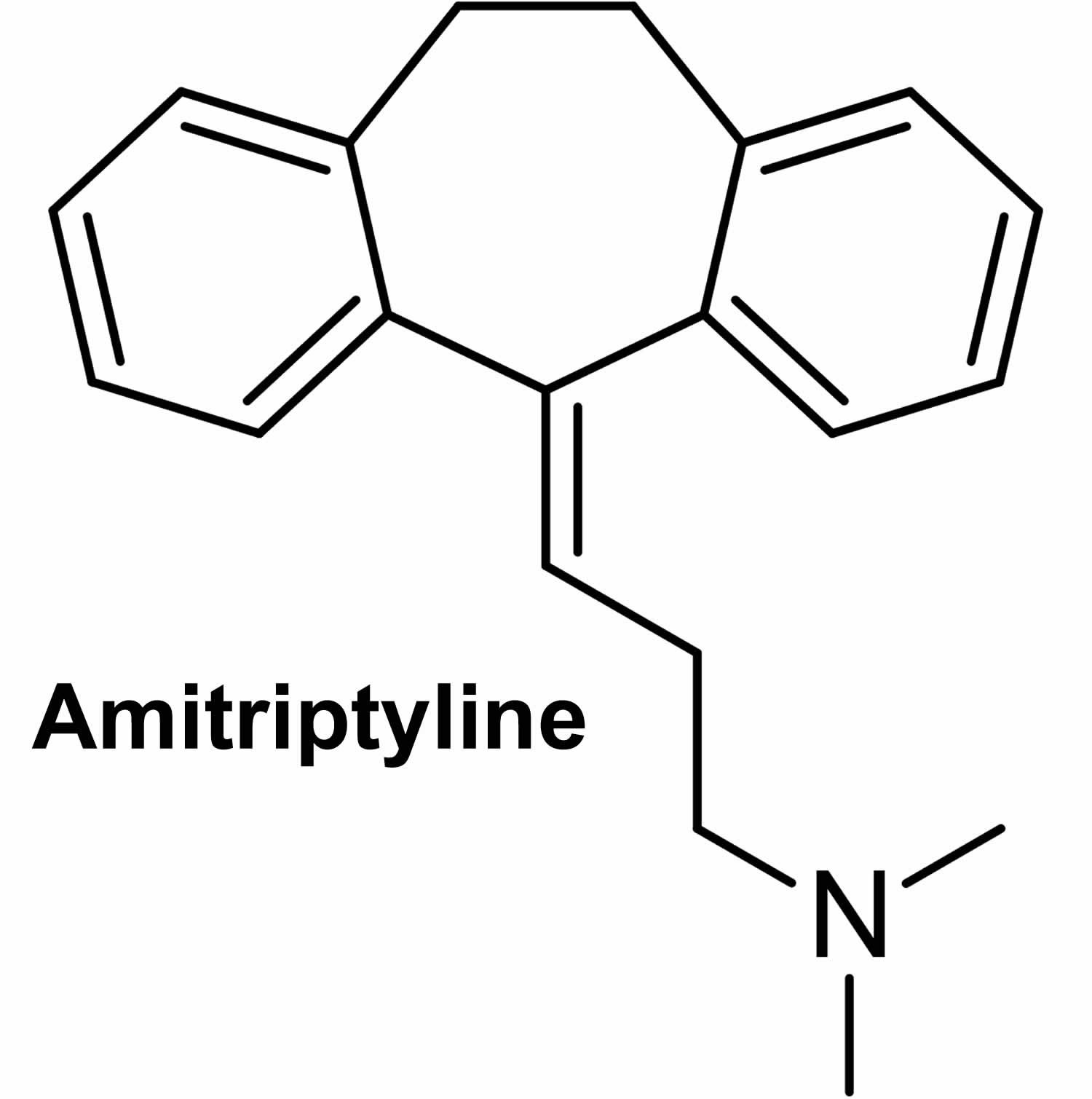
What is amitriptyline
Amitriptyline or amitriptyline elavil is a tricyclic antidepressant with sedative effects that is used to treat symptoms of depression. Amitriptyline is also used to treat eating disorders, post-herpetic neuralgia (the burning, stabbing pains, or aches that may last for months or years after a shingles infection), and to prevent migraine headaches. Amitriptyline has anticholinergic and sedative properties. Amitriptyline appears to prevent the re-uptake of norepinephrine and serotonin at nerve terminals in the central nervous system (CNS), thereby increasing the synaptic concentration of norepinephrine and serotonin, thus potentiating the action of these neurotransmitters. Due to constant stimulation to these receptors, amitriptyline may produce a downregulation of adrenergic and serotonin receptors, which may contribute to the antidepressant activity. Amitriptyline also appears to antagonize cholinergic and alpha-1 adrenergic responses to bioactive amines. Talk to your doctor about the possible risks of using amitriptyline medication for your condition.
