What is anaphylaxis
Anaphylaxis also known as anaphylactic shock, is a severe and potentially life-threatening allergic reaction to a trigger such as an allergy 1. Anaphylaxis can occur within seconds or minutes of exposure to something you’re allergic to, such as foods (especially peanuts), medications, and stinging insects (bee stings). Other causes of anaphylaxis include exercise and exposure to latex. Sometimes the offending agent is not identified; these reactions are identified as idiopathic anaphylaxis 2, 3. Anaphylaxis causes your immune system to release a flood of chemicals (histamine, tryptase, leukotrienes, carboxypeptidase A, proteoglycans and prostaglandins) that can cause you to go into shock — your blood pressure drops suddenly and your airways narrow, blocking breathing — resulting in death within minutes. Signs and symptoms of anaphylaxis include a rapid, weak pulse; a skin rash; and nausea and vomiting.
- Anaphylaxis is a medical emergency that requires immediate medical assistance and treatment.
- Anaphylaxis can occur within seconds or minutes of exposure to something you’re allergic to, such as peanuts or bee stings.
Anaphylaxis requires an injection of epinephrine and a follow-up trip to an emergency room 4. If you don’t have epinephrine, you need to go to an emergency room immediately. If anaphylaxis isn’t treated right away, it can be fatal. Sometimes anaphylaxis symptoms go away, and then return a few hours later, so it is important to take these steps as soon as an anaphylactic reaction begins and to remain under medical observation for as long as the reaction and symptoms continue. And, if you’ve experienced anaphylaxis your risk of having another anaphylactic reaction is increased.
Three patterns of anaphylactic reactions have been described based on disease expression 5:
- Uniphasic anaphylaxis accounts for 70% to 90% of anaphylaxis cases, peaks at 30 to 60 minutes, and resolves over the next hour with no recurrence of symptoms.
- Biphasic anaphylaxis is defined by recurrence of symptoms hours after resolution of the initial event in the absence of re-exposure to the trigger 6. Biphasic anaphylaxis has been variably reported to occur in less than 13 to up to 23% of reactions, with a recent report suggesting that 3% of adults and up to 15% of children experience biphasic anaphylaxis 6. Early administration of epinephrine may be beneficial in preventing biphasic reactions; the role of glucocorticoids in preventing this type is unclear but physiologically reasonable.
- Protracted or persistent anaphylaxis refers to the rare reaction lasting for days or even weeks 7.
Jerschow et al 8 examined rates of fatal anaphylaxis in the United States between 1999 and 2010. Using International Classification of Diseases, version 10, diagnostic codes on death certificates, they identified 2,458 anaphylaxis-related deaths over an 11-year period with a prevalence of 0.69 people per million. In this study population (>96% adult), medication-induced anaphylaxis fatalities were the most frequent (58.8%), followed by “unspecified” (19.3%), venom (15.2%), and food (6.2%). Fatal anaphylaxis in the outpatient setting was most commonly food-induced anaphylaxis, whereas drug-induced anaphylaxis was most frequent in the inpatient setting. Two case series reported median time from clinical manifestation to death as 30 to 35 minutes for food, 10 to 15 minutes for insect venom, and 5 minutes for IV medications 9.
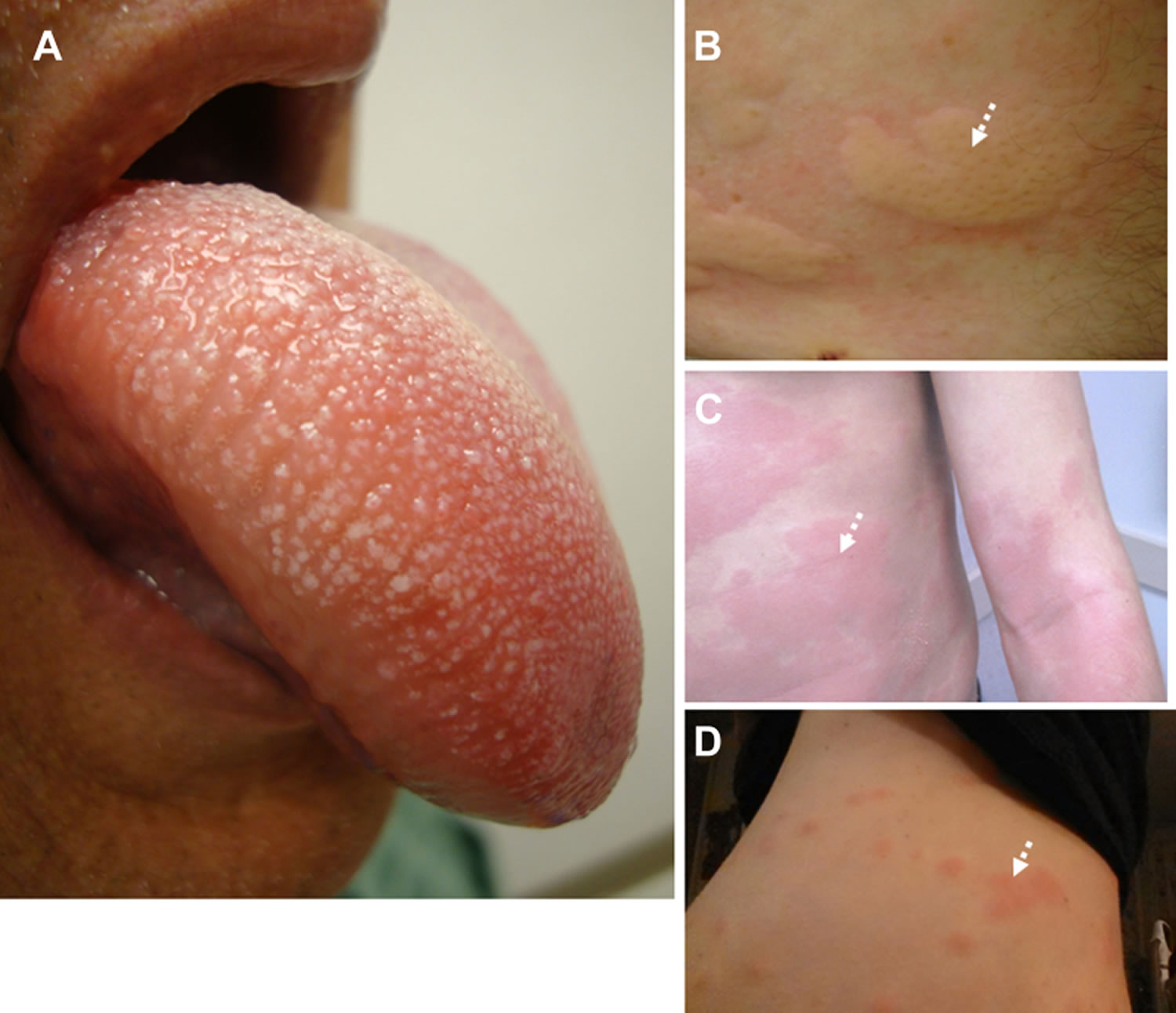
Figure 1. Signs of anaphylaxis
Footnotes: (A) Angioedema of the tongue and oropharynx. (B) Discrete urticarial lesions in a patient with acute allergic reaction. (C) Coalescent urticaria and diffuse erythema in a patient with a severe systemic allergic reaction. (D) Delayed urticarial reactions in response to beef ingestion in an entomologist who had sustained multiple occupation-related tick bites months earlier. White dotted arrows indicate clinical findings.
Urticaria also known as hives, is a transient eruption of erythematous (reddish) or edematous swellings of the dermis and is usually associated with itching. Urticaria can affect any site of the body and tends to be distributed widely. Urticarial weals can be a few millimeters or several centimeters in diameter, colored white or red, with or without a red flare. Each weal may last a few minutes or several hours and may change shape. Weals may be round, or form rings, a map-like pattern, or giant patches.
Angioedema is a skin reaction similar to urticaria, that is characterized by an abrupt, temporary, localized swelling of the deep dermal layer, subcutaneous tissue, and mucous membranes. Although it can affect any part of the body, it most often occurs around the eyelids and lips and genitals. Swelling may occur in other organs, including the intestines and upper airway.
A key differentiation between angioedema and anaphylaxis is urticaria, the oral symptoms and need for airway control can otherwise mimic each other. When in doubt, treat aggressively.
[Source 5 ]Figure 2. Urticaria (hives)
Figure 3. Angioedema
[Source 10 ]- Trouble breathing or noisy breathing
- Difficulty talking more than a few words and/or hoarse voice
- Wheeze
- Cough
- Swelling and tightness of the throat
- Collapse
- Light-headedness or dizziness
- Diarrhea
- Tingling in the hands, feet, lips or scalp
- Swelling of tongue
- Pale and floppy (in young children)
A severe allergic reaction (anaphylaxis) is a medical emergency. Call your local emergency services number immediately. Lay the person down. If they have an adrenaline injector and you are able to administer it, do so.
Anaphylaxis is a medical emergency. It can be very serious if not treated quickly.
If someone has symptoms of anaphylaxis, you should:
- Call your local emergency number for an ambulance immediately – mention that you think the person has anaphylaxis
- Remove any trigger if possible – for example, carefully remove any wasp or bee sting stuck in the skin
- Lie the person down flat and elevate his or her legs – unless they’re unconscious, pregnant or having breathing difficulties
- Use an adrenaline auto-injector if the person has one – but make sure you know how to use it correctly first
- Check the person’s pulse and breathing and, if necessary, administer CPR (cardiopulmonary resuscitation) or other first-aid measures
- Give another injection after 5-15 minutes if the symptoms don’t improve and a second auto-injector is available
If you’re having an anaphylactic reaction, you can follow these steps yourself if you feel able to.
Anaphylaxis signs and symptoms
Anaphylaxis symptoms usually occur within minutes of exposure to an allergen. Sometimes, however, anaphylaxis can occur a half-hour or longer after exposure. In rare cases, anaphylaxis may be delayed for hours.
Anaphylaxis signs and symptoms can include:
- trouble breathing or noisy breathing
- nasal stuffiness/congestion
- difficulty talking more than a few words and/or hoarse voice
- wheeze
- cough
- swelling and tightness of the throat or swollen tongue, which can cause wheezing and trouble breathing
- collapse or loss of consciousness
- light-headedness, dizziness or fainting
- nausea, abdominal pain/cramps, vomiting or diarrhea
- tingling in the hands, feet, lips or scalp
- itchy mouth/throat
- swelling of tongue
- pale and floppy (in young children)
- skin reactions, including hives (urticaria), rash and itching and flushed or pale skin
- a weak and rapid pulse
- low blood pressure (hypotension)
- anxiety, feeling of impending doom, itchy/red/watery eyes, headache, cramping of the uterus
A severe allergic reaction (anaphylaxis) is a medical emergency. The most dangerous symptoms are low blood pressure, breathing difficulty and loss of consciousness, all of which can be fatal. If you have any of these symptoms, particularly after eating, taking medication or being stung by an insect, seek medical care immediately (call your local emergency services number immediately). Don’t wait to see if symptoms go away or get better on their own. If they have an adrenaline injector and you are able to administer it, do so.
