What is albinism
Albinism is a group of genetic conditions where people are born without the usual pigment (melanin) in the skin, hair and eyes. Melanin also plays a role in the development of certain optical nerves, so all forms of albinism cause problems with the development and function of the eyes.
So most people with albinism have very pale skin, hair, and eyes. Albinism symptoms can include light skin or changes in skin color; very white to brown hair; very light blue to brown eye color that may appear red in some light and may change with age; sensitivity to sun exposure; and increased risk of developing skin cancer 1. Albinism is caused by mutations in one of several genes, and most types are inherited in an autosomal recessive manner 2. Although there’s no cure, people with the disorder can take steps to improve vision and avoid too much sun exposure 3. Albinism can affect people of all races, and there are different kinds of albinism.
The genes for albinism are passed down from both parents, who may not be directly affected by it themselves. However, there is no simple test to determine whether a person carries a gene for albinism.
In the United States, most people with albinism live normal life spans and have the same types of general medical problems as the rest of the population. The lives of people with Hermansky-Pudlak Syndrome can be shortened by lung disease or other medical problems.
In tropical countries, people with albinism who do not have access to adequate skin protection may develop life-threatening skin cancers. If they use appropriate skin protection, such as broad spectrum sunscreens rated SPF 30 or higher and opaque clothing, people with albinism can enjoy outdoor activities even in summer.
People with albinism are just like anyone else, with the same lifespan and ability to reach their goals. But living with any medical condition can be difficult. People with albinism can also suffer from discrimination and social stigmatization. People with albinism are at risk of isolation because the condition is often misunderstood. Good support for all involved can help deal with it. Because the social scene can be more about fitting in than standing out, teens with albinism may face bullying or prejudice. Voicing any frustration or sadness to a family member or friend who understands can help. So can talking to a counselor or therapist to get ideas on coping with the challenges that come up during the teen years. Families and schools must also make an effort to include children with albinism in group activities. Contact with others with albinism or who have albinism in their families or communities is most helpful. National Organization for Albinism and Hypopigmentation 4 can provide the names of contacts in many regions of the country.
It is important for people with albinism to protect their skin and eyes from the sun, and have their eyes checked regularly.
Impact on eye development
Regardless of which gene mutation is present, vision impairment is a key feature of all types of albinism. These impairments are caused by irregular development of the optic nerve pathways from the eye to the brain and from abnormal development of the retina.
Except for eye problems, most people with albinism are just as healthy as anyone else. In very rare cases a person’s albinism is part of another condition that involves other health problems in addition to albinism. People with these types of albinism can have such health complications as bleeding, lung, bowel, and immune system problems.
If your child lacks pigment in his or her hair or skin at birth that affects the eyelashes and eyebrows — as is often the case in infants with albinism — your doctor will likely order an eye exam and closely follow any changes in your child’s pigmentation.
For some infants, the first sign of albinism is poor visual tracking. This may be followed at 3 to 4 months of age by rapid back-and-forth shifting (nystagmus) in the eyes. If you observe these signs in your baby, talk to your doctor.
Contact your doctor if your child with albinism experiences frequent nosebleeds, easy bruising or chronic infections. These signs and symptoms may indicate the presence of Hermansky-Pudlak or Chediak-Higashi syndromes, which are rare but serious genetic disorders.
Melanin biosynthesis
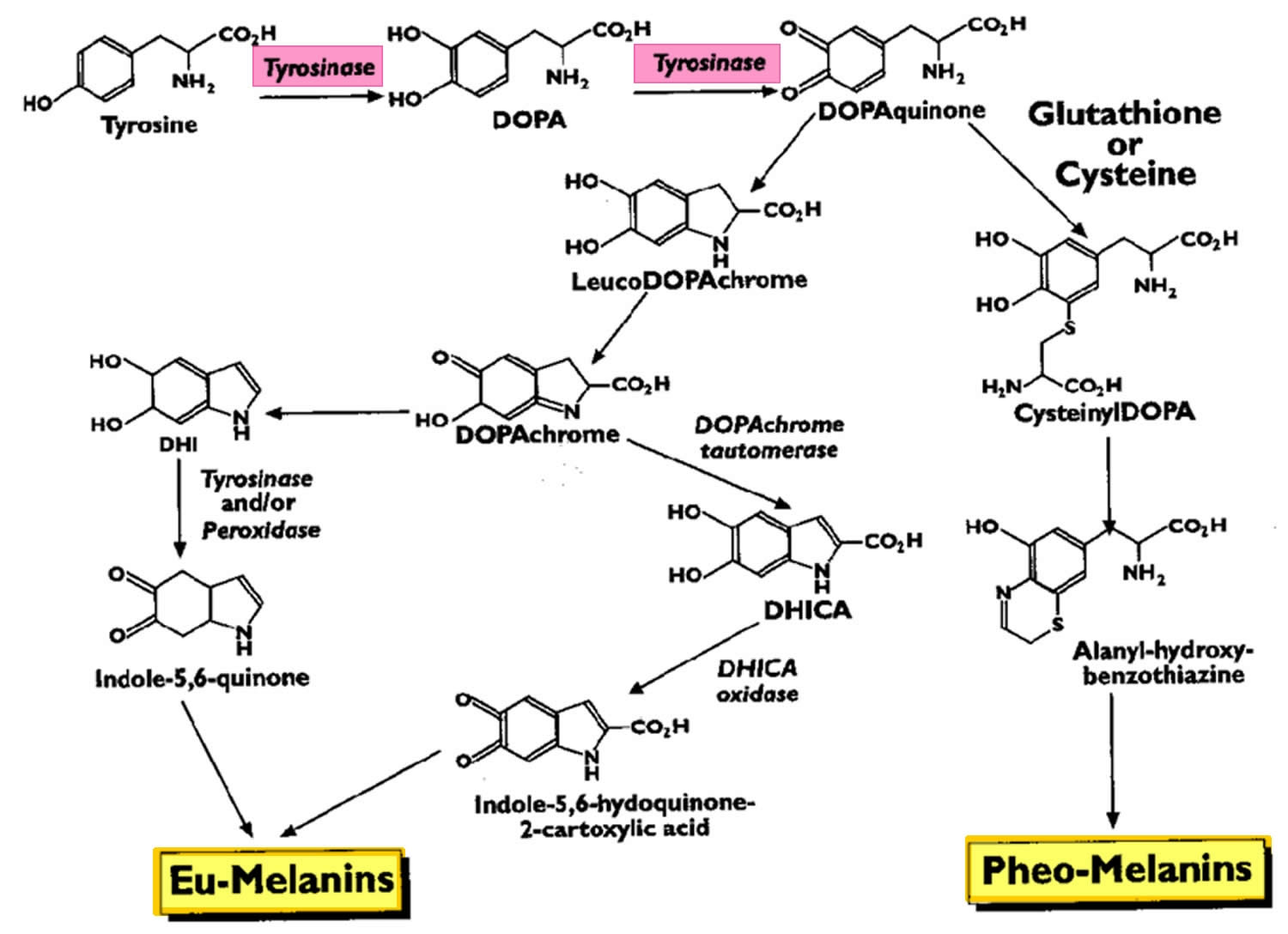
In humans, melanin exists as three forms: eumelanin (which is subdivided further into black and brown forms), pheomelanin, and neuromelanin 5. Eumelanin and pheomelanin are produced in various amounts in the basal layer of the epidermis within cells called melanocytes. The first step of biosynthesis of both eumelanin and pheomelanin begins the same way. Tyrosine is converted into dihydroxyphenylalanine (DOPA), which requires tyrosine hydroxylase and tetrahydrobiopterin as a cofactor. The enzyme tyrosinase then converts dihydroxyphenylalanine into dopaquinone, which can follow a variety of pathways to form the eumelanin or pheomelanin (Figure 1).
The primary stimulus for melanogenesis and subsequent melanosome production is ultraviolet (UV) radiation, which upregulates melanocyte production of pro-opiomelanocortin (POMC) and its downstream products, alpha-melanocyte-stimulating hormone (alpha-MSH) and adrenocorticotropic hormone (ACTH) 5. The overall effect is to increase eumelanin production. Interestingly, people with pro-opiomelanocortin mutations have red hair and Fitzpatrick skin type 1 due to the relative increase in pheomelanin to eumelanin expression.
Neuromelanin is a dark pigment produced by dopaminergic and noradrenergic cells of the substantia nigra and locus coeruleus as a breakdown product of dopamine 6.
Figure 1. Melanin biosynthesis
[Source 7 ]Melanin function
In its various forms, melanin fulfills a variety of biological functions, including skin and hair pigmentation and photoprotection of the skin and eye.
Pigmentation of the skin results from the accumulation of melanin-containing melanosomes in the basal layer of the epidermis. Differences in skin pigmentation result both from the relative ratio of eumelanin (brown–black) to pheomelanin (yellow–red), as well as the number of melanosomes within melanocytes. Pheomelanin accounts for the pinkish skin constituting the lips, nipples, vagina, and glans of the penis. In general, lightly pigmented skin tends to contain melanocytes with clusters of two to three melanosomes, whereas darkly pigmented skin tends to contain individual melanosomes which can melanize neighboring keratinocytes more readily. The overall melanin density correlates with the darkness of skin as well as Fitzpatrick skin type.
The interplay between melanin and UV radiation is complex. Researchers widely believe that melanin production in melanocytes increased as an evolutionary adaptation to the widespread loss of human body hair more than a million years ago. Populations living closer to the equator tended to develop a greater proportion of eumelanin, which is a UV–absorbent, antioxidant, and free radical scavenger. Conversely, populations living further from the equator are relatively richer in pheomelanin, which produces free radicals in response to UV radiation, accelerating carcinogenesis. As the main stimulus for cutaneous vitamin D production is UV light exposure, it follows that dark-skinned individuals also tend to have lower levels of vitamin D and should be screened accordingly.
Less clear is the link between melanin, the sun, and cutaneous immunology. Both acute and chronic UV light exposure induces immunosuppression; UVA light is used therapeutically for a large number of skin conditions, including psoriasis. Intriguingly, melanin is believed to have immunomodulatory and even anti-bacterial properties, although the underlying mechanisms have not yet been fully elucidated. Malignant melanocytes rich in melanin are less sensitive to chemo-, radio-, or photodynamic therapy, and amelanotic melanomas have longer disease-free and overall survival than melanotic ones. Therefore, some have suggested inhibition of melanogenesis as a therapy for malignant melanoma.