Amitriptyline is extremely sedating, and thus improvement of sleep patterns can be the first benefit of treatment. Amitriptyline exhibits strong anticholinergic activity, cardiovascular effects including orthostatic hypotension, changes in heart rhythm and conduction, and a lowering of the seizure threshold. As with other antidepressants, several weeks of therapy may be required in order to realize the full clinical benefit of amitriptyline. Although not a labelled indication, amitriptyline is widely used in the management of chronic nonmalignant pain (e.g., post-herpetic neuralgia, fibromyalgia).
Suicidality and Antidepressant Drugs
A small number of children, teenagers, and young adults (up to 24 years of age) who took antidepressants (‘mood elevators’) such as amitriptyline during clinical studies became suicidal (thinking about harming or killing oneself or planning or trying to do so). Children, teenagers, and young adults who take antidepressants to treat depression or other mental illnesses may be more likely to become suicidal than children, teenagers, and young adults who do not take antidepressants to treat these conditions. However, experts are not sure about how great this risk is and how much it should be considered in deciding whether a child or teenager should take an antidepressant. Children younger than 18 years of age should not normally take amitriptyline, but in some cases, a doctor may decide that amitriptyline is the best medication to treat a child’s condition.
You should know that your mental health may change in unexpected ways when you take amitriptyline or other antidepressants even if you are an adult over age 24. You may become suicidal, especially at the beginning of your treatment and any time that your dose is increased or decreased. You, your family, or your caregiver should call your doctor right away if you experience any of the following symptoms: new or worsening depression; thinking about harming or killing yourself, or planning or trying to do so; extreme worry; agitation; panic attacks; difficulty falling asleep or staying asleep; aggressive behavior; irritability; acting without thinking; severe restlessness; and frenzied abnormal excitement. Be sure that your family or caregiver knows which symptoms may be serious so they can call the doctor when you are unable to seek treatment on your own.
Your healthcare provider will want to see you often while you are taking amitriptyline, especially at the beginning of your treatment. Be sure to keep all appointments for office visits with your doctor.
The doctor or pharmacist will give you the manufacturer’s patient information sheet (Medication Guide) when you begin treatment with amitriptyline. Read the information carefully and ask your doctor or pharmacist if you have any questions. You also can obtain the Medication Guide from the FDA website: https://www.accessdata.fda.gov/scripts/cder/daf/index.cfm.
No matter your age, before you take an antidepressant, you, your parent, or your caregiver should talk to your doctor about the risks and benefits of treating your condition with an antidepressant or with other treatments. You should also talk about the risks and benefits of not treating your condition. You should know that having depression or another mental illness greatly increases the risk that you will become suicidal. This risk is higher if you or anyone in your family has or has ever had bipolar disorder (mood that changes from depressed to abnormally excited) or mania (frenzied, abnormally excited mood) or has thought about or attempted suicide. Talk to your doctor about your condition, symptoms, and personal and family medical history. You and your doctor will decide what type of treatment is right for you.
Other important information
You should not use amitriptyline if you have recently had a heart attack.
Do not use amitriptyline if you have used a MAO inhibitor in the past 14 days, such as isocarboxazid, linezolid, methylene blue injection, phenelzine, rasagiline, selegiline, or tranylcypromine.
Before taking amitriptyline, tell your doctor if you have used an “SSRI” antidepressant in the past 5 weeks, such as citalopram (Celexa), escitalopram (Lexapro), fluoxetine (Prozac, Sarafem, Symbyax), fluvoxamine (Luvox), paroxetine (Paxil), or sertraline (Zoloft).
You may have thoughts about suicide when you first start taking an antidepressant such as amitriptyline, especially if you are younger than 24 years old. Your doctor will need to check you at regular visits for at least the first 12 weeks of treatment.
Report any new or worsening symptoms to your doctor, such as: mood or behavior changes, anxiety, panic attacks, trouble sleeping, or if you feel impulsive, irritable, agitated, hostile, aggressive, restless, hyperactive (mentally or physically), more depressed, or have thoughts about suicide or hurting yourself.
Special precautions
Before taking amitriptyline:
- tell your doctor and pharmacist if you are allergic to amitriptyline or any other medications.
- tell your doctor if you are taking cisapride (Propulsid) (not available in the U.S.) or monoamine oxidase (MAO) inhibitors such as isocarboxazid (Marplan), phenelzine (Nardil), selegiline (Eldepryl, Emsam, Zelapar), and tranylcypromine (Parnate), or if you have taken an MAO inhibitor during the past 14 days. Your doctor will probably tell you that you should not take amitriptyline.