Table 1. Clinical features of anaphylaxis
| Organ system | Presentation | Sequelae |
|---|---|---|
| Skin/mucosa | Urticarial eruption | Hypovolemia |
| (80%-90%) | Angioedema | |
| Oropharyngeal | Airway obstruction | |
| Laryngeal | Stridor | |
| Airway obstruction | ||
| Intestinal | Abdominal pain | |
| Flushing | Hypotension | |
| Pruritus (palms/soles/oral/genitalia) | ||
| Bronchopulmonary | Laryngeal edema | Hoarseness/stridor |
| (60%-70%) | Dysphonia | |
| Wheeze/cough | Respiratory failure | |
| Hypoxemia/cyanosis | ||
| Rhinitis | Nasal obstruction | |
| Cardiac | Vasodilation/reduced systemic vascular resistance | Hypotension/shock |
| (40%-50%) | Myocardial vasoconstriction | Reduced cardiac output |
| Myocardial depression | Myocardial ischemia | |
| Arrhythmia | ||
| Cardiac arrest | ||
| Gastrointestinal | Nausea, vomiting | Dehydration |
| (40%-50%) | Diarrhea | Hypovolemia |
| Intestinal edema | Abdominal pain | |
| Neurological | Dizziness | Syncope |
| (<15%) | Confusion | Seizures |
| Headache | ||
| Feeling of impending doom | ||
| Tunnel vision | ||
| Genitourinary | Uterine cramps (♀) | Pain |
| Uterine bleeding (♀) | ||
| Scrotal edema (♂) | Pain |
Footnote: Prevalence of symptom cluster is showed as percentages (%).
[Source 5 ]How to use Adrenaline auto-injectors
People with potentially serious allergies will often be given an adrenaline auto-injector to carry at all times. This can help stop an anaphylactic reaction becoming life threatening.
This should be used as soon as a serious reaction is suspected, either by the person experiencing anaphylaxis or someone helping them.
If you’ve been given an auto-injector, make sure you’re aware how to use it correctly.
There are three main types of adrenaline auto-injector, which are used in slightly different ways.
These are:
- EpiPen – see Figure 1 on how to use Epipen
- Jext
- Emerade
Instructions are also included on the side of each injector if you forget how to use it or someone else needs to give you the injection.
The immediate administration of 0.3 to 0.5 mg of epinephrine (1:1,000) in the mid-outer aspect of the thigh (anterolateral vastus lateralis, mid-muscle belly) is the most essential intervention 11, 12. This may need to be repeated every 5 to 15 minutes 11, 12. Studies show absorption is faster with higher tissue and plasma levels when injected in the mid-outer aspect of the thigh (anterolateral vastus lateralis, mid-muscle belly) compared with other muscles or following subcutaneous administration 11, 12. In emergencies, an epinephrine autoinjector may be used, realizing that the dose is fixed (0.3 mg in adults and 0.15 mg in children weighing <15 kg). In obese individuals, autoinjector needle length may not be sufficient for intramuscular epinephrine delivery 13.
Figure 4. How to use the Epipen
Demonstration of appropriate deployment of the (A) Epipen (released in 2008). For demonstration purposes, a trainer device is being used instead of a live device; however, the coloring of key components is the same as the actual adult device. (B) Open the yellow cap of the carrying case and remove the device from its storage tube (the Epipen Jr. has a green cap). (C) Grasp and form a fist around the unit with the orange tip facing down. (D) With the other hand, remove the blue safety release. (E) Aim the orange tip toward the outer thigh. (F) Swing the arm and jab the device firmly into the outer thigh, at a 90-degree angle, until the device clicks. The needle will deploy at this time into thigh (the autoinjector is designed to work through clothing). Hold the device firmly against the thigh for 10 seconds, so the entire dose will be delivered. (G) Remove the device from the thigh and massage the injection area for 10 seconds. (H) The safety feature of the device, extension of the orange tip that locks into place, will completely cover the needle immediately after use. The used device should be taken to the hospital emergency department with the patient for disposal.
Positioning and resuscitation
Someone experiencing anaphylaxis should be placed in a comfortable position.
- Most people should lie flat.
- Pregnant women should lie on their left side to avoid putting too much pressure on the large vein that leads to the heart.
- People having trouble breathing should sit up to help make breathing easier.
- People who are unconscious should be placed in the recovery position to ensure the airway remains open and clear – place them on their side, making sure they’re supported by one leg and one arm, and open their airway by lifting their chin.
- Avoid a sudden change to an upright posture such as standing or sitting up – this can cause a dangerous fall in blood pressure.
Despite the lack of prospective data, there is uniform agreement that patients should be placed in the supine position (lying horizontally with the face and torso facing up) unless contraindicated by active vomiting, respiratory distress or pregnancy; in which case, the left lateral decubitus position is more appropriate 14. Elevation of the legs (or the Trendelenburg position using a tilting table) remains controversial. This position may play a role initially while the patient is undergoing fluid resuscitation if no vasopressors are available 15. It is important to note that this position is seldom used in the ICU (other than during procedures) as vasopressors and IV fluids are more effective and readily available 12.
If the person’s breathing or heart stops, cardiopulmonary resuscitation (CPR) should be performed immediately.
How to perform a Cardiopulmonary Resuscitation (CPR)
Hands-only CPR
To carry out a chest compression:
- Place the heel of your hand on the breastbone at the center of the person’s chest. Place your other hand on top of your first hand and interlock your fingers.
- Position yourself with your shoulders above your hands.
- Using your body weight (not just your arms), press straight down by 5-6 cm (2-2.5 inches) on their chest.
- Keeping your hands on their chest, release the compression and allow the chest to return to its original position.
- Repeat these compressions at a rate of 100 to 120 times per minute until an ambulance arrives or you become exhausted.
When you call for an ambulance, telephone systems now exist that can give basic life-saving instructions, including advice about CPR. These are now common and are easily accessible with mobile phones.
Cardiopulmonary Resuscitation (CPR) with rescue breaths
If you’ve been trained in CPR, including rescue breaths, and feel confident using your skills, you should give chest compressions with rescue breaths. If you’re not completely confident, attempt hands-only CPR instead (see above).
Adults
- Place the heel of your hand on the center of the person’s chest, then place the other hand on top and press down by 5-6cm (2-2.5 inches) at a steady rate of 100 to 120 compressions per minute.
- After every 30 chest compressions, give two rescue breaths.
- Tilt the casualty’s head gently and lift the chin up with two fingers. Pinch the person’s nose. Seal your mouth over their mouth and blow steadily and firmly into their mouth for about one second. Check that their chest rises. Give two rescue breaths.
- Continue with cycles of 30 chest compressions and two rescue breaths until they begin to recover or emergency help arrives.
Children over one year old
- Open the child’s airway by placing one hand on the child’s forehead and gently tilting their head back and lifting the chin. Remove any visible obstructions from the mouth and nose.
- Pinch their nose. Seal your mouth over their mouth and blow steadily and firmly into their mouth, checking that their chest rises. Give five initial rescue breaths.
- Place the heel of one hand on the center of their chest and push down by 5cm (about two inches), which is approximately one-third of the chest diameter.
- The quality (depth) of chest compressions is very important. Use two hands if you can’t achieve a depth of 5cm using one hand.
- After every 30 chest compressions at a rate of 100 to 120 per minute, give two breaths.
- Continue with cycles of 30 chest compressions and two rescue breaths until they begin to recover or emergency help arrives.
Infants under one year old
- Open the infant’s airway by placing one hand on their forehead and gently tilting the head back and lifting the chin. Remove any visible obstructions from the mouth and nose.
- Place your mouth over the mouth and nose of the infant and blow steadily and firmly into their mouth, checking that their chest rises. Give five initial rescue breaths.
- Place two fingers in the middle of the chest and push down by 4cm (about 1.5 inches), which is approximately one-third of the chest diameter. The quality (depth) of chest compressions is very important. Use the heel of one hand if you can’t achieve a depth of 4cm using the tips of two fingers.
- After 30 chest compressions at a rate of 100 to 120 per minute, give two rescue breaths.
- Continue with cycles of 30 chest compressions and two rescue breaths until they begin to recover or emergency help arrives.
Recovery position
If a person is unconscious but is breathing and has no other life-threatening conditions, they should be placed in the recovery position.
Putting someone in the recovery position will keep their airway clear and open. It also ensures that any vomit or fluid won’t cause them to choke.
Figure 5. Recovery position
The video shows a step-by-step guide to putting someone in the recovery position.
Or you can follow these steps:
- with the person lying on their back, kneel on the floor at their side
- place the arm nearest you at a right angle to their body with their hand upwards, towards the head
- tuck their other hand under the side of their head, so that the back of their hand is touching their cheek
- bend the knee farthest from you to a right angle
- carefully roll the person onto their side by pulling on the bent knee
- the top arm should be supporting the head and the bottom arm will stop you rolling them too far
- open their airway by gently tilting their head back and lifting their chin, and check that nothing is blocking their airway
- stay with the person and monitor their condition until help arrives.
Figure 6. Anaphylaxis Emergency Action Plan
Anaphylaxis causes
Anaphylaxis is most often caused by exposure to an allergen. Your immune system produces antibodies that defend against foreign substances. This is good when a foreign substance is harmful, such as certain bacteria or viruses. But some people’s immune systems overreact to substances that don’t normally cause an allergic reaction. Allergy symptoms aren’t usually life-threatening, but a severe allergic reaction can lead to anaphylaxis. Even if you or your child has had only a mild anaphylactic reaction in the past, there’s a risk of more severe anaphylaxis after another exposure to the allergy-causing substance.
The most common anaphylaxis triggers in children are food allergies, such as to peanuts and tree nuts, fish, shellfish, wheat, soy, sesame and milk. Besides allergy to peanuts, nuts, fish, sesame and shellfish, anaphylaxis triggers in adults include:
- Certain medications, including antibiotics, aspirin and other pain relievers available without a prescription, allergy shots, and the intravenous (IV) contrast used in some imaging procedures.
- Stings from bees, yellow jackets, wasps, hornets, sawflies and fire ants
- Latex or rubber found in surgical gloves, medical supplies, and many products in your home.
- Alpha-gal – Alpha-gal anaphylaxis is severe adverse reactions to the oligosaccharide, alpha-gal, present in mammalian meats and in the chemotherapeutic medication cetuximab were recently described 16. This involves an IgE antibody response to mammalian galactose alpha-1,3-galactose. These patients present with urticaria or delayed anaphylactic reactions to red meat and often have a preceding history of tick bites 17. In the US, these patients often volunteer a history of pruritic tick bites by the Lone Star tick (Amblyomma americanum). The development of urticaria and anaphylaxis 3 to 5 hours after mammalian meat ingestion is consistent with the alpha-gal anaphylaxis 18.
- Pork-cat syndrome. The pork-cat syndrome refers to sensitization to cat albumin that leads to cross-reactivity with pork albumin and resultant allergic reactions and anaphylaxis 19.
