Hyperamylasemia
Hyperamylasemia is defined as a twofold or greater increase in serum amylase to a level exceeding the upper limit of normal (>99 U/L) 1. Normal serum amylase range is 40 to 140 units per liter (U/L) or 0.38 to 1.42 microkat/L (µkat/L) 2. Note that normal value ranges may vary slightly among different laboratories. Some laboratories use different measurement methods. A study found that 32% of Asian Americans and 50% of Native Americans had higher total amylase levels above the upper limit of normal compared to the White population 3. Another study found that the total serum amylase was higher in the elderly for both men and women, potentially resulting from an age-related decrease in kidney clearance 4. Talk to your doctor about the meaning of your test results.
Hyperamylasemia or high amylase level in the blood may indicate the presence of a condition affecting the pancreas 5. The pancreas is a long, flat glandular organ that’s tucked behind your stomach. The pancreas is surrounded by the stomach, intestines, and other organs. The pancreas exocrine glands make pancreatic juices that includes amylase, which contain enzymes that aid in food, fat and carbohydrates digestion; and the pancreas endocrine cells produce several hormones like insulin and glucagon, both of which help control blood sugar level.
Amylase is a digestive enzyme that helps you digest carbohydrates starch (also known as complex carbohydrates, which are made of lots of simple sugars strung together) into smaller carbohydrate groups and, finally, into monosaccharides also called simple sugars, by hydrolysis of the internal alpha-1,4-glycoside bonds, which results in the production of maltose and oligosaccharides. In healthy individuals, most of all the serum amylase in your body is made by your pancreas and salivary glands with 40%-45% from your pancreas and 55%-60% from your salivary glands 6. Normal blood amylase in Adult is 60-120 Somogyi units/dL or 30-220 units/L (SI units) 7. A small amount of amylase in your blood and urine is normal. A slight increase in values may seen during normal pregnancy and in the elderly. But having too much or too little amylase in your blood and urine may be a sign of a disorder of the pancreas or salivary glands, or another medical condition.
Amylase is usually present in the blood and urine in small quantities. When cells in the pancreas are injured, increased amounts of amylase are released into the blood. This also increases amylase concentrations in the urine because amylase is eliminated from the blood through the urine (25%) and the reticuloendothelial system (75%) 8, 9. An increased amount of amylase in the urine is called amylasuria.
Electrophoresis shows that serum amylase is of two main types, as follows:
- P-type amylase from the pancreas,
- S-type amylase from the salivary glands.
Serum isoamylase measurements to determine S-type isoamylase, P-type isoamylase, or macroamylasemia are the best tests to use when the cause of hyperamylasemia is obscure 10.
Blood amylase test is used to help diagnose and monitor acute pancreatitis, which is inflammation of the pancreas that occurs when the pancreatic duct is blocked by a gallstone or, in rare cases, with a pancreatic tumor 11, 12, 13, 14. In acute pancreatitis, patients usually presents with severe upper abdominal pain and amylase in the blood often increases to 4 to 6 times higher than the highest reference value, sometimes called the upper limit of normal 5. The blood amylase increase occurs within 4 to 8 hours of injury to the pancreas and generally remains elevated until the cause is successfully treated. A person with acute pancreatitis usually looks and feels very ill and needs immediate medical attention. Most cases require hospitalization for 3 to 5 days for close monitoring, pain control, and intravenous hydration.
In acute pancreatitis elevated serum amylase levels usually return to baseline in 3 to 7 days. In the first instance of acute pancreatitis, if hyperamylasemia persists for longer than usual it may be associated with recurrence of the disease 15.
Blood amylase test may also diagnose and monitor chronic pancreatitis and other disorders involving your pancreas such as blunt trauma, surgery, or recent endoscopic retrograde cholangiopancreatography (ERCP) of the pancreatic duct leading to the release of amylase enzyme from within the pancreatic cells. Risk factors include difficult cannulation, age below 60 years, history of diabetes, a stent in the biliary duct, and nasobiliary drainage 16, 17.
However, the major limitation of using serum amylase measurement in diagnosing pancreatitis is it is not specific 7, 13. That means an elevated amylase level may indicate a problem, but the cause may not necessarily be related to your pancreas. Serum amylase is increased in at least 75% of pancreatitis cases; however, serum amylase can be normal, even in the face of massive pancreatic necrosis 6. It has been shown that the magnitude of the serum amylase level is not correlated with the severity of acute pancreatitis 18, 19. Furthermore, besides the pancreas, amylase can also come from other inflamed or damaged tissues and organs such as salivary glands, intestines, and ovaries.
In a study involving 1000 emergency department patients presenting with abdominal pain, 39% of individuals received a test for amylase, but only 3.9% of individuals were diagnosed with pancreatitis 20. Furthermore, in patients with nonpancreatic abdominal pain, 11% to 13% of patients have elevated pancreatic enzymes 21. Hyperamylasemia is common following heart surgery and occurs in 30% to 60% of patients 22.
In typical acute pancreatitis, the serum amylase activity reaches its peak within the first 1 to 2 days after an attack of pancreatitis, then returns to normal levels over the next 3 to 5 days regardless of the height of the initial amylase level 23, 24, 25, 26. On the other hand, there is a group of patients who present with acute pancreatitis whose serum amylase levels remain or fluctuate above the upper normal limit for over a week 23. Such prolonged hyperamylasemia has been reported to be related to pancreatic complications, such as pseudocysts or pancreatic necrosis 13, 27. However, some patients with prolonged hyperamylasemia have no identifiable complications and recover their serum amylase levels after a week. The clinical characteristics of patients with such prolonged hyperamylasemia including complicated and uncomplicated cases as well as their prognoses have not yet been clarified 28.
Patients with prolonged hyperamylasemia (prolonged elevation of serum amylase level) would have the presence of pancreatic complications, such as pseudocyst, pancreatic necrosis, or pancreatic abscess 13, 19. However, there are some cases that do not have any identifiable causes or complications related to prolonged hyperamylasemia. A previous study reported that 24/78 (30.8%) patients had hyperamylasemia over 10 days, and that 29% of patients with prolonged hyperamylasemia did not have obvious cause for the prolonged elevation of serum amylase level 29. Another study showed that 6/233 (2.6%) patients were observed to have significant hyperamylasemia for periods over 21 days 30. Among six patients, there were three cases of pseudocysts, 2 cases of persistent pancreatitis, and 1 case without any complications. In etiologic aspect, there was a study that high amylase levels persisted longer in alcohol than biliary causes 29. A study by Kim et al 15 also revealed that 45.2% of alcohol causes was related to prolonged hyperamylasemia, but only 26.8% in biliary causes. Other related factors to prolonged hyperamylasemia in that study were higher computed tomography (CT) severity index, pancreatic necrosis, pseudocyst, and moderately severe pancreatitis 15. These suggest that prolonged hyperamylasemia might be related to more pancreatic injury 15.
Your doctor may also recommend other tests, depending on your symptoms or other conditions you may have. A urine amylase test may be ordered along with or following a blood amylase test. One or both may also be ordered periodically if your doctor wants to monitor or evaluate the effectiveness of treatment and determine whether amylase levels increase or decrease over time.