- tell your doctor and pharmacist what other prescription and nonprescription medications, vitamins, nutritional supplements, and herbal products you are taking. Be sure to mention any of the following: antihistamines; cimetidine (Tagamet); diet pills; disulfiram (Antabuse); guanethidine (Ismelin); ipratropium (Atrovent); quinidine (Quinidex); medications for irregular heartbeats such as flecainide (Tambocor) and propafenone (Rythmol); medications for anxiety, asthma, colds, irritable bowel disease, mental illness, nausea, Parkinson’s disease, seizures, ulcers, or urinary problems; other antidepressants; phenobarbital (Bellatal, Solfoton); sedatives; selective serotonin reuptake inhibitors (SSRIs) such as citalopram (Celexa), fluoxetine (Prozac, Sarafem), fluvoxamine (Luvox), paroxetine (Paxil), and sertraline (Zoloft); sleeping pills; thyroid medications; and tranquilizers. Tell your doctor or pharmacist if you have stopped taking fluoxetine (Prozac, Sarafem) in the past 5 weeks.Your doctor may need to change the doses of your medications or monitor you carefully for side effects.
- tell your doctor if you have recently had a heart attack. Your doctor will probably tell you not to take amitriptyline.
- tell your doctor if you drink large amounts of alcohol and if you have or have ever had glaucoma (an eye condition); an enlarged prostate (a male reproductive gland); difficulty urinating; seizures; an overactive thyroid gland (hyperthyroidism); diabetes; schizophrenia (a mental illness that causes disturbed or unusual thinking, loss of interest in life, and strong or inappropriate emotions); or liver, kidney, or heart disease.
- Do not drink alcohol. Dangerous side effects or death can occur when alcohol is combined with amitriptyline.
- tell your doctor if you are pregnant or plan to become pregnant. If you become pregnant while taking amitriptyline, call your doctor. Do not breast-feed while you are taking amitriptyline.
- talk to your doctor about the risks and benefits of taking this medication if you are 65 years of age or older. Older adults should not usually take amitriptyline because it is not as safe or effective as other medication(s) that can be used to treat the same condition.
- if you are having surgery, including dental surgery, tell the doctor or dentist that you are taking amitriptyline.
- you should know that amitriptyline may make you drowsy. Do not drive a car or operate machinery until you know how this medication affects you.
- remember that alcohol can add to the drowsiness caused by amitriptyline medication.
How should amitriptyline medication be used?
Amitriptyline comes as a tablet to take by mouth. It is usually taken one to four times a day. Take amitriptyline at around the same time(s) every day. Follow the directions on your prescription label carefully, and ask your doctor or pharmacist to explain any part you do not understand. Take amitriptyline exactly as directed. Do not take more or less of it or take it more often than prescribed by your doctor.
Your doctor will probably start you on a low dose of amitriptyline and gradually increase your dose.
It may take a few weeks or longer before you feel the full benefit of amitriptyline. Continue to take amitriptyline even if you feel well. Do not stop taking amitriptyline without talking to your doctor. If you suddenly stop taking amitriptyline, you may experience withdrawal symptoms such as nausea, headache, and lack of energy. Your doctor will probably decrease your dose gradually.
Schizophrenic patients may develop increased symptoms of psychosis; patients with paranoid symptomatology may have an exaggeration of such symptoms. Depressed patients, particularly those with known manic-depressive illness, may experience a shift to mania or hypomania. In these circumstances the dose of Amitriptyline may be reduced or a major tranquilizer such as perphenazine may be administered concurrently.
Concurrent administration of Amitriptyline hydrochloride and electroshock therapy may increase the hazards associated with such therapy. Such treatment should be limited to patients for whom it is essential.
When possible, the drug should be discontinued several days before elective surgery.
Both elevation and lowering of blood sugar levels have been reported.
Amitriptyline hydrochloride should be used with caution in patients with impaired liver function.
Amitriptyline usage in pregnancy
Pregnancy Category C: Animal reproduction studies have shown an adverse effect on the fetus and there are no adequate and well-controlled studies in humans, but potential benefits may warrant use of the drug in pregnant women despite potential risks.
Teratogenic effects were not observed in mice, rats, or rabbits when Amitriptyline was given orally at doses of 2 to 40 mg/kg/day (up to 13 times the maximum recommended human dose). Based on a maximum recommended Amitriptyline dose of 150 mg/day or 3 mg/kg/day for a 50 kg patient. Studies in literature have shown Amitriptyline to be teratogenic in mice and hamsters when given by various routes of administration at doses of 28 to 100 mg/kg/day (9 to 33 times the maximum recommended human dose), producing multiple malformations. Another study in the rat reported that an oral dose of 25 mg/kg/day (8 times the maximum recommended human dose) produced delays in ossification of fetal vertebral bodies without other signs of embryotoxicity. In rabbits, an oral dose of 60 mg/kg/day (20 times the maximum recommended human dose) was reported to cause incomplete ossification of cranial bones.
