Balance and gait problems
A balance problem is a condition that makes you feel unsteady or dizzy. If you are standing, sitting, or lying down, you might feel as if you are moving, spinning, or floating. If you are walking, you might suddenly feel as if you are tipping over.
Having good balance is important for many everyday activities, such as going up and down the stairs. It also helps you walk safely and avoid tripping and falling over objects in your way.
Everyone has a dizzy spell now and then, but the term “dizziness” can mean different things to different people. For one person, dizziness might mean a fleeting feeling of faintness, while for another it could be an intense sensation of spinning (vertigo) that lasts a long time.
Experts believe that more than four out of 10 Americans, sometime in their lives, will experience an episode of dizziness significant enough to send them to a doctor. Balance disorders can be caused by certain health conditions — your muscles, bones, joints, vision, the balance organ in the inner ear, nerves, heart and blood vessels, medications, or a problem in the brain. However, most balance problems result from issues in your balance end-organ in the inner ear (vestibular system). A balance disorder can profoundly impact your daily activities and cause psychological and emotional hardship.
Vertigo, a type of dizziness, is an unpleasant disturbance of spatial orientation or to the erroneous perception of movement 1. Vertigo involves a perceived movement either of one’s own body, such as swaying or rotation, or of the environment, or both. Alongside headache, dizziness and vertigo are among the more common symptoms with which patients present to physicians in general, not just to neurologists. Their lifetime prevalence is approximately 20% to 30% 2. Dizziness, a common symptom that affects more than 90 million Americans, has been reported to be the most common complaint in patients 75 years of age or older 3.
To help you decide whether to seek medical help for a dizzy spell, ask yourself the following questions. If you answer “yes” to any of these questions, talk to your doctor:
- Do you feel unsteady?
- Do you feel as if the room is spinning around me?
- Do you feel as if you’re moving when you know you’re sitting or standing still?
- Do you lose your balance and fall?
- Do you feel as if you’re falling?
- Do you feel lightheaded or as if you might faint?
- Do you have blurred vision?
- Do you ever feel disoriented–losing your sense of time or location?
It is important to see your doctor about balance problems. They can be a sign of other health problems, such as an ear infection or a stroke.
By strengthening your body and doing regular balance exercises, you may help reduce your chances of a fall-related head injury or traumatic brain injury, which can cause memory issues and impaired thinking. Work to improve your balance and talk to your doctor if you’ve experienced a fall.
Some balance problems are due to problems in the inner ear. Others may involve another part of the body, such as the brain or the heart. Aging, infections, head injury, certain medicines, or problems with blood circulation may also cause balance problems.
Your doctor may send you to a specialist for a diagnosis. You may need a hearing test, blood tests, or imaging studies of your head and brain. Other possible tests look at your eye movements, and how your body responds to movement.
In some cases, treating the illness that is causing the disorder will help with the balance problem. Exercises, a change in diet, and some medicines also can help.
How does my body keep its balance?