Just as melanin protects the skin from photodamage, it also protects the eye. Melanin is concentrated in the iris and choroid, and those with grey, blue, and green eye colors, as well as albinos, have more sun-related ocular issues.
Hair color is determined by the relative proportion of various forms of melanin:
- Black and brown hair results from varying degrees of black and brown eumelanin
- Blonde hair results from a small amount of brown eumelanin in the absence of black eumelanin
- Red hair results from roughly equal amounts of pheomelanin as eumelanin. Strawberry blonde hair results from brown eumelanin in the presence of pheomelanin.
Complications of albinism
Complications of albinism include skin disorders as well as social and emotional challenges.
Eye complications
People with albinism may be legally blind, but they can learn to use their vision over time. Problems with vision can impact learning, employment and the ability to drive. Some people may be able to correct problems with astigmatism, farsightedness and nearsightedness with eyeglasses or contacts.
Skin complications
People with albinism have skin that is very sensitive to light and sun exposure. Sunburn is one of the most serious complications associated with albinism because it can increase the risk of developing skin cancer and sun damage-related thickening of the skin.
Social and emotional challenges
Some people with albinism may experience discrimination. People with albinism are at an increased risk of isolation due to the social stigma behind the condition. The reactions of other people to those with albinism can often have a negative impact on people with the condition.
The reactions of other people to those with albinism can often have a negative impact on people with the condition.
- Children with albinism may experience name-calling, bullying, teasing or questions regarding their appearance, eyewear or visual aid devices.
- Many people with albinism find the word “albino” hurtful because they’re being labeled simply on the basis of looks rather than being thought of as individuals. Using the term “person with albinism” is preferred to avoid the stigma of other terms.
- People with albinism usually look very different from members of their own families or ethnic groups, so they may feel like outsiders or be treated like outsiders.
All of these factors may contribute to social isolation, poor self-esteem and stress.
Types of albinism
There are several different types of albinism. Levels of pigmentation vary depending on which type of albinism you have. The different types of albinism include:
- Oculocutaneous albinism (OCA): Oculocutaneous albinism or OCA, is the most common type of albinism. People with oculocutaneous albinism (OCA) have extremely pale hair, skin and eyes. There are seven different subtypes of oculocutaneous albinism (OCA), caused by mutations in one of seven genes (OCA1 to OCA7).
- Ocular albinism: Ocular albinism or OA, is much less common than oculocutaneous albinism (OCA). Ocular albinism affects only your eyes. People with ocular albinism usually have blue eyes. Sometimes your irises (colored part of your eyes) are very pale, so your eyes may appear red or pink. This is because the blood vessels inside your eyes show through the irises. Your skin and hair color are usually normal.
- Hermansky-Pudlak syndrome: Hermansky-Pudlak syndrome or HPS, is a type of albinism that includes a form of oculocutaneous albinism (OCA) along with blood disorders, bruising issues and lung, kidney or bowel diseases.
- Chediak-Higashi syndrome: Chediak-Higashi syndrome (CHS) is a type of albinism that includes a form of oculocutaneous albinism (OCA) along with immune and neurological issues.
Oculocutaneous albinism (OCA)
Oculocutaneous albinism or OCA, involves dilution of the color of the hair, skin and eyes and is the most common type of albinism. People with oculocutaneous albinism (OCA) have white or light-colored hair, very fair skin and eyes. Long-term sun exposure greatly increases the risk of skin damage and skin cancers, including an aggressive form of skin cancer called melanoma, in people with this condition. Oculocutaneous albinism (OCA) also reduces pigmentation of the colored part of the eye (the iris) and the light-sensitive tissue at the back of the eye (the retina). People with this condition usually have vision problems such as reduced sharpness; rapid, involuntary eye movements (nystagmus); and increased sensitivity to light (photophobia).
Over the years, researchers have identified multiple types of oculocutaneous albinism (OCA), which are distinguished by their specific skin, hair, and eye color changes and by their genetic cause. Oculocutaneous albinism type 1 is characterized by white hair, very pale skin, and light-colored irises. Type 2 is typically less severe than type 1; the skin is usually a creamy white color and hair may be light yellow, blond, or light brown. Type 3 includes a form of albinism called rufous oculocutaneous albinism, which usually affects dark-skinned people. Affected individuals have reddish-brown skin, ginger or red hair, and hazel or brown irises. Type 3 is often associated with milder vision abnormalities than the other forms of oculocutaneous albinism. Type 4 has signs and symptoms similar to those seen with type 2. In general, these systems contrasted types of albinism having almost no pigmentation with types having slight pigmentation. In less pigmented types of albinism, hair and skin are cream-colored and vision is often in the range of 20/200. In types with slight pigmentation, hair appears more yellow or has a reddish tinge and vision may be better.
DNA tests can determine the precise type of albinism. Research on albinism genes is ongoing. To date there are seven different subtypes of oculocutaneous albinism (OCA) caused by mutations in one of seven genes – OCA1, OCA2, OCA3, OCA4, OCA5, OCA6 and OCA7. Some are further divided into subtypes. Oculocutaneous albinism type 1 (OCA-1) and type 2 (OCA-2) are the most common types of oculocutaneous albinism. All seven types of oculocutaneous albinism (OCA) are inherited in an autosomal recessive manner and are thus found in both males and females, which is in contrast to that of X-linked recessive inheritance of ocular albinism (OA). Ocular nystagmus is seen in virtually all forms of oculocutaneous albinism (OCA) 8.
Researchers have also identified several other genes that result in albinism with other features. One group includes at least 10 genes leading to Hermansky-Pudlak Syndrome (HPS). In addition to albinism, Hermansky-Pudlak Syndrome (HPS) is associated with bleeding problems and bruising. Some forms are also associated with lung and bowel disease. Hermansky-Pudlak Syndrome (HPS) is a less common form of albinism but should be suspected if a person with albinism shows unusual bruising or bleeding or if a genetic test for a type of OCA produces inconclusive results.
Other albinism-related syndromes include Chediak-Higashi syndrome and Griscelli syndrome.
Overall, an estimated 1 in 20,000 people worldwide are born with oculocutaneous albinism (OCA). The condition affects people in many ethnic groups and geographical regions. Types 1 and 2 are the most common forms of this condition; types 3 and 4 are less common. Type 2 occurs more frequently in African Americans, some Native American groups, and people from sub-Saharan Africa. Type 3, specifically rufous oculocutaneous albinism, has been described primarily in people from southern Africa. Studies suggest that type 4 occurs more frequently in the Japanese and Korean populations than in people from other parts of the world.
OCA Type 1
OCA1 is also known as tyrosinase-related albinism or tyrosinase-related OCA, constitutes several subtypes that occur due to mutation in TYR gene for tyrosinase (chromosome 11q14-q21) 9. Tyrosinase enzyme catalyzes the first two steps in the melanin biosynthesis pathway, responsible for converting tyrosine to DOPA and subsequently to DOPAquinone (see Figure 1 above). Depending on differential production of the end product melanin, the severity of phenotype varies. A point mutation of TYR gene drives the conformation of the tyrosinase enzyme, which results in either absent or decreased enzyme activity. Almost 200 mutations in TYR gene are known to date.
OCA 1A
OCA 1A was formerly known as “tyrosinase-negative” albinism is due to the tyrosinase enzyme being inactive and no melanin is produced, leading to white hair and very light skin 10. Patients affected by OCA 1A thus have the most profound phenotype of all oculocutaneous albinisms with the greatest risk for skin cancer and highest frequency of visual symptoms and acuity loss. Hair bulbs of the affected individuals remain DOPA-negative throughout their lives, indicating that the tyrosinase activity is fully inactive 11. Due to the relative severity of ocular and dermatologic problems, close ophthalmic and dermatologic care is essential.
OCA 1B
OCA-1B was known as the “yellow variant” albinism due to reduced, but not absent, tyrosinase activity that produce some melanin pigment. Patients with 1B may be indistinguishable from OCA-1A at birth due to lack of any detectable pigment early on 12, but during the first several years of life OCA-1B patients accumulate yellow pigment in their skin, eye, and hair. In OCA1B, the hair may darken to blond, yellow/orange or even light brown, as well as slightly more pigment in the skin. Their vision is moderately to severely reduced.
OCA 1MP
OCA 1MP stands for “OCA 1 Mimal Pigment.” King et al in 1986 13 first proposed oculocutaneous albinism (OCA) minimal pigment as a subtype of OCA-1 by showing disordered TYR activity and clinically detectable accumulation of pigment only in the irises that increases with age. The most recent update of the definition proposed by Kono et al 14 claimed that the sites of pigment accumulation include hair and lentigo. With life-long negative DOPA staining of hair bulbs, however, OCA-1MP phenotype contrasts with OCA-1B that has positive DOPA staining.
OCA 1 TS
OCA 1 TS is the Temperature Sensitive albinism that earned its name from variable tyrosinase activity depending on skin temperature. In this subtype, tyrosinase activity is inversely proportional to temperature, leading to dark hair on the cooler extremities but white hairs near the body core such as the armpits, pubic area, and scalp. As in OCA-1B, the patients can be indistinguishable at birth from OCA-1A 12.
OCA Type 2
OCA type 2 (OCA-2) is the most common type of albinism throughout the world with the highest frequency in equatorial Africa 15. The characteristic gene involvement for OCA-2 is the OCA2 gene, previously known as P gene. OCA2 gene is responsible for melanosome function as it helps regulate the influx of tyrosine and other internal environment of the melanosome thus affecting the functionality of the organelle and melanin production. Of note, non-pathologic polymorphisms of the OCA2 contribute to iris colors in normal individuals 12. This disorder is generally a milder form of OCA type 1 (OCA-1), with skin pigmentation ranging from white to fair; hair color ranging from yellow to even black; and generally milder visual dysfunction compared to OCA type 1 (OCA-1). At times the affected individual may be indistinguishable from having OCA-1B and OCA-1MP 16. Interestingly, about 1% of patients with either Prader-Willi syndrome or Angelman syndrome are hypopigmented though often without ocular features of albinism. This phenomenon is due to the position of the OCA2 gene between the genes whose deletions are responsible for the two syndromes 17.
OCA 2 Brown Albinism (BOCA or brown oculocutaneous albinism) is a part of the clinical spectrum of OCA type 2 (OCA-2). This variant of OCA type 2 (OCA-2) was initially identified in Africans of Nigerian and Ghanan ancestry and in and African Americans with light brown hair and skin 18. OCA 2 Brown Albinism (BOCA) patients can present anywhere between the classic phenotype (yellow/blond hair, creamy skin, blue/hazel irides) to brown-pigmentation. Affected individuals from other ethnic groups can have moderate to near-normal skin pigmentation 19.
