What is autosomal dominant
Autosomal dominant means one copy of the abnormal gene from only one parent or in each cell is sufficient to cause the disorder or disease. In some cases, an affected person inherits the autosomal dominant condition from an affected parent. In others, the autosomal dominant condition may result from a new mutation in the gene and occur in people with no history of the disorder in their family. This is called a de novo mutation. Huntington’s disease, Marfan syndrome and neurofibromatosis type 1 are common examples of an autosomal dominant genetic disorders.
Autosomal refers to the fact that whatever gene is involved is found on one of the first 22 chromosomes (called the autosomes) and not on the X or Y chromosome (the sex chromosomes).
Dominant refers to the above explanation that you have two copies of each gene, one from mom and one from dad, and in order to have an autosomal dominant condition, a person only has to have one copy of the abnormal gene. They can inherit this copy from mom or dad, who may also have the condition.
What does autosomal dominant mean?
Often autosomal dominant conditions can be seen in multiple generations within the family. If one looks back through their family history they notice their mother, grandfather, aunt/uncle, etc., all had the same condition. In cases where the autosomal dominant condition does run in the family, the chance for an affected person to have a child with the same condition is 50% regardless of whether it is a boy or a girl. These possible outcomes occur randomly. The chance remains the same in every pregnancy and is the same for boys and girls.
- When one parent has the abnormal gene, they will pass on either their normal gene or their abnormal gene to their child. Each of their children therefore has a 50% (1 in 2) chance of inheriting the changed gene and being affected by the condition.
- There is also a 50% (1 in 2) chance that a child will inherit the normal copy of the gene. If this happens the child will not be affected by the disorder and cannot pass it on to any of his or her children.
There are cases of autosomal dominant gene changes, or mutations, where no one in the family has it before and it appears to be a new thing in the family. This is called a de novo mutation. For the individual with the condition, the chance of their children inheriting it will be 50%. However, other family members are generally not likely to be at increased risk.
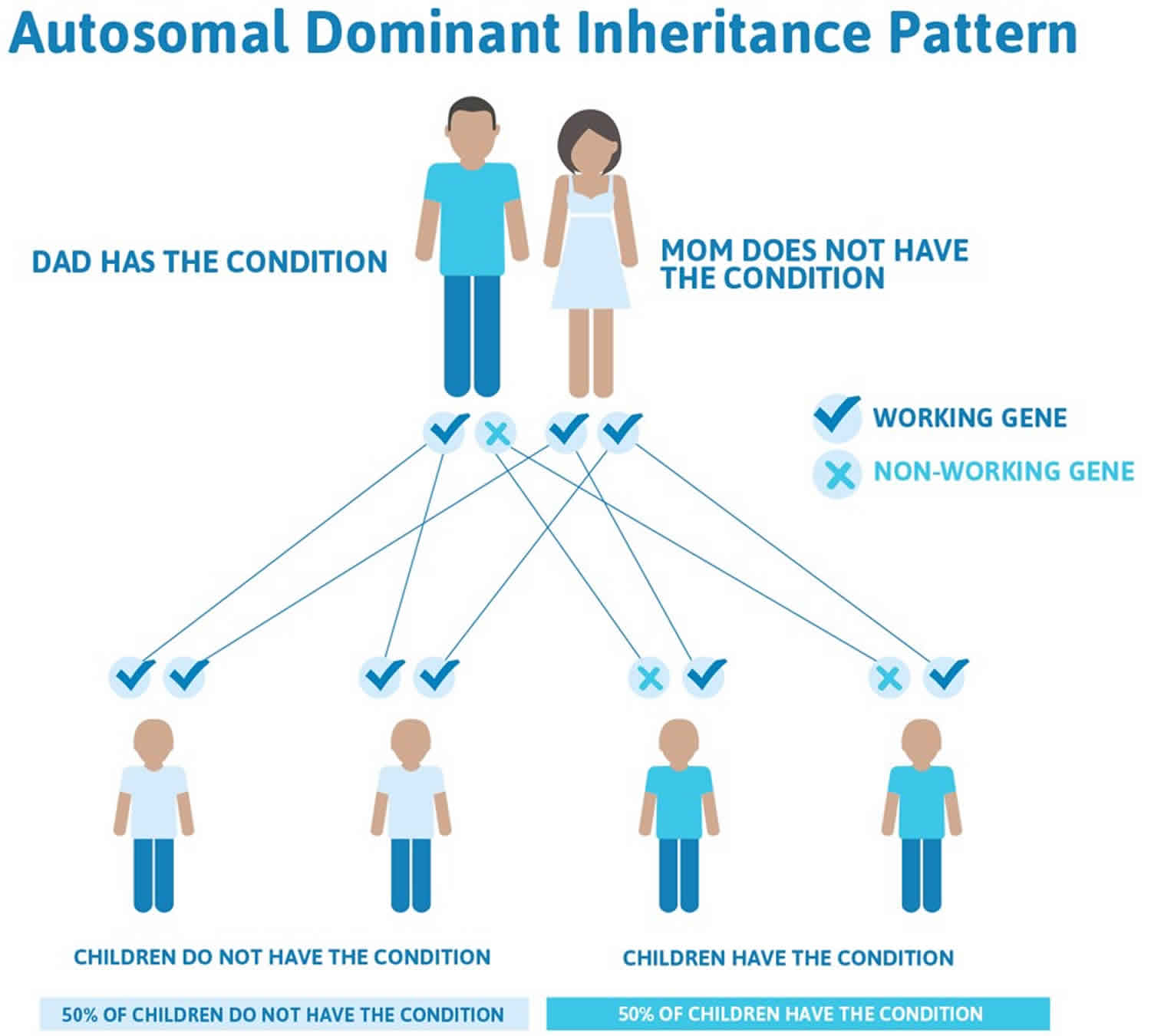
Figure 1 illustrates autosomal dominant inheritance. The example below shows what happens when dad has the condition, but the chances of having a child with the condition would be the same if mom had the condition.
Key points to remember
- A person only needs to inherit one copy of the abnormal gene in order to be affected by the condition (50% chance). These outcomes occur randomly. They remain the same in every pregnancy and are the same for boys and girls.
- A abnormal gene cannot be corrected if it is present for life.
- A abnormal gene is not something that can be caught from other people. They can still be a blood donor, for example.
- People often feel guilty about a genetic condition which runs in the family. It is important to remember that it is no-one’s fault and no-one has done anything to cause it to happen.
Figure 1. Autosomal dominant inheritance
