What is agranulocytosis
Agranulocytosis is a serious and sometimes fatal condition whereby your body has too few granulocytes (white blood cells). Agranulocytosis is characterized by an absolute neutrophil count below 0.5 × 109/L (500/μL) 1. This makes it harder for your body to fight off germs. As a result, the person with agranulocytosis is more likely to get sick from infections. Because white blood cells fight infections from bacteria, viruses, fungi, and other germs. One important type of white blood cell is the granulocyte, which is made in the bone marrow and travels in the blood throughout the body. Granulocytes sense infections, gather at sites of infection, and destroy the germs.
Things you can do yourself to avoid infections
If you have a low white blood cell count caused by illness or medication you should take steps to avoid infections.
DO
- avoid close contact with people who are sick
- store and prepare food properly to avoid food poisoning
- wash your hands with soap and warm water regularly
- use an electric shaver instead of a razor
- avoid shared hot tubs
DON’T
- share food, cups, utensils, toothbrushes or make-up
- eat raw foods, like meat, shellfish and eggs
- change cat litter or handle animal poo
- change nappies
- walk outside barefoot
- swim in ponds and rivers
Congenital agranulocytosis
Congenital agranulocytosis also known as congenital neutropenia syndromes, severe congenital neutropenia, severe infantile genetic neutropenia, infantile genetic agranulocytosis, or Kostmann disease, are a group of rare disorders present from birth that are characterized by low levels of neutrophils, a type of white blood cell necessary for fighting infections.
The incidence of severe congenital agranulocytosis is estimated to be 1 in 200,000 individuals 2.
People with congenital agranulocytosis have a shortage (deficiency) of neutrophils, a type of white blood cell that plays a role in inflammation and in fighting infection. The deficiency of neutrophils, called neutropenia, is apparent at birth or soon afterward 2. Congenital agranulocytosis leads to recurrent infections beginning in infancy, including infections of the sinuses, lungs, and liver. Affected individuals can also develop fevers and inflammation of the gums (gingivitis) and skin. Approximately 40 percent of affected people have decreased bone density (osteopenia) and may develop osteoporosis, a condition that makes bones progressively more brittle and prone to fracture 2. In people with severe congenital neutropenia, these bone disorders can begin at any time from infancy through adulthood.
Approximately 20 percent of people with severe congenital neutropenia develop certain cancerous conditions of the blood, particularly myelodysplastic syndrome or leukemia during adolescence 2.
Some people with severe congenital neutropenia have additional health problems such as seizures, developmental delay, or heart and genital abnormalities 2.
Congenital agranulocytosis are primary immune deficiency diseases (PIDD). Primary immune deficiency diseases (PIDDs) are rare, genetic disorders that impair the immune system. Without a functional immune response, people with primary immune deficiency diseases (PIDDs) may be subject to chronic, debilitating infections, such as Epstein-Barr virus (EBV), which can increase the risk of developing cancer. Some primary immune deficiency diseases can be fatal. Primary immune deficiency diseases (PIDDs) may be diagnosed in infancy, childhood, or adulthood, depending on disease severity.
Researchers have identified numerous genetic mutations that cause congenital agranulocytosis (congenital neutropenia syndromes). Generally, mutations that result in congenital agranulocytosis affect the development, lifespan, or function of neutrophils.
Congenital agranulocytosis are inherited through autosomal recessive, autosomal dominant, and X-linked inheritance patterns. The genes linked to these syndromes include the following 3:
- ELANE
- HAX1
- G6PC3
- GFI1
- CSF3R
- X-linked WAS
- CXCR4
- VPS45A
- JAGN1
In some people, however, the disease-causing mutation of their congenital agranulocytosis is unknown.
People with congenital agranulocytosis experience bacterial infections early in life. These may cause inflammation of the umbilical cord stump, abscesses (or boils) on the skin, oral infections, and pneumonia.
Congenital agranulocytosis also increases one’s risk for developing myelodysplastic syndromes (MDS), blood disorders that are distinguished by low levels of various blood cells. MDS may progress to a type of blood-cell cancer called acute myeloid leukemia.
Bone marrow and blood tests can measure the levels of various white blood cells to test for deficiencies. A person suspected of having congenital agranulocytosis also may undergo genetic testing for one of the genetic mutations known to cause the syndromes.