OCA Type 3
OCA 3 occurs due to a mutation in TYRP1 (tyrosinase-related protein) gene. This subtype of OCA is seen in African-born blacks but rarely in other ethnicities 20. Phenotypes overlap with OCA-2 Brown Albinism (BOCA or brown oculocutaneous albinism) and with red/rufous OCA (ROCA) 21, although as the phenotype names imply, the BOCA can be differentiated from ROCA based on skin and hair color. ROCA phenotype is characterized by red-bronze skin color, ginger hair, and blue or brown irises 22. Studies have since shown that TYRP1 contributes to melanin synthesis as well as melanocyte proliferation and apoptosis 23.
OCA Type 4
Recessive mutation in membrane-associated transport protein gene (MATP), also known as SLC45A2 , is responsible for OCA type 4. Although the gene was first identified in a Turkish patient 24, it has since been found in albino subjects in Japan and elsewhere in Europe as well. This is the third most common type of OCA after OCA2 and OCA1 25.
OCA Type 5
A new OCA gene called OCA5 was found to be responsible for the typical OCA phenotype in a consanguinous Pakistani family 26. This gene is mapped onto chromosome 4q24 and the genotype was designated OCA 5. Further studies on this gene are underway.
OCA Type 6
In 2013, a Chinese group of researchers, Wei et al 27 found mutations in SLC24A5 on 15q21.1 among patients of Chinese origin who presented with characteristic phenotype of non-syndromic OCA. This gene, previously studied but not linked directly to OCA phenotype, is believed to impair or disrupt melanosomal maturation 28. OCA due to mutation in SLC24A5 gene has been since termed OCA type 6. Morice-Picard et al 29 have since shown that this mutation is seen in different ethnic groups, indicating that the mutation is not limited to the Chinese population.
OCA Type 7
As the latest addition to the subtype of oculocutaneous albinism (OCA), OCA type 7 was identified in 2013 by Karen Grønskov and Thomas Rosenberg based on homozygosity mapping and gene sequencing of a consanguineous family with oculocutaneous albinism (OCA) symptoms on the Faroe Islands of Denmark 28. The probands as well as unrelated but affected individuals on the island had homozygous non-sense mutation in C10orf11, a previously unknown gene that has been since shown to contribute to melanocyte differentiation. Production of OCA phenotype due to this gene mutation is thus termed OCA type 7 30.
Ocular albinism (OA)
Ocular albinism (OA) is much less common than oculocutaneous albinism (OCA), accounting for 10-15% of all albinism cases. Ocular albinism affects only your eyes with melanin pigment mainly missing from the eyes while the skin and hair appear normal or only slightly lighter. Ocular albinism (OA) reduces the coloring (pigmentation) of the iris, which is the colored part of the eye, and the retina, which is the light-sensitive tissue at the back of the eye. People with ocular albinism (OA) usually have blue eyes. Sometimes your irises (colored part of your eyes) are very pale, so your eyes may appear red or pink. This is because the blood vessels inside your eyes show through the irises. Your skin and hair color are usually normal.
Ocular albinism is characterized by severely impaired sharpness of vision (visual acuity) and problems with combining vision from both eyes to perceive depth (stereoscopic vision). Although the vision loss is permanent, it does not worsen over time. Other eye abnormalities associated with this condition include rapid, involuntary eye movements (nystagmus); eyes that do not look in the same direction (strabismus); and increased sensitivity to light (photophobia). Many affected individuals also have abnormalities involving the optic nerves, which carry visual information from the eye to the brain.
Unlike some other forms of albinism, ocular albinism (OA) does not significantly affect the color of the skin and hair. People with ocular albinism may have a somewhat lighter complexion than other members of their family, but these differences are usually minor.
There are two known types of ocular albinism (OA) without cutaneous involvement. The most common form of ocular albinism is known as the Nettleship-Falls ocular albinism or ocular albinism type 1 (OA-1). Other forms of ocular albinism are much rarer and may be associated with additional signs and symptoms, such as hearing loss.
The most common form of this disorder, ocular albinism type 1 (OA-1), affects at least 1 in 60,000 males. The classic signs and symptoms of this condition are much less common in females.
OA Type 1
Ocular albinism type 1 (OA-1) also known as Nettleship-Falls ocular albinism, is inherited in an X-linked recessive manner and thus occurs only in boys. Ocular albinism type 1 (OA-1) is the most common form of ocular albinism representing 10% of all albinism and estimated prevalence of 1 in 50,000 to 150,000 live births 31. Mutations in GPR143 gene at Xp22.3-22.2 are known to be causative 32. The affected gene codes for intracellular GPCR (G-protein coupled receptor) that controls the melanosome transport in pigment cells, disruption of which affects the number and size of the melanosomes. OA1 patients produce macromelanosomes seen on skin biopsy 12.
The clinical manifestation of OA1 depend on the ethnic background of the individual, with those who are of darkly pigmented background being less severely affected than those from light pigmentation groups 33. Albinism of the eye with OA tends to be severe with poor vision. Diagnostic methods include molecular analysis of OA1 gene (GPR143), family pedigree analysis, and examination of the carrier mother. Due to lyonization of one X chromosome in each somatic cell, carrier females may exhibit evidence of speckled albinism. In up to 90% of carrier females, mud-splattered fundus is seen 34 due to the patchy dissemination of amelanotic patches of retinal pigment epithelium (RPE) among melanotic patches. Other potential findings are iris transillumination in 75%, hypopigmented macules of the skin, and biopsy evidence of macromelanosomes in those skin segments 35. Of note, OA1 has been associated with late-onset sensorineural deafness (OASD) 36. The syndrome is likely the consequence of a contiguous gene defect that includes OA1 gene. Late-onset sensorineural deafness (OASD) shares similarities but is but etiologically distinct from Waardenburg syndrome, which is characterized by patchy depigmentation of hair and skin, heterochromia irides, and congenital deafness 37.
OA Type 2
Ocular albinism type 2 (OA-2) also known as Aland Island eye disease or Forsius-Eriksson type ocular albinism, is a rare X-linked disorder with similar clinical manifestations as OA1 with the additional protan color vision defect and defective dark adaptation. In addition to such differences, biopsy examination of skin samples from OA2 individuals revealed that OA2 is morphologically distinct from OA1 38. Additionally, female carriers of OA2 do not exhibit characteristic fundus pattern seen in those of OA1 carriers. Based on molecular analysis, the defective gene that gives rise to this disorder is likely in Xp21.3-p21.2 for CACNA1F gene 39. The clinical findings, however, overlap with congenital stationary night blindness (CSNB2A). Due to similar features of OA2 and CSNB2A, Hawksworth et al 40 raised the question of whether these two entities are the same.
Hermansky-Pudlak Syndrome
Ocular albinism is a component of Hermansky-Pudlak syndrome (HPS), a rare autosomal recessive disorder that is further characterized by bleeding tendency due to platelet storage deficiency, interstitial lung disease, and granulomatous colitis (depending on the subtype) 41. Hermansky-Pudlak syndrome (HPS) is believed to be due to an abnormality in the formation of intracellular vesicles such as melanosomes and the dense bodies of platelets most commonly due to a mutation in HPS1 gene on chromosome 10 12. Because Hermansky-Pudlak syndrome (HPS) is seen most commonly among those of Swiss or Puerto Rican descent at the prevalence of 1:1800, it should be suspected in patients with albinism with the relevant ethnic background plus the associated systemic symptoms 42.
Chediak-Higashi Syndrome
Chediak-Higashi syndrome (CHS) is a rare autosomal recessive disorder boasts less than 500 reported cases in the literature in the past 20 years 43 and is among the triad of rare diseases grouped together as “silvery hair syndromes” 44. Chediak-Higashi syndrome (CHS) presents with variable but often intermediate form of hypopigmentation recurrent severe pyogenic infections that is ultimately lethal accompanied by progressive neurologic abnormalities, coagulation defects, and mucosal defects such as gingivitis, oral ulcerations, and periodontal diseases . The underlying defect of Chediak-Higashi syndrome (CHS) is a mutation in the lysosomal trafficking regulator in the CHS1/LYST gene 43. The resultant abnormal protein trafficking leads to dysfunctional fusion of vesicles and failure of transport of lysosomes to the appropriate intracellular site. The diagnosis should be considered in a young patient—many patients do not live past early childhood—presenting with oculocutaneous albinism (OCA) with the aforementioned systemic symptoms. Blood smear showing giant azurophilic granules in neutrophils, eosinophils, and other granulocytes is pathognomonic for Chediak-Higashi syndrome (CHS) 45. Bone marrow transplant is curative in some patients 46.
Griscelli Syndrome
Another member of the silvery hair syndrome triad, Griscelli syndrome (GS) is a rare autosomal-recessive disorder that results in hypopigmentation of skin and hair (silver hair), neurologic deficit, with or without immunologic impairment or hematophagocytic syndrome. The severity of the diseases is determined by the involved gene– MYO5A (GS type 1), RAB27A (GS type 2), and melanophilin (Mlph) (GS type 3). Griscelli syndrome (GS) can be distinguished from Chediak-Higashi syndrome (CHS) due to lack of giant intracellular granules that are seen in Chediak-Higashi syndrome.
Albinism facts
Eyesight and Albinism
People with albinism often have trouble with their eyesight. They may wear glasses or contact lenses to help correct problems like nearsightedness, farsightedness, or astigmatism. Others might need eye surgery. Just as there are different degrees of albinism there are also different levels of eye problems for a person who has the condition.
Albinism does not make a person completely blind. Although some people with albinism are “legally blind,” that doesn’t mean they have lost their vision completely. They can still read and study — they just may need larger print or magnifiers to help them.
People with albinism can be very sensitive to light because the iris doesn’t have enough color to shield the retina properly. Wearing sunglasses or tinted contact lenses can help make them more comfortable out in the sun.
Skin Precautions
Besides giving skin, eyes, and hair their color, melanin helps protect our skin from the sun. It does this by causing skin to tan instead of burn — which is why people with darker skin (more melanin) are less likely to burn than people with lighter skin. So people with albinism can sunburn very easily.
People with light skin are also particularly at risk for skin cancer. So it’s important for people with albinism to use a sunscreen with a high SPF factor at all times and to wear clothing that offers protection from the sun, such as hats, dark-colored clothing, or long pants and long-sleeved shirts.