Amitriptyline has been shown to cross the placenta. Although a causal relationship has not been established, there have been a few reports of adverse events, including CNS effects, limb deformities, or developmental delay, in infants whose mothers had taken Amitriptyline during pregnancy.
There are no adequate and well-controlled studies in pregnant women. Amitriptyline hydrochloride should be used during pregnancy only if the potential benefit to the mother justifies the potential risk to the fetus.
Amitriptyline and breastfeeding
Amitriptyline is excreted into breast milk. In one report in which a patient received Amitriptyline 100 mg/day while nursing her infant, levels of 83 to 141 ng/mL were detected in the mother’s serum. Levels of 135 to 151 ng/mL were found in the breast milk, but no trace of the drug could be detected in the infant’s serum.
Because of the potential for serious adverse reactions in nursing infants from Amitriptyline, a decision should be made whether to discontinue nursing or to discontinue the drug, taking into account the importance of the drug to the mother.
Amitriptyline HCL Contraindications
Amitriptyline hydrochloride is contraindicated in patients who have shown prior hypersensitivity to it.
It should not be given concomitantly with monoamine oxidase inhibitors. Hyperpyretic crises, severe convulsions, and deaths have occurred in patients receiving tricyclic antidepressant and monoamine oxidase inhibiting drugs simultaneously. When it is desired to replace a monoamine oxidase inhibitor with Amitriptyline hydrochloride, a minimum of 14 days should be allowed to elapse after the former is discontinued. Amitriptyline hydrochloride should then be initiated cautiously with gradual increase in dosage until optimum response is achieved.
Amitriptyline hydrochloride should not be given with cisapride due to the potential for increased QT interval and increased risk for arrhythmia.
This drug is not recommended for use during the acute recovery phase following myocardial infarction.
What is amitriptyline used for
Amitriptyline used to treat the symptoms of depression. Endogenous depression is more likely to be alleviated than are other depressive states.
Amitriptyline for neuropathic pain
Neuropathic pain is defined as pain that arises as a direct consequence of a lesion or diseases affecting the somatosensory system. Peripheral neuropathic pain can be caused by nerve injury or disease 1. Important causes include lumbar radiculopathy (“sciatica”), postherpetic neuralgia (persistent pain after a shingles episode), diabetic neuropathy, HIV-related neuropathy, and chronic postsurgical pain. Central neuropathic pain can arise after a stroke or spinal cord injury, in multiple sclerosis, or in other neurological and metabolic conditions.
Results from over a dozen randomized controlled trials of tricyclic antidepressants (e.g., amitriptyline) support their efficacy for neuropathic pain conditions including diabetic neuropathy 2, postherpetic neuralgia 3, and central post stroke pain 4, with recently estimated number needed-to-treat to obtain a clinically meaningful response in one patient is betwen 2.5–4.2 for amitriptyline (lower number needed-to-treat suggests better efficacy). However, it is important to note that high quality randomized controlled trials failed to demonstrate efficacy of tricyclic antidepressants in HIV-related neuropathy 5 or in lumbar radiculopathy 6.
However, a 2015 Cochrane Review 7 found no supportive unbiased evidence for a beneficial effect of amitriptyline. There is no good evidence of a lack of effect; rather the concern should be of overestimation of treatment effect. Amitriptyline should continue to be used as part of the treatment of neuropathic pain, but only a minority of people will achieve satisfactory pain relief 7.
Amitriptyline probably does not work in neuropathic pain associated with human immunodeficiency virus (HIV) or treatments for cancer 7. Amitriptyline probably does work in other types of neuropathic pain, though the review authors cannot be certain of this. The 2015 Cochrane Review best guess is that amitriptyline provides pain relief in about 1 in 4 (25%) more people than does placebo, and about 1 in 4 (25%) more people than placebo report having at least one adverse event, which may be troublesome, but probably not serious 7.
The most important message is that amitriptyline probably does give really good pain relief to some people with neuropathic pain, but only a minority of them; amitriptyline will not work for most people.