- Bird-egg syndrome. The bird-egg syndrome refers to cross-reactivity between proteins present in egg yolk and tissue albumin present in muscle tissue of birds 20. The protein alpha-livetin (also referred to as chicken serum albumin [Gal d 5]), is the allergen component in egg yolk that is involved in anaphylactic manifestations of the bird-egg syndrome.
Although not common, some people develop anaphylaxis from aerobic exercise, such as jogging, or even less intense physical activity, such as walking. Eating certain foods before exercise or exercising when the weather is hot, cold or humid also have been linked to anaphylaxis in some people. Talk with your health care provider about precautions to take when exercising.
In 2008, a world-wide recall of Chinese heparin was initiated based on severe anaphylactic reactions triggered by a contaminant, oversulfated chondroitin sulfate, in several countries 21. Activation of the contact system culminating in kallikrein pathway activation and resultant bradykinin generation was deemed a likely mechanism 22.
Progesterone hypersensitivity can result in symptoms ranging from dermatitis to cyclical anaphylaxis during the luteal phase of the menstrual cycle 23. The patients are usually young women with recurrent perimenstrual anaphylactic events 24. Allergic reactions to human seminal fluid have been described in women manifesting as local urticaria and pruritus to florid anaphylaxis and death 25.
If you don’t know what triggers an allergy attack, certain tests can help identify the allergen. In some cases, the cause of anaphylaxis is not identified (idiopathic anaphylaxis). It is estimated that 30% to 60% of patients presenting with anaphylaxis may have no obvious trigger to explain the disease 26.
Triggers of anaphylaxis
Anaphylaxis is the result of the immune system – the body’s natural defence system – overreacting to a trigger. This is often something you’re allergic to, but isn’t always.
The most common anaphylaxis triggers in children are food allergies, such as to peanuts, and tree nuts, fish, shellfish and milk. Besides allergy to peanuts, nuts, fish and shellfish, anaphylaxis triggers in adults include:
- Foods – including nuts, milk, fish, shellfish, eggs and some fruits
- Medicines – including some antibiotics and non-steroidal anti-inflammatory drugs (NSAIDs) such as aspirin
- Insect stings – particularly wasp and bee stings
- General anesthetic
- Contrast agents – special dyes used in some medical tests to help certain areas of your body show up better on scans
- Latex – a type of rubber found in some rubber gloves and condoms
In some cases, there’s no obvious trigger. This is known as idiopathic anaphylaxis.
Exercise induced anaphylaxis
Although not common, some people develop anaphylaxis from aerobic exercise, such as jogging, or even less intense physical activity, such as walking. Eating certain foods before exercise or exercising when the weather is hot, cold or humid also has been linked to anaphylaxis in some people. Talk with your doctor about precautions to take when exercising.
If you don’t know what triggers your allergy attack, certain tests can help identify the allergen. In some cases, the cause of anaphylaxis is never identified (idiopathic anaphylaxis).
Risk factors for anaphylaxis
There aren’t many known risk factors for anaphylaxis, but some things that might increase your risk include 5:
- Previous anaphylaxis. If you’ve had anaphylaxis once, your risk of having this serious reaction increases. Future reactions might be more severe than the first reaction. Example: latex anaphylaxis, radiocontrast media, exercise-induced anaphylaxis and idiopathic anaphylaxis
- Allergies or asthma. People who have either condition are at increased risk of having anaphylaxis. More severe asthma increases risk for anaphylaxis.
- Certain other conditions. These include heart disease and an abnormal accumulation of a certain type of white blood cell (mastocytosis).
- Age:
- Boys <15 years and women >15 years of age
- Route of allergen introduction: Parenteral > ingested
- Interruption of medication: insulin interruption after desensitization
- Prior exposure: protamine/zinc insulin (NPH) use and reaction to protamine used for heparin reversal
- Geography: higher incidence in Northern latitudes
- Gender:
- Latex, aspirin, and certain medication reactions more common in women.
- Venom reactions more common in men.
Risk factors for severe anaphylaxis
- Infants and elderly
- Comorbidity: asthma, ischemic dilated cardiomyopathy, coronary artery disease
- Medication use
- Antihypertensive medications (beta-adrenergic blockers, calcium channel blockers, angiotensin-converting enzyme inhibitors, angiotensin receptor blockers, direct renin inhibitors)
- Monoamine oxidase inhibitors and tricyclic antidepressants
- Impaired cognition: alcohol, sedative medications, recreational drugs
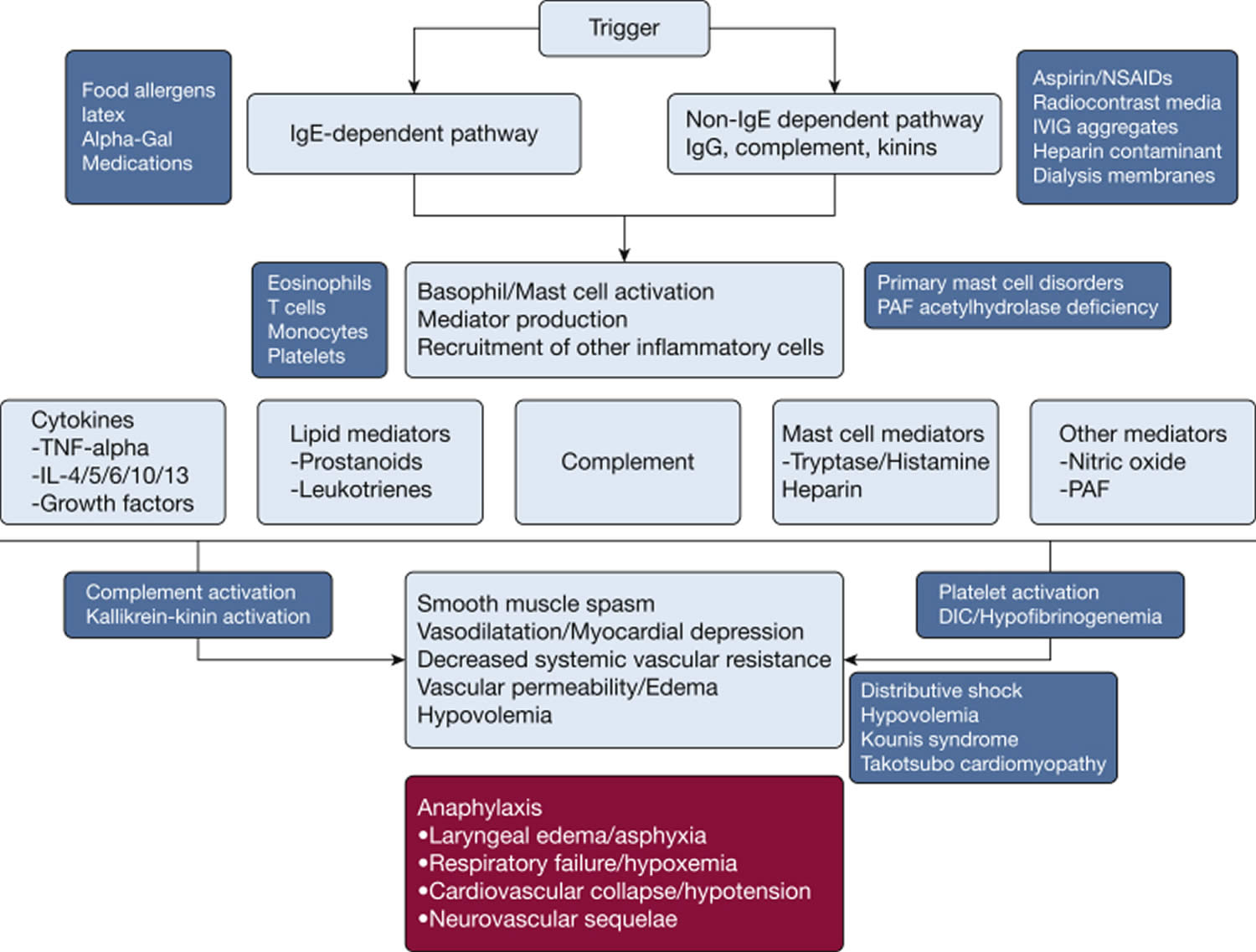
Anaphylaxis pathophysiology
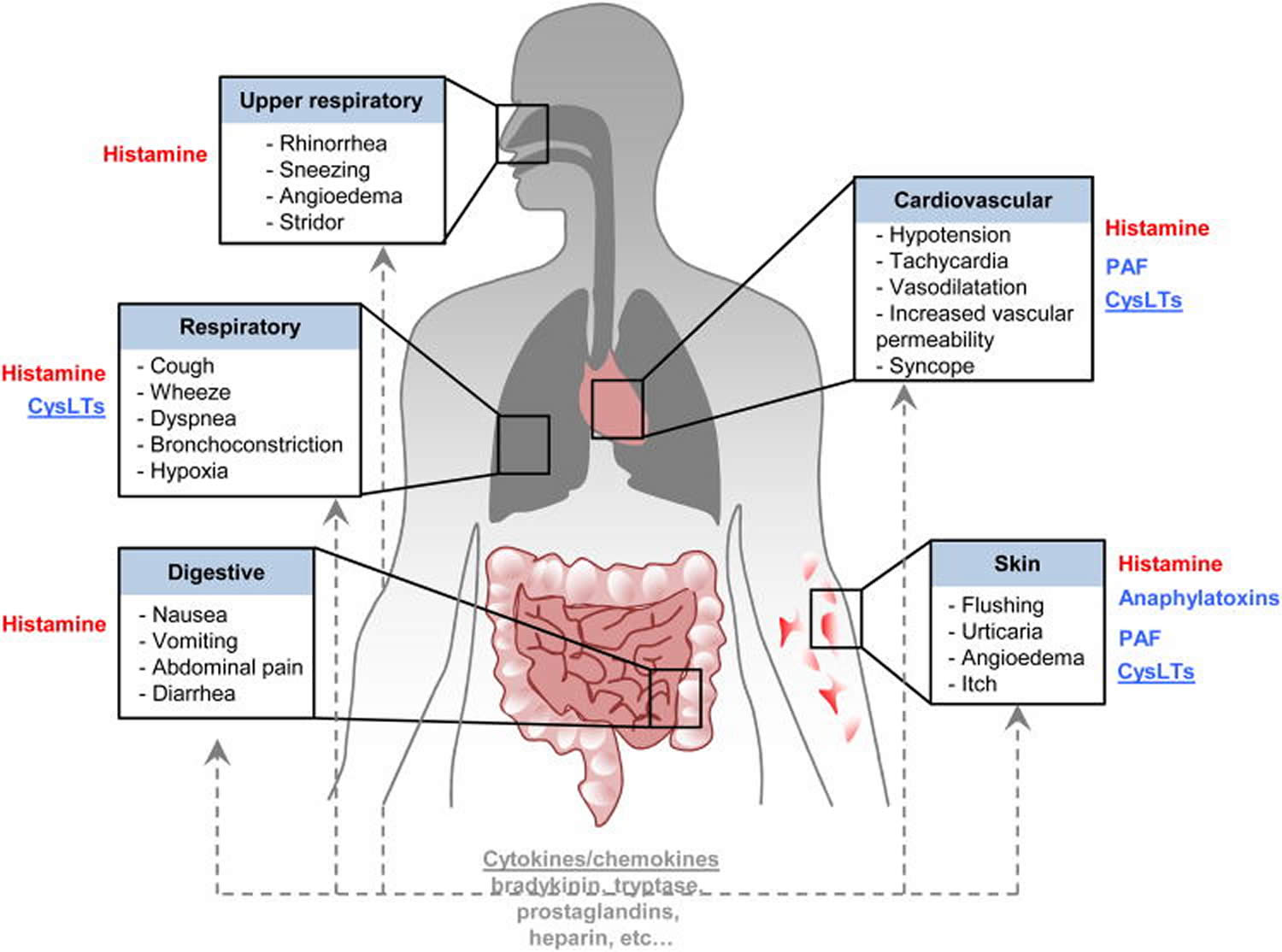
Anaphylaxis is a systemic, life-threatening disorder triggered by mediators released by mast cells and basophils activated via allergic (IgE-mediated) or non-allergic (non-IgE-mediated) mechanisms 5. Anaphylaxis is typically an immunoglobulin E (IgE)-mediated (type 1) hypersensitivity reaction that involves the release of numerous chemical mediators from the degranulation of basophils and mast cells after re-exposure to a specific antigen 27. IgE crosslinking and resultant aggregation of high-affinity receptors induce the rapid release of stored chemical mediators. These chemical mediators include histamine, tryptase, carboxypeptidase A, and proteoglycans. Via activation of phospholipase A, cyclooxygenases, and lipoxygenases they then form arachidonic acid metabolites including leukotrienes, prostaglandins, and platelet-activating factors 28, 29. The inflammatory response is then mediated by TNF-alpha (tumor necrosis factor), both as a preformed and late-phase reactant. The detailed physiology of these chemical mediators is as follows 27:
- Histamine increases vascular permeability and vasodilation leading to hypoperfusion of tissues. The body responds to these changes by increasing heart rate and cardiac contraction.