Diagnosis of acute pancreatitis is confirmed by medical history, physical examination, and typically a blood test (amylase or lipase) for digestive enzymes of the pancreas. Lipase is an enzyme produced by your pancreas that helps the body digest fats. A lipase test measures the amount of lipase in the blood. Your doctor may order a lipase test if you are having abdominal pains or other symptoms that could be caused by pancreatitis. Lipase may also be elevated due to other issues in your pancreas, the use of certain medications, or health conditions such as kidney disease, cancer, and problems with the gallbladder or esophagus. Blood amylase or lipase levels are typically elevated 3 times the normal level during acute pancreatitis. Serum lipase to amylase ratio may also be used to determine the cause of acute pancreatitis, with a higher ratio positively correlating with the specificity of alcohol as the cause if it is more than 2 it could suggest alcoholic pancreatitis 31, 32. However, a prospective follow-up study was unable to confirm the lipase-to-amylase ratio as a reliable indicator of alcoholic pancreatitis 33.
In some cases when the blood tests are not elevated and the diagnosis is still in question, abdominal imaging, such as a computed tomography (CT) scan, ultrasound or endoscopic ultrasound might be performed. Stool tests that measure levels of fat in your stools may also be ordered to find out why your digestive system isn’t absorbing nutrients.
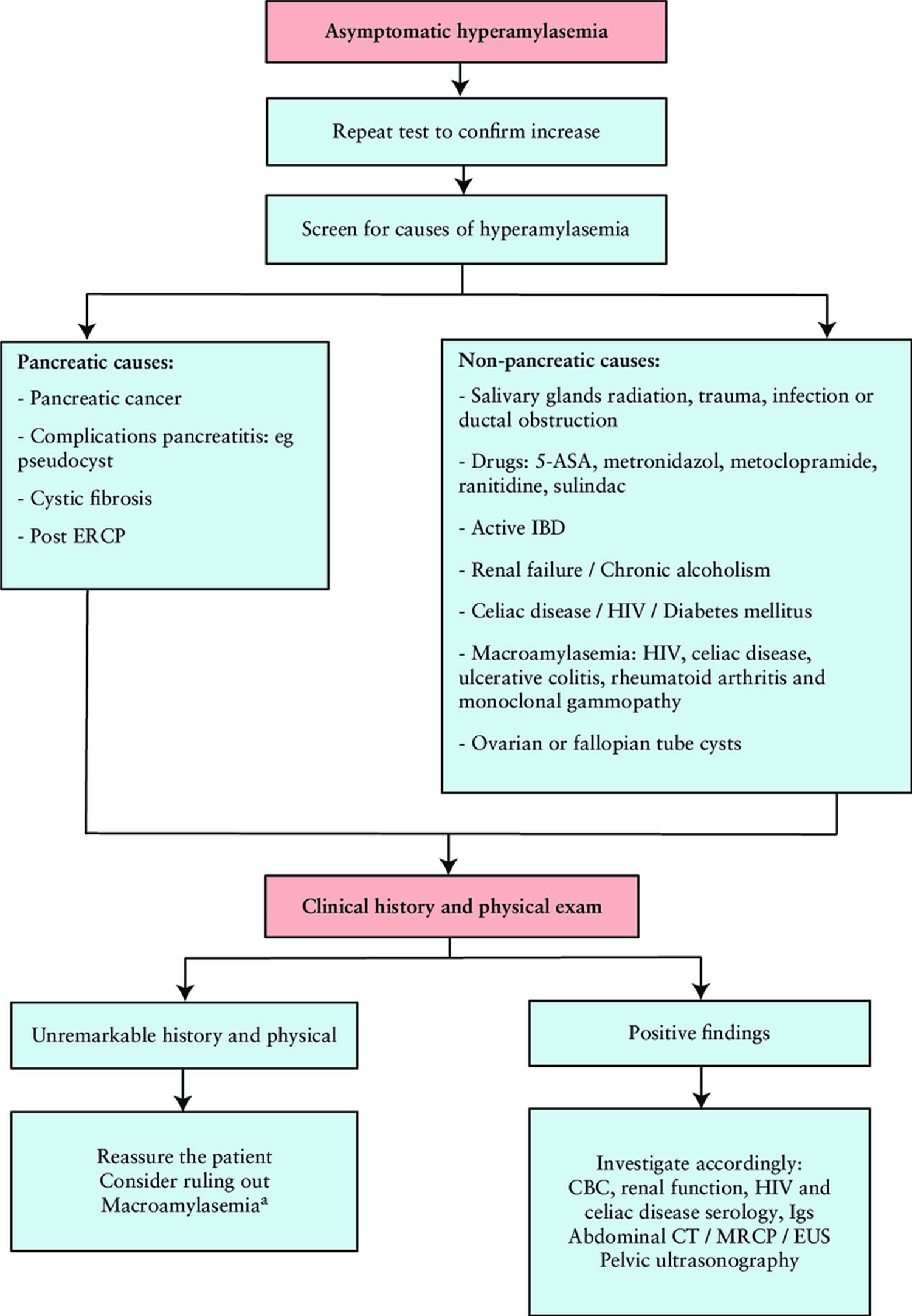
Figure 1. Hyperamylasemia diagnostic algorithm
Footnotes: Approach to asymptomatic hyperamylasemia in inflammatory bowel disease (IBD). Molecular weight of serum amylase will be increased in macroamylasemia. Amylase-to-creatinine ratio (24-h urine): in macroamylasaemia the ratio will be reduced since there is decreased glomerular filtration of the macroamylase complexes.
Abbreviations: 5-ASA = aminosalicylates; CBC = complete blood count; CT = computed tomography; ERCP = endoscopic retrograde cholangiopancreatography; EUS = endoscopic ultrasound; HIV = human immunodeficiency virus; Igs = serum immunoglobulin; MRCP = magnetic resonance cholangiopancreatography.
[Source 34 ]Hyperamylasemia symptoms
A blood amylase test may be ordered if you have signs or symptoms of pancreatitis (inflammation of the pancreas). However, serum amylase is not the most appropriate test for diagnosing pancreatitis as it lacks specificity. Although blood amylase level is increased in around 75% of cases of pancreatitis, serum amylase may be within the normal range, even in a case of massive pancreatic necrosis 7.
Acute pancreatitis usually begins with gradual or sudden pain in the upper abdomen that sometimes extends to the back. The pain may be mild at first and become worse after eating. The pain is often severe, constant, and commonly lasts for several days in the absence of treatment. Other acute pancreatitis symptoms can include:
- Pain in the upper belly.
- Severe upper abdominal pain that radiates to the back or feels worse after eating.
- Tenderness when touching the belly.
- Loss of appetite.
- Fever.
- Rapid pulse.
- Upset stomach.
- Swollen and tender abdomen.
- Nausea and vomiting.
- Yellowing of the eyes or skin (jaundice).
Chronic pancreatitis signs and symptoms include:
- Pain in the upper belly.
- Belly pain that feels worse after eating.
- Losing weight without trying.
- Oily, loose, fatty, foul-smelling stools (steatorrhea)
Some people with chronic pancreatitis only develop symptoms after they get complications of the disease.
Hyperamylasemia complications
Prolonged hyperamylasemia is associated with complications of acute pancreatitis such as the presence of pancreatic pseudocysts, necrosis, or abscess 35. Prolonged hyperamylasemia has also been shown to be independently associated with alcohol use 15.
Pancreatitis can cause serious complications, including:
- Kidney failure. Acute pancreatitis may result in the kidneys not filtering waste from the blood. Artificial filtering, called dialysis, may be needed for short-term or long-term treatment.