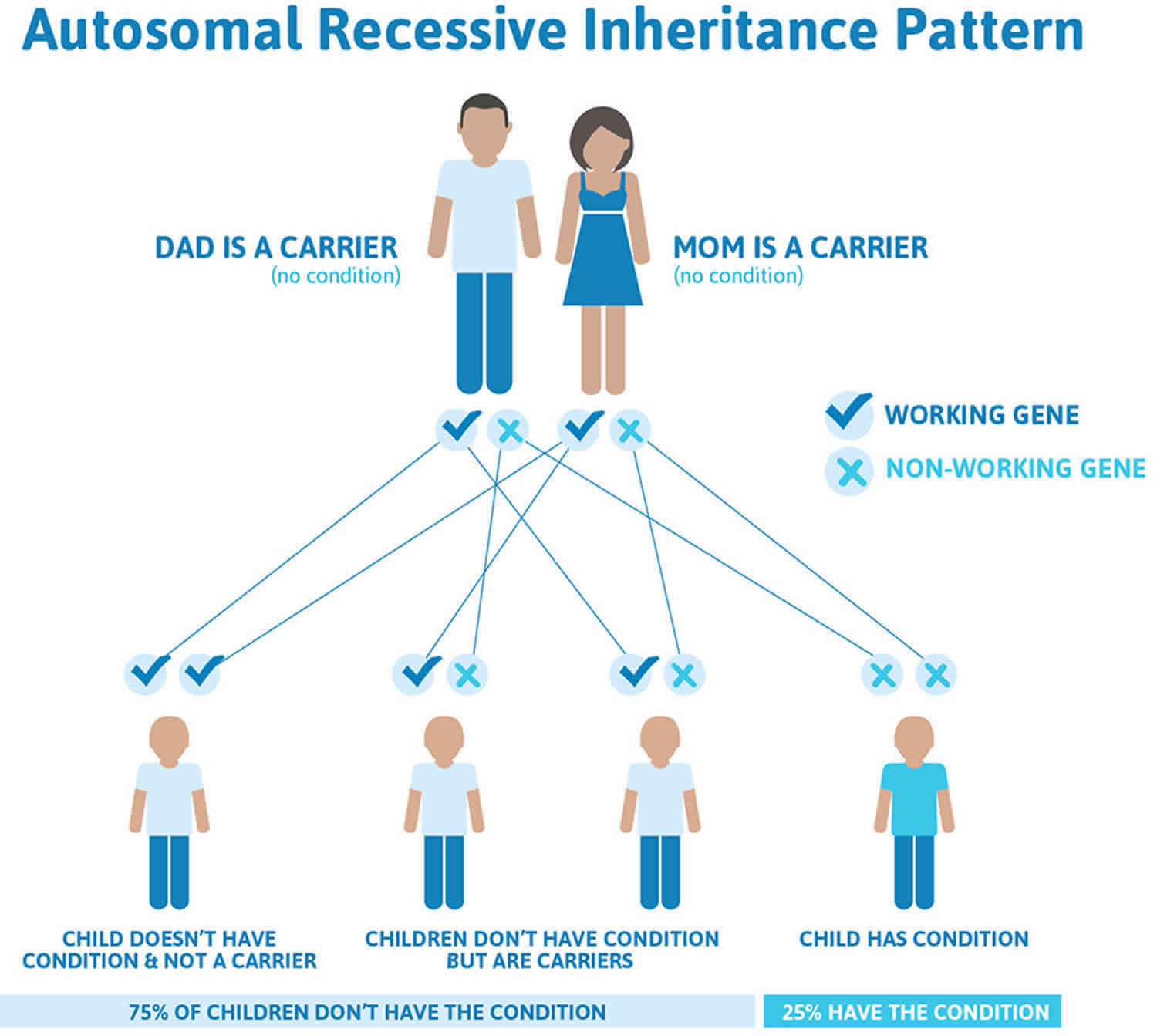
Albinism genetics
The genes for oculocutaneous albinism (OCA) are located on “autosomal” chromosomes. Autosomes are the 22 pairs of chromosomes that contain genes for our general body characteristics, compared to the one pair of sex chromosomes. You normally have two copies of these chromosomes and the many genes on them – one inherited from your father, the other inherited from your mother. For a recessive trait (like most types of albinism) to occur, both of the person’s chromosomes must carry that trait. That means that most types of albinism result from inheriting an albinism trait from both the mother and the father who often have typical pigmentation. In this case, the mother and father are considered to be carriers of the albinism trait because they each carry a recessive gene for the condition but do not manifest the condition themselves. When both parents carry the albinism gene (and neither parent has albinism) there is a one in four chance at each pregnancy that the baby will be born with albinism. This type of inheritance is called “autosomal recessive” inheritance.
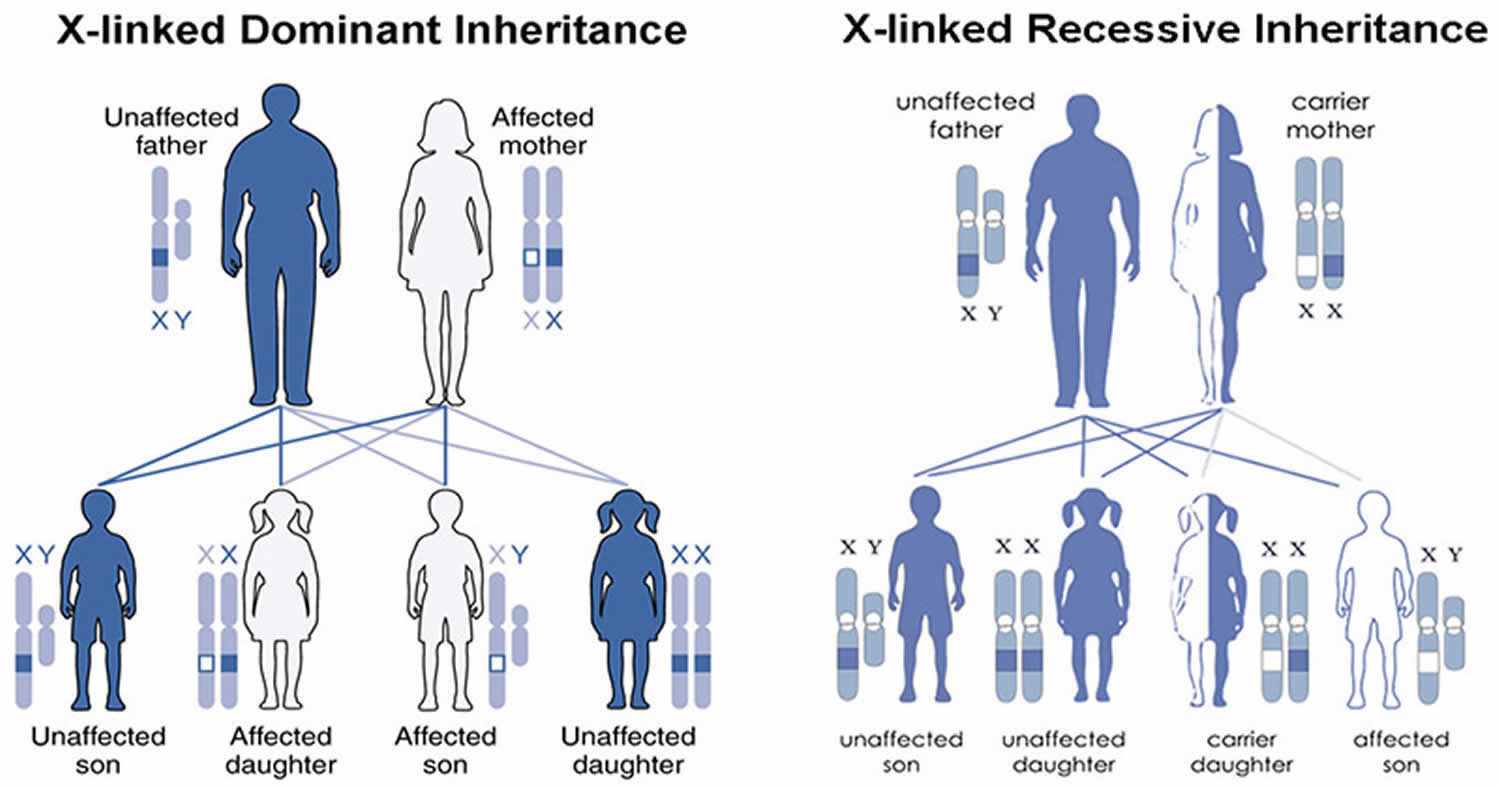
Ocular albinism (OA1) is caused by a change in the GPR143 gene that plays a signaling role that is especially important to pigmentation in the eye. OA1 follows a simpler pattern of inheritance because the gene for OA1 is on the X chromosome. Females have two copies of the X chromosome while males have only one copy (and a Y chromosome that makes them male). To have ocular albinism, a male only needs to inherit one changed copy of the gene for ocular albinism from his carrier mother. Therefore almost all of the people with OA1 are males. Parents should be suspicious if a female child is said to have ocular albinism. While possible if the mother is a carrier of ocular albinism and the father has ocular albinism, it is extremely rare.
For couples who have not had a child with albinism, there is no simple test to determine whether a person carries a gene for albinism. Researchers have analyzed the DNA of many people with albinism and found the changes that cause albinism, but these changes are not always in exactly the same place, even for a given type of albinism. Moreover, many of the tests do not find all possible changes. Therefore, the tests for the albinism gene may be inconclusive. If parents have had a child with albinism previously, and if that affected child has had a confirmed diagnosis by DNA analysis, there is a way to test in subsequent pregnancies to see if the fetus has albinism. The test uses either amniocentesis (placing a needle into the uterus to draw off fluid) or chorionic villous sampling (CVS). Cells in the fluid are examined to see if they have an albinism gene from each parent.
For specific information and genetic testing, seek the advice of a qualified geneticist or genetic counselor. Those considering prenatal testing should be made aware that people with albinism usually adapt quite well to their disabilities and lead very fulfilling lives.