- Prostaglandin D functions as a bronchoconstrictor, with simultaneous cardiac and pulmonary vascular constriction. It also potentiates peripheral vasodilation thus contributing to the hypo-perfusion of vital organs.
- Leukotrienes add to bronchoconstriction, vascular permeability, and induce airway remodeling.
- The platelet activation factor also acts as a bronchoconstrictor and increases vascular permeability.
- TNF-alpha activates neutrophils (as part of stress response leukocytosis) and increases chemokine synthesis.
Figure 7. Anaphylaxis pathophysiology
Footnote: Mechanisms underlying anaphylaxis-IgE and non-IgE-dependent pathway. First line treatment of anaphylaxis consists of the rapid administration of epinephrine. Although there is evidence that the mediators shown in the figure, particularly histamine and cysteinyl leukotrienes, contribute to some of the various signs and symptoms of anaphylaxis, and anti-histamines are routinely administered to patients with anaphylaxis, pharmacological targeting of such mediators represents second line treatment and should not be considered as an alternative to epinephrine.
In red: Strong evidence for the importance of that mediator, in humans, in the development of some of the signs and symptoms listed in the adjacent box;
In blue: these elements can be important in mouse models of anaphylaxis but their importance in human anaphylaxis is not yet clear (studies in human subjects suggest that cysteinyl leukotrienes may contribute importantly to the bronchoconstriction and enhanced vascular permeability associated with anaphylaxis);
In grey: elements with the potential to influence anaphylaxis, but their importance in human or mouse anaphylaxis not yet clear. Note that some mediators (underlined) are likely to contribute to the development of late consequences of anaphylaxis.
Abbreviations: DIC = disseminated intravascular coagulation; IVIG = intravenous immunoglobulin; NSAIDs = nonsteroidal antiinflammatory drugs; PAF = platelet activating factor; TNF = tumor necrosis factor.
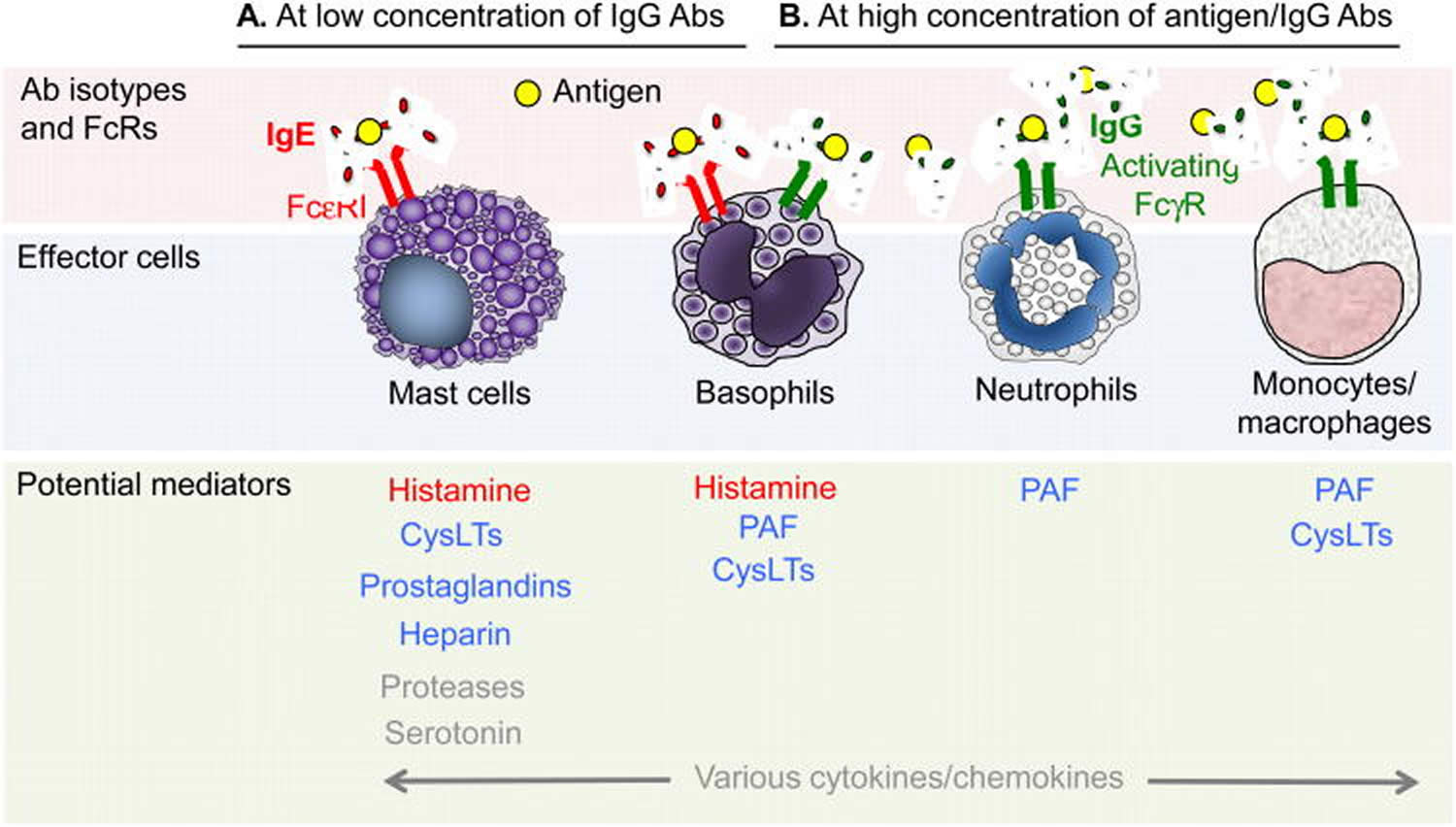
[Source 5 ]Figure 8. Immunological mechanisms of anaphylaxis
Footnotes:
(A) Antigen-specific IgE antibodies and high affinity IgE receptor (FcεRI)-bearing effector cells (e.g. mast cells, basophils) play a dominant role in anaphylaxis induced (sometimes by very small amounts of antigen) when concentrations of IgG antibodies are low.
(B) Mouse models of anaphylaxis suggest that IgG antibodies and Fc-gamma receptor (FcγR)-bearing effector cells (e.g. basophils, macrophages, neutrophils, as well as mast cells) can be important effectors of anaphylaxis induced by large amounts of antigen in the presence of high concentrations of IgG antibodies. Some examples of anaphylaxis likely involve both pathways (A and B). Note that co-engagement of ITAM-containing activating Fc-gamma receptors (FcγRs) or high affinity IgE receptor (FcεRI) with the ITIM-bearing FcγRIIB (on mast cells [in mice, but perhaps not in humans] or basophils [in humans and mice]) can act to diminish effector cell activation. In red: Strong evidence for the importance of these mediators in human anaphylaxis induced by antigen; in blue: These elements can participate in models of anaphylaxis in mice but their importance in human anaphylaxis is not yet clear; in grey: Elements with the potential to influence anaphylaxis, but their importance in human or mouse anaphylaxis not yet clear (e.g., human mast cells are thought to make little or no serotonin).
Abbreviations: IgE = immunoglobulin E; IgG = immunoglobulin G; IL = interleukin; PAF = platelet-activating factor; TNF-α = tumor necrosis factor alpha.
[Source 30 ]Allergic anaphylaxis (IgE-dependent anaphylaxis)
Allergic anaphylaxis also known as type 1 hypersensitivity reaction or immunoglobulin E (IgE)-dependent anaphylaxis, denotes reactions mediated by an immunologic mechanism – for example, IgE-, Ig, or an immune complex complement-related (corresponding to the classic hypersensitivity reactions described by Gell and Coombs) pathways 31, 32. After exposure to the allergen, a series of signals trigger the production of allergen-specific IgE by B cells (sensitization phenomenon). In subsequent exposures, the antigen–allergen-specific IgE complex binds to the Fc-epsilon-RI receptor (FcεRI) on mast cells and/or basophils and, with adequate signaling, activates and degranulates these cells, thereby releasing preformed mediators, enzymes, and cytokines and facilitating the synthesis of de novo inflammatory mediators (eg, tryptase, histamine, leukotrienes, prostaglandins, platelet-activating factor [PAF], cytokines) 30.
The mediators cause allergic symptoms by directly acting on tissues. The reaction is propagated by recruiting and activating additional inflammatory cells – particularly eosinophils, which release more mediators, including lipid-derived mediators such as prostaglandin D2 and cysteinyl leukotrienes 30.
In addition to the classical pathway mediated by IgE, other possible pathways have been described in animal models that are difficult to explore in humans 33. One of these alternative pathways is similar to the IgE-mediated pathway, but involves IgG antibodies. IgG-mediated reactions are mediated by IgG complexes that cross-link to the macrophage low-affinity receptor (FcgRIII) thus stimulating platelet-activating factor [PAF] (rather than histamine) release 34.