- Breathing problems. Acute pancreatitis can cause changes in how the lungs work, causing the level of oxygen in the blood to fall to dangerously low levels.
- Infection. Acute pancreatitis can make the pancreas vulnerable to infections. Pancreatic infections are serious and require intensive treatment, such as surgery or other procedures to remove the infected tissue.
- Pseudocyst. Acute and chronic pancreatitis can cause fluid and debris to collect in a “pocket” in the pancreas, called a pseudocyst. A large pseudocyst that ruptures can cause complications such as internal bleeding and infection.
- Malnutrition. With both acute and chronic pancreatitis, the pancreas may not produce enough enzymes for the digestive system. This can lead to malnutrition, diarrhea and weight loss.
- Diabetes. Diabetes can develop when chronic pancreatitis damages cells that produce insulin.
- Pancreatic cancer. Long-standing inflammation in the pancreas is a risk factor for cancer of the pancreas.
Hyperamylasemia causes
Hyperamylasemia is defined as a twofold or greater increase in serum amylase to a level exceeding the upper limit of normal (>99 U/L) 1. A variety of organs and body secretions contain amylase activity. The pancreas and salivary glands contain amylase concentrations that are several orders of magnitude greater than other organs with 40%-45% from your pancreas and 55%-60% from your salivary glands 6. The other locations of amylase include fallopian tubes and cyst fluid, testes, lungs, thyroid, tonsils, breast milk, sweat, tears, and some malignant neoplasms 36. They contribute little to the serum amylase level.
Many conditions have been reported to cause hyperamylasemia. Although hyperamylasemia is commonly assumed to be due to the release of amylase into the serum by the diseased organ, the precise relationship between hyperamylasemia and an affecting condition is not entirely clear 36.
Hyperamylasemia or high amylase level in the blood is most commonly the result of:
- Pancreatitis
- Salivary gland-related causes include 37, 38, 39:
- Trauma to the salivary gland
- Radiation to the neck area involving the parotid gland
- Salivary gland obstruction with calculi,
- Another cause of damage to the salivary gland is from chronic alcoholism. Salivary amylase levels are three times higher than normal in 10% of patients with alcoholism; this may be related to chronic liver disease.
- Decreased metabolic clearance of amylase can also lead to hyperamylasemia and can be due to:
- Kidney failure
- Liver failure (i.e., hepatitis or cirrhosis)
- Amylase released from an involved organ
- Macroamylasemia. Macroamylasemia is a benign condition in which the amylase molecule binds with a large complex molecule (eg, immunoglobulin, polysaccharide), thereby decreasing renal clearance and prolonging its half-life 40. About 2%-5% of patients with hyperamylasemia have macroamylasemia. Macroamylasemia occurs in settings of inflammatory states, including celiac disease, rheumatoid arthritis, and monoclonal gammopathy. In the inflammatory state, amylase is bound to macromolecules such as immunoglobins and polysaccharides to form large complexes. These complexes are too large to be excreted by the kidney and result in isolated hyperamylasemia.
- Intestinal disease (e.g., inflammatory disease of the small intestine, mesenteric ischemia, mesenteric infarction, intestinal obstruction, appendicitis, and peritonitis). Gut diseases usually result in increased P-type isoamylase because of increased absorption of amylase from the intestinal lumen. Gut perforation is associated with leakage of intestinal contents into the peritoneum causing inflammation and absorption of amylase across the inflamed peritoneum. This can result in hyperamylasemia.
- Female reproductive tract disease (e.g., ruptured ectopic pregnancy, fallopian or ovarian cysts, salpingitis). Ruptured ectopic pregnancy, fallopian or ovarian cysts, and salpingitis can result in increased S-type isoamylase.
- Malignancy (e.g., lung, ovary, pancreas, pheochromocytoma, thymoma, multiple myeloma, breast). Ectopic amylase production by lung, ovary, pancreas, and colon malignancies; pheochromocytoma; thymoma; multiple myeloma (increased salivary amylase); and breast cancer (increased pancreatic amylase) are miscellaneous causes of hyperamylasemia.
- Acidosis (ketoacidosis and nonketotic acidosis) 7. Acidosis, which can be due to (1) ketoacidosis that results in increased S-type and P-type isoamylases or (2) nonketotic acidosis that results in increased S-type isoamylase, can cause hyperamylasemia.
- Balloon-assisted enteroscopy 41, 42, 43
Rare cases of hyperamylasemia have been reported in association with systemic lupus erythematosus (SLE), as well as with ciprofloxacin treatment 40. Other causes of hyperamylasemia include pneumonia (increased salivary amylase), cerebral trauma, burns, abdominal aortic aneurysms (increased pancreatic amylase), drugs (increased salivary and/or pancreatic amylase), anorexia nervosa and bulimia (increased salivary amylase), nonpathologic (increased salivary and/or pancreatic amylase), and organophosphate poisoning 40. Postprocedure balloon-assisted enteroscopy has also been associated with elevated amylase levels; measure pancreatic amylase levels rather than total amylase levels following these procedures 41, 44, 42, 43.
Elevated pancreatic enzymes can be found in critically injured trauma patients with hemorrhagic shock even in the absence of true pancreatitis 45. Reviewing data from 2,711 critically injured trauma patients who had not suffered pancreatic injury, Malinoski and colleagues 45 found that 481 (18%) of these patients had elevated amylase levels (defined in the study as more than twice the upper limit of normal amylase levels). The investigators also found that, in comparison with patients without elevated serum amylase, a greater proportion of patients with elevated serum levels presented in hemorrhagic shock (16% vs 8%), required massive transfusion (19% vs 9%), or developed organ failure (34% vs 16%) 45. Their mortality rate was higher as well (23% vs 13%). Similarly, patients with elevated serum lipase also were more likely to need massive transfusion or to suffer from organ failure. The investigators could not determine whether the higher pancreatic enzyme levels reported in the study resulted from ischemia of the pancreas or from the translocation of intraluminal enteric pancreatic enzymes 45.
Hyperamylasemia may occur due to 2:
- Acute pancreatitis
- Alcohol consumption
- Cancer of the pancreas, ovaries, or lungs
- Cholecystitis (inflammation of the gallbladder)
- Gallbladder disease
- Infection of the salivary glands called sialoadenitis (may be caused by bacteria, mumps) or a blockage of the salivary gland duct
- Intestinal blockage or obstruction
- Macroamylasemia. Macroamylasemia is a benign condition in which the amylase molecule binds with a large complex molecule (eg, immunoglobulin, polysaccharide), thereby decreasing renal clearance and prolonging its half-life 40. About 2%-5% of patients with hyperamylasemia have macroamylasemia.
- Pancreatic or bile duct blockage
- Perforated ulcer
- Ectopic or ruptured tubal pregnancy
- Pelvic inflammatory disease
- Viral hepatitis.
In acute pancreatitis, inflammation of pancreatic cells leads to the secretion of amylase into the bloodstream. Pathologies that involve trauma of the organs, such as blunt trauma to the pancreas or parotid gland or even endoscopic retrograde cholangiopancreatography (ERCP) to the pancreatic duct, can lead to the release of stored amylase. Given amylase is cleared by the kidney and the reticuloendothelial system, renal failure and liver disease (i.e., hepatitis or cirrhosis) are associated with hyperamylasemia. Chronic alcohol abuse can also lead to hyperamylasemia and is thought to be related to liver damage 46.