Standard therapy for congenital agranulocytosis includes injections of granulocyte colony-stimulating factor (G-CSF), an immune-cell-growth molecule that can help restore the function of the immune system. People on granulocyte colony-stimulating factor (G-CSF) therapy may have a lower incidence and severity of infections, improving their quality of life, but effects vary. For some individuals, a bone-marrow transplant may be recommended to replace defective immune cells with healthy ones from a donor.
What are white blood cells
White blood cells, also called leukocytes (or leucocytes), are the cells of the immune system that are involved in protecting the body against both infectious disease and foreign invaders 4. All white blood cells are produced and derived from multipotent cells in the bone marrow known as hematopoietic stem cells. Leukocytes are found throughout the body, including the blood and lymphatic system.
Most blood samples are about 45% red blood cells by volume, with the white blood cells and platelets accounting for less than 1% of blood volume. The remaining blood sample, about 55%, is the plasma, a clear, straw-colored liquid (see Figure 1). Blood transports leukocytes to sites of infection. Leukocytes may then leave the bloodstream.
Like red blood cells, white blood cells (leukocytes) have limited life spans, so they must constantly be replaced. Leukocytes develop from hematopoietic stem cells in the red bone marrow (see Figure 2) in response to hormones, much as red blood cells form from precursors upon stimulation from erythropoietin. The hormones that affect leukocyte development fall into two groups—interleukins and colony-stimulating factors (CSFs). Interleukins are numbered, while most colony stimulating factors are named for the cell population they stimulate.
Types of white blood cells
All white blood cells have nuclei, which distinguishes them from the other blood cells, the anucleated red blood cells and platelets. They differ in size, the nature of their cytoplasm, the shape of the nucleus, and their staining characteristics, and they are named for these distinctions. Two pairs of broadest categories classify them either by structure (granulocytes or agranulocytes) or by cell division lineage (myeloid cells or lymphoid cells) (see Figure 3). These broadest categories can be further divided into the five main types: neutrophils, eosinophils, basophils, lymphocytes, and monocytes 5. These types are distinguished by their physical and functional characteristics. Monocytes and neutrophils are phagocytic. Further subtypes can be classified; for example, among lymphocytes, there are B cells, T cells, and NK (natural killer) cells.
Normally, five types of white blood cells are in circulating blood. For example, leukocytes with granular cytoplasm are called granulocytes, whereas those without cytoplasmic granules are called agranulocytes (see Figure. 3).
A typical granulocyte is about twice the size of a red blood cell. Members of this group include neutrophils, eosinophils, and basophils. Granulocytes develop in red bone marrow as do red blood cells, but they have short life spans, averaging about 12 hours.
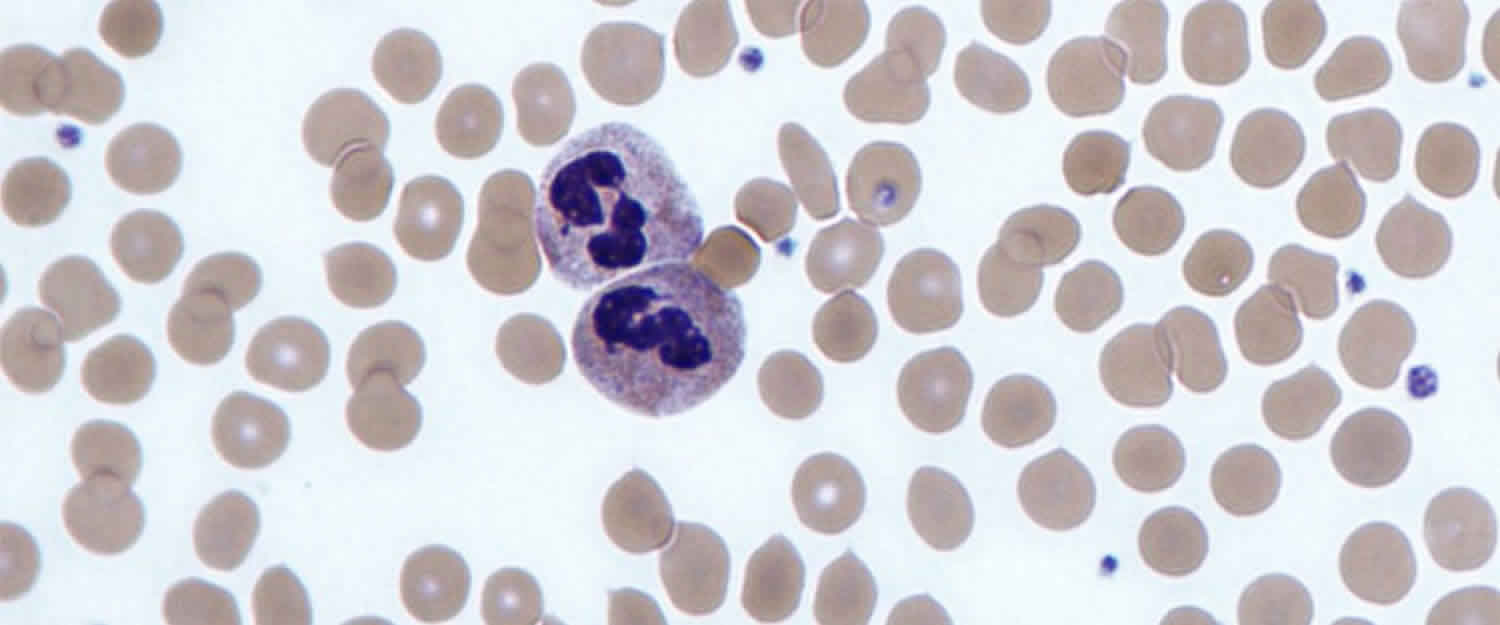