Table 1. Genes associated with albinism
| Full name | Abbreviation | Type | Gene/protein | Locus | Inheritance |
|---|---|---|---|---|---|
| Tyrosine negative | OCA 1A | OCA | Tyrosinase | 11q14-q21 | AR |
| Yellow variant | OCA 1B | OCA | Tyrosinase | 11q14-q21 | AR |
| Minimal pigment | OCA 1MP | OCA | Tyrosinase | 11q14-q21 | AR |
| Temperature sensitive | OCA 1TS | OCA | Tyrosinase | 11q14-q21 | AR |
| OCA Type 2 | OCA 2 | OCA | P gene / OCA2 | 15q11.2-q12 | AR |
| Brown albinism | BOCA | OCA | P gene / OCA2 | 15q11.2-q12 | 15q11.2-q12 |
| OCA Type 3 | OCA 3 / ROCA | OCA | Tyrosinase related protein (TYRP1) | 9p23 | AR |
| OCA Type 4 | OCA 4 | OCA | Membrane-associated transporter protein (MATP) = SLC45A2 | 5p13.3 | AR |
| OCA Type 5 | OCA 5 | OCA | Unknown | 4q24 | AR |
| OCA Type 6 | OCA 6 | OCA | SLC24A5 | 15q21.1 | AR |
| OCA Type 7 | OCA 7 | OCA | C10orf11 | 10q22 | AR |
| Oculoalbinism 1 aka Nettleship-Falls ocular albinism | OA 1 | OA | GPR143 | Xp22.3 | XR |
| Oculoalbinism 2 aka Forsius-Eriksson type ocular albinism | OA 2 | OA | CACNA1F | Xp21.3-p21.2 | XR |
Footnotes: *OMIM indicates Online Mendelian Inheritance in Man
Abbreviations: AD = autosomal dominant; AR = autosomal recessive; OA = ocular albinism; OCA = oculocutaneous albinism; XR = X-linked recessive.
[Source 12 ]People with specific questions about genetic risks or genetic testing for themselves or family members should speak with a genetics professional.
Resources for locating a genetics professional in your community are available online:
- The National Society of Genetic Counselors (https://www.findageneticcounselor.com/) offers a searchable directory of genetic counselors in the United States and Canada. You can search by location, name, area of practice/specialization, and/or ZIP Code.
- The American Board of Genetic Counseling (https://www.abgc.net/about-genetic-counseling/find-a-certified-counselor/) provides a searchable directory of certified genetic counselors worldwide. You can search by practice area, name, organization, or location.
- The Canadian Association of Genetic Counselors (https://www.cagc-accg.ca/index.php?page=225) has a searchable directory of genetic counselors in Canada. You can search by name, distance from an address, province, or services.
- The American College of Medical Genetics and Genomics (http://www.acmg.net/ACMG/Genetic_Services_Directory_Search.aspx) has a searchable database of medical genetics clinic services in the United States.
What causes albinism
Albinism is inherited. Albinism is caused by a genetic mutation that is usually passed from parents to child. Albinism is not contagious — you can’t “catch” it from someone else. People are born with albinism because they inherit an albinism gene or genes from their parents. Mutations in several different genes, on different chromosomes, can cause different types of albinism. A total of 15 genes are currently associated with various types of albinism 25 with as many as 729 mutations reported in the Human Gene Mutation Database associated with any of those loci 47. The mutation disrupts the production of melanin, the pigment that protects the skin from UV rays. Melanin is also important for the proper development of the eye. Without melanin, the retina and the optic nerve may not develop properly. The retina is the light-sensitive tissue lining the back of the eye, and the optic nerve fibers, help relay images to the brain.
Oculocutaneous albinism (OCA) can result from mutations in several genes, including TYR, OCA2, TYRP1, and SLC45A2. Changes in the TYR gene cause OCA type 1; mutations in the OCA2 gene are responsible for OCA type 2; TYRP1 mutations cause OCA type 3; and changes in the SLC45A2 gene result in OCA type 4. Mutations in additional genes likely underlie the other forms of this disorder (see Table 1 below). The genes associated with oculocutaneous albinism (OCA) are involved in producing a pigment called melanin, which is the substance that gives skin, hair, and eyes their color. In the retina, melanin also plays a role in normal vision. Mutations in any of these genes disrupt the ability of cells to make melanin, which reduces pigmentation in the skin, hair, and eyes. A lack of melanin in the retina leads to the vision problems characteristic of oculocutaneous albinism.
Alterations in the MC1R gene can change the appearance of people with oculocutaneous albinism type 2 (OCA-2). This gene helps regulate melanin production and is responsible for some normal variation in pigmentation. People with genetic changes in both the OCA2 and MC1R genes have many of the usual features of oculocutaneous albinism type 2, including light-colored eyes and vision problems; however, they typically have red hair instead of the usual yellow, blond, or light brown hair seen with this condition.
Some individuals with oculocutaneous albinism do not have mutations in any of the known genes. In these people, the genetic cause of the condition is unknown.
Oculocutaneous albinism (OCA) is inherited in an autosomal recessive manner (Figure 2). This means that two mutations are necessary for an individual to have OCA. Individuals normally have two copies of each numbered chromosome and the genes on them – one inherited from the father, the other inherited from the mother. Neither of these gene copies is functional in people with albinism. Each unaffected parent of an individual with an autosomal recessive condition carries one functional copy of the causative gene and one nonfunctional copy. They are referred to as carriers, and do not typically show signs or symptoms of the condition. Both parents must carry a defective OCA gene to have a child with albinism. When two individuals who are carriers for the same autosomal recessive condition have children, with each pregnancy there is a 25% (1 in 4) risk for the child to have the condition, a 50% (1 in 2) risk for the child to be an unaffected carrier like each of the parents, and a 25% chance for the child to not have the condition and not be a carrier.
Ocular albinism type 1 (OA-1) results from mutations in the GPR143 gene. The GPR143 gene provides instructions for making a protein that plays a role in pigmentation of the eyes and skin. It helps control the growth of melanosomes, which are cellular structures that produce and store a pigment called melanin. Melanin is the substance that gives skin, hair, and eyes their color. In the retina, this pigment also plays a role in normal vision. Most mutations in the GPR143 gene alter the size or shape of the GPR143 protein. Many of these genetic changes prevent the protein from reaching melanosomes to control their growth. In other cases, the protein reaches melanosomes normally but mutations disrupt the protein’s function. As a result of these changes, melanosomes in skin cells and the retina can grow abnormally large. Researchers are uncertain how these giant melanosomes are related to vision loss and other eye abnormalities in people with ocular albinism.
Rare cases of ocular albinism are not caused by mutations in the GPR143 gene. In these cases, the genetic cause of the condition is often unknown.
Ocular albinism type 1 (OA-1) is inherited in an X-linked pattern (Figure 3). A condition is considered X-linked if the mutated gene that causes the disorder is located on the X chromosome, one of the two sex chromosomes. In males (who have only one X chromosome and one Y), one altered copy of the causative gene (GPR143 gene) in each cell is sufficient to cause the characteristic features of ocular albinism, because males do not have another X chromosome with a working copy of the gene. Because females have two copies of the X chromosome, women with only one copy of a GPR143 mutation in each cell usually do not experience vision loss or other significant eye abnormalities. They may have mild changes in retinal pigmentation that can be detected during an eye examination 48.
A less common type of ocular albinism (OA) shows a different pattern of inheritance, autosomal recessive. With this type of inheritance, both parents of a child with autosomal recessive ocular albinism carry the gene for it (Figure 2). Boys and girls are equally affected. If both mother and father carry the gene, then at each birth there is a one in four chance that the child will have ocular albinism. Newer research suggests that autosomal recessive ocular albinism (OA) is a variant of oculocutaneous albinism (OCA). The skin and hair color may be somewhat lighter than that of other family members. Autosomal recessive ocular albinism may be a variant of either tyrosinase-related (type 1) or P gene (type 2) oculocutaneous albinism.
Researchers have also identified several other genes in which mutations can result in albinism with other features. One group of these includes at least nine genes (on different chromosomes) leading to Hermansky-Pudlak syndrome (HPS). In addition to albinism, Hermansky-Pudlak syndrome (HPS) is associated with bleeding problems and bruising. Some forms are also associated with lung and bowel disease. Like oculocutaneous albinism (OCA), Hermansky-Pudlak syndrome (HPS) is inherited in an autosomal recessive manner.
Figure 2. Oculocutaneous albinism autosomal recessive inheritance pattern
Footnotes: To have an autosomal recessive disorder, you inherit two mutated genes, one from each parent (who are carriers of the mutated gene). These disorders are usually passed on by two carriers. Carriers of the mutated gene is rarely affected, but they have one mutated gene (recessive gene) and one normal gene (dominant gene) for the condition. Two carriers have a 25% chance of having an unaffected child with two normal genes (left), a 50% chance of having an unaffected child who also is a carrier (middle), and a 25% chance of having an affected child with two recessive genes (right).
Figure 3. Ocular albinism X-linked inheritance pattern
Footnotes: A condition is considered X-linked if the mutated gene that causes the disorder is located on the X chromosome, one of the two sex chromosomes. In males (who have only one X chromosome), one altered copy of the GPR143 gene in each cell is sufficient to cause the characteristic features of ocular albinism. Because females have two copies of the X chromosome, women with only one copy of a GPR143 mutation in each cell usually do not experience vision loss or other significant eye abnormalities. They may have mild changes in retinal pigmentation that can be detected during an eye examination.
Prevention of albinism
Albinism is an inherited condition. If a family member has albinism, a genetic counselor can help you understand the type of albinism and the chances of having a future child with albinism. He or she can also explain the available tests.
People with specific questions about genetic risks or genetic testing for themselves or family members should speak with a genetics professional.
Resources for locating a genetics professional in your community are available online:
- The National Society of Genetic Counselors (https://www.findageneticcounselor.com/) offers a searchable directory of genetic counselors in the United States and Canada. You can search by location, name, area of practice/specialization, and/or ZIP Code.
- The American Board of Genetic Counseling (https://www.abgc.net/about-genetic-counseling/find-a-certified-counselor/) provides a searchable directory of certified genetic counselors worldwide. You can search by practice area, name, organization, or location.
- The Canadian Association of Genetic Counselors (https://www.cagc-accg.ca/index.php?page=225) has a searchable directory of genetic counselors in Canada. You can search by name, distance from an address, province, or services.
- The American College of Medical Genetics and Genomics (http://www.acmg.net/ACMG/Genetic_Services_Directory_Search.aspx) has a searchable database of medical genetics clinic services in the United States.