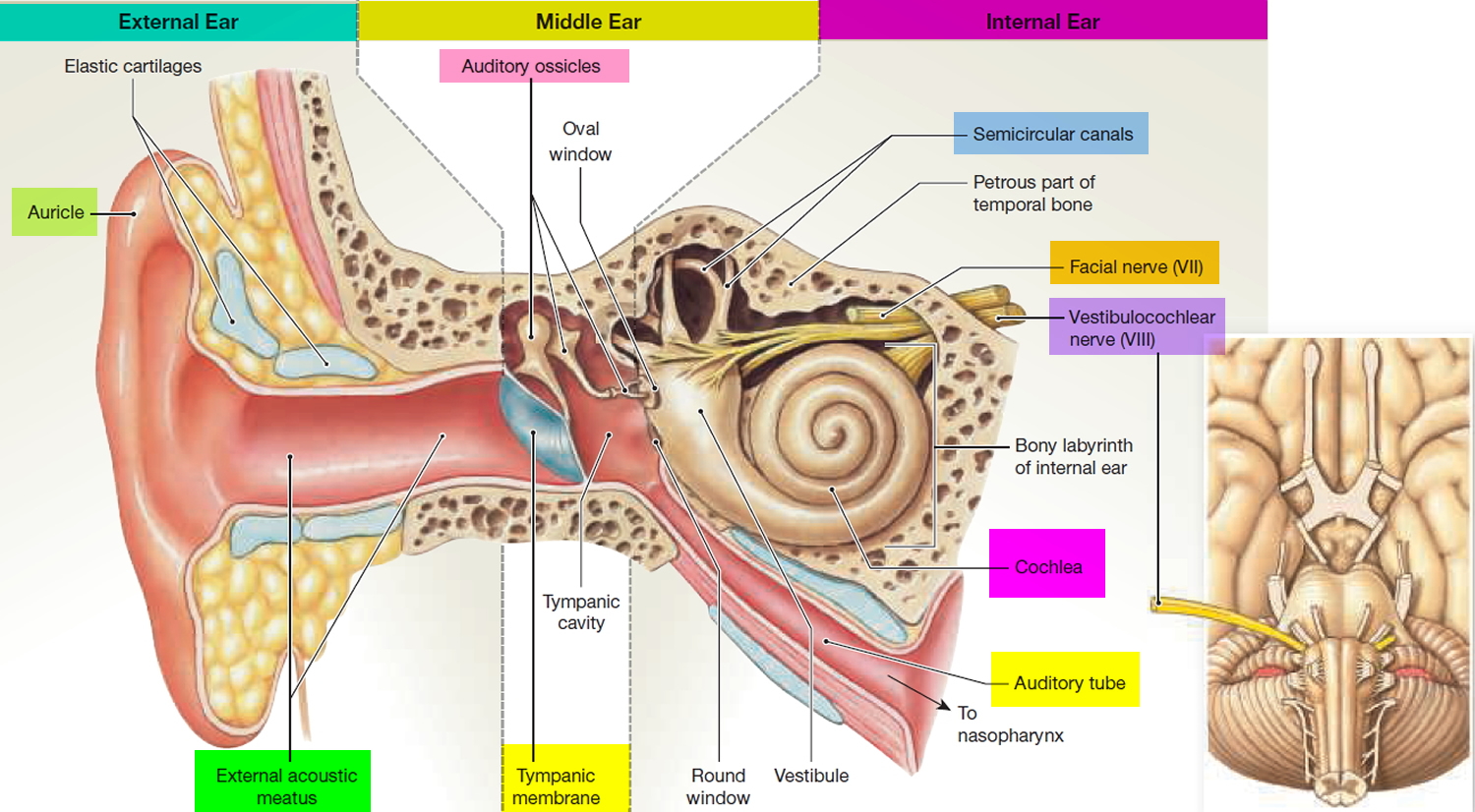
Your sense of balance relies on a series of signals to the brain from several organs and structures in the body, which together are known as the vestibular system. The vestibular system begins with a maze-like structure in your inner ear called the labyrinth, which is made of bone and soft tissue.