Amitriptyline for migraine
Amitriptyline was first used in the treatment of migraine in 1964, and in this study on 27 subjects, amitriptyline resulted in significant improvement in 56% patients 8. Amitriptyline was also found to be superior to placebo in reducing the headache frequency (55% vs 34%) 9. In a randomized controlled trial, amitriptyline resulted in significant improvement in headache frequency at 8 and 16 weeks compared with placebo in chronic daily headache 10. Amitriptyline was found to be as effective as topiramate in a recent randomized controlled trial 11. In addition to reducing the frequency, duration and intensity of headache attacks, therapy with amitriptyline may improve the response to acute treatment, reduce disability, and reduce associated economic costs 12. In this study 13, amitriptyline at 25 mg/day was an effective treatment for chronic migraine, but its efficacy was increased when combined with aerobic exercise. In the aerobic exercise program patients were instructed to perform a 40 minutes fast walk outdoors with a frequency of 3 times/week for 12 consecutive weeks and daily, fill out a headache questionnaire. All patients received written instructions and performed a training session with physiotherapist.
Amitriptyline for fibromyalgia
Amitriptyline will be one option in the treatment of fibromyalgia, while recognizing that only a minority of patients will achieve satisfactory pain relief 14. Amitriptyline has been a first‐line treatment for fibromyalgia for many years. The fact that there is no supportive unbiased evidence for a beneficial effect is disappointing, but has to be balanced against years of successful treatment in many patients with fibromyalgia.
Amitriptyline probably does provide good levels of pain relief for some people with fibromyalgia, although we cannot be certain of this. A 2015 Cochrane review authors’ best guess is that amitriptyline provides good pain relief in about 1 in 4 (25%) more people than does placebo 14. About 1 in 3 (31%) more people than with placebo report having one or more adverse events, which are usually not serious but may be troublesome and interfere with taking the treatment.
The most important message is that amitriptyline probably does give really good pain relief to some patients with fibromyalgia, but only a minority of them; amitriptyline will not work for most people 14.
Amitriptyline dosage
Adult Dose for Depression
Use: Relief of symptoms of depression
OUTPATIENTS:
- Initial dose: 75 mg orally per day in divided doses; this may be increased to 150 mg/day (if needed)
- Maintenance dose: 40 to 100 mg orally per day
- Maximum dose: 150 mg/day
Alternate outpatient treatment regimen: 50 to 100 mg orally as a single dose at bedtime; this may be increased by 25 or 50 mg as needed at bedtime to a total of 150 mg/day
INPATIENTS:
- Initial dose: 100 mg orally per day
- Maintenance dose: 40 to 100 mg orally as a single dose at bedtime
- Maximum dose: 300 mg/day
Comments:
- Dose increases should preferably be made in the late afternoon or at bedtime due to the sedative effect.
- The full therapeutic effect may take as long as 30 days to develop.
- Maintenance doses should be reduced to the lowest amount that will maintain relief of symptoms when satisfactory improvement has been obtained.
- Maintenance therapy should be continued for 3 months or longer to lessen the possibility of relapse.
Geriatric Dose for Depression
Use: Relief of symptoms of depression
- 10 mg orally 3 times a day AND 20 mg orally once a day at bedtime
Comments:
- The full therapeutic effect may take as long as 30 days to develop.
- Elderly patients should be monitored carefully and serum levels obtained as clinically appropriate.
- Dose adjustments should be made according to clinical response.
Pediatric Dose for Depression
Use: Relief of symptoms of depression
- 12 years or older: 10 mg orally 3 times a day AND 20 mg orally once a day at bedtime
Comments:
- The full therapeutic effect may take as long as 30 days to develop.
- Dose adjustments should be made according to clinical response.
Renal Dose Adjustments
- Data not available
Liver Dose Adjustments
- Use with caution
What should I do if I forget a dose?
Take the missed dose as soon as you remember it. However, if it is almost time for the next dose, skip the missed dose and continue your regular dosing schedule. Do not take a double dose to make up for a missed one.
Amitriptyline side effects
The most commonly reported side effects were tremors, dizziness, headache, dry mouth, constipation, and nausea.