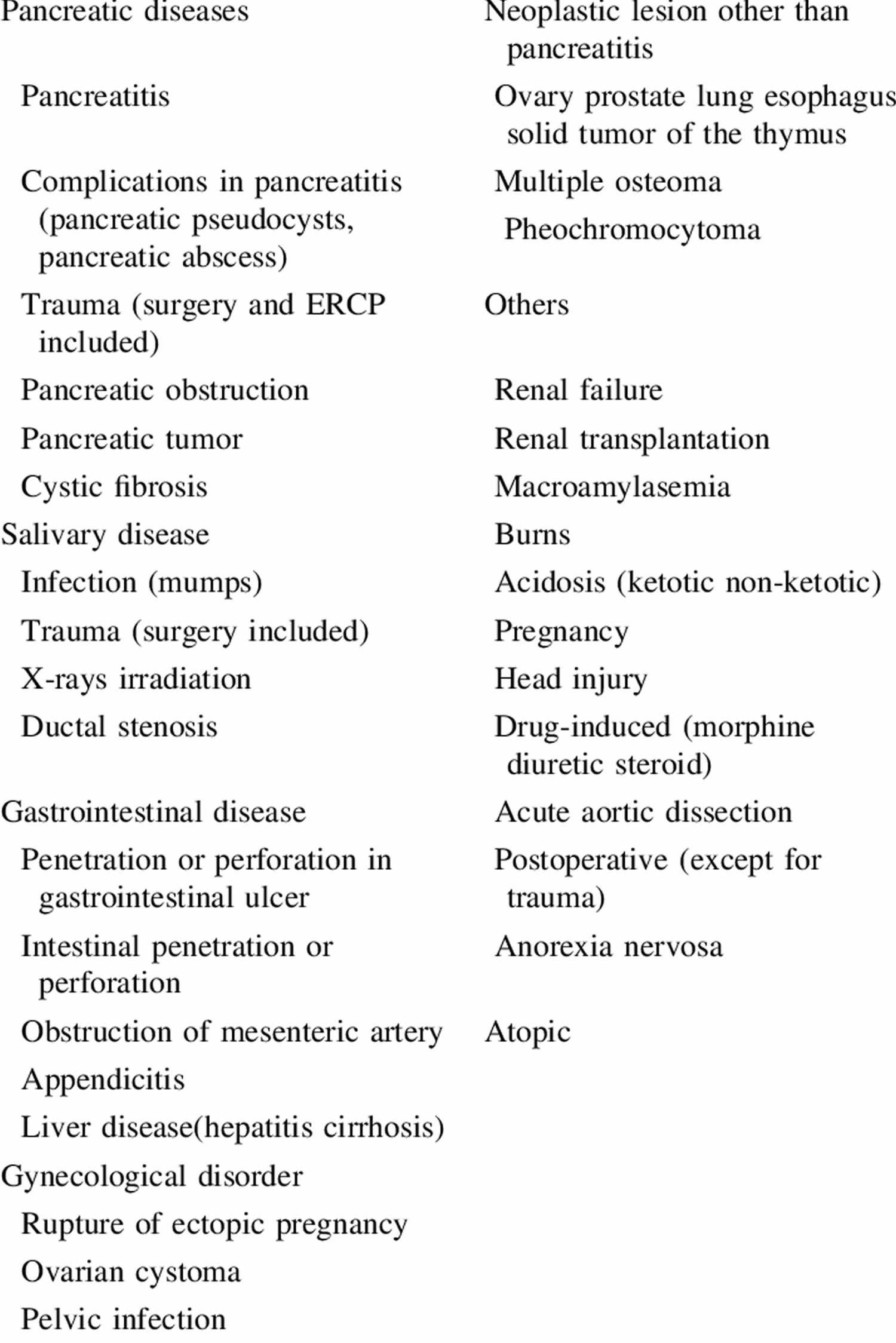
Figure 2. Causes of hyperamylasemia
[Source 47 ]Pancreatic causes
Acute or chronic pancreatitis is associated with hyperamylasemia. In acute pancreatitis, serum amylase is usually elevated 3-fold and then returns to normal by 3-7 days. Prolonged hyperamylasemia in patients experiencing a first attack of acute pancreatitis is associated with recurrence of acute pancreatitis 15. Patients with pancreatitis associated with hypertriglyceridemia or those with considerable acinar cell injury due to previous episodes of pancreatitis or chronic pancreatitis may not exhibit hyperamylasemia 40.
Other reasons for hyperamylasemia that are associated with pancreatitis are pseudocysts, pancreatic ascites, pancreatic trauma and choledocholithiasis 45. Pancreatic trauma can be a result of blunt trauma, abdominal or retroperitoneal surgery, or endoscopic retrograde cholangiopancreatography (ERCP) 45, 5. Trauma related to ERCP is thought to result from the regurgitation of amylase into the blood, which may occur in 75% of ERCPs, but most have no evidence of pancreatic injury. A 3- to 4-times increase in serum amylase levels 4 hours after ERCP predicts the occurrence of complicating postprocedure pancreatitis. In patients presenting with biliary-type abdominal pain, a 3-fold increase in serum amylase levels that returns to normal within 48-72 hours suggests stone passage through the common bile duct.
Risk factors for developing post-ERCP hyperamylasemia appear to include difficult cannulation and pancreatography, and age younger than 60 years, as well as a previous history of diabetes, biliary duct stent placement, and nasobiliary drainage 16, 17.
Conditions can lead to acute pancreatitis, including:
- Blockage in the bile duct caused by gallstones.
- Heavy alcohol use.
- Certain medicines.
- High triglyceride levels in the blood.
- High calcium levels in the blood.
- Pancreas cancer.
- Injuries from trauma or surgery.
Risk factors that increase your risk of pancreatitis include:
- Excessive alcohol use. Research shows that having four or five drinks a day increases the risk of pancreatitis.
- Cigarette smoking. Compared with nonsmokers, smokers are on average three times more likely to develop chronic pancreatitis. Quitting smoking can decrease the risk.
- Obesity. People with a body mass index (BMI) of 30 or higher are at increased risk of pancreatitis.
- Diabetes. Having diabetes increases the risk of pancreatitis.
- Family history of pancreatitis. A number of genes have been linked to chronic pancreatitis. A family history of the disease is linked to an increased risk, especially when combined with other risk factors.
Conditions that can lead to chronic pancreatitis include:
- Damage from repeated acute pancreatitis.
- Heavy alcohol use.
- Inherited genes linked to pancreatitis.
- High triglyceride levels in the blood.
- High calcium levels in the blood.
Sometimes, a cause for pancreatitis is never found. This is known as idiopathic pancreatitis.