Neutrophils have fine cytoplasmic granules that appear light purple in neutral stain. The nucleus of an older neutrophil is lobed and consists of two to five sections (segments, so these cells are sometimes called segs) connected by thin strands of chromatin (Figure 4). Younger neutrophils are also called bands because their nuclei are C-shaped. Neutrophils account for 54% to 62% of the leukocytes in a typical blood sample from an adult.
Eosinophils contain coarse, uniformly sized cytoplasmic granules that appear deep red in acid stain (Figure 4). The nucleus usually has only two lobes (termed
bilobed). Eosinophils make up 1% to 3% of the total number of circulating leukocytes.
Basophils are similar to eosinophils in size and in the shape of their nuclei, but they have fewer, more irregularly shaped cytoplasmic granules that appear deep
blue in basic stain (Figure 4). Basophils usually account for less than 1% of the circulating leukocytes.
The leukocytes of the agranulocyte group include monocytes and lymphocytes. Monocytes generally arise from red bone marrow. Lymphocytes are formed in the organs of the lymphatic system, as well as in the red bone marrow.
Monocytes, the largest blood cells, are two to three times greater in diameter than red blood cells. Their nuclei are round, kidney-shaped, oval, or lobed. They usually make up 3% to 9% of the leukocytes in a blood sample and live for several weeks or even months.
Lymphocytes are only slightly larger than red blood cells. A typical lymphocyte has a large, round nucleus surrounded by a thin rim of cytoplasm. These cells account for 25% to 33% of circulating leukocytes. Lymphocytes may live for years.
Figure 1. Blood composition
Note: Blood is a complex mixture of formed elements in a liquid extracellular matrix, called blood plasma. Note that water and proteins account for 99% of the blood plasma.
Note: Blood consists of a liquid portion called plasma and a solid portion (the formed elements) that includes red blood cells, white blood cells, and platelets. When blood components are separated by centrifugation, the white blood cells and platelets form a thin layer, called the “buffy coat,” between the plasma and the red blood cells, which accounts for about 1% of the total blood volume. Blood cells and platelets can be seen under a light microscope when a blood sample is smeared onto a glass slide.
Normal Leukocyte Life Cycle and Responses
The life cycle of leukocytes includes development and differentiation, storage in the bone marrow, margination within the vascular spaces, and migration to tissues. Stem cells in the bone marrow produce cell lines of erythroblasts, which become red blood cells; megakaryoblasts, which become platelets; lymphoblasts; and myeloblasts. Lymphoblasts develop into various types of T and B cell lymphocytes. Myeloblasts further differentiate into monocytes and granulocytes, a designation that includes neutrophils, basophils, and eosinophils (Figure 2 and 3). Once white blood cells have matured within the bone marrow, 80% to 90% remain in storage in the bone marrow. This large reserve allows for a rapid increase in the circulating white blood cell count within hours. A relatively small pool (2% to 3%) of leukocytes circulate freely in the peripheral blood 6; the rest stay deposited along the margins of blood vessel walls or in the spleen. Leukocytes spend most of their life span in storage. Once a leukocyte is released into circulation and peripheral tissues, its life span ranges from two to 16 days, depending on the type of cell.