Why does a genetic condition sometimes appear to miss out a generation?
Some dominant genetic conditions can affect family members very differently. This is called variable expression. The condition does not actually miss out a generation, but some people have such mild symptoms of the condition that they appear to be unaffected. They may not even know that they have the condition.
In conditions which occur later in life (adult onset conditions e.g. inherited breast cancer and Huntington’s disease), people may have died earlier of unrelated causes leaving no time for the condition to appear, or the correct diagnosis may never have been given. However, the parents may have passed on the condition to their children.
What if a child is the first person in the family to have the condition?
Sometimes a child born with a dominant genetic condition can be the first person to be affected in the family. This may happen because a new gene change has occurred, for the first time, in either the egg or the sperm that went to make that child. When this happens, the parent of that child is not affected. The parents are very unlikely to have another child affected by the same condition, but you should always discuss the risks with your doctor. However, an affected child, who now has the changed gene, can pass it on to his or her children.
Autosomal dominant disorders
Autosomal dominant disorders list
- 18q deletion syndrome (chromosome 18q-syndrome, monosomy 18q syndrome or chromosome 18 long arm deletion syndrome)
- Achondroplasia
- Achondrogenesis type 2
- Acroosteolysis Dominant Type
- Alexander disease (dysmyelinogenic leukodystrophy, demyelinogenic leukodystrophy)
- Severe Achondroplasia-Developmental Delay-Acanthosis Nigricans Syndrome
- ADNP-Related Multiple Congenital Anomalies – Intellectual Disability – Autism Spectrum Disorder
- Acro–dermato–ungual–lacrimal–tooth syndrome (ADULT Syndrome)
- AHDC1-Related Intellectual Disability – Obstructive Sleep Apnea – Mild Dysmorphism Syndrome
- Alternating hemiplegia of childhood (alternating hemiplegia syndrome)
- Amelogenesis Imperfecta Type 1B
- Andersen-Tawil syndrome (Andersen syndrome, long QT syndrome 7 or LQTS7)
- Aniridia
- Antithrombin III deficiency (hereditary antithrombin deficiency)
- Autism Spectrum Disorder Due To AUTS2 Deficiency
- Bannayan-Riley-Ruvalcaba Syndrome
- Beare-Stevenson Cutis Gyrata Syndrome
- Bethlem myopathy
- Birk-Barel Syndrome
- Birt-Hogg-Dube Syndrome
- Blepharo-Cheilo-Odontic Syndrome
- Blepharophimosis, Ptosis, And Epicanthus Inversus Syndrome
- Bohring Opitz syndrome (Opitz trigonocephaly-like syndrome, C-like syndrome or Oberklaid-Danks syndrome)
- Branchio-Oto-Renal Syndrome
- Branchiooculofacial Syndrome
- Brooke-Spiegler Syndrome
- Carney complex or Carney syndrome
- Charcot-Marie-Tooth Disease
- Cherubism
- CLCN7-related osteopetrosis
- Congenital Polycystic Liver Disease
- Congenital Radioulnar Synostosis
- Congenital Stationary Night Blindness Autosomal Dominant 3
- Costello Syndrome
- Cowden Syndrome (Cowden disease)
- Craniometaphyseal Dysplasia
- Crouzon Syndrome-Acanthosis Nigricans Syndrome
- Cyclic neutropenia
- Darier’s disease
- Denys Drash syndrome
- Diamond Blackfan anemia
- DiGeorge syndrome (Velocardiofacial syndrome)
- Dravet syndrome (SCN1A mutation)
- Duane-Radial Ray Syndrome
- DYRK1A-Related Intellectual Disability Syndrome