Drugs
Drugs that can increase amylase measurements include 2:
- Asparaginase
- Aspirin
- Birth control pills
- Cholinergic medicines
- Ethacrynic acid
- Methyldopa
- Opiates (codeine, meperidine, and morphine)
- Thiazide diuretics
Hyperamylasemia differential diagnosis
Hyperamylasemia may occur due to 2:
- Acute pancreatitis
- Chronic pancreatitis
- Complications of acute pancreatitis, such as abscess, pseudocyst, ascites
- Alcohol consumption
- Chronic alcohol abuse
- Cancer of the pancreas, ovaries, breast, thymoma, multiple myeloma, pheochromocytoma, colon or lungs
- Cholecystitis (inflammation of the gallbladder)
- Gallbladder disease
- Infection of the salivary glands called sialoadenitis (may be caused by bacteria, mumps) or a blockage of the salivary gland duct
- Intestinal blockage or obstruction
- Inflammatory bowel disease
- Macroamylasemia
- Pancreatic or bile duct blockage
- Trauma (ERCP, blunt trauma, recent surgery)
- Perforated ulcer
- Ectopic or ruptured tubal pregnancy
- Pelvic inflammatory disease
- Sjogren syndrome
- Anorexia/bulimia
- Kidney failure
- Liver disease (hepatitis, cirrhosis, hepatocellular carcinoma)
- Ketotic and non-ketotic acidosis
- Viral hepatitis.
Drugs that can increase amylase measurements include 2:
- Asparaginase
- Aspirin
- Birth control pills
- Cholinergic medicines
- Ethacrynic acid
- Methyldopa
- Opiates (codeine, meperidine, and morphine)
- Thiazide diuretics
Hyperamylasemia diagnosis
Serum amylase is primarily used to support the diagnosis of acute pancreatitis despite its low specificity. In acute pancreatitis, the serum amylase is increased at least 3-fold in approximately 75% of cases on the initial day of symptoms; then, it usually returns to normal by 3-7 days. The specificity of the test increases with higher levels of the enzyme. If the patient has severe epigastric pain that can be reproduced on palpation during a physical examination and has a serum amylase elevated to three times the upper limit of normal or higher, a diagnosis of acute pancreatitis can be made without further imaging.
A patient with asymptomatic chronic hyperamylasemia almost never has pancreatic disease as the cause of the amylase elevation 48.
Serum amylase measurements are not very sensitive or specific for pancreatic injury because they may be normal in patients with preexisting acinar injury or chronic pancreatitis and because many other causes of hyperamylasemia are described (see Hyperamylasemia causes) 7. In pancreatitis with associated hypertriglyceridemia, serum amylase levels may be erroneously normal. This is attributed to an inhibitor associated with triglyceride elevations that interferes with the assay for the enzyme. Diluting the serum can reduce the activity of the inhibitor such that a recalculation of serum amylase can uncover the true serum amylase levels.
If abdominal pain is associated with an elevated serum amylase but less than three times the upper limit of normal, additional imaging with computed tomography (CT scan) with contrast can be made. Additional laboratory workup such as complete blood count, basic metabolic panel, alanine aminotransferase (ALT), calcium, albumin, aspartate aminotransferase (AST), and direct and total bilirubin can also be obtained to guide the diagnosis. Magnetic resonance imaging (MRI) and magnetic resonance cholangiopancreatogram (MRCP) can also be used to find pancreatic pathologies and may reveal pancreatic pseudocysts or ascites 49.
Amylase levels can also be obtained after an endoscopic retrograde cholangiopancreatogram (ERCP) due to its value in predicting postprocedure pancreatitis 50. An amylase level that is done within a few hours post-ERCP is valuable in predicting postprocedure pancreatitis. In a study, it was observed that a 6-hour amylase level more than five times normal had an 86% predictive accuracy 51, 50.
In patients with isolated amylase elevation without the presence of any other symptoms, the diagnosis of macroamylasemia should be considered. Macroamylasemia is a benign condition in which the amylase molecule binds with a large complex molecule (eg, immunoglobulin, polysaccharide), thereby decreasing renal clearance and prolonging its half-life 40. About 2%-5% of patients with hyperamylasemia have macroamylasemia. Macroamylasemia occurs in settings of inflammatory states, including celiac disease, rheumatoid arthritis, and monoclonal gammopathy. In the inflammatory state, amylase is bound to macromolecules such as immunoglobins and polysaccharides to form large complexes. These complexes are too large to be excreted by the kidney and result in isolated hyperamylasemia. Macroamylasemia is diagnosed using the amylase-to-creatinine clearance ratio (ACCR). Amylase-to-Creatinine Clearance Ratio (ACCR) is reduced to a ratio of less than one in macroamylasemia due to poor filtration of the large macroamylase complexes.
Amylase-to-Creatinine Clearance Ratio (ACCR) formula is as follows 52:
- Amylase-to-Creatinine Clearance Ratio (ACCR) = [amylase (urine) x creatinine (serum) x 100]/[amylase (serum) x creatinine (urine)]
An Amylase-to-Creatinine Clearance Ratio (ACCR) of less than 1% suggests macroamylasemia. An Amylase-to-Creatinine Clearance Ratio (ACCR) of greater than 5% suggests acute pancreatitis. However, the Amylase-to-Creatinine Clearance Ratio (ACCR) is also known to be increased in diabetic ketoacidosis and renal disease and after surgery. Because findings of urinary amylase are relatively nonspecific, calculations for urinary amylase excretion have almost no clinical value. Generally, the Amylase-to-Creatinine Clearance Ratio (ACCR) measurement has been abandoned, except to confirm a diagnosis of macroamylasemia, which is characterized by a low Amylase-to-Creatinine Clearance Ratio (ACCR) 10.
For patients with isolated hyperamylasemia negative for macroamylasemia or abdominal pain with no other specific signs or symptoms to suggest alternative diagnoses, no further evaluation is needed 5.
An amylase level obtained within a few hours after an endoscopic retrograde cholangiopancreatogram (ERCP) has value in predicting postprocedure pancreatitis. In one study, a 6-hour level of greater than 5 times normal had a predictive accuracy of 86% 51.
In patients undergoing pancreatoduodenectomy, a postoperative serum amylase level less than 130 IU/l on day 0 allows early and reliable categorization of patients being at the least risk for the development of postoperative pancreatic fistula 53. This could be taken as an indicator to identify patients appropriate for early removal of surgical drains 53.
Serum lipase can also be collected, though the co-ordering of both tests has not been shown to increase diagnostic sensitivity and specificity 13.
A lipase-to-amylase ratio is not a reliable indicator of alcoholic pancreatitis. However, if lipase-to-amylase ratio is more than 2 it could suggest alcoholic pancreatitis 31.
Hyperamylasemia treatment
Treatment of hyperamylasemia will be directed at the suspected underlying cause. Asymptomatic isolated hyperamylasemia without suspicion of any underlying cause is benign and does not warrant treatment 5.
In patients where the cause of hyperamylasemia is a parotid disease, appropriate management should be started to treat the underlying parotid illness. With treatment, the inflammation of the parotid gland reduces and serum amylase levels return to baseline 5.
In most cases, acute pancreatitis may improve with therapy, but approximately 15% of patients develop severe disease 54, 55, 56, 57, 58. Severe acute pancreatitis can lead to life-threatening failure of multiple organs and to infection. More-serious pancreatitis requires treatment in a hospital and can cause life-threatening complications. Therefore, it is extremely important to seek medical attention if experiencing signs or symptoms of acute pancreatitis.
Treatment of acute pancreatitis begins with a hospital stay to manage your symptoms and complications. These include:
- Pain Control. Pancreatitis can cause severe pain. Your healthcare team will give you medicines to help control the pain. Intravenous medications are effective in controlling pain associated with acute pancreatitis. Nausea is a common symptom and can be due to pancreatic inflammation as well as slowing of your bowels. Effective intravenous medications are available for nausea. Pain and nausea will decrease as the inflammation resolves.