Albinism symptoms
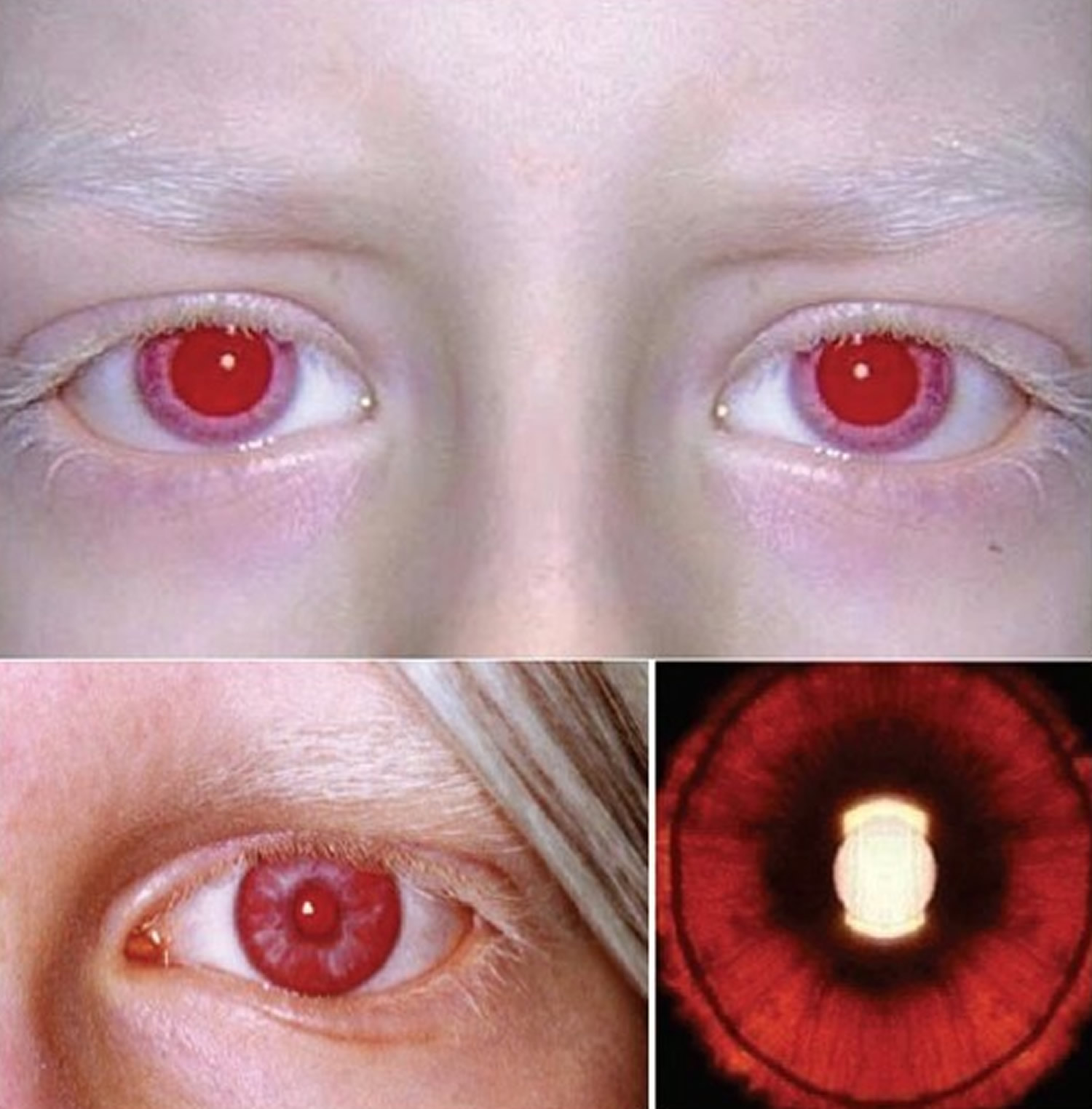
Signs and symptoms of albinism involve skin, hair, and eye color and vision. Some children with albinism are born with pinkish-white skin and white hair. Their eyes are usually light grey, blue or hazel, although they can look pink in the light.
People with albinism usually have poor vision. Glasses can help, but some have poor vision even with glasses. Some people with albinism also have nystagmus, which is involuntary flicking movements of the eye.
Skin
The most recognizable form of albinism results in white hair and very light-colored skin compared with siblings. Skin coloring (pigmentation) and hair color can range from white to brown, and may be nearly the same as that of parents or siblings without albinism.
With exposure to the sun, some people may develop:
- Freckles
- Moles, with or without pigment — moles without pigment are generally pink-colored
- Large freckle-like spots (lentigines)
- Sunburn and the inability to tan
For some people with albinism, skin pigmentation never changes. For others, melanin production may begin or increase during childhood and the teen years, resulting in slight changes in pigmentation.
Hair
Hair color can range from very white to brown. People of African or Asian descent who have albinism may have hair color that’s yellow, reddish or brown. Hair color may also darken by early adulthood or stain from exposure to normal minerals in water and the environment, and appear darker with age.
Symptoms of ocular albinism
Vision impairment is a key feature of all types of albinism. Eye problems and issues may include:
- Poor vision: Vision can range from normal for those minimally affected to legal blindness or worse (vision less than 20/200) for those with more severe forms of albinism. Near vision is often better than distance vision. Generally, those who have the least amount of pigment (i.e. most severely affected) have the poorest vision.
- Foveal hypoplasia (absence of a foveal pit) also known as macular hypoplasia: In albinism, the retina does not develop normally before birth and in infancy because of inappropriate retinal pigment epithelium (RPE) pigmentation that is required for macular development. Optical coherence tomography (OCT) can demonstrate an absence of the foveal pit and the loss of normal thinning of the retina. Also, the foveal avascular zone is small or nonexistent with vessels crossing the area 2 disc diameter temporal to the optic disc margin. Foveal hypoplasia is the single most important contributor to poor vision in albino people 12.
- Pendular nystagmus: Nystagmus refers to rhythmic, involuntary, flicker of the eyes (back-and-forth movement of the eyes). Affected infants may have large amplitude with low frequency pattern of eye movement starting at 2-3 months of age, later changing to a pendular form without distinct fast or slow phases. Head movements, such as bobbing or tilting the head, to try to reduce the involuntary eye movements and see better. Eye muscle surgery may be considered to reduce nystagmus.
- Sensitivity to light (photophobia) – an intolerance or sensitivity to bright light due to reduced or absent pigment in the iris. The iris in albinism has little to no pigment to screen out stray light coming into the eye resulting in scattering of light within the eye. On slit lamp exam, the examiner may detect speckled or diffuse transillumination defect. This finding, while common with albinism, is not specific as iris transillumination occurs in diseases unrelated to albinism such as pseudoexfoliation, pigment dispersion syndrome, megalocornea, iris atrophy, and Axenfeld-Rieger spectrum 12. When present in an otherwise normal individual, this finding may indicate carrier status of a hypomelanotic gene mutation. The iris may be translucent and the margin of the crystalline lens may be visible on transillumunation during slit lamp examination. Patients may prefer to wear sunglasses to reduce their sensitivity to light.
- Refractive errors: Both myopia (nearsightedness) and hyperopia (farsightedness) can occur, and astigmatism (abnormal curvature of the front surface of the eye or the lens inside the eye) is very common.
- Strabismus (‘squint’. ‘lazy eye’ or ‘turned eye’): Misalignment of the eyes and related anomalous head tilt can occur in association with albinism. Kumar et al 49 reported that the strabismus is seen in higher proportions of those with albinism compared to those with idiopathic infantile nystagmus, suggesting different mechanisms underlying the cause of strabismus in the two disorders.
- Visual pathway anomalies (misrouting of the optic nerve) may also be present, particularly problems with depth perception. Nerve signals from the retina to the brain that don’t follow the usual nerve pathways. Normally about half of optic nerve fibers from each eye decussates at the optic chiasm to the contralateral side, contributing to stereopsis. Albinism is associated with fiber over-decussation, resulting in crossing of up to 90% of fibers to the contralateral side and thus strabismus and loss of stereopsis. Evidence of this abnormality can be detected by 3-lead visual evoked potential (VEP) for proper counseling regarding visual potential of a patient.
Eye color
Eyelashes and eyebrows are often pale. Eye color can range from very light blue to brown and may change with age.
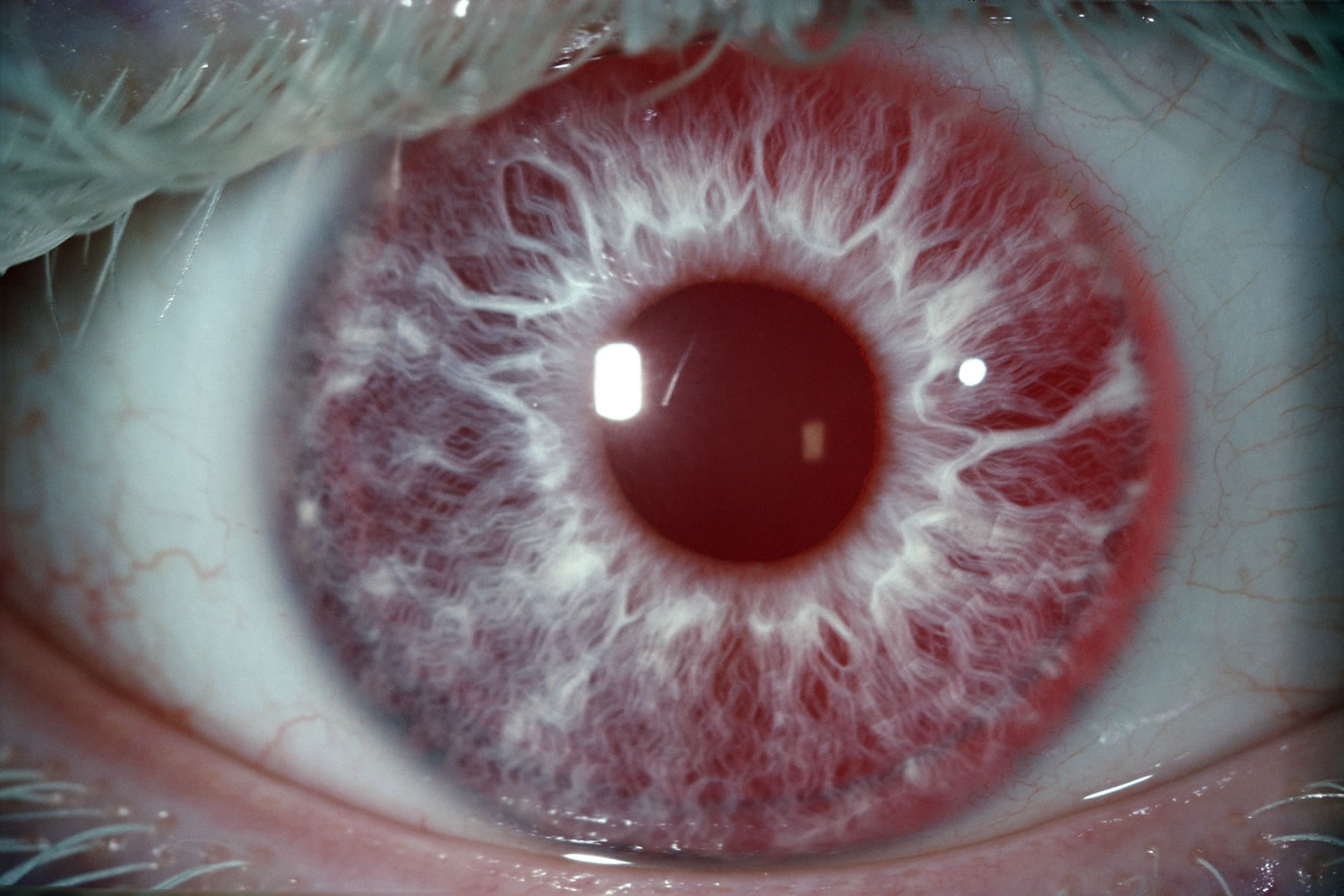
The lack of pigment in the colored part of the eyes (irises) makes the irises somewhat translucent. This means that the irises can’t completely block light from entering the eye. Because of this, very light-colored eyes may appear red in some lighting.