Platelet-activating factor (PAF) causes platelet aggregation and release of the potent vasoconstrictor thromboxane A2 and serotonin; acts directly on vascular endothelial cells to increase vascular permeability; decreases cardiac output, which can produce hypotension and cardiac dysfunctions; and increases smooth muscle contraction in the airways, gut, and uterus, among other effects 35.
However, IgE levels alone do not explain an individual’s susceptibility to anaphylaxis 30. Some patients can experience near fatal anaphylaxis despite having low or undetectable levels of circulating allergen-specific IgE 36. On the other hand, allergen-specific IgE can be detected in the plasma of many subjects who do not develop clinical symptoms when exposed to that allergen 37. This is particularly true for hymenoptera venom, where the vast majority (∼80%) of people with IgE antibodies specific for hymenoptera (bees, yellow jackets, wasps, and hornets) venoms have no history of systemic reactions to such venoms 38. Therefore, the presence of antigen-specific IgE antibodies, taken in isolation, does not indicate that the person necessarily will exhibit any, let alone severe, clinical reactivity to the recognized antigens 39.
Although IgG-dependent anaphylaxis has not been demonstrated in humans, it has been hypothesized that IgG antibodies can mediate systemic anaphylaxis if there are large numbers of both IgG and antigen present 40. IgG receptors are capable of activating macrophages and neutrophils to secrete PAF and activate mast cells in vitro, which may contribute to human anaphylaxis 41. Chimeric IgG monoclonal antibodies (mAbs), such as rituximab, have been shown to induce anaphylaxis even in the absence of IgE, suggesting IgG-dependent anaphylaxis 42.
Recent reports with regard to the direct activation of mast cells, independent of those mediated by IgE, indicate that the human G-protein–coupled receptor – MRGPRX2 – may be the receptor for many drugs and cationic proteins, such as quinolone antibiotics (eg, ciprofloxacin, levofloxacin), general anesthetics such as atracuronium and rocuronium, icatibant, and other drugs with tetrahydroisoquinoline (THIQ) motifs 43.
The health condition for IgE-mediated reactions is mast cell and basophil mediator release that causes flushing, pruritus, hives, angioedema, shortness of breath, wheezing, nausea, vomiting, diarrhea, hypotension, oxygen desaturation, and cardiovascular collapse along with other symptoms 30. The common triggers for these reactions include foods, drugs, latex, Hymenoptera (bees, yellow jackets, wasps, and hornets) venoms, and environmental allergens 44. There are important geographic and age-related variations between countries; however, the most common food allergens are peanut, milk, eggs, nuts, shellfish, fruits and vegetables 45; antibiotics such as β-lactams, nonsteroidal anti-inflammatory drugs (NSAIDs), chemotherapeutic agents such as platins and taxanes, chimeric humanized human mAbs, general anesthetics, and immunotherapy allergens are other common allergens both in children and adults 46.
Immunologic non-IgE-mediated reactions
Anaphylaxis has been reported to IV immunoglobulins 47, non-steroidal anti-inflammatory drugs (NSAIDs) 48, dialysis membranes 49, dextrans, iron 50, biological agents, and heparin. In the case of dialysis-associated anaphylaxis, most hypersensitivity reactions to components of the dialysis circuit are due to ethylene oxide or complement activating bio-incompatible membranes, whereas anaphylaxis to erythropoietin, latex, heparin, and medications have also been recorded 49, dextrans, iron 50.
Nonimmunologic anaphylactic reactions
Nonimmunologic triggers for anaphylaxis including physical factors (eg, exercise, cold, heat) and iatrogenic agents (including radiocontrast media and opiates) that can stimulate direct mast cell degranulation 51. In primary mast cell disorders, mast cells can degranulate both independently and in response to allergens such as foods and medications 52.
Anaphylaxis prevention
If you have a serious allergy or have experienced anaphylaxis before, it’s important to try to prevent future episodes.
The following can help reduce your risk:
- Identify any triggers – you may be referred to an allergy clinic for allergy tests to check for anything that could trigger anaphylaxis
- Avoid triggers whenever possible – for example, you should be careful when food shopping or eating out if you have a food allergy
- If you have food allergies, carefully read the labels of all the foods you buy and eat. Manufacturing processes can change, so it’s important to periodically recheck the labels of foods you commonly eat.
- When eating out, ask how each dish is prepared, and find out what ingredients it contains. Even small amounts of food you’re allergic to can cause a serious reaction.
- If you’re allergic to stinging insects, use caution around them. Wear long-sleeved shirts and pants; don’t walk barefoot on grass; avoid bright colors; don’t wear perfumes, colognes or scented lotions; and don’t drink from open soda cans outdoors. Stay calm when near a stinging insect. Move away slowly and avoid slapping at the insect.
- Carry your adrenaline auto-injector at all times – give yourself an injection whenever you think you may be experiencing anaphylaxis, even if you’re not completely sure.
- If you have an epinephrine autoinjector, check the expiration date and be sure to refill your prescription before it expires.
- Wear a medical alert necklace or bracelet to indicate you have an allergy to specific drugs or other substances.
- Be sure to alert all your doctors to medication reactions you’ve had.
Identify triggers
Finding out if you’re allergic to anything that could trigger anaphylaxis can help you avoid these triggers in the future.
If you’ve had anaphylaxis and haven’t already been diagnosed with an allergy, you should be referred to an allergy clinic for tests to identify any triggers.
The most commonly used tests are:
- Skin prick test – your skin is pricked with a tiny amount of a suspected allergen to see if it reacts
- Blood test – a sample of your blood is taken to test its reaction to a suspected allergen
Avoid triggers
If a trigger has been identified, you’ll need to take steps to avoid it in the future whenever possible. See below for advice about avoiding some specific triggers.
Food
You can reduce the chances of being exposed to a food allergen by:
- checking food labels and ingredients
- letting staff at a restaurant know what you’re allergic to so it’s not included in your meal
- remembering some types of food may contain small traces of potential allergens – for example, some sauces contain wheat and peanuts
Insect stings
You can reduce your risk of being stung by an insect by taking basic precautions, such as:
- moving away from wasps, hornets or bees slowly without panicking – don’t wave your arms around or swat at them
- using an insect repellent if you spend time outdoors, particularly in the summer
- being careful drinking out of cans when there are insects around – insects may fly or crawl inside the can and sting you in the mouth when you take a drink
- not walking around outside with bare feet
Some specialist allergy centers can also offer special treatment to help desensitize you to insect stings (immunotherapy).
Medicines
If you’re allergic to certain types of medicines, there are normally alternatives that can be safely used.
For example, if you’re allergic to:
- penicillin – you can normally safely take a different group of antibiotics known as macrolides
- non-steroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen and aspirin – you can normally safely take paracetamol; read the ingredients of things like colds medicines carefully to make sure they don’t contain NSAIDs
- one type of general anesthetic – others are available, or it may be possible to perform surgery using a local anaesthetic or an epidural injection
Always tell any healthcare professional about medicine allergies you have, as they may not be aware of them.
Be prepared
Even if you’re careful, at some point you’ll likely be exposed to what you’re allergic to. Fortunately, you can respond quickly and effectively to an allergy emergency by knowing the signs and symptoms of an anaphylactic reaction and having a plan to quickly treat those symptoms.
It’s important to remember the following:
- carry an auto-injector at all times – there should be no exceptions; you may also be advised to get an emergency card or bracelet with full details of your allergy and doctor’s contact details to alert others
- extremes of heat can make adrenaline less effective – so don’t leave your auto-injector in the fridge or your car’s glove compartment, for example
check the expiry date regularly – an out-of-date injector will offer limited protection - manufacturers offer a reminder service, where you can be contacted near the expiry date – check the information leaflet that comes with your medicine for more information
- don’t delay injecting yourself if you think you may be experiencing anaphylaxis, even if your initial symptoms are mild – it’s better to use adrenaline early and then find out it was a false alarm than delay treatment until you’re sure you’re experiencing severe anaphylaxis
If your child has an auto-injector, they will need to change over to an adult dose once they reach 30kg (approximately 4.5 stone).
Anaphylaxis diagnosis
Your doctor will ask you questions about previous allergic reactions, including whether you’ve reacted to:
- Particular foods
- Medications
- Latex
- Insect stings
To help confirm the diagnosis:
- You might be given a blood test to measure the amount of a certain enzyme (tryptase) that can be elevated up to three hours after anaphylaxis
- You might be tested for allergies with skin tests or blood tests to help determine your trigger
Many conditions have signs and symptoms similar to those of anaphylaxis. Your doctor will want to rule out other conditions.
Total serum tryptase is the biomarker most widely used to confirm a diagnosis of anaphylaxis retrospectively 53. Small amounts of the immature form of tryptase (beta-protryptase) are constitutively secreted into the systemic circulation. Following mast cell and basophil degranulation, total serum tryptase levels increase significantly because of release of mature beta-tryptase. Ideally, serum tryptase should be measured within 1 to 2 hour after symptom onset because tryptase levels typically peak within 60 to 90 minutes after symptom onset but can persist for 6 hours 54.
Plasma histamine levels rise 5 to 10 minutes after the onset of anaphylaxis and can also be assayed. However, plasma histamine levels are only transiently elevated, returning to normal within 60 minutes, making them of little utility if the patient is evaluated greater than 1 hour after symptom onset. Twenty-four-hour urinary histamine metabolites may be elevated for up to 24 hours after the anaphylactic event.
Vadas and colleagues 55 have shown that serum histamine and tryptase levels are not always elevated, even in patients with severe manifestations of anaphylaxis including cutaneous, gastrointestinal and respiratory, or cardiovascular compromise. In addition, serum tryptase levels are not always elevated during food-induced anaphylaxis 56. As a result, there is growing interest in identifying alternative serum biomarkers such as platelet-activating factor (PAF) or carboxypeptidase A3 that more accurately confirm the diagnosis of anaphylaxis and correlate with severity, but these have not yet been developed for clinical use 55.
If the clinical history is suspicious for IgE-mediated anaphylaxis, allergy testing (serum or epicutaneous) is indicated to identify the trigger and often requires referral to a board-certified allergist-immunologist 57. This could be accomplished emergently in the ICU or as an outpatient after discharge.
Clinical criteria of anaphylaxis
A consensus criterion has been constructed to improve clinical recognition of anaphylaxis and to prevent delayed treatment as this poses a great risk to patients.