- Intravenous (IV) Fluids. One of the primary therapies for acute pancreatitis is adequate early fluid resuscitation, especially within the first 24 hours of onset. Pancreatitis is associated with a lot of swelling and inflammation. Giving fluids intravenously prevents dehydration and ensures that the rest of the organs in your body get adequate blood flow to support the healing process.
- Fluid resuscitation is typically provided at a rate of 5 ml/kg/hr to 10 ml/kg/hour for all patients 5. In patients with severe volume loss, rapid repletion should be given with up to 20 ml/kg of fluid over 30 minutes, followed by 3 ml/kg/hour for 8 to 12 hours 5. Reassess fluid requirements every 6 hours over the next 24 to 48 hours based on clinical assessment of volume status, creatinine, and blood urea nitrogen (BUN) values. The target heart rate should be less than 120 beats/minute with mean arterial pressure between 65 mmHg to 85 mmHg and urine output of at least 0.5 ml/kg/hour to 1 ml/kg/hour 5. For most mild cases of acute pancreatitis, patients can be managed with intravenous (IV) fluids and resume a low-fat solid diet within 24 hours as tolerated if pain and nausea/vomiting symptoms are improving 59.
- Nutritional Support. Initially, no nutrition is given to rest your pancreas and bowels during the first 24 to 48 hours. After 48 hours, a plan to provide nutrition should be implemented because acute pancreatitis is a highly active state of inflammation and injury that requires a lot of calories to support the healing process. In most cases, patients can start to take in food on their own by 48 hours. If this is not possible, then a feeding tube that is passed through your nose into the intestines can be used to provide nutrition. This method is safer than providing nutrition intravenously. There is no benefit to using probiotics for acute pancreatitis.
Treatment of Underlying Issues
When your symptoms and complications are under control, other treatments are used to treat underlying causes. If the acute pancreatitis is thought to be due to gallstones, medication, high triglycerides, or high calcium levels within the patient’s body (or other external causes), directed therapy can be implemented.
- Procedures to open bile ducts. A procedure called Endoscopic Retrograde Cholangiopancreatography (ERCP) is used to locate and remove a gallstone. ERCP is a procedure in which a physician with specialized training passes an endoscope (a flexible, thin tube with a camera attached at the end) through the patient’s mouth and into the first part of the small intestine, where the bile duct and pancreatic duct exit. With this device, a small catheter can be passed into the bile duct to remove gallstones that might have gotten stuck and are the cause of pancreatitis. In certain situations, a special catheter (a tiny piece of plastic or metal that looks like a straw) can also be passed into a narrowed pancreatic or bile duct to keep it open. This procedure is called Stent Placement. It is well documented that ERCP may itself trigger acute pancreatitis 60, 61; risk factors include difficult cannulation, age below 60 years, history of diabetes, a stent in the biliary duct, and nasobiliary drainage 16, 17. However, there are several clearly defined situations when urgent ERCP is indicated for acute pancreatitis.
- Sphincterotomy. Using a small wire on the endoscope, a physician finds the muscle that surrounds the pancreatic duct or bile duct and makes a tiny cut to enlarge the duct opening. When a pseudocyst is present, the duct is drained.
- Balloon Dilatation. Some endoscopes have a small balloon that a physician uses to dilate, or stretch, a narrowed pancreatic or bile duct. A temporary stent can be placed for a few months to keep the duct open.
- Gallstone Removal. The endoscope is used to remove pancreatic or bile duct stones with a tiny basket. Gallstone removal is sometimes performed along with a sphincterotomy.
- Gallbladder surgery. If gallstones caused the pancreatitis, surgery to remove the gallbladder may be recommended. This procedure is called a cholecystectomy.
- Treatment for alcohol dependence. If excessive alcohol use has caused pancreatitis, a treatment program for alcohol addiction is recommended. Continuing to drink alcohol worsens pancreatitis and leads to serious complications.
- Changes in medicines. If a medicine is the likely cause of acute pancreatitis, your doctor will work with you to find other options.
- Antioxidant Therapies. Basic and clinical evidence suggests that the development of both acute pancreatitis and chronic pancreatitis can be associated with oxidative stress. Findings show that free radical activity and oxidative stress indices are higher in the blood and duodenal juice of patients with pancreatitis. Based on these findings, the idea of using antioxidant regimens in the management of both acute pancreatitis and chronic pancreatitis as a supplement and complementary in combination with its traditional therapy is reasonable. In practice, however, the overall effectiveness of antioxidants is not known, and the best mixture of agents and dosages is not clear. Currently, a trial of a mixture of antioxidants containing vitamin C, vitamin E, selenium, and methionine is reasonable as one component of overall medical management. In summation, there is no definite consensus on the dosage, length of therapy, and ultimately, the benefits of antioxidant therapy in the management of acute pancreatitis or chronic pancreatitis. Further well-designed clinical studies are needed to determine the appropriate combination of agents, time of initiation, and duration of therapy.
Chronic pancreatitis may require additional treatments, including:
- Pain management. Chronic pancreatitis often causes severe, long-term pain. In addition to prescribing medicine, your healthcare professional will look for causes or complications of chronic pancreatitis that cause pain. Treatments may include procedures to improve drainage from the pancreas or injections to block nerve signals from the pancreas to the brain. You may be referred to a pain specialist.
- Enzymes to improve digestion. When chronic pancreatitis causes diarrhea or weight loss, you may take pancreatic enzyme supplements. Taken with each meal, these enzyme supplements help your body break down and use the nutrients in food.
- Changes to your diet. Your doctor may refer you to a dietitian who can help you plan low-fat meals that are high in nutrients.
Hyperamylasemia prognosis
Prolonged hyperamylasemia for over a week after an initial episode of acute pancreatitis may be associated with future recurrence 15. However, amylase level does not play a role in determining the severity or the cause of acute pancreatitis 18. There is no benefit of trending amylase levels once the diagnosis of acute pancreatitis has been made 21.
Patients with a prolonged hyperamylasemia would have more risk of developing pancreatic complications, such as necrosis, pseudocyst, or abscess 13, 19.
References- Teshima CW, Aktas H, Kuipers EJ, Mensink PB. Hyperamylasemia and pancreatitis following spiral enteroscopy. Can J Gastroenterol. 2012 Sep;26(9):603-6. doi: 10.1155/2012/696187
- Amylase – blood. https://medlineplus.gov/ency/article/003464.htm
- Tsianos EB, Jalali MT, Gowenlock AH, Braganza JM. Ethnic ‘hyperamylasaemia’: clarification by isoamylase analysis. Clin Chim Acta. 1982 Sep 1;124(1):13-21. doi: 10.1016/0009-8981(82)90314-x
- Ueda M, Araki T, Shiota T, Taketa K. Age and sex-dependent alterations of serum amylase and isoamylase levels in normal human adults. J Gastroenterol. 1994 Apr;29(2):189-91. doi: 10.1007/BF02358681
- Lam R, Muniraj T. Hyperamylasemia. [Updated 2022 Dec 11]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK559273
- Hyperamylasemia. https://emedicine.medscape.com/article/186389-overview
- Muniraj T, Dang S, Pitchumoni CS. PANCREATITIS OR NOT?–Elevated lipase and amylase in ICU patients. J Crit Care. 2015 Dec;30(6):1370-5. doi: 10.1016/j.jcrc.2015.08.020
- Argiris A, Mathur-Wagh U, Wilets I, Mildvan D. Abnormalities of serum amylase and lipase in HIV-positive patients. Am J Gastroenterol. 1999 May;94(5):1248-52. doi: 10.1111/j.1572-0241.1999.01074.x
- Pieper-Bigelow C, Strocchi A, Levitt MD. Where does serum amylase come from and where does it go? Gastroenterol Clin North Am. 1990 Dec;19(4):793-810.