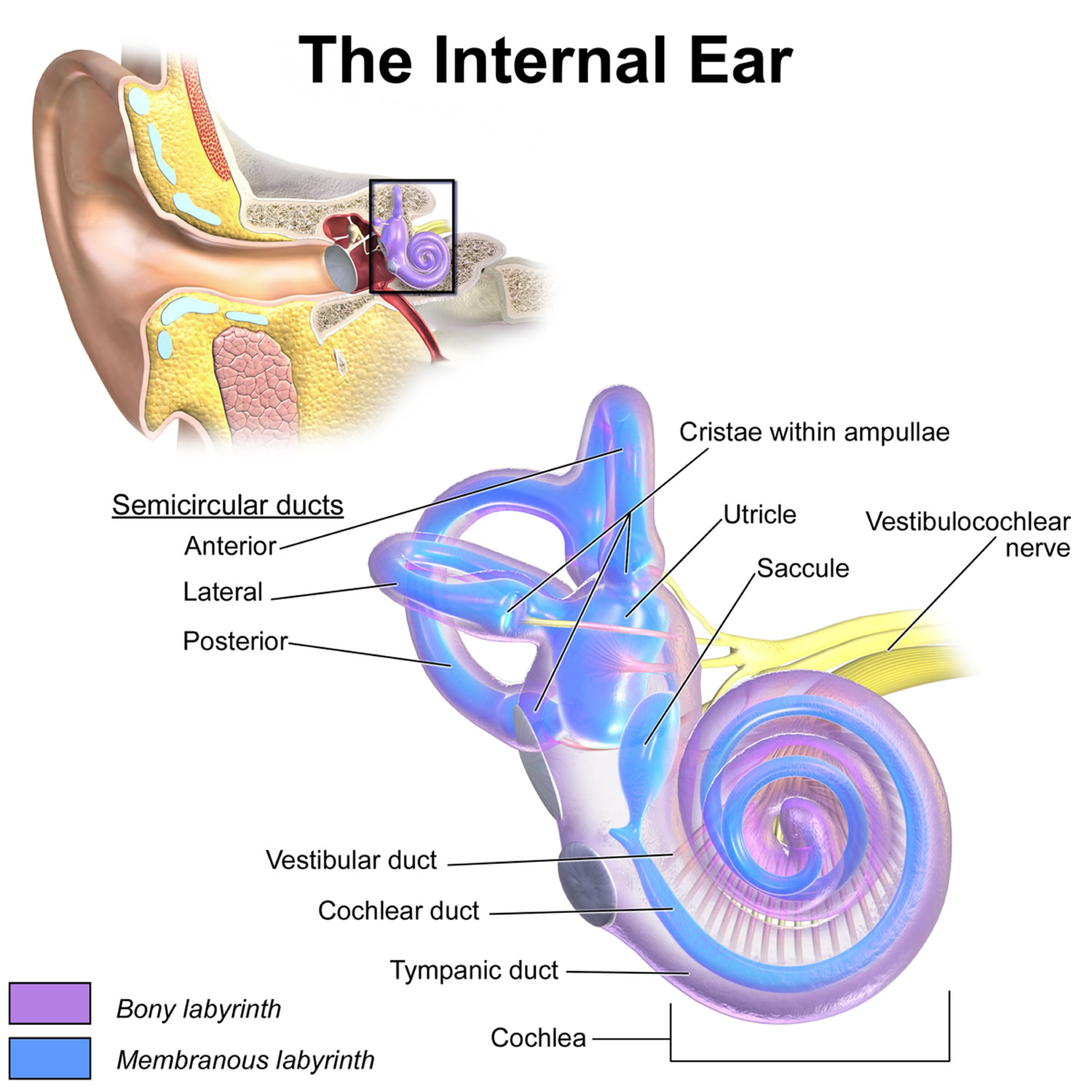
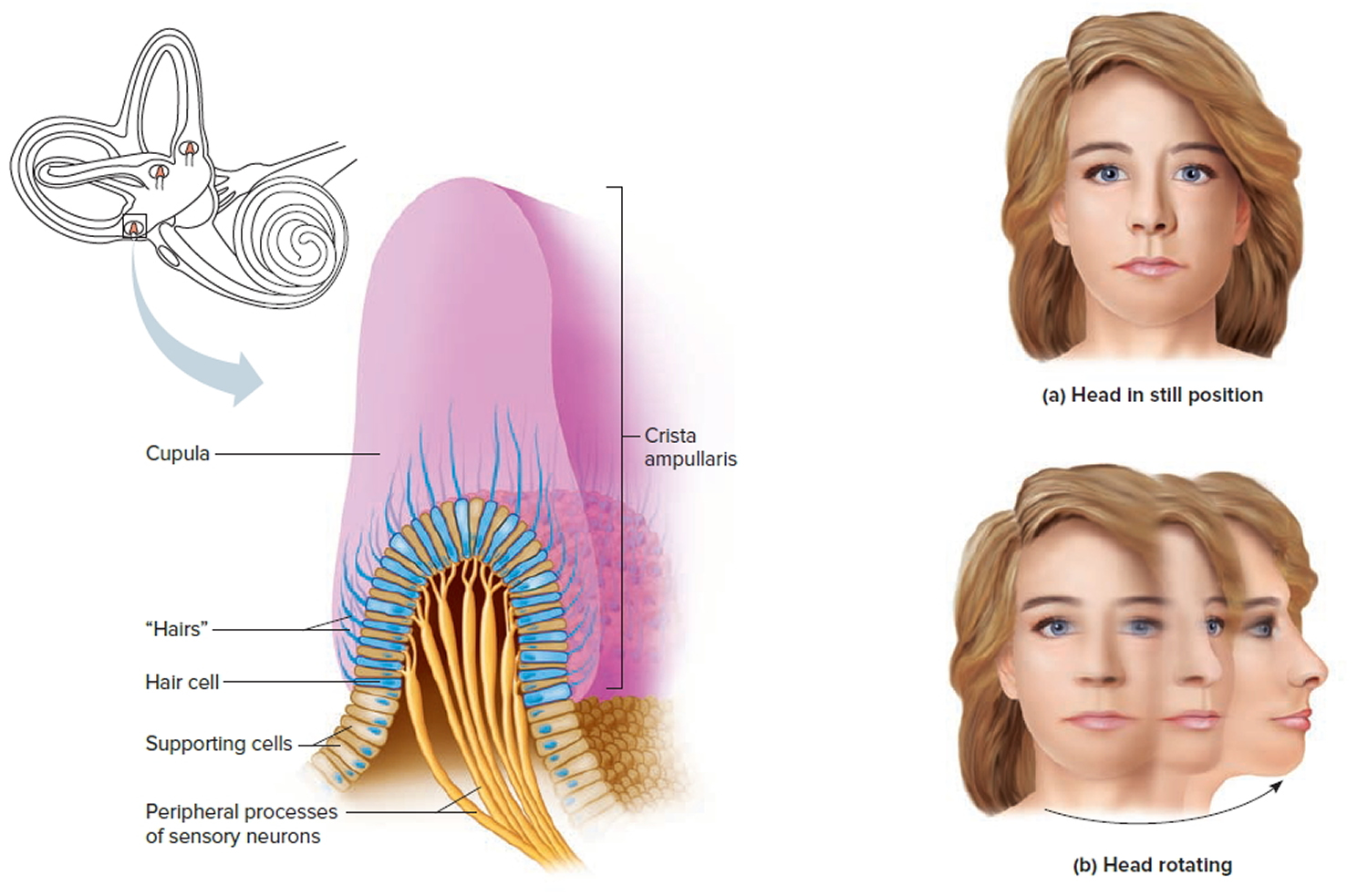
Within the labyrinth are structures known as semicircular canals. The semicircular canals contain three fluid-filled ducts, which form loops arranged roughly at right angles to one another. They tell your brain when your head rotates or moves up or down. Inside each canal is a gel-like structure called the cupula, stretched like a thick drumhead across its duct (see Figure 5 Dynamic inner ear organs). The cupula sits on a cluster of sensory hair cells. Each hair cell has tiny, thin extensions called stereocilia that protrude into the cupula.
When you turn your head, fluid inside the semicircular canal moves, causing the cupula to flex, which bends the stereocilia. This bending creates a nerve signal to the brain to tell it which way your head has turned.
