. While rare, post-surgical wound infections may occur if non-sterile equipment is used. Pulmonary forms of nocardiosis are induced via aerosolized inoculation of the bacterium into the airways. Dissemination throughout the remainder of the body may occur from either of these initial inoculations 9.
Nocardia symptoms
The clinical presentation of nocardiosis is variable and depends greatly on the organ systems involved in the infection.
Pulmonary nocardiosis symptoms
May present as either an acute infection, a subacute infection, or a chronic infection. Pulmonary nocardiosis is clinically determined with the findings of inflammatory bronchial mass or pneumonia with fever, productive cough, dyspnea, or chest pain. Pulmonary disease may be complicated by cavitation, abscess formation, pleural effusion, or empyema.
Disseminated nocardiosis symptoms
Deep abscesses are possible to form at any disseminated site. Signs and symptoms in these scenarios are tailored to the location of the abscess. Non-central nervous system (CNS) findings will at a minimum typically include fever. Dissemination to the central nervous system will additionally show signs of slow growth mass lesion effect with neurological signs such as numbness or muscular weakness representative of the region of the brain or spinal cord impacted. Signs of meningitis such as headache, stiff neck, lethargy, confusion, seizures, sudden onset of paralysis or altered mental status may be present as well 10.
Nocardia skin infection symptoms
Primary cutaneous nocardiosis presents in the form of skin and skin structure infections. There is usually a history of trauma to the skin with breaking the skin in a “dirty” environment several days to several months prior. Patients will present with complaints of an erythematous, a tender, warm, swollen area around the traumatic site that appears similar to simple cellulitis. They may complain of tender nodules or abscesses in the vicinity. Purulent drainage may be present as well. In more progressed cases, suppurative necrosis formation occurs. Clinically, this form of infection is indistinguishable from other bacterial pathologies.
- Superficial skin infection – This is characterized by pus-filled blisters, ulcers, abscesses, or cellulitis. Pyoderma (pus-filled crusting lesion that heals with ulcer formation) may be present. Fever is common, but lymph nodes are not usually enlarged. This condition cannot be distinguished clinically from infections caused by more common organisms, such as Staphylococcus aureus. Less common superficial infections include primary eye infection; this is an uncommon complication of cataract surgery or LASIK eye surgery.