- Dyskeratosis Congenita, Autosomal Dominant 2
- Dyskeratosis Congenita, Autosomal Dominant 3
- Dyskeratosis Congenita, Autosomal Dominant 6
- Dysplastic Nevus Syndrome
- Early-Onset Autosomal Dominant Alzheimer Disease
- EEC Syndrome
- Ehlers-Danlos Syndrome, Classic Type
- Familial amyloid polyneuropathy (FAP) (familial transthyretin amyloidosis, transthyretin familial amyloid polyneuropathy or hereditary transthyretin amyloidosis)
- Familial amyloidosis or hereditary amyloidosis
- Familial Exudative Vitreoretinopathy
- Familial Hypercholesterolemia
- Familial porencephaly (porencephaly type 1, autosomal dominant porencephaly type 1 or infantile hemiplegia with porencephaly)
- Feingold Syndrome
- Frasier Syndrome
- Generalized Basal Epidermolysis Bullosa Simplex With Skin Atrophy, Scarring And Hair Loss
- Generalized Juvenile Polyposis/Juvenile Polyposis Coli
- Glass-Chapman-Hockley Syndrome
- Gorlin syndrome (basal cell nevus syndrome)
- Hailey Hailey disease (benign familial pemphigus)
- Hand-Foot-Genital Syndrome
- Heart-Hand Syndrome, Slovenian Type
- Hereditary Breast Ovarian Cancer Syndrome
- Hereditary coproporphyria
- Hereditary Hemorrhagic Telangiectasia
- Holt-Oram syndrome
- Hyper IgE Syndrome or Job syndrome
- Hypophosphatasia
- IMAGe syndrome
- Infantile cortical hyperostosis or Caffey disease
- Intellectual Disability, Autosomal Dominant 12
- Intellectual Disability, Autosomal Dominant 14
- Intellectual Disability, Autosomal Dominant 15
- Intellectual Disability, Autosomal Dominant 16
- Intellectual Disability, Autosomal Dominant 27
- Intellectual Disability, Autosomal Dominant 29
- Intellectual Disability, Autosomal Dominant 30
- Intellectual Disability, Autosomal Dominant 48
- Intellectual Disability-Craniofacial Dysmorphism-Cryptorchidism Syndrome
- Intellectual Disability-Facial Dysmorphism Syndrome Due To SETD5 Haploinsufficiency
- Intellectual Disability-Feeding Difficulties-Developmental Delay-Microcephaly Syndrome
- Intellectual Disability-Macrocephaly-Hypotonia-Behavioral Abnormalities Syndrome
- Intellectual Disability-Microcephaly-Strabismus-Behavioral Abnormalities Syndrome
- Juvenile polyposis syndrome or juvenile intestinal polyposis
- Severe Intellectual Disability-Poor Language-Strabismus-Grimacing Face-Long Fingers Syndrome
- Severe Intellectual Disability-Progressive Spastic Diplegia Syndrome
- Lacrimo-auriculo-dento-digital syndrome (LADD syndrome)
- Laron syndrome (rare autosomal dominat form)
- Larsen Syndrome
- Legius syndrome (neurofibromatosis type 1-like syndrome)
- LEOPARD syndrome (Noonan syndrome with multiple lentigines)
- Leukodystrophy with Autonomic Disease
- Liddle syndrome (pseudoaldosteronism)
- Li-Fraumeni Syndrome
- Loeys-Dietz syndrome
- Lymphedema-distichiasis syndrome
- Lynch Syndrome
- Machado Joseph disease (spinocerebellar ataxia type 3, Azorean disease or Azorean ataxia)
- Macrocephaly-Autism Syndrome
- Mandibulofacial Dysostosis-Microcephaly Syndrome
- Marfan Syndrome
- Marshall syndrome
- May-Hegglin anomaly
- Medullary cystic kidney disease (Autosomal Dominant Tubulointerstitial Kidney Disease)
- Mendelian Susceptibility To Mycobacterial Diseases Due To Partial IRF8 Deficiency
- Mendelian Susceptibility To Mycobacterial Diseases Due To Partial STAT1 Deficiency
- Microcephaly-Corpus Callosum Hypoplasia-Intellectual Disability-Facial Dysmorphism Syndrome