- Hyperamylasemia. https://emedicine.medscape.com/article/186389-overview#a4
- Elman R, Arneson N, Graham E. Value of blood amylase estimations in the diagnosis of pancreatic disease: a clinical study. Arch Surg 1929;19:943–67.
- Banks PA, Bollen TL, Dervenis C, Gooszen HG, Johnson CD, Sarr MG, Tsiotos GG, Vege SS; Acute Pancreatitis Classification Working Group. Classification of acute pancreatitis–2012: revision of the Atlanta classification and definitions by international consensus. Gut. 2013 Jan;62(1):102-11. doi: 10.1136/gutjnl-2012-302779
- Yadav D, Agarwal N, Pitchumoni CS. A critical evaluation of laboratory tests in acute pancreatitis. Am J Gastroenterol. 2002 Jun;97(6):1309-18. doi: 10.1111/j.1572-0241.2002.05766.x
- Steinberg W, Tenner S. Acute pancreatitis. N Engl J Med. 1994 Apr 28;330(17):1198-210. doi: 10.1056/NEJM199404283301706
- Kim YS, Chang JH, Kim TH, Kim CW, Kim JK, Han SW. Prolonged hyperamylasemia in patients with acute pancreatitis is associated with recurrence of acute pancreatitis. Medicine (Baltimore). 2020 Jan;99(3):e18861. doi: 10.1097/MD.0000000000018861
- He QB, Xu T, Wang J, Li YH, Wang L, Zou XP. Risk factors for post-ERCP pancreatitis and hyperamylasemia: A retrospective single-center study. J Dig Dis. 2015 Aug;16(8):471-8. doi: 10.1111/1751-2980.12258
- Li GZ, Wang F, Fang J, Zha HL, Zhao Q. Risk Factors for Post-Endoscopic Retrograde Cholangiopancreatography Pancreatitis: Evidence from 1786 Cases. Med Sci Monit. 2018 Nov 26;24:8544-8552. doi: 10.12659/MSM.913314
- Papachristou GI, Whitcomb DC. Predictors of severity and necrosis in acute pancreatitis. Gastroenterol Clin North Am. 2004 Dec;33(4):871-90. doi: 10.1016/j.gtc.2004.07.004
- Clavien PA, Burgan S, Moossa AR. Serum enzymes and other laboratory tests in acute pancreatitis. Br J Surg. 1989 Dec;76(12):1234-43. doi: 10.1002/bjs.1800761205
- Powers RD, Guertler AT. Abdominal pain in the ED: stability and change over 20 years. Am J Emerg Med. 1995 May;13(3):301-3. doi: 10.1016/0735-6757(95)90204-X
- Chase CW, Barker DE, Russell WL, Burns RP. Serum amylase and lipase in the evaluation of acute abdominal pain. Am Surg. 1996 Dec;62(12):1028-33.
- Wan S, Arifi AA, Chan CS, Ng CS, Wan IY, Lee TW, Yim AP. Is hyperamylasemia after cardiac surgery due to cardiopulmonary bypass? Asian Cardiovasc Thorac Ann. 2002 Jun;10(2):115-8. doi: 10.1177/021849230201000205
- Veith FJ, Filler RM, Berard CW. Significance of prolonged elevation of the serum amylase. Ann Surg 1963;158:20–6. doi: 10.1097/00000658-196307000-00005
- Winslet M, Hall C, London NJ, Neoptolemos JP. Relation of diagnostic serum amylase levels to aetiology and severity of acute pancreatitis. Gut. 1992 Jul;33(7):982-6. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1379418/pdf/gut00574-0138.pdf
- Vissers RJ, Abu-Laban RB, McHugh DF. Amylase and lipase in the emergency department evaluation of acute pancreatitis. J Emerg Med. 1999 Nov-Dec;17(6):1027-37. doi: 10.1016/s0736-4679(99)00136-5
- Banks PA. Practice guidelines in acute pancreatitis. Am J Gastroenterol. 1997 Mar;92(3):377-86.
- Grossman MS. Prolonged hyperamylasemia following acute pancreatitis. Am J Dig Dis 1964;9:618–24. doi: 10.1007/BF02232120
- Kim YS, Chang JH, Kim TH, Kim CW, Kim JK, Han SW. Prolonged hyperamylasemia in patients with acute pancreatitis is associated with recurrence of acute pancreatitis. Medicine (Baltimore). 2020 Jan;99(3):e18861. doi: 10.1097/MD.000000000001886
- Bockus HL, Kalser MH, Roth JL, et al. Clinical features of acute inflammation of the pancreas; analysis of ninety-four attacks in seventy-eight patients. AMA Arch Intern Med 1955;96:308–21. doi: 10.1001/archinte.1955.00250140030003
- Veith FJ, Filler RM, Berard CW. Significance of prolonged elevation of the serum amylase. Ann Surg 1963;158:20–6. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1408353/pdf/annsurg00948-0028.pdf
- Yilmaz UE, Yilmaz N, Titiz I, Basaranoglu M, Tarcin O. The utility of amylase and lipase as reliable predictive markers for functioning renal graft. Ann Transplant. 2012 Jul-Sep;17(3):77-84. doi: 10.12659/aot.883461
- Tenner SM, Steinberg W. The admission serum lipase:amylase ratio differentiates alcoholic from nonalcoholic acute pancreatitis. Am J Gastroenterol. 1992 Dec;87(12):1755-8.
- Pezzilli R, Billi P, Barakat B, Miglio F. Lipase-amylase ratio does not determine the etiology of acute pancreatitis. Another myth bites the dust. J Clin Gastroenterol. 1998 Jan;26(1):34-8. doi: 10.1097/00004836-199801000-00010
- Lídia Roque Ramos, David B. Sachar, Christopher J. DiMaio, Jean-Frédéric Colombel, Joana Torres, Inflammatory Bowel Disease and Pancreatitis: A Review, Journal of Crohn’s and Colitis, Volume 10, Issue 1, January 2016, Pages 95–104, https://doi.org/10.1093/ecco-jcc/jjv153
- Schmidt J, Lewandrowski K, Fernandez-del Castillo C, Mandavilli U, Compton CC, Warshaw AL, Rattner DW. Histopathologic correlates of serum amylase activity in acute experimental pancreatitis. Dig Dis Sci. 1992 Sep;37(9):1426-33. doi: 10.1007/BF01296014
- Hyperamylasemia. https://emedicine.medscape.com/article/186389-overview#a2
- Chen CC, Chen SY, Chen YS, Lo CY, Cheng PW. Mycobacterium fortuitum-induced persistent parotitis: successful therapy with clarithromycin and ciprofloxacin. Head Neck. 2007 Nov;29(11):1061-4. doi: 10.1002/hed.20626
- Gokel Y, Gulalp B, Acikalin A. Parotitis due to organophosphate intoxication. J Toxicol Clin Toxicol. 2002;40(5):563-5. doi: 10.1081/clt-120014648
- Ericson S, Sjöbäck I. Salivary factors in children with recurrent parotitis. Part 2: Protein, albumin, amylase, IgA, lactoferrin lysozyme and kallikrein concentrations. Swed Dent J. 1996;20(5):199-207.