- Lymphocutaneous nocardiosis – This is rare. Presents similarly to primary cutaneous nocardiosis with the addition of ascending regional lymphadenopathy. An ulcerating lump is found at the site of the injury, followed by spreading inflammation and subcutaneous nodular (lumpy) lesions along the lymphatic chain. Pus may drain from the lesions and other nearby lymph nodes may be enlarged. Lymph nodes may ulcerate to have weeping necrotic or purulent drainage in severe cases.
Nocardia infection complications
- Lung infection, empyema
- Brain abscess
- Meningitis
- Osteomyelitis
Nocardia diagnosis
Nocardiosis diagnosis can be difficult, as Nocardia grow slowly in the laboratory. Blood tests for antibodies against Nocardia are unreliable and not available commercially. Current diagnostic tests include:
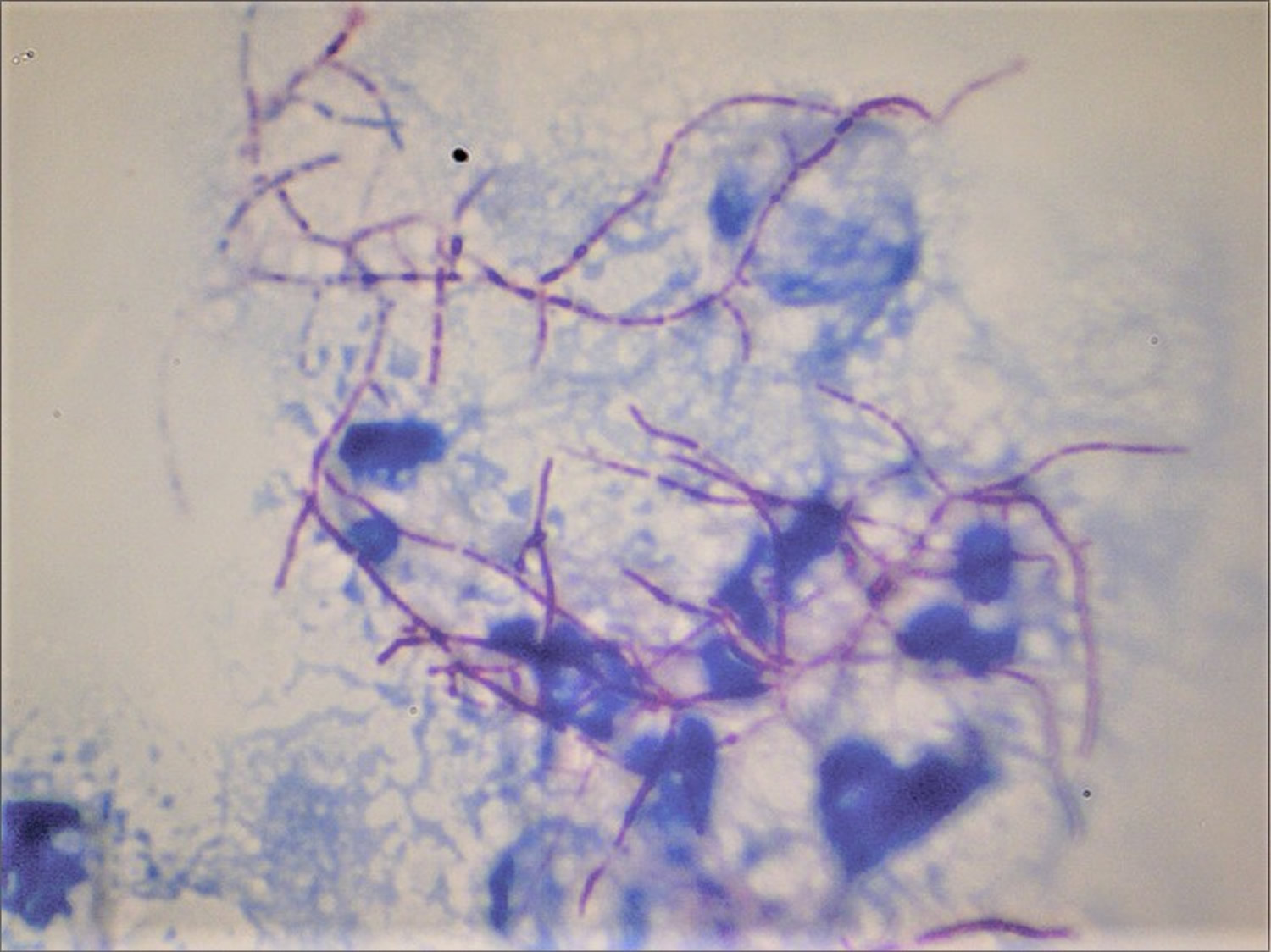
- Gram staining and modified acid-fast staining from smears of draining areas or skin biopsy specimens.
- Nocardia may take up to 2-3 weeks to grow in the laboratory; specimens from multiple clinical sites should be submitted.
Essential evaluation when suspecting nocardiosis should include bacterial cultures of the infectious sites, skin biopsy, purulent discharge, sputum, deep abscess or pleural aspirates, and others. Nocardia is notoriously slow growing, so suspicion should be shared with the laboratory to allow for ample growth time of up to 3 to 5 days. Additionally, blood cultures should be collected whenever a disseminated or pulmonary infection is suspected.
Imaging studies should include plain film chest radiography and CT chest for pulmonary infection. While there are no classical findings on radiography, they may show irregular nodules, cavitation, diffuse alveolar pulmonary infiltrates, lung abscess, or pleural effusion. Additional imaging should include CT or MRI of the brain to evaluate for disseminated Nocardia to the central nervous system (CNS). If meningeal signs are present, lumbar puncture with evaluation of cerebrospinal fluid (CSF) should be performed 11.
Nocardia treatment
Long-term antibiotic therapy is required to prevent relapse; suggested treatment duration ranges from a minimum of 6 months for minor infections, to 1 year for severe disseminated disease 6. Treatment for nocardiosis using of antibiotics should extend for at least 1 month after symptoms of infection have resolved using of antibiotics
- The most commonly used antibiotic is trimethoprim-sulfamethoxazole (TMP-SMZ).