- Micrognathia-Recurrent Infections-Behavioral Abnormalities-Mild Intellectual Disability Syndrome
- Monilethrix
- Muckle-Wells Syndrome
- Muenke syndrome (Muenke nonsyndromic coronal craniosynostosis or syndrome of coronal craniosynostosis)
- Muir-Torre syndrome
- Multiple Epiphyseal Dysplasia
- Multiple Cutaneous And Mucosal Venous Malformations
- Multiple Endocrine Neoplasia Type 1
- Multiple Endocrine Neoplasia Type 2B
- Multiple Endocrine Neoplasia Type 4
- Myotonic Dystrophy (myotonic dystrophy type 1 and type 2)
- Nail-Patella Syndrome
- Neurofibromatosis
- Nevoid Basal Cell Carcinoma Syndrome
- Nocturnal Frontal Lobe Epilepsy
- Noonan syndrome
- Osler Weber Rendu syndrome (Osler Weber Rendu disease or hereditary hemorrhagic telangiectasia)
- Osteogenesis Imperfecta
- Pachyonychia congenita
- Palmoplantar keratodermas
- Paramyotonia congenita (Eulenburg disease, Von Eulenberg’s disease or paralysis periodica paramyotonia)
- Partial Epilepsy with Auditory Features
- PCWH Syndrome (Peripheral demyelinating neuropathy-central dysmyelinating leukodystrophy-Waardenburg syndrome-Hirschsprung disease)
- Pelger-Huet anomaly
- Peutz Jeghers syndrome
- Photic sneeze reflex (Autosomal Dominant Compelling Helio Ophthalmic Outburst [ACHOO] syndrome, sneezing from light exposure or photic sneezing)
- Piebaldism
- Pilarowski-Bjornsson Syndrome
- Pitt-Hopkins syndrome
- Polycystic Kidney Disease
- Porphyria
- Postaxial Polydactyly-Anterior Pituitary Anomalies-Facial Dysmorphism Syndrome
- Proximal Symphalangism Disease
- Pseudoachondroplasia (PSACH), pseudoachondroplastic dysplasia, pseudoachondroplastic spondyloepiphyseal dysplasia syndrome
- PTEN hamartoma tumor syndrome
- PURA-Related Severe Neonatal Hypotonia-Seizures-Encephalopathy Syndrome Due To A Point Mutation
- Rapp-Hodgkin Syndrome
- Renal Coloboma Syndrome
- Retinitis Pigmentosa
- Retinoschisis (autosomal dominant)
- Robinow Syndrome
- Rubinstein-Taybi Syndrome (broad thumb-hallux syndrome)
- Sodium Channelopathy-Related Small Fiber Neuropathy
- Spondyloepiphyseal Dysplasia Tarda, Autosomal Dominant
- Stickler syndrome
- Stiff skin syndrome
- Tarsal-Carpal Coalition Syndrome
- Tatton-Brown Rahman syndrome (DNMT3A overgrowth syndrome, Rahman syndrome or TBRS)
- Thanatophoric dysplasia (thanatophoric dwarfism or thanatophoric short stature)
- Thin Basement Membrane Nephropathy
- Thomsen disease (autosomal dominant myotonia congenita)
- Thrombophilia Due To Protein S Deficiency (autosomal dominant)
- Timothy Syndrome
- Townes-Brocks Syndrome
- Treacher-Collins Syndrome
- Trichorhinophalangeal Syndrome Type I
- Trichorhinophalangeal Syndrome Type II
- TRPV4-associated disorders
- Tubulointerstitial Kidney Disease, MUC1-Related
- Tubulointerstitial Kidney Disease, REN-Related
- Tubulointerstitial Kidney Disease, UMOD-Related
- Tuberous Sclerosis
- Transthyretin amyloidosis
- Van der Woude syndrome
- Von Hippel-Lindau syndrome
- Waardenburg Syndrome
- White sponge nevus (oral white sponge naevus, congenital leukokeratosis, familial white folded mucosal dysplasia, leukoderma exfoliativum mucosae oris, hereditary leukokeratosis, white folded gingivostomatitis, oral epithelial nevus, nevus of Cannon or white sponge nevus of Cannon)
- Xia Gibbs syndrome
- Autosomal Dominant Aarskog Syndrome
- Autosomal Dominant Alport Syndrome
- Autosomal Dominant Ehlers-Danlos Syndrome, Vascular Type