Clinical criteria for anaphylaxis (1 of the following with onset inside minutes to hours)*
Unknown exposure to an antigen yet rapidly developing urticaria or other skin/mucosal layer symptoms associated with any one of the following:
- Respiratory symptoms (dyspnea, wheeze, stridor, hypoxemia, inability to maintain patency; persistent cough and/or throat clearing can be heralding symptom)
- Hypotension (systolic less than 90 mm Hg or a decrease of greater than 30% from baseline)
- Signs or symptoms of end-organ dysfunction, for example, hypotonia, syncope, incontinence
Likely exposure to an antigen and symptoms involving any 2 of the following body systems:
- Skin symptoms: Skin or mucosal layer (rash, pruritus, erythema, hives [urticaria], swelling of the face, lips, tongue, or uvula)
- Respiratory symptoms: Dyspnea, wheeze, stridor, hypoxemia, inability to maintain patency; persistent cough and/or throat clearing can be heralding symptom
- Hypotension: Systolic less than 90 mm Hg or a decrease of greater than 30% from baseline
- Gastrointestinal symptoms: Persistent painful cramps or vomiting
Known exposure to an antigen and hypotension (systolic less than 90 mm Hg or a decrease of greater than 30% from baseline)
*Note: It is not required to meet these criteria to treat, only to serve as a guide for diagnosis. Angioedema can also mimic these symptoms.
Laboratory testing is of little to no use, as there is no accurate testing for diagnosis or confirmation. Serum histamine is of no use due to transient elevation and late presentation. Serum tryptase can be considered for confirmation of an anaphylactic episode as it remains elevated for several hours, however, as a diagnostic modality, this has low sensitivity.
Kounis syndrome (allergic angina): This is myocardial infarction (heart attack) or ischemia that can occur in the setting of anaphylaxis 58.
Diagnostic criteria of anaphylaxis
Anaphylaxis is highly likely if any one of the following three conditions is satisfied 5.
- Acute onset of illness with:
- Mucocutaneous involvement (pruritus, flushing, urticaria, angioedema) and one of the following:
- A. Respiratory complications (wheezing, stridor, hypoxemia/cyanosis)
- B. Hypotension a or end-organ damage (encephalopathy, kidney injury, etc.)
- Mucocutaneous involvement (pruritus, flushing, urticaria, angioedema) and one of the following:
- Two or more of the following occurring rapidly after exposure to known or likely allergen:
- Mucocutaneous involvement (pruritus, flushing, urticaria, angioedema)
- Respiratory complications (wheezing, stridor, hypoxemia/cyanosis)
- Hypotension a or evidence of end organ hypoperfusion (encephalopathy, kidney injury, etc.)
- Persistent gastrointestinal symptoms (pain, nausea, vomiting)
- Reduced blood pressure soon after exposure to a known allergen.
Note: a Hypotension (low blood pressure) in adults is regarded as systolic blood pressure of <90 mm Hg or greater than a 30% decrease in systolic blood pressure from the patient’s baseline. Hypotension in infants and children: systolic blood pressure <70 mm Hg (1-12 months); <(70 mm Hg + [2x age ]) (1-10 years); <90 mm Hg (11-17 years); or >30% decrease in systolic blood pressure.
Anaphylaxis treatment
During an anaphylactic shock, you might receive cardiopulmonary resuscitation (CPR) if you stop breathing or your heart stops beating. You might also be given medications, including:
- Epinephrine (adrenaline) to reduce your body’s allergic response
- Oxygen, to help you breathe
- Intravenous (IV) antihistamines and cortisone to reduce inflammation of your air passages and improve breathing
- A beta-agonist (such as albuterol) to relieve breathing symptoms
The preferred route of administration for epinephrine is intramuscular injection because it provides more reliable and quicker rise to effective plasma levels than the subcutaneous route 59. An intramuscular 1:1,000 aqueous solution of epinephrine at a dose of 0.01 mg per kg (maximal dose of 0.3 mg in children and 0.5 mg in adults) is given every five to 15 minutes until the patient is without symptoms of respiratory or vascular compromise 60. The onset of action is usually three to five minutes. The use of a commercially made autoinjector is preferred, because dosing errors are common when drawing epinephrine from a vial. Commercial devices allow for a set dose with the correct dilution (e.g., 0.15 mg for patients weighing less than 66 lb [30 kg]; 0.3 mg for patients weighing more than 66 lb) 61. Intravenous epinephrine may be used to manage refractory anaphylaxis in consultation with an intensivist, because dosing requires close cardiovascular monitoring 62.
Epinephrine activates the α1 adrenergic receptors and β1 and β2 adrenergic receptors, leading to immediate vasoconstriction, increased peripheral resistance, decreased mucosal edema, increased cardiac inotropy/chronotropy, and bronchodilation, reversing the airway obstruction and vascular collapse 59. In a retrospective review of food-induced anaphylaxis in 13 children, all seven of the surviving patients received epinephrine within five minutes of severe respiratory symptoms, whereas the six who died did not 63.
- You will need to go to hospital for observation – usually for 6-12 hours – as the symptoms can occasionally return during this period.
In most cases of anaphylaxis, symptoms completely abate with intramuscular epinephrine. Your physician will need to determine the length of postreaction monitoring. The unpredictable nature of biphasic reactions makes this decision difficult, and no guidelines address this issue 64. Reaction severity is not a predictor of biphasic reactions 60. The patient’s ability to recognize symptoms and to self-administer epinephrine using an autoinjector should drive this decision. Ten hours of observation is probably adequate in most situations, but some investigators recommend a minimum of 24 hours 64.
While in hospital:
- An oxygen mask may be used to help breathing
- Fluids may be given directly into a vein to help increase blood pressure
- Additional medications such as antihistamines, steroids, inhaled bronchodilators, and vasopressors may be used to help relieve symptoms
- Corticosteroids are given for the reduction of length or biphasic response of anaphylaxis. There is minimal literature to support this use specifically in anaphylaxis, but it has been proven effective in reactive airway diseases. Therefore, use, dosages, and proposed mechanism of action mimic those of airway management protocols. Methylprednisolone (80 to 125 mg IV) or hydrocortisone (250 to 500 mg IV) are the accepted treatments during the acute phase, after which oral treatment of prednisone (40 to 60 mg daily or divided twice per day) is continued for 3 to 5 days. Again, if the source is unknown and/or there is a concern for a prolonged time prior to physician follow up steroid taper up to 2 weeks may be provided. Mineralocorticoid activity is responsible for fluid retention; in those at risk, dexamethasone and methylprednisolone are the preferred agents as they induce the least mineralocorticoid effect.
- Antihistamines (antagonists H1 and H2) are often routinely used; most commonly is the administration of diphenhydramine 25 to 50 mg IV/IM. While the clinical benefit is unproven in anaphylaxis, its utility is evident in more minor allergic processes. In severe cases, H blockers such as ranitidine (50 mg IV over 5 minutes) or cimetidine (300 mg IV) may also be used in conjunction with H-blocker as there is evidence suggesting histamine has crossover selectivity of receptors. Note that cimetidine has multiple precautions in at-risk populations such as renal or hepatic impaired patients, or those taking beta-blockers. While IV is the initial route during stabilization, once the patient is stabilized they may be switched to oral if continued therapy is desired.
- Bronchodilators are useful adjuncts in patients with bronchospasm. Patients with previous histories of respiratory disease, most notably asthma are at the highest risk. Treated with inhaled beta-agonists are the first-line treatment in wheezing; albuterol alone or as ipratropium bromide/albuterol. If there is refractory wheezing IV magnesium is appropriate with dosage and treatment similar to severe asthma exacerbations.
- Vasopressors may be substituted when a patient requires more doses of epinephrine but has unacceptable side effects from the epinephrine IV infusion (arrhythmia or chest pain).
- Blood tests may be carried out to confirm anaphylaxis
You should be able to go home when the symptoms are under control and it’s thought they won’t return quickly. This will usually be after a few hours, but may be longer if the reaction was severe.
You may be asked to take antihistamine and steroid tablets for a few days after leaving hospital to help stop your symptoms returning.
You will also probably be asked to attend a follow-up appointment with an allergy specialist so you can be given advice about how you can avoid further episodes of anaphylaxis.
An adrenaline auto-injector may be provided for emergency use between leaving hospital and attending the follow-up appointment.
Table 2. Medications used in anaphylaxis treatment
| Medication | Concentration | Dose | Route | Frequency | Adverse Effects |
|---|---|---|---|---|---|
| Epinephrine | 1:1,000 (1 mg/mL) | 0.01 mg/kg 0.3 to 0.5 mg | IM | Every 5-15 min | Tachycardia, palpitations, tachyarrhythmia, anxiety, palpitations, flushing |
| 1:10,000 (0.1 mg/mL) | 0.01 mg/kg 0.5-1.0 mg (5-10 mL) | IV | Every 5-15 min Push | As above | |
| Vasopressin | NA | 0.04 U | IV | Per minute | Ischemia |
| Dopamine | NA | 1-50 mcg/kg | IV | Per minute | Tachycardia, tachyarrhythmia |
| Norepinephrine | NA | 0.02-1 mcg/kg | IV | Per minute | Tachycardia, tachyarrhythmia |
| Albuterol | |||||
| Metered dose inhaler | 2.5 mg per puff | 1-2 puffs (2.5-5 mg) | inhaled | Every 2-4 h | Tachycardia, palpitations, anxiety |
| Nebulized | 2.5 mg/3 mL | 3 mL | inhaled | Every 2-4 h | As above |
| 5 mg/3 mL | 3 mL | inhaled | Continuous | As above | |
| Glucagon | 3-10 mga 0.05-0.1 mg/kg/h | IV IV | Once Continuous | Nausea, vomiting, tachycardia | |
| Diphenhydramine (antihistamine) | |||||
| Treatment | NA | 25-50 mg | IV, by mouth (orally) b | Once | Drowsiness, sedation |
| Prophylaxis | NA | 25-50 mg | Oncec | ||
| Corticosteroids | |||||
| Hydrocortisone | NA | 100 mg | IV | Every 8 h | Hyperglycemia |
| Prednisoned | |||||
| Treatment | NA | 1-2 mg/kg | by mouth (orally) b | Once | Agitation, anxiety, psychosis |
| Prophylaxis | NA | 50 mg | by mouth (orally) b | 13 h, then 7 h, then 1 h before | As above |
Footnotes:
a Infuse slowly over 2-5 min to minimize nausea and vomiting.
b Avoid po medications in patients who are nauseated, vomiting, or unable to protect their airway (unless intubated and gastric tube in place).
c 1 h before procedure.
d IV alternatives should be dosed in prednisone equivalents.
NA = not available
[Source 5 ]Using an autoinjector
Many people at risk of anaphylaxis carry an autoinjector. This device is a combined syringe and concealed needle that injects a single dose of medication when pressed against the thigh. Always replace epinephrine before its expiration date, or it might not work properly.
Using an autoinjector immediately can keep anaphylaxis from worsening and could save your life. Be sure you know how to use the autoinjector. Also, make sure the people closest to you know how to use it.
Long-term treatment
If insect stings trigger your anaphylactic reaction, a series of allergy shots (immunotherapy) might reduce your body’s allergic response and prevent a severe reaction in the future.
Unfortunately, in most other cases there’s no way to treat the underlying immune system condition that can lead to anaphylaxis. But you can take steps to prevent a future attack — and be prepared if one occurs.
- Try to avoid your allergy triggers.
- Carry self-administered epinephrine. During an anaphylactic attack, you can give yourself the drug using an autoinjector (EpiPen, others).