- Hyperamylasemia. https://emedicine.medscape.com/article/186389-overview#a3
- Pata C, Akyüz U, Erzin Y, Mutlu N, Mercan A, Dirican A. Post-procedure elevated amylase and lipase levels after double-balloon enteroscopy: relations with the double-balloon technique. Dig Dis Sci. 2010 Jul;55(7):1982-8. doi: 10.1007/s10620-009-0956-4
- Zepeda-Gómez S, Barreto-Zuñiga R, Ponce-de-León S, Meixueiro-Daza A, Herrera-López JA, Camacho J, Tellez-Avila F, Valdovinos-Andraca F, Vargas-Vorackova F. Risk of hyperamylasemia and acute pancreatitis after double-balloon enteroscopy: a prospective study. Endoscopy. 2011 Sep;43(9):766-70. doi: 10.1055/s-0030-1256473
- Tsujikawa T, Bamba S, Inatomi O, Hasegawa H, Ban H, Nishida A, Imaeda H, Itoh A, Saotome T, Sasaki M, Andoh A. Factors affecting pancreatic hyperamylasemia in patients undergoing peroral single-balloon enteroscopy. Dig Endosc. 2015 Sep;27(6):674-8. doi: 10.1111/den.12449
- Aktas H, Mensink PB, Haringsma J, Kuipers EJ. Low incidence of hyperamylasemia after proximal double-balloon enteroscopy: has the insertion technique improved? Endoscopy. 2009 Aug;41(8):670-3. doi: 10.1055/s-0029-1214976
- Malinoski DJ, Hadjizacharia P, Salim A, Kim H, Dolich MO, Cinat M, Barrios C, Lekawa ME, Hoyt DB. Elevated serum pancreatic enzyme levels after hemorrhagic shock predict organ failure and death. J Trauma. 2009 Sep;67(3):445-9. doi: 10.1097/TA.0b013e3181b5dc11
- Pezzilli R, Andreone P, Morselli-Labate AM, Sama C, Billi P, Cursaro C, Barakat B, Gramenzi A, Fiocchi M, Miglio F, Bernardi M. Serum pancreatic enzyme concentrations in chronic viral liver diseases. Dig Dis Sci. 1999 Feb;44(2):350-5. doi: 10.1023/a:1026662719514
- Kiriyama, S., Gabata, T., Takada, T., Hirata, K., Yoshida, M., Mayumi, T., Hirota, M., Kadoya, M., Yamanouchi, E., Hattori, T., Takeda, K., Kimura, Y., Amano, H., Wada, K., Sekimoto, M., Arata, S., Yokoe, M. and Hirota, M. (2010), New diagnostic criteria of acute pancreatitis. Journal of Hepato-Biliary-Pancreatic Sciences, 17: 24-36. https://doi.org/10.1007/s00534-009-0214-3
- Dylewski ML, Prelack K, Keaney T, Sheridan RL. Asymptomatic hyperamylasemia and hyperlipasemia in pediatric patients with toxic epidermal necrolysis. J Burn Care Res. 2010 Mar-Apr;31(2):292-6. doi: 10.1097/BCR.0b013e3181d0f448
- Mortelé KJ, Wiesner W, Zou KH, Ros PR, Silverman SG. Asymptomatic nonspecific serum hyperamylasemia and hyperlipasemia: spectrum of MRCP findings and clinical implications. Abdom Imaging. 2004 Jan-Feb;29(1):109-14. doi: 10.1007/s00261-003-0072-4
- Christoforidis E, Goulimaris I, Kanellos I, Tsalis K, Demetriades C, Betsis D. Post-ERCP pancreatitis and hyperamylasemia: patient-related and operative risk factors. Endoscopy. 2002 Apr;34(4):286-92. doi: 10.1055/s-2002-23630
- Kapetanos D, Kokozidis G, Kinigopoulou P, Xiarchos P, Antonopoulos Z, Progia E, Kitis G. The value of serum amylase and elastase measurements in the prediction of post-ERCP acute pancreatitis. Hepatogastroenterology. 2007 Mar;54(74):556-60.
- Dreiling DA, Leichtling JJ, Janowitz HD. The amylase-creatinine clearance ratio. Diagnostic parameter or physiologic phenomenon? Am J Gastroenterol. 1974 Apr;61(4):290-6.
- Palani Velu LK, Chandrabalan VV, Jabbar S, McMillan DC, McKay CJ, Carter CR, Jamieson NB, Dickson EJ. Serum amylase on the night of surgery predicts clinically significant pancreatic fistula after pancreaticoduodenectomy. HPB (Oxford). 2014 Jul;16(7):610-9. doi: 10.1111/hpb.12184
- Crockett SD, Wani S, Gardner TB, Falck-Ytter Y, Barkun AN; American Gastroenterological Association Institute Clinical Guidelines Committee. American Gastroenterological Association Institute Guideline on Initial Management of Acute Pancreatitis. Gastroenterology. 2018 Mar;154(4):1096-1101. doi: 10.1053/j.gastro.2018.01.032
- Lankisch PG, Breuer N, Bruns A, Weber-Dany B, Lowenfels AB, Maisonneuve P. Natural history of acute pancreatitis: a long-term population-based study. Am J Gastroenterol. 2009 Nov;104(11):2797-805; quiz 2806. doi: 10.1038/ajg.2009.405
- Ahmed Ali U, Issa Y, Hagenaars JC, Bakker OJ, van Goor H, Nieuwenhuijs VB, Bollen TL, van Ramshorst B, Witteman BJ, Brink MA, Schaapherder AF, Dejong CH, Spanier BW, Heisterkamp J, van der Harst E, van Eijck CH, Besselink MG, Gooszen HG, van Santvoort HC, Boermeester MA; Dutch Pancreatitis Study Group. Risk of Recurrent Pancreatitis and Progression to Chronic Pancreatitis After a First Episode of Acute Pancreatitis. Clin Gastroenterol Hepatol. 2016 May;14(5):738-46. doi: 10.1016/j.cgh.2015.12.040
- Nøjgaard C. Prognosis of acute and chronic pancreatitis – a 30-year follow-up of a Danish cohort. Dan Med Bull. 2010 Dec;57(12):B4228.
- Takeyama Y. Long-term prognosis of acute pancreatitis in Japan. Clin Gastroenterol Hepatol. 2009 Nov;7(11 Suppl):S15-7. doi: 10.1016/j.cgh.2009.08.022
- Chatila AT, Bilal M, Guturu P. Evaluation and management of acute pancreatitis. World J Clin Cases. 2019 May 6;7(9):1006-1020. doi: 10.12998/wjcc.v7.i9.1006
- Cotton PB, Lehman G, Vennes J, Geenen JE, Russell RC, Meyers WC, Liguory C, Nickl N. Endoscopic sphincterotomy complications and their management: an attempt at consensus. Gastrointest Endosc. 1991 May-Jun;37(3):383-93. doi: 10.1016/s0016-5107(91)70740-2
- Gottlieb K, Sherman S. ERCP and biliary endoscopic sphincterotomy-induced pancreatitis. Gastrointest Endosc Clin N Am. 1998 Jan;8(1):87-114.