Figure 4. Albino person eyes
[Source 50 ]Albinism diagnosis
Diagnosis of albinism is based on:
- A physical exam that includes checking skin and hair pigmentation
- A thorough eye exam
- Comparison of your child’s pigmentation to that of other family members
- Review of your child’s medical history, including whether there has been bleeding that doesn’t stop, excessive bruising or unexpected infections
A medical doctor specializing in vision and eye disorders (ophthalmologist) should conduct your child’s eye exam. The exam includes an assessment of potential nystagmus, strabismus and photophobia. The doctor also uses a device to visually inspect the retina and determine if there are signs of abnormal development.
Genetic consultation can help determine the type of albinism and the inheritance.
Researchers have identified some, but not all of the DNA defects in ocular albinism. Therefore blood tests to identify genes for various types of albinism are not conclusive enough to be used for genetic counseling. Most of the time an ophthalmologist can identify a carrier of the X-linked albinism gene by seeing mottling of pigment in her retinas. If this mottling is not apparent, research labs can examine a hair bulb or skin biopsy from a child. This will show unusually large granules of pigment in X-linked ocular albinism, but not in autosomal recessive ocular albinism.
Albinism treatment
Albinism can’t be “cured.” But it only rarely leads to serious health problems.
Because most people with albinism don’t have health problems, treatment — apart from vision care — isn’t usually necessary.
People with Hermansky-Pudlak and Chediak-Higashi syndromes usually require regular specialized care to prevent complications.
People with albinism have a higher risk than others of sunburn, skin problems and skin cancer. So people with alibinism need to take certain precautions, such as wearing sunglasses and sunscreen when outdoors.
When health problems are serious, doctors usually can treat the symptoms.
Vision Rehabilitation
Proper eye care and monitoring skin for signs of abnormalities are especially important to your child’s health.
- Your child will most likely need to wear prescription lenses, and he or she should receive annual eye exams by an ophthalmologist. Although surgery is rarely part of treatment for albinism, your ophthalmologist may recommend surgery on optical muscles to minimize nystagmus. Surgery to correct strabismus may make the condition less noticeable, but it won’t improve vision.
- Your doctor should conduct an annual assessment of your child’s skin to screen for skin cancer or lesions that can lead to cancer. Adults with albinism need annual eye and skin exams throughout their lives.
Eye problems in albinism result from the abnormal development of the eye because of a lack of pigment and often include:
- Nystagmus: Regular horizontal back and forth movement of the eyes
- Strabismus: Muscle imbalance of the eyes, “crossed eyes” (esotropia), “lazy eye” or an eye that deviates out (exotropia)
- Photophobia: Sensitivity to bright light and glare
- Refractive Error: People with albinism may be either farsighted or nearsighted and usually have astigmatism
- Foveal hypoplasia: The retina, the surface inside the eye that receives light, does not develop normally before birth and in infancy
- Optic nerve misrouting: The nerve signals from the retina to the brain do not follow the usual nerve routes
The iris, the colored area in the center of the eye, has very little or no pigment to screen out stray light coming into the eye. Light normally enters the eye only through the pupil, the dark opening in the center of the iris, but in albinism light can pass through the iris as well.
For the most part, treatment consists of visual rehabilitation. Surgery to correct strabismus may improve the appearance of the eyes. However, since surgery will not correct the misrouting of nerves from the eyes to the brain, surgery will not improve eyesight or fine binocular vision. In the case of esotropia or “crossed eyes,” surgery may help vision by expanding the visual field (the area that the eyes can see while looking at one point). Surgical intervention is also available to minimize nystagmus.
People with albinism are sensitive to glare, but they do not prefer to be in the dark, and they need light to see just like anyone else. Sunglasses or tinted contact lenses may help outdoors. Indoors, it is important to place lights for reading or close work over a shoulder rather than in front.
Various optical aids are helpful to people with albinism, and the choice of an optical aid depends on how a person uses his or her eyes in jobs, hobbies or other usual activities. Some people do well using bifocals which have a strong reading lens, prescription reading glasses or contact lenses. Others use handheld magnifiers or special small telescopes, and some prefer to use screen magnification products on computers.
Some people with albinism use bioptics, glasses which have small telescopes mounted on, in or behind their regular lenses so that one can look through either the regular lens or the telescope. Some states allow the use of bioptic telescopes for driving.
Optometrists or ophthalmologists who are experienced in working with low vision patients can recommend various optical aids. Clinics should provide instruction in their use. The American Foundation for the Blind 51 maintains a directory of low vision clinics. In Canada, support is available from the Canadian National Institute for the Blind 52.
Lifestyle and home remedies
You can help your child learn self-care practices that should continue into adulthood:
- Use low vision aids, such as a hand-held magnifying glass, a monocular or a magnifier that attaches to glasses.
- Apply sunscreen with a sun protection factor (SPF) of at least 30 that protects against both UVA and UVB light.
- Avoid high-risk sun exposure, such as being outside in the middle of the day, at high altitudes, and on sunny days with thin cloud cover.
- Wear protective clothing, including long-sleeved shirts, long pants and broad-rimmed hats.
- Protect eyes by wearing dark, UV-blocking sunglasses or transition lenses that darken in bright light.
Coping and support
Coping with vision impairment
Many people with albinism develop coping skills to adjust to vision impairments. Tilting the head to one side may minimize the effect of nystagmus and improve vision. Holding a book very close can make it easier to read without causing any harm to the eyes.
Coping with educational challenges
Despite visual handicaps and abnormal optic nerve pathways, children with albinism are developmentally normal. If your child has albinism, begin early to work with teachers and school administrators to facilitate measures to help your child adapt. These may include sitting in the front of the class, using large-print books or a tablet computer for learning, avoiding bright light in the learning setting, or allowing more time for taking tests.
If necessary, start with educating the school professionals about what albinism is and how it affects your child. Also ask about services the school can provide to assess your child’s needs.
Adjustments to the classroom environment that may help your child include:
- A seat near the front of the classroom
- A tablet computer that can be synced to an interactive whiteboard (SMART board) at the front of the room, allowing the child to sit farther back in the classroom
- Handouts of the content written on boards or overhead screens
- High-contrast printed documents, such as black type on white paper rather than colored print or paper
- Large-print textbooks
- Other options, such as showing the child how to enlarge font size on a computer screen
Help your child develop skills to deal with other people’s reactions to albinism:
- Encourage your child to talk to you about experiences and feelings.
- Practice responses to teasing or embarrassing questions.
- Find a peer support group or online community through agencies such as the National Organization for Albinism and Hypopigmentation 4.
- Seek the services of a mental health professional, who can help you and your child develop healthy communication and coping skills.
Albinism prognosis
Most people with albinism live a normal lifespan and have the same types of medical problems as the rest of the population 53. Although the risk to develop skin cancer is increased, with careful surveillance, UV protection and prompt treatment, this is usually curable 54.
Patients may have children with no complications. Whether or not their children have albinism depends on the genetic makeup of their partner.
Albinism does not cause a delay in development or mental retardation.
Hermansky-Pudlak syndrome (HPS) can shorten a person’s lifespan due to lung disease or bleeding problems.
References- Albinism. https://www.mayoclinic.org/diseases-conditions/albinism/symptoms-causes/syc-20369184
- What is Albinism? http://www.albinism.org/site/c.flKYIdOUIhJ4H/b.9253761/k.24EE/Information_Bulletin__What_is_Albinism.htm
- Albinism. MedlinePlus. https://medlineplus.gov/ency/article/001479.htm
- National Organization for Albinism and Hypopigmentation. http://www.albinism.org
- Schlessinger DI, Anoruo MD, Schlessinger J. Biochemistry, Melanin. [Updated 2021 May 9]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK459156
- Del Bino, S., Duval, C., & Bernerd, F. (2018). Clinical and Biological Characterization of Skin Pigmentation Diversity and Its Consequences on UV Impact. International journal of molecular sciences, 19(9), 2668. https://doi.org/10.3390/ijms19092668
- Ismail, Rosnah & Ahmad, Salmiah & Aotd,. (2004). {PAGE } Sodium lactates in skin lightening formulations: its synergy with other skin lightening agents. https://www.researchgate.net/publication/307863602_PAGE_Sodium_lactates_in_skin_lightening_formulations_its_synergy_with_other_skin_lightening_agents
- Cruz-Inigo AE, Ladizinski B, Sethi A. Albinism in Africa: stigma, slaughter and awareness campaigns. Dermatol Clin. 2011 Jan;29(1):79-87.
- Boissy RE, Nordlund JJ. Molecular basis of congenital hypopigmentary disorders in humans: a review. Pigment Cell Res. 1997 Feb-Apr;10(1-2):12-24.
- RGiebel LB, Musarella MA, Spritz RA. A nonsense mutation in the tyrosinase gene of Afghan patients with tyrosinase negative (type IA) oculocutaneous albinism. J Med Genet. 1991 Jul;28(7):464-7.