Anaphylaxis prognosis
With rapid and adequate treatment and monitoring, the risk of morbidity and mortality is low. Rapid access to medical care and rapid diagnosis of the disease process are essential to patient prognosis. The first hour after symptoms exposure is responsible for half of the related fatalities 65.
Hospital admission is required in 4% or less of acute allergic reactions diagnosed in the emergency department. If epinephrine is required, as in cases of anaphylaxis, and complete resolution is noted. Emergency department (ED) observation for 4 hours is recommended 27. If no further intervention is required, the patient can be discharged home with a prescription for an epinephrine autoinjector and follow-up is appropriate. If the patient requires airway intervention, is refractory to treatment, or is deemed unstable, admission to the intensive care unit (ICU) for close monitoring is advised 27. For patients with a history of biphasic reactions, severe reactions, beta-blocker use, elderly, those who live alone, or those with poor access to health care, or deemed at risk should be monitored longer.
Along with the prescription for an epinephrine pen, antihistamines and corticosteroids are appropriate for 3 to 5 days. If the inciting source is unknown and the patient will have a prolonged time before follow-up, consider corticosteroid use for 1 to 2 weeks with an appropriate taper. Also consider writing for multiple epinephrine autoinjectors to ensure they are kept in various locations (home, school, work, vehicle). Educate and document the need for 24-hour access to the epinephrine autoinjector is symptoms begin to recur.
Patients with severe allergic reactions and anaphylaxis who take beta-blockers are at greater risk for prolonged or more severe symptoms; consider other classes of medication if possible. Patients may also consider obtaining medical alert bracelets or the like for assistance in the future.
- Simons, F. E., Ardusso, L. R., Bilò, M. B., Cardona, V., Ebisawa, M., El-Gamal, Y. M., Lieberman, P., Lockey, R. F., Muraro, A., Roberts, G., Sanchez-Borges, M., Sheikh, A., Shek, L. P., Wallace, D. V., & Worm, M. (2014). International consensus on (ICON) anaphylaxis. The World Allergy Organization journal, 7(1), 9. https://doi.org/10.1186/1939-4551-7-9[↩]
- Yue, D., Ciccolini, A., Avilla, E., & Waserman, S. (2018). Food allergy and anaphylaxis. Journal of asthma and allergy, 11, 111–120. https://doi.org/10.2147/JAA.S162456[↩]
- Pattanaik D, Lieberman P, Lieberman J, Pongdee T, Keene AT. The changing face of anaphylaxis in adults and adolescents. Ann Allergy Asthma Immunol. 2018 Nov;121(5):594-597. doi: 10.1016/j.anai.2018.07.017[↩]
- Castells M. Diagnosis and management of anaphylaxis in precision medicine. J Allergy Clin Immunol. 2017 Aug;140(2):321-333. doi: 10.1016/j.jaci.2017.06.012[↩]
- LoVerde, D., Iweala, O. I., Eginli, A., & Krishnaswamy, G. (2018). Anaphylaxis. Chest, 153(2), 528–543. https://doi.org/10.1016/j.chest.2017.07.033[↩][↩][↩][↩][↩][↩][↩][↩]
- Lee S, Sadosty AT, Campbell RL. Update on biphasic anaphylaxis. Curr Opin Allergy Clin Immunol. 2016 Aug;16(4):346-51. doi: 10.1097/ACI.0000000000000279[↩][↩]
- Zisa G, Riccobono F, Calamari AM, D’Antonio CD, Galimberti M. A case of protracted hypotension as unique symptom of a biphasic anaphylaxis to amoxicillin. Eur Ann Allergy Clin Immunol. 2009 Apr;41(2):60-1.[↩]
- Jerschow, E., Lin, R. Y., Scaperotti, M. M., & McGinn, A. P. (2014). Fatal anaphylaxis in the United States, 1999-2010: temporal patterns and demographic associations. The Journal of allergy and clinical immunology, 134(6), 1318–1328.e7. https://doi.org/10.1016/j.jaci.2014.08.018[↩]
- Pumphrey RS. Fatal anaphylaxis in the UK, 1992-2001. Novartis Found Symp. 2004;257:116-28; discussion 128-32, 157-60, 276-85.[↩]
- Urticaria and angioedema – an overview. https://www.pcds.org.uk/clinical-guidance/urticaria-and-angioedema[↩]
- Simons, F. E., Ebisawa, M., Sanchez-Borges, M., Thong, B. Y., Worm, M., Tanno, L. K., Lockey, R. F., El-Gamal, Y. M., Brown, S. G., Park, H. S., & Sheikh, A. (2015). 2015 update of the evidence base: World Allergy Organization anaphylaxis guidelines. The World Allergy Organization journal, 8(1), 32. https://doi.org/10.1186/s40413-015-0080-1[↩][↩][↩]
- Lieberman P, Nicklas RA, Randolph C, Oppenheimer J, Bernstein D, Bernstein J, Ellis A, Golden DB, Greenberger P, Kemp S, Khan D, Ledford D, Lieberman J, Metcalfe D, Nowak-Wegrzyn A, Sicherer S, Wallace D, Blessing-Moore J, Lang D, Portnoy JM, Schuller D, Spector S, Tilles SA. Anaphylaxis–a practice parameter update 2015. Ann Allergy Asthma Immunol. 2015 Nov;115(5):341-84. doi: 10.1016/j.anai.2015.07.019[↩][↩][↩][↩]
- Tsai, G., Kim, L., Nevis, I. F., Dominic, A., Potts, R., Chiu, J., & Kim, H. L. (2014). Auto-injector needle length may be inadequate to deliver epinephrine intramuscularly in women with confirmed food allergy. Allergy, asthma, and clinical immunology : official journal of the Canadian Society of Allergy and Clinical Immunology, 10(1), 39. https://doi.org/10.1186/1710-1492-10-39[↩]
- Commins S. P. (2017). Outpatient Emergencies: Anaphylaxis. The Medical clinics of North America, 101(3), 521–536. https://doi.org/10.1016/j.mcna.2016.12.003[↩]
- Brown SG. Cardiovascular aspects of anaphylaxis: implications for treatment and diagnosis. Curr Opin Allergy Clin Immunol. 2005 Aug;5(4):359-64. doi: 10.1097/01.all.0000174158.78626.35[↩]
- Commins, S. P., Satinover, S. M., Hosen, J., Mozena, J., Borish, L., Lewis, B. D., Woodfolk, J. A., & Platts-Mills, T. A. (2009). Delayed anaphylaxis, angioedema, or urticaria after consumption of red meat in patients with IgE antibodies specific for galactose-alpha-1,3-galactose. The Journal of allergy and clinical immunology, 123(2), 426–433. https://doi.org/10.1016/j.jaci.2008.10.052[↩]
- Iweala OI, Burks AW. Food Allergy: Our Evolving Understanding of Its Pathogenesis, Prevention, and Treatment. Curr Allergy Asthma Rep. 2016 May;16(5):37. doi: 10.1007/s11882-016-0616-7[↩]
- Commins, S. P., Jerath, M. R., Cox, K., Erickson, L. D., & Platts-Mills, T. (2016). Delayed anaphylaxis to alpha-gal, an oligosaccharide in mammalian meat. Allergology international : official journal of the Japanese Society of Allergology, 65(1), 16–20. https://doi.org/10.1016/j.alit.2015.10.001[↩]
- Sabbah A, Lauret MG, Chène J, Boutet S, Drouet M. Le syndrome porc-chat ou l’allergie croisée entre viande de porc et épithélia de chat (2e partie) [The pork-cat syndrome or crossed allergy between pork meat and cat epithelia (2)]. Allerg Immunol (Paris). 1994 May;26(5):173-4, 177-80. French.[↩]
- Hemmer, W., Klug, C., & Swoboda, I. (2016). Update on the bird-egg syndrome and genuine poultry meat allergy. Allergo journal international, 25, 68–75. https://doi.org/10.1007/s40629-016-0108-2[↩]
- Hedlund KD, Coyne DP, Sanford DM, Huddelson J. The heparin recall of 2008. Perfusion. 2013 Jan;28(1):61-5. doi: 10.1177/0267659112462274[↩]
- Kishimoto, T. K., Viswanathan, K., Ganguly, T., Elankumaran, S., Smith, S., Pelzer, K., Lansing, J. C., Sriranganathan, N., Zhao, G., Galcheva-Gargova, Z., Al-Hakim, A., Bailey, G. S., Fraser, B., Roy, S., Rogers-Cotrone, T., Buhse, L., Whary, M., Fox, J., Nasr, M., Dal Pan, G. J., … Sasisekharan, R. (2008). Contaminated heparin associated with adverse clinical events and activation of the contact system. The New England journal of medicine, 358(23), 2457–2467. https://doi.org/10.1056/NEJMoa0803200[↩]
- Snyder JL, Krishnaswamy G. Autoimmune progesterone dermatitis and its manifestation as anaphylaxis: a case report and literature review. Ann Allergy Asthma Immunol. 2003 May;90(5):469-77; quiz 477, 571. doi: 10.1016/S1081-1206(10)61838-8[↩]
- Bauer CS, Kampitak T, Messieh ML, Kelly KJ, Vadas P. Heterogeneity in presentation and treatment of catamenial anaphylaxis. Ann Allergy Asthma Immunol. 2013 Aug;111(2):107-11. doi: 10.1016/j.anai.2013.06.001[↩]
- Lee, J., Kim, S., Kim, M., Chung, Y. B., Huh, J. S., Park, C. M., Lee, K. H., & Kim, J. H. (2008). Anaphylaxis to husband’s seminal plasma and treatment by local desensitization. Clinical and molecular allergy : CMA, 6, 13. https://doi.org/10.1186/1476-7961-6-13[↩]
- Fenny N, Grammer LC. Idiopathic anaphylaxis. Immunol Allergy Clin North Am. 2015 May;35(2):349-62. doi: 10.1016/j.iac.2015.01.004[↩]
- McLendon K, Sternard BT. Anaphylaxis. [Updated 2021 Dec 21]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK482124[↩][↩][↩][↩]
- Valenta R, Karaulov A, Niederberger V, Gattinger P, van Hage M, Flicker S, Linhart B, Campana R, Focke-Tejkl M, Curin M, Eckl-Dorna J, Lupinek C, Resch-Marat Y, Vrtala S, Mittermann I, Garib V, Khaitov M, Valent P, Pickl WF. Molecular Aspects of Allergens and Allergy. Adv Immunol. 2018;138:195-256. doi: 10.1016/bs.ai.2018.03.002[↩]