Amitriptyline may cause side effects. Tell your doctor if any of these symptoms are severe or do not go away:
- nausea
- vomiting
- drowsiness
- weakness or tiredness
- nightmares
- headaches
- dry mouth
- constipation
- difficulty urinating
- blurred vision
- pain, burning, or tingling in the hands or feet
- changes in sex drive or ability
- excessive sweating
- changes in appetite or weight
- confusion
- unsteadiness
Some side effects can be serious. If you experience any of the following symptoms or those listed in the IMPORTANT WARNING section, call your doctor immediately:
- slow or difficult speech
- dizziness or faintness
- weakness or numbness of an arm or a leg
- crushing chest pain
- rapid, pounding, or irregular heartbeat
- severe skin rash or hives
- swelling of the face and tongue
- yellowing of the skin or eyes
- jaw, neck, and back muscle spasms
- uncontrollable shaking of a part of the body
- fainting
- unusual bleeding or bruising
- seizures
- hallucinating (seeing things or hearing voices that do not exist)
Some side effects of amitriptyline may occur that usually do not need medical attention. These side effects may go away during treatment as your body adjusts to the medicine. Also, your health care professional may be able to tell you about ways to prevent or reduce some of these side effects. Check with your health care professional if any of the following side effects continue or are bothersome or if you have any questions about them:
Incidence Not Known
- bigger, dilated, or enlarged pupils (black part of eye)
- black tongue
- bloating
- breast enlargement in females
- constipation
- decreased interest in sexual intercourse
- diarrhea
- hair loss, thinning of hair
- hives or welts
- inability to have or keep an erection
- increased in sexual ability, desire, drive, or performance
- increased interest in sexual intercourse
- increased sensitivity of eyes to light
- loss in sexual ability, desire, drive, or performance
- loss of sense of taste
- redness or other discoloration of skin
- severe sunburn
- skin rash
- swelling of testicles
- swelling of the breasts or breast soreness in males
- swelling of the parotid glands
- swelling or inflammation of the mouth
- unexpected or excess milk flow from breasts
Amitriptyline may cause other side effects. Call your doctor if you have any unusual problems while taking amitriptyline medication.
Nervous system
- Common (1% to 10%): Ataxia, disturbance in attention, dizziness, dysarthria/speech disorders, dysgeusia, drowsiness, headache, paresthesia, somnolence, tremors
- Uncommon (0.1% to 1%): Convulsions
- Very rare (less than 0.01%): Akathisia, polyneuropathy
- Frequency not reported: Abnormal voluntary movements, ageusia, alteration in cognition, alteration in electroencephalogram patterns, anticholinergic effects, autonomic nervous system function alterations, coma, disturbed concentration, extrapyramidal effects, extremity paresthesia, incoordination, neuromuscular activity alterations, numbness, peculiar taste, peripheral neuropathy, seizures, serotonin syndrome, stroke, syncope, tardive dyskinesia, tingling
- Postmarketing reports: Neuroleptic malignant syndrome
Cardiovascular
- Common (1% to 10%): Atrioventricular (AV) block, bundle branch block, electrocardiogram (ECG) abnormal, electrocardiogram QRS complex prolonged, electrocardiogram QT prolonged, orthostatic hypotension, palpitations, tachycardia
- Uncommon (0.1% to 1%): Collapse conditions, hypertension, worsening of cardiac failure
- Rare (0.01% to 0.1%): Arrhythmias
- Very rare (less than 0.01%): Cardiomyopathies, torsade de pointes
- Frequency not reported: Changes in AV conduction, edema, heart block, hypersensitivity myocarditis, hypotension, myocardial infarction, nonspecific ECG changes
Gastrointestinal
- Common (1% to 10%): Constipation, diarrhea, dry mouth, nausea, tongue edema, vomiting
- Rare (0.01% to 0.1%): Paralytic ileus, salivary gland enlargement
- Frequency not reported: Black tongue, epigastric distress, parotid swelling, stomatitis
Respiratory
- Common (1% to 10%): Allergic inflammation of the pulmonary alveoli, allergic inflammation of the lung tissue, alveolitis, congested nose, Loffler’s syndrome
Psychiatric
- Common (1% to 10%): Aggression, agitation, confusional states, libido decrease
- Uncommon (0.1% to 1%): Anxiety, hypomania, insomnia, mania, nightmares
- Rare (0.01% to 0.1%): Delirium (in elderly patients), hallucinations (in schizophrenic patients), suicidal behavior, suicidal thoughts
- Frequency not reported: Behavioral changes, delusions, disorientation, dream disturbances, excitement, increased libido, irritability, libido fluctuations, nightmares, paranoia, restlessness, sleep disturbances
- Postmarketing reports: Mental status changes
Metabolic
- Common (1% to 10%): Hyponatremia, thirst, weight increased
- Rare (0.01% to 0.1%): Blood alkaline phosphatase increased, decreased appetite, weight decreased
- Frequency not reported: Anorexia, blood sugar level elevation/lowering, increased appetite
Genitourinary
- Common (1% to 10%): Erectile dysfunction, micturition disorders
- Frequency not reported: Breast enlargement, dilation of urinary tract, impotence, interference with sexual function, testicular swelling, urinary frequency