Figure 2. Bone marrow anatomy
Anatomy of the bone. The bone is made up of compact bone, spongy bone, and bone marrow. Compact bone makes up the outer layer of the bone. Spongy bone is found mostly at the ends of bones and contains red marrow. Bone marrow is found in the center of most bones and has many blood vessels. There are two types of bone marrow: red and yellow. Red marrow contains blood stem cells that can become red blood cells, white blood cells, or platelets. Yellow marrow is made mostly of fat.
Figure 3. White blood cells development. A blood stem cell goes through several steps to become a red blood cell, platelet, or white blood cell
Figure 4. White blood cells
Agranulocytosis signs and symptoms
People with agranulocytosis are more likely to have fevers, sore throat, mouth ulcers and infections.
Signs of an infection may include:
- high temperature of 100.4 °F (38 °C) or above
- chills and shivering
- sore throat
- mouth sores that keep returning
- toothache
- skin rashes
- tiredness
- flu-like symptoms
Occasionally, infections can lead to a life-threatening condition called sepsis.
Agranulocytosis causes
Common causes of agranulocytosis include:
- Cancer treatment, like radiotherapy and chemotherapy
- Anti-psychotic drugs e.g. clozapine 7
- Medication for an overactive thyroid e.g., methimazole, carbimazole and propylthiouracil 8
- Some cancers, like leukemia
- Infections such as HIV or hepatitis
- Autoimmune disorders, like rheumatoid arthritis
- Bone marrow diseases, such as myelodysplasia or large granular lymphocyte leukemia
- Certain medicines used to treat diseases, including cancer and inflammation e.g. antibiotics (β-lactam and cotrimoxazole), antiplatelet agenst (ticlopidine), antithyroid drugs, sulfasalazine, neuroleptics (clozapine), antiepileptic agents (carbamazepine), nonsteroidal anti-inflammatory agents and dipyrone 9.
- Certain street drugs e.g., cocaine
- Poor nutrition
- Preparation for bone marrow transplant
- Problem with genes
Some groups, such as people of Afro-Caribbean and Middle Eastern descent, often have a low white blood cell count but this is normal and doesn’t increase their risk of infections.
Agranulocytosis diagnosis
A blood differential test will be done to measure the percentage of each type of white blood cell in your blood.
Agranulocytosis treatment
Treatment depends on the cause of the low white blood cell count. Your treatment will depend on what is causing your condition and will often include antibiotics. For example, if a medicine is the cause, stopping or changing to another drug may help. In other cases, medicines to help the body make more white blood cells will be used.
You may also need specific treatment:
- to boost your white blood cells
- if you’ve got an infection
- Andres E. & Maloisel F. Idiosyncratic drug‐induced agranulocytosis or acute neutropenia. Curr. Opin. Hematol. 15, 15–21.2008 https://www.ncbi.nlm.nih.gov/pubmed/18043241
- Severe congenital neutropenia. https://ghr.nlm.nih.gov/condition/severe-congenital-neutropenia
- Congenital Neutropenia Syndromes. https://www.niaid.nih.gov/diseases-conditions/congenital-neutropenia-syndromes
- Maton, D., Hopkins, J., McLaughlin, Ch. W., Johnson, S., Warner, M. Q., LaHart, D., & Wright, J. D., Deep V. Kulkarni (1997). Human Biology and Health. Englewood Cliffs, New Jersey, US: Prentice Hall. ISBN 0-13-981176-1.
- LaFleur-Brooks, M. (2008). Exploring Medical Language: A Student-Directed Approach (7th ed.). St. Louis, Missouri, US: Mosby Elsevier. p. 398. ISBN 978-0-323-04950-4.
- Cerny J, Rosmarin AG. Why does my patient have leukocytosis? Hematol Oncol Clin North Am. 2012;26(2):303–319, viii.
- Worldwide Differences in Regulations of Clozapine Use. Nielsen J, Young C, Ifteni P, Kishimoto T, Xiang YT, Schulte PF, Correll CU, Taylor D. CNS Drugs. 2016 Feb; 30(2):149-61. https://www.ncbi.nlm.nih.gov/pubmed/26884144/
- He Y, Zheng J, Zhang Q, et al. Association of HLA-B and HLA-DRB1 polymorphisms with antithyroid drug-induced agranulocytosis in a Han population from northern China. Scientific Reports. 2017;7:11950. doi:10.1038/s41598-017-12350-2. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5607267/
- Andres E. & Maloisel F. Idiosyncratic drug‐induced agranulocytosis or acute neutropenia. Curr. Opin. Hematol. 15, 15–21, 2008. https://www.ncbi.nlm.nih.gov/pubmed/18043241