- Jimenez-Rodriguez, T. W., Garcia-Neuer, M., Alenazy, L. A., & Castells, M. (2018). Anaphylaxis in the 21st century: phenotypes, endotypes, and biomarkers. Journal of asthma and allergy, 11, 121–142. https://doi.org/10.2147/JAA.S159411[↩]
- Reber, L. L., Hernandez, J. D., & Galli, S. J. (2017). The pathophysiology of anaphylaxis. The Journal of allergy and clinical immunology, 140(2), 335–348. https://doi.org/10.1016/j.jaci.2017.06.003[↩][↩][↩][↩][↩]
- Johansson SG, Bieber T, Dahl R, Friedmann PS, Lanier BQ, Lockey RF, Motala C, Ortega Martell JA, Platts-Mills TA, Ring J, Thien F, Van Cauwenberge P, Williams HC. Revised nomenclature for allergy for global use: Report of the Nomenclature Review Committee of the World Allergy Organization, October 2003. J Allergy Clin Immunol. 2004 May;113(5):832-6. doi: 10.1016/j.jaci.2003.12.591[↩]
- Ring J, Behrendt H, de Weck A. History and classification of anaphylaxis. Chem Immunol Allergy. 2010;95:1-11. doi: 10.1159/000315934[↩]
- Finkelman, F. D., Khodoun, M. V., & Strait, R. (2016). Human IgE-independent systemic anaphylaxis. The Journal of allergy and clinical immunology, 137(6), 1674–1680. https://doi.org/10.1016/j.jaci.2016.02.015[↩]
- Gillis CM, Jönsson F, Mancardi DA, Tu N, Beutier H, Van Rooijen N, Macdonald LE, Murphy AJ, Bruhns P. Mechanisms of anaphylaxis in human low-affinity IgG receptor locus knock-in mice. J Allergy Clin Immunol. 2017 Apr;139(4):1253-1265.e14. doi: 10.1016/j.jaci.2016.06.058[↩]
- Gill P, Jindal NL, Jagdis A, Vadas P. Platelets in the immune response: Revisiting platelet-activating factor in anaphylaxis. J Allergy Clin Immunol. 2015 Jun;135(6):1424-32. doi: 10.1016/j.jaci.2015.04.019[↩]
- Simons FE, Frew AJ, Ansotegui IJ, Bochner BS, Golden DB, Finkelman FD, Leung DY, Lotvall J, Marone G, Metcalfe DD, Müller U, Rosenwasser LJ, Sampson HA, Schwartz LB, van Hage M, Walls AF. Risk assessment in anaphylaxis: current and future approaches. J Allergy Clin Immunol. 2007 Jul;120(1 Suppl):S2-24. doi: 10.1016/j.jaci.2007.05.001[↩]
- Sicherer SH, Sampson HA. Food allergy. J Allergy Clin Immunol. 2010 Feb;125(2 Suppl 2):S116-25. doi: 10.1016/j.jaci.2009.08.028[↩]
- Haftenberger M, Laußmann D, Ellert U, Kalcklösch M, Langen U, Schlaud M, Schmitz R, Thamm M. Prävalenz von Sensibilisierungen gegen Inhalations- und Nahrungsmittelallergene : Ergebnisse der Studie zur Gesundheit Erwachsener in Deutschland (DEGS1) [Prevalence of sensitisation to aeraoallergens and food allergens: results of the German Health Interview and Examination Survey for Adults (DEGS1)]. Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz. 2013 May;56(5-6):687-97. German. doi: 10.1007/s00103-012-1658-1[↩]
- Hamilton RG. Allergic sensitization is a key risk factor for but not synonymous with allergic disease. J Allergy Clin Immunol. 2014 Aug;134(2):360-1. doi: 10.1016/j.jaci.2014.02.022[↩]
- Finkelman FD. Anaphylaxis: lessons from mouse models. J Allergy Clin Immunol. 2007 Sep;120(3):506-15; quiz 516-7. doi: 10.1016/j.jaci.2007.07.033[↩]
- Sala-Cunill A, Björkqvist J, Senter R, Guilarte M, Cardona V, Labrador M, Nickel KF, Butler L, Luengo O, Kumar P, Labberton L, Long A, Di Gennaro A, Kenne E, Jämsä A, Krieger T, Schlüter H, Fuchs T, Flohr S, Hassiepen U, Cumin F, McCrae K, Maas C, Stavrou E, Renné T. Plasma contact system activation drives anaphylaxis in severe mast cell-mediated allergic reactions. J Allergy Clin Immunol. 2015 Apr;135(4):1031-1043.e6. doi: 10.1016/j.jaci.2014.07.057[↩]
- Castells MC. Anaphylaxis to chemotherapy and monoclonal antibodies. Immunol Allergy Clin North Am. 2015 May;35(2):335-48. doi: 10.1016/j.iac.2015.01.011[↩]
- Spoerl, D., Nigolian, H., Czarnetzki, C., & Harr, T. (2017). Reclassifying Anaphylaxis to Neuromuscular Blocking Agents Based on the Presumed Patho-Mechanism: IgE-Mediated, Pharmacological Adverse Reaction or “Innate Hypersensitivity”?. International journal of molecular sciences, 18(6), 1223. https://doi.org/10.3390/ijms18061223[↩]
- Altman, A. M., Camargo, C. A., Jr, Simons, F. E., Lieberman, P., Sampson, H. A., Schwartz, L. B., Zitt, F. M., Collins, C., Tringale, M., Wilkinson, M., & Wood, R. A. (2015). Anaphylaxis in America: A national physician survey. The Journal of allergy and clinical immunology, 135(3), 830–833. https://doi.org/10.1016/j.jaci.2014.10.049[↩]
- Mostmans Y, Blykers M, Mols P, Gutermuth J, Grosber M, Naeije N. Anaphylaxis in an urban Belgian emergency department: epidemiology and aetiology. Acta Clin Belg. 2016 Apr;71(2):99-106. doi: 10.1179/2295333715Y.0000000060[↩]
- Turner, P. J., Jerschow, E., Umasunthar, T., Lin, R., Campbell, D. E., & Boyle, R. J. (2017). Fatal Anaphylaxis: Mortality Rate and Risk Factors. The journal of allergy and clinical immunology. In practice, 5(5), 1169–1178. https://doi.org/10.1016/j.jaip.2017.06.031[↩]
- Williams SJ, Gupta S. Anaphylaxis to IVIG. Arch Immunol Ther Exp (Warsz). 2017 Feb;65(1):11-19. doi: 10.1007/s00005-016-0410-1[↩]
- Dona I, Salas M, Perkins JR, Barrionuevo E, Gaeta F, Cornejo-Garcia JA, Campo P, Torres MJ. Hypersensitivity Reactions to Non-Steroidal Anti-Inflammatory Drugs. Curr Pharm Des. 2016;22(45):6784-6802. doi: 10.2174/1381612822666160928142814[↩]
- Alvarez-de Lara MA, Martín-Malo A. Hypersensitivity reactions to synthetic haemodialysis membranes an emerging issue? Nefrologia. 2014 Nov 17;34(6):698-702. English, Spanish. doi: 10.3265/Nefrologia.pre2014.Jul.12682[↩][↩]
- Wang C, Wong S, Graham DJ. Risk of Anaphylaxis With Intravenous Iron Products. JAMA. 2016 May 24-31;315(20):2232-3. doi: 10.1001/jama.2016.0965[↩][↩]
- Lee, S. Y., Ahn, K., Kim, J., Jang, G. C., Min, T. K., Yang, H. J., Pyun, B. Y., Kwon, J. W., Sohn, M. H., Kim, K. W., Kim, K. E., Yu, J., Hong, S. J., Kwon, J. H., Kim, S. W., Song, T. W., Kim, W. K., Kim, H. Y., Jeon, Y. H., Lee, Y. J., … Korean Academy of Pediatric Allergy and Respiratory Diseases Food Allergy and Atopic Dermatitis Study Group (2016). A Multicenter Retrospective Case Study of Anaphylaxis Triggers by Age in Korean Children. Allergy, asthma & immunology research, 8(6), 535–540. https://doi.org/10.4168/aair.2016.8.6.535[↩]
- Schuch A, Brockow K. Mastocytosis and Anaphylaxis. Immunol Allergy Clin North Am. 2017 Feb;37(1):153-164. doi: 10.1016/j.iac.2016.08.017[↩]
- Waterfield T, Dyer E, Wilson K, Boyle RJ. How to interpret mast cell tests. Arch Dis Child Educ Pract Ed. 2016 Oct;101(5):246-51. doi: 10.1136/archdischild-2015-309887[↩]
- Vitte J. Human mast cell tryptase in biology and medicine. Mol Immunol. 2015 Jan;63(1):18-24. doi: 10.1016/j.molimm.2014.04.001[↩]
- Vadas P, Gold M, Perelman B, Liss GM, Lack G, Blyth T, Simons FE, Simons KJ, Cass D, Yeung J. Platelet-activating factor, PAF acetylhydrolase, and severe anaphylaxis. N Engl J Med. 2008 Jan 3;358(1):28-35. doi: 10.1056/NEJMoa070030[↩][↩]
- Burks, A. W., Jones, S. M., Boyce, J. A., Sicherer, S. H., Wood, R. A., Assa’ad, A., & Sampson, H. A. (2011). NIAID-sponsored 2010 guidelines for managing food allergy: applications in the pediatric population. Pediatrics, 128(5), 955–965. https://doi.org/10.1542/peds.2011-0539[↩]
- Järvinen KM. Food-induced anaphylaxis. Curr Opin Allergy Clin Immunol. 2011 Jun;11(3):255-61. doi: 10.1097/ACI.0b013e32834694d8[↩]
- Navaradnam, P., Suganthan, N., Kumanan, T., Sujanitha, V., & Mayorathan, U. (2021). Kounis Syndrome and Multiorgan Failure Following Multiple Wasp Stings. Cureus, 13(4), e14606. https://doi.org/10.7759/cureus.14606[↩]
- Kemp SF, Lockey RF, Simons FE. Epinephrine: the drug of choice for ananphylaxis. A statement of the World Allergy Organization. Allergy. 2008;63(8):1061–1070.[↩][↩]
- Oswalt ML, Kemp SF. Anaphylaxis: office management and prevention Immunol Allergy Clin North Am. 2007;27(2):177–191vi.[↩][↩]
- Baker TW, Stolfi A, Johnson TL. Use of epinephrine autoinjectors for treatment of anaphylaxis: which commercially available autoinjector do patients prefer? Ann Allergy Asthma Immunol. 2009;103(4):356–358.[↩]
- McLean-Tooke AP, Bethune CA, Fay AC, Spickett GP. Adrenaline in the treatment of anaphylaxis: what is the evidence? BMJ. 2003;327(7427):1332–1335.[↩]
- Sampson HA, Mendelson L, Rosen JP. Fatal and nearfatal anaphylactic reactions to food in children and adolescents. N Engl J Med. 1992;327(6):380–384.[↩]
- Kemp SF. The post-anaphylaxis dilemma: how long is long enough to observe a patient after resolution of symptoms? Curr Allergy Asthma Rep. 2008;8(1):45–48.[↩][↩]
- Lindor, R. A., McMahon, E. M., Wood, J. P., Sadosty, A. T., Boie, E. T., & Campbell, R. L. (2018). Anaphylaxis-related Malpractice Lawsuits. The western journal of emergency medicine, 19(4), 693–700. https://doi.org/10.5811/westjem.2018.4.37453[↩]