- Grønskov K, Ek J, Brondum-Nielsen K. Oculocutaneous albinism. Orphanet J Rare Dis. 2007 Nov 2;2:43.
- Levin AV, Stroh E. Albinism for the busy clinician. J AAPOS. 2011 Feb;15(1):59-66. doi: 10.1016/j.jaapos.2010.10.012
- King RA, Wirtschafter JD, Olds DP, Brumbaugh J. Minimal pigment: a new type of oculocutaneous albinism. Clin Genet. 1986 Jan;29(1):42-50.
- Kono M, Kondo T, Ito S, Suzuki T, Wakamatsu K, Ito S, Tomita Y. Genotype analysis in a patient with oculocutaneous albinism 1 minimal pigment type. Br J Dermatol. 2012 Apr;166(4):896-8.
- Lund PM. Oculocutaneous albinism in southern Africa: population structure, health and genetic care. Ann Hum Biol. 2005 Mar-Apr;32(2):168-73. Review
- Spritz RA, Oh J, Fukai K, Holmes SA, Ho L, Chitayat D, France TD, Musarella MA, Orlow SJ, Schnur RE, Weleber RG, Levin AV. Novel mutations of the tyrosinase (TYR) gene in type I oculocutaneous albinism (OCA1). Hum Mutat. 1997;10(2):171-4.
- Fridman C, Hosomi N, Varela MC, Souza AH, Fukai K, Koiffmann CP. Angelman syndrome associated with oculocutaneous albinism due to an intragenic deletion of the P gene.Am J Med Genet A. 2003 Jun 1;119A(2):180-3.
- King RA, Lewis RA, Townsend D, Zelickson A, Olds DP, Brumbaugh J. Brown oculocutaneous albinism. Clinical, ophthalmological, and biochemical characterization. Ophthalmology. 1985 Nov;92(11):1496-505.
- Manga P, Kromberg J, Turner A, Jenkins T, Ramsay M. In Southern Africa, brown oculocutaneous albinism (BOCA) maps to the OCA2 locus on chromosome 15q: P-gene mutations identified. Am J Hum Genet. 2001;68:782–7.
- Zhang KH, Li Z, Lei J, Pang T, Xu B, Jiang WY, Li HY. Oculocutaneous albinism type 3 (OCA3): analysis of two novel mutations in TYRP1 gene in two Chinese patients. Cell Biochem Biophys. 2011 Dec;61(3):523-9.
- Kromberg JG, Castle DJ, Zwane EM, Bothwell J, Kidson S, Bartel P, Phillips JI, Jenkins T. Red or rufous albinism in southern Africa. Ophthalmic Paediatr Genet. 1990 Sep;11(3):229-35.
- Manga P, Kromberg JG, Box NF, Sturm RA, Jenkins T, Ramsay M. Rufous oculocutaneous albinism in southern African Blacks is caused by mutations in the TYRP1 gene. Am J Hum Genet. 1997 Nov;61(5):1095-101.
- Jimbow K. Biological role of tyrosinase-related protein and its relevance to pigmentary disorders (vitiligo vulgaris). J Dermatol. 1999 Nov;26(11):734-7.
- Newton JM, Cohen-Barak O, Hagiwara N, Gardner JM, Davisson MT, King RA, Brilliant MH. Mutations in the human orthologue of the mouse underwhite gene (uw) underlie a new form of oculocutaneous albinism, OCA4. Am J Hum Genet. 2001 Nov;69(5):981-8.
- Mártinez-García M, Montoliu L. Albinism in Europe. J Dermatol. 2013 May;40(5):319-24.
- Kausar T, Bhatti MA, Ali M, Shaikh RS, Ahmed ZM. OCA5, a novel locus for non-syndromic oculocutaneous albinism, maps to chromosome 4q24. Clin Genet. 2013 Jul;84(1):91-3.
- Wei AH, Zang DJ, Zhang Z, Liu XZ, He X, Yang L, Wang Y, Zhou ZY, Zhang MR, Dai LL, Yang XM, Li W. Exome sequencing identifies SLC24A5 as a candidate gene for nonsyndromic oculocutaneous albinism. J Invest Dermatol. 2013 Jul;133(7):1834-40.
- Grønskov K, Dooley CM, Østergaard E, Kelsh RN, Hansen L, Levesque MP, Vilhelmsen K, Møllgård K, Stemple DL, Rosenberg T. Mutations in c10orf11, a melanocyte-differentiation gene, cause autosomal-recessive albinism.Am J Hum Genet. 2013 Mar 7;92(3):415-21.
- Morice-Picard F, Lasseaux E, François S, Simon D, Rooryck C, Bieth E, Colin E, Bonneau D, Journel H, Walraedt S, Leroy BP, Meire F, Lacombe D, Arveiler B. SLC24A5 Mutations Are Associated with Non-Syndromic Oculocutaneous Albinism. J Invest Dermatol. 2013 Aug 28.
- Montoliu L, Grønskov K, Wei AH, Martínez-García M, Fernández A, Arveiler B, Morice-Picard F, Riazuddin S, Suzuki T, Ahmed ZM, Rosenberg T, Li W. Increasing the complexity: new genes and new types of albinism. Pigment Cell Melanoma Res. 2013 Sep 21.
- Rosenberg T, Schwartz M. X-linked ocular albinism: prevalence and mutations–a national study. Eur J Hum Genet. 1998;6(6):570.
- Bassi MT, Schiaffino MV, Renieri A, De Nigris F, Galli L, Bruttini M, Gebbia M, Bergen AA, Lewis RA, Ballabio A. Cloning of the gene for ocular albinism type 1 from the distal short arm of the X chromosome. Nat Genet. 1995 May;10(1):13-9.
- Shiono T, Tsunoda M, Chida Y, Nakazawa M, Tamai M. X linked ocular albinism in Japanese patients. Br J Ophthalmol. 1995;79(2):139.
- Lang GE, Rott HD, Pfeiffer RA. X-linked ocular albinism. Characteristic pattern of affection in female carriers. Ophthalmic Paediatr Genet. 1990 Dec;11(4):265-71.
- Schnur RE, Gao M, Wick PA, Keller M, Benke PJ, Edwards MJ, Grix AW, Hockey A, Jung JH, Kidd KK, Kistenmacher M, Levin AV, Lewis RA, Musarella MA, Nowakowski RW, Orlow SJ, Pagon RS, Pillers DA, Punnett HH, Quinn GE, Tezcan K, Wagstaff J, Weleber RG. OA1 mutations and deletions in X-linked ocular albinism. Am J Hum Genet. 1998 Apr;62(4):800-9.
- Winship IM, Babaya M, Ramesar RS. X-linked ocular albinism and sensorineural deafness: linkage to Xp22.3. Genomics. 1993 Nov;18(2):444-5.
- Dourmishev AL, Dourmishev LA, Schwartz RA, Janniger CK. Waardenburg syndrome. Int J Dermatol. 1999;38(9):656.
- O’Donnell FE, Green WR, McKusick VA, Forsius H, Eriksson AW. Forsius-Eriksson syndrome: its relation to the Nettleship-Falls X-linked ocular albinism. Clin Genet. 1980 Jun;17(6):403-8.
- Pillers DA, Towbin JA, Chamberlain JS, Wu D, Ranier J, Powell BR, McCabe ER. Deletion mapping of Aland Island eye disease to Xp21 between DXS67 (B24) and Duchenne muscular dystrophy. Am J Hum Genet. 1990 Nov;47(5):795-801.
- Hawksworth NR, Headland S, Good P, Thomas NS, Clarke A. Aland island eye disease: clinical and electrophysiological studies of a Welsh family. Br J Ophthalmol. 1995 May;79(5):424-30.
- Seward SL Jr, Gahl WA. Hermansky-Pudlak syndrome: health care throughout life. Pediatrics. 2013 Jul;132(1):153-60.
- Wildenberg SC, Oetting WS, Almodóvar C, Krumwiede M, White JG, King RA. A gene causing Hermansky-Pudlak syndrome in a Puerto Rican population maps to chromosome 10q2. Am J Hum Genet. 1995;57(4):755–765.
- Kaplan J, De Domenico I, Ward DM. Chediak-Higashi syndrome. Curr Opin Hematol. 2008 Jan;15(1):22-9.
- Reddy RR, Babu BM, Venkateshwaramma B, Hymavathi Ch. Silvery hair syndrome in two cousins: Chediak-Higashi syndrome vs Griscelli syndrome, with rare associations. Int J Trichology. 2011 Jul;3(2):107-11.
- Antunes H, Pereira A, Cunha I. Chediak-Higashi syndrome: pathognomonic feature. Lancet. 2013 Nov 2;382(9903):1514.
- Karim MA, Suzuki K, Fukai K, Oh J, Nagle DL, Moore KJ, Barbosa E, Falik-Borenstein T, Filipovich A, Ishida Y, Kivrikko S, Klein C, Kreuz F, Levin A, Miyajima H, Regueiro J, Russo C, Uyama E, Vierimaa O, Spritz RA. Apparent genotype-phenotype correlation in childhood, adolescent, and adult Chediak-Higashi syndrome. Am J Med Genet. 2002 Feb 15;108(1):16-22.
- Cooper DN, Ball EV, Krawczak M. The human gene mutation database. Nucleic Acids Res. 1998 Jan 1;26(1):285-7.
- Ocular albinism. https://medlineplus.gov/genetics/condition/ocular-albinism/
- Kumar A, Gottlob I, McLean RJ, Thomas S, Thomas MG, Proudlock FA. Clinical and oculomotor characteristics of albinism compared to FRMD7 associated infantile nystagmus. Invest Ophthalmol Vis Sci. 2011 Apr 8;52(5):2306-13.
- Hertle, Richard. (2013). Albinism: Particular Attention to the Ocular Motor System. Middle East African journal of ophthalmology. 20. 248-255. 10.4103/0974-9233.114804
- American Foundation for the Blind. https://www.afb.org/default.aspx
- Canadian National Institute for the Blind. http://www.cnib.ca/en/Pages/default.aspx
- Albinism. https://emedicine.medscape.com/article/1200472-overview#a2
- Chalya PL, Gilyoma JM, Kanumba ES, Mawala B, Masalu N, Kahima JK, Rambau P: Dermatological malignancies at a University Teaching Hospital in north-western Tanzania: a retrospective review of 154 cases. Tanzania Journal of Health Research 2021, 14(1):1-7.