Ocular
- Common (1% to 10%): Accommodation disorder, mydriasis
- Uncommon (0.1% to 1%): Intraocular pressure increased
- Very rare (less than 0.01%): Acute glaucoma
- Frequency not reported: Blurred vision, disturbance in accommodation, increased intraocular pressure
Dermatologic
- Common (1% to 10%): Hyperhidrosis
- Uncommon (0.1% to 1%): Face edema, rash/skin rash, urticaria
- Rare (0.01% to 0.1%): Alopecia, photosensitivity reaction
- Frequency not reported: Diaphoresis, increased perspiration, itching/pruritus, mild sweating, photosensitization
Other
- Common (1% to 10%): Fatigue
- Uncommon (0.1% to 1%): Tinnitus
- Rare (0.01% to 0.1%): Pyrexia
- Frequency not reported: Fever/hyperpyrexia, hyperthermia, malaise, weakness
Hepatic
- Uncommon (0.1% to 1%): Cholestatic liver disease, hepatic impairment
- Rare (0.01% to 0.1%): Jaundice, liver function test abnormal, transaminases increased
- Frequency not reported: Altered liver function, hepatic failure, hepatitis
Hematologic
- Rare (0.01% to 0.1%): Agranulocytosis, bone marrow depression, eosinophilia, leukopenia, purpura, thrombocytopenia
Endocrine
- Rare (0.01% to 0.1%): Gynecomastia
- Frequency not reported: Syndrome of inappropriate antidiuretic hormone (SIADH) secretion
Immunologic
- Frequency not reported: Positive antinuclear antibodies (ANA), positive rheumatoid factor
Musculoskeletal
- Frequency not reported: Increased risk of bone fractures, lupus-like syndrome, migratory arthritis
- Postmarketing reports: Muscle rigidity
Amitriptyline withdrawal
The abrupt cessation of amitriptyline administration can also be detrimental to the patient, triggering withdrawal phenomena often characterized by an exacerbation of the symptoms for which the patient was originally treated. The literature includes only 1 report of positional nystagmus and another case report of a patient who manifested signs of serotonin syndrome 15.
Amitriptyline overdose
In case of overdose, call the poison control helpline at 1-800-222-1222. Information is also available online at https://www.poisonhelp.org/help. If the victim has collapsed, had a seizure, has trouble breathing, or can’t be awakened, immediately call your local emergency services number.
Symptoms of amitriptyline overdose may include:
- irregular heartbeat
- seizures
- coma (loss of consciousness for a period of time)
- confusion
- problems concentrating
- hallucinating (seeing things or hearing voices that do not exist)
- agitation
- drowsiness
- rigid muscles
- vomiting
- fever
- cold body temperature
Concomitant administration of tricyclic antidepressants such as amitriptyline with sympathomimetic drugs such as isoproterenol, phenylephrine, norepinephrine, epinephrine, or amphetamines may increase sympathetic activity to the extent that pressor and cardiac effects of the sympathomimetics could be fatal. If tricyclic antidepressants (e.g., amitriptyline) are used with adrenergic agents, dosage must be monitored closely 16.
A fatality attributed to concurrent administration of 150 mg/day of amitriptyline and 40 mg/day of fluoxetine is reported in a 36-yr-old male patient who was prescribed the drugs for major depression 17; the patient died approximately 6 weeks after the drugs were prescribed, and his body was found several weeks later 17. Toxicological testing revealed only amitriptyline, fluoxetine, and their metabolites, nortriptyline and norfluoxetine. The most plausible explanation for the patient’s death was chronic intoxication with amitriptyline because of a reduction in its clearance caused by fluoxetine. An acute overdose was ruled out by blood and gastric distribution of the amitriptyline:nortriptyline ratio and other forensic findings. The interaction was attributed to inhibition of the CYP 2D6 enzyme by fluoxetine, which resulted in an effective daily dose of 600-1050 mg/day of amitriptyline. It was concluded that this case illustrates the significant effect that fluoxetine can have when coprescribed with drugs that are dependent on CYP 2D6 for clearance.
Management of amitriptyline overdose
All patients suspected of tricyclic antidepressant overdose should receive gastrointestinal decontamination. This should include, large volume gastric lavage followed by activated charcoal. If consciousness is impaired, the airway should be secured prior to lavage. Induced vomiting is contraindicated.
Obtain an ECG and immediately initiate cardiac monitoring. Protect the patient’s airway, establish an intravenous line and initiate gastric decontamination. A minimum of six hours of observation with cardiac monitoring and observation for signs of CNS or respiratory depression, hypotension, cardiac dysrhythmias and/or conduction blocks, and seizures is necessary. If signs of toxicity occur at any time during the period extended monitoring is required. There are case reports of patients succumbing to fatal dysrhythmias late after overdose; these patients had clinical evidence of significant poisoning prior to death and most received inadequate gastrointestinal decontamination. Monitoring of plasma drug levels should not guide management of the patient.