- Some species of Nocardia are resistant to trimethoprim-sulfamethoxazole, so antibiotic susceptibility testing is important.
- Patients with severe disseminated disease require intravenous antibiotics such as amikacin in combination with imipenem.
Surgical drainage or excision is often required for abscesses.
Skin infections in an immunocompetent patient may be managed with monotherapy. For pulmonary or disseminated disease, empiric therapy should consist of 2 to 3 agents. However, there are no therapies proven to be superior at this time. As such, antibiotics should be tailored following culture and sensitivity patterns. Potential agents to use include trimethoprim/sulfamethoxazole, amikacin, imipenem, meropenem, third-generation cephalosporins such as ceftriaxone and cefotaxime, minocycline, extended spectrum fluoroquinolones such as moxifloxacin, linezolid, tigecycline, dapsone, and clarithromycin.
Simple abscesses require surgical incision and drainage. Brain abscesses will require surgical intervention if the mass effect is large or if there is no improvement after 2 weeks of antibiotic therapy.
Close monitoring is essential for up to 1 year following cessation of antibiotics to detect relapse infection. Likewise, radiographic studies and laboratory studies should be monitored 9.
Nocardia prognosis
Prognosis of nocardiosis is variable. It depends upon the organ infected, duration, immunological state of the person, and severity of the infection. Approximately 10% of cases of uncomplicated pulmonary disease are fatal. The case-fatality rate increases with disseminated disease or brain abscesses, particularly in patients with impaired immunity. Cutaneous nocardiosis is rarely fatal, but long-lasting mycetomal infection can be significantly disfiguring.
References- Al Akhrass, F., Hachem, R., Mohamed, J. A., Tarrand, J. J., Kontoyiannis, D. P., Chandra, J, Raad, I. (2011). Central Venous Catheter–associated Nocardia Bacteremia in Cancer Patients. Emerging Infectious Diseases, 17(9), 1651-1658. https://dx.doi.org/10.3201/eid1709.101810
- Phillip I. Lerner, Nocardiosis, Clinical Infectious Diseases, Volume 22, Issue 6, June 1996, Pages 891–905, https://doi.org/10.1093/clinids/22.6.891
- McNeil MM, Brown JM. The medically important aerobic actinomycetes: epidemiology and microbiology. Clin Microbiol Rev. 1994;7:357–417.
- Wilson JW. Nocardiosis: updates and clinical overview. Mayo Clin. Proc. 2012 Apr;87(4):403-7.
- Lui WY, Lee AC, Que TL. Central venous catheter–associated Nocardia bacteremia. Clin Infect Dis. 2001;33:1613–4.
- Rawat D, Sharma S. Nocardiosis. [Updated 2019 Mar 2]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK526075
- Boamah H, Puranam P, Sandre RM. Disseminated Nocardia farcinica in an immunocompetent patient. IDCases. 2016;6:9-12.
- Wang HK, Sheng WH, Hung CC, Chen YC, Lee MH, Lin WS, Hsueh PR, Chang SC. Clinical characteristics, microbiology, and outcomes for patients with lung and disseminated nocardiosis in a tertiary hospital. J. Formos. Med. Assoc. 2015 Aug;114(8):742-9.
- Mazzaferri F, Cordioli M, Segato E, Adami I, Maccacaro L, Sette P, Cazzadori A, Concia E, Azzini AM. Nocardia infection over 5 years (2011-2015) in an Italian tertiary care hospital. New Microbiol. 2018 Apr;41(2):136-140.
- Singh AK, Shukla A, Bajwa R, Agrawal R, Srivastwa N. Pulmonary Nocardiosis: Unusual Presentation in Intensive Care Unit. Indian J Crit Care Med. 2018 Feb;22(2):125-127.
- Thirouvengadame S, Muthusamy S, Balaji VK, Easow JM. Unfolding of a Clinically Suspected Case of Pulmonary Tuberculosis. J Clin Diagn Res. 2017 Aug;11(8):DD01-DD03.