- Autosomal Dominant Emery-Dreifuss Muscular Dystrophy
- Autosomal Dominant Kenny-Caffey Syndrome
- Autosomal Dominant Opitz G/BBB Syndrome
- Autosomal Dominant Robinow Syndrome
- Autosomal Dominant Brachyolmia
- Autosomal Dominant Centronuclear Myopathy
- Autosomal Dominant Cerebellar Ataxia
- Autosomal Dominant Chondrodysplasia Punctata
- Autosomal Dominant Coarctation Of Aorta
- Autosomal Dominant Complex Spastic Paraplegia
- Autosomal Dominant Cutis Laxa
- Autosomal Dominant Deafness – Onychodystrophy Syndrome
- Autosomal Dominant Disease Associated With Focal Palmoplantar Keratoderma As A Major Feature
- Autosomal Dominant Disease Associated With Punctate Palmoplantar Keratoderma As A Major Feature
- Autosomal Dominant Disease With Diffuse Palmoplantar Keratoderma As A Major Feature
- Autosomal Dominant Distal Hereditary Motor Neuropathy
- Autosomal Dominant Distal Myopathy
- Autosomal Dominant Distal Renal Tubular Acidosis
- Autosomal Dominant Epidermolytic Ichthyosis
- Autosomal Dominant Hereditary Sensory And Autonomic Neuropathy
- Autosomal Dominant Hypocalcemia
- Autosomal Dominant Hypohidrotic Ectodermal Dysplasia
- Autosomal Dominant Hypophosphatemic Rickets
- Autosomal Dominant Ichthyosis Vulgaris
- Autosomal Dominant Intellectual Disability-Craniofacial Anomalies-Cardiac Defects Syndrome
- Autosomal Dominant Intermediate Charcot-Marie-Tooth Disease
- Autosomal Dominant Isolated Diffuse Palmoplantar Keratoderma
- Autosomal Dominant Keratitis
- Autosomal Dominant Limb-Girdle Muscular Dystrophy
- Autosomal Dominant Mendelian Susceptibility To Mycobacterial Diseases Due To Partial IFNgammaR1 Deficiency
- Autosomal Dominant Mendelian Susceptibility To Mycobacterial Diseases Due To Partial IFNgammaR2 Deficiency
- Autosomal Dominant Multiple Pterygium Syndrome
- Autosomal Dominant Myoglobinuria
- Autosomal dominant Myotonia Congenita (Thomsen disease)
- Autosomal Dominant Nager syndrome
- Autosomal Dominant Non-Syndromic Intellectual Disability
- Autosomal Dominant Nonsyndromic Deafness
- Autosomal Dominant Oculocutaneous Albinism
- Autosomal Dominant Omodysplasia
- Autosomal Dominant Optic Atrophy
- Autosomal Dominant Osteopetrosis
- Autosomal Dominant Polycystic Kidney Disease
- Autosomal Dominant Popliteal Pterygium Syndrome
- Autosomal Dominant Primary Microcephaly
- Autosomal Dominant Progressive External Ophthalmoplegia
- Autosomal Dominant Proximal Renal Tubular Acidosis
- Autosomal Dominant Proximal Spinal Muscular Atrophy
- Autosomal Dominant Pure Spastic Paraplegia
- Autosomal Dominant Rhegmatogenous Retinal Detachment
- Autosomal Dominant Secondary Polycythemia
- Autosomal Dominant Severe Congenital Neutropenia
- Autosomal Dominant Sideroblastic Anemia
- Autosomal Dominant Spondylocostal Dysostosis
- Autosomal Dominant Vibratory Urticaria
Autosomal recessive vs Autosomal dominant
Autosomal recessive means two copies of the abnormal gene, one from each parent (one abnormal gene from mum and one abnormal gene from dad), is needed to cause the disorder or disease. The parents of an individual with an autosomal recessive condition each carry one copy of the mutated gene, but they typically do not show signs and symptoms of the condition. Autosomal recessive disorders are typically not seen in every generation of an affected family. Cystic fibrosis and sickle cell anemia are common examples of an autosomal recessive genetic disorders.