A maximal limb-lead QRS duration of ≥0.10 seconds may be the best indication of the severity of the overdose. Intravenous sodium bicarbonate should be used to maintain the serum pH in the range of 7.45 to 7.55. If the pH response is inadequate, hyperventilation may also be used. Concomitant use of hyperventilation and sodium bicarbonate should be done with extreme caution, with frequent pH monitoring. A pH >7.60 or a pCO2 <20 mm Hg is undesirable. Dysrhythmias unresponsive to sodium bicarbonate therapy/hyperventilation may respond to lidocaine, bretylium or phenytoin. Type 1 A and 1 C antiarrhythmics are generally contraindicated (e.g., quinidine, disopyramide, and procainamide).
In rare instances, hemoperfusion may be beneficial in acute refractory cardiovascular instability in patients with acute toxicity. However, hemodialysis, peritoneal dialysis, exchange transfusions, and forced diuresis generally have been reported as ineffective in tricyclic antidepressant poisoning.
In patients with CNS depression early intubation is advised because of the potential for abrupt deterioration. Seizures should be controlled with benzodiazepines, or if these are ineffective, other anticonvulsants (e.g., phenobarbital, phenytoin). Physostigmine is not recommended except to treat life-threatening symptoms that have been unresponsive to other therapies, and then only in consultation with a poison control center.
References- What is Neuropathic Pain? International Association for the Study of Pain 2014-2015. http://www.neupsig.org/
- Max MB, Lynch SA, Muir J, Shoaf SE, Smoller B, Dubner R. Effects of desipramine, amitriptyline, and fl uoxetine on pain in diabetic neuropathy. N Engl J Med 1992;326:1250–6.
- Raja SN, Haythornthwaite JA, Pappagallo M, Clark MR, Travison TG, Sabeen S, Royall RM, Max MB. Opioids versus antidepressants in postherpetic neuralgia: a randomized, placebo-controlled trial. Neurology 2002;59:1015–21.
- Leijon G, Boivie J. Central post-stroke pain: a controlled trial of amitriptyline and carbamazepine. Pain 1989;36:27–36.
- Shlay JC, Chaloner K, Max MB, Flaws B, Reichelderfer P, Wentworth D, Hillman S, Brizz B, Cohn DL. Acupuncture and amitriptyline for pain due to HIV-related peripheral neuropathy: a randomized controlled trial. Terry Beirn Community Programs for Clinical Research on AIDS. JAMA 1998;280:1590–5.
- Khoromi S, Cui L, Nackers L, Max MB. Morphine, nortriptyline and their combination vs. placebo in patients with chronic lumbar root pain. Pain 2007;130:66–75.
- Moore RA, Derry S, Aldington D, Cole P, Wiffen PJ. Amitriptyline for neuropathic pain in adults. Cochrane Database of Systematic Reviews 2015, Issue 7. Art. No.: CD008242. DOI: 10.1002/14651858.CD008242.pub3
- LANCE JW, CURRAN DA. Treatment of chronic tension headache. Lancet 1964;1:1236–9.
- COUCH JR, HASSANEIN RS. Amitriptyline in migraine prophylaxis. Arch Neurol 1979;36:695–99.
- COUCH JR. Amitriptyline Versus Placebo Study Group. Amitriptyline in the prophylactic treatment of migraine and chronic daily headache. Headache 2011;51:33–51.
- DODICK DW, FREITAG F, BANKS J et al. CAPSS-277 Investigator Group. Topiramate versus amitriptyline in migraine prevention: a 26-week, multicenter, randomized, double-blind, double-dummy, parallel-group noninferiority trial in adult migraineurs. Clin Ther 2009;31:542–59.
- Modi S, Lowder DM. Medications for migraine prophylaxis. Am Fam Physician. 2006;73(1):72-8.
- SANTIAGO, Michelle Dias Santos et al. Amitriptyline and aerobic exercise or amitriptyline alone in the treatment of chronic migraine: a randomized comparative study. Arq. Neuro-Psiquiatr. [online]. 2014, vol.72, n.11
- Moore RA, Derry S, Aldington D, Cole P, Wiffen PJ. Amitriptyline for fibromyalgia in adults. Cochrane Database of Systematic Reviews 2015, Issue 7. Art. No.: CD011824. DOI: 10.1002/14651858.CD011824
- Blay SL. Nystagmus as a Discontinuation Symptom After Antidepressant Therapy: A Case Report. The Primary Care Companion for CNS Disorders. 2014;16(2):PCC.13l01615. doi:10.4088/PCC.13l01615. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4116288/
- American Society of Health-System Pharmacists 2015; Drug Information 2015. Bethesda, MD. 2015, p. 2396
- Preskorn SH, Baker B; JAMA 277 (Jun 4): 1682, 1997