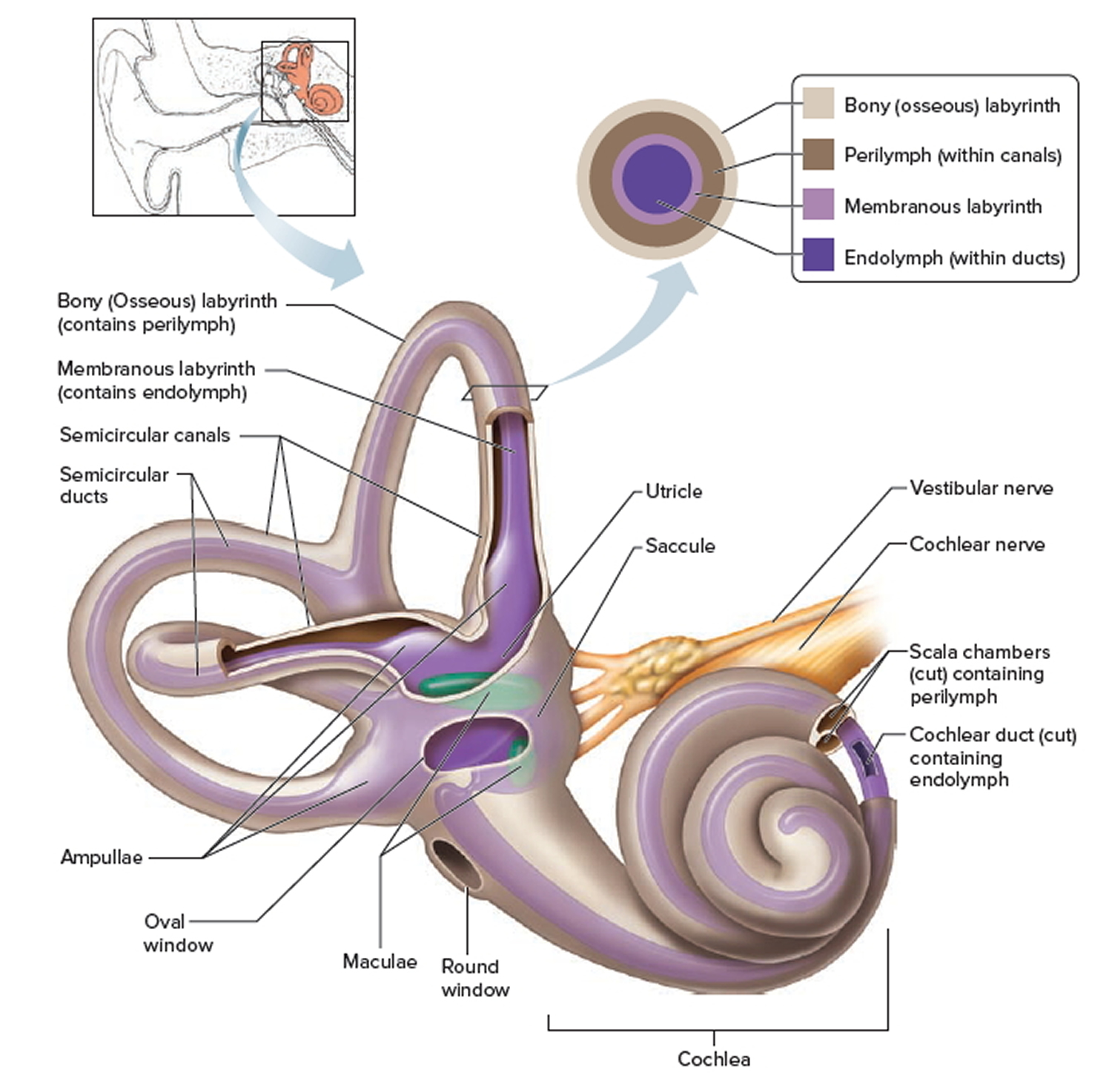
Between the semicircular canals and the cochlea lie two otolithic organs: fluid-filled pouches called the utricle and the saccule (see Figures 2, 3 and 4). These organs tell your brain the position of your head with respect to gravity, such as whether you are sitting up, leaning back, or lying down, as well as when your head is moving in a straight line, such as up, forward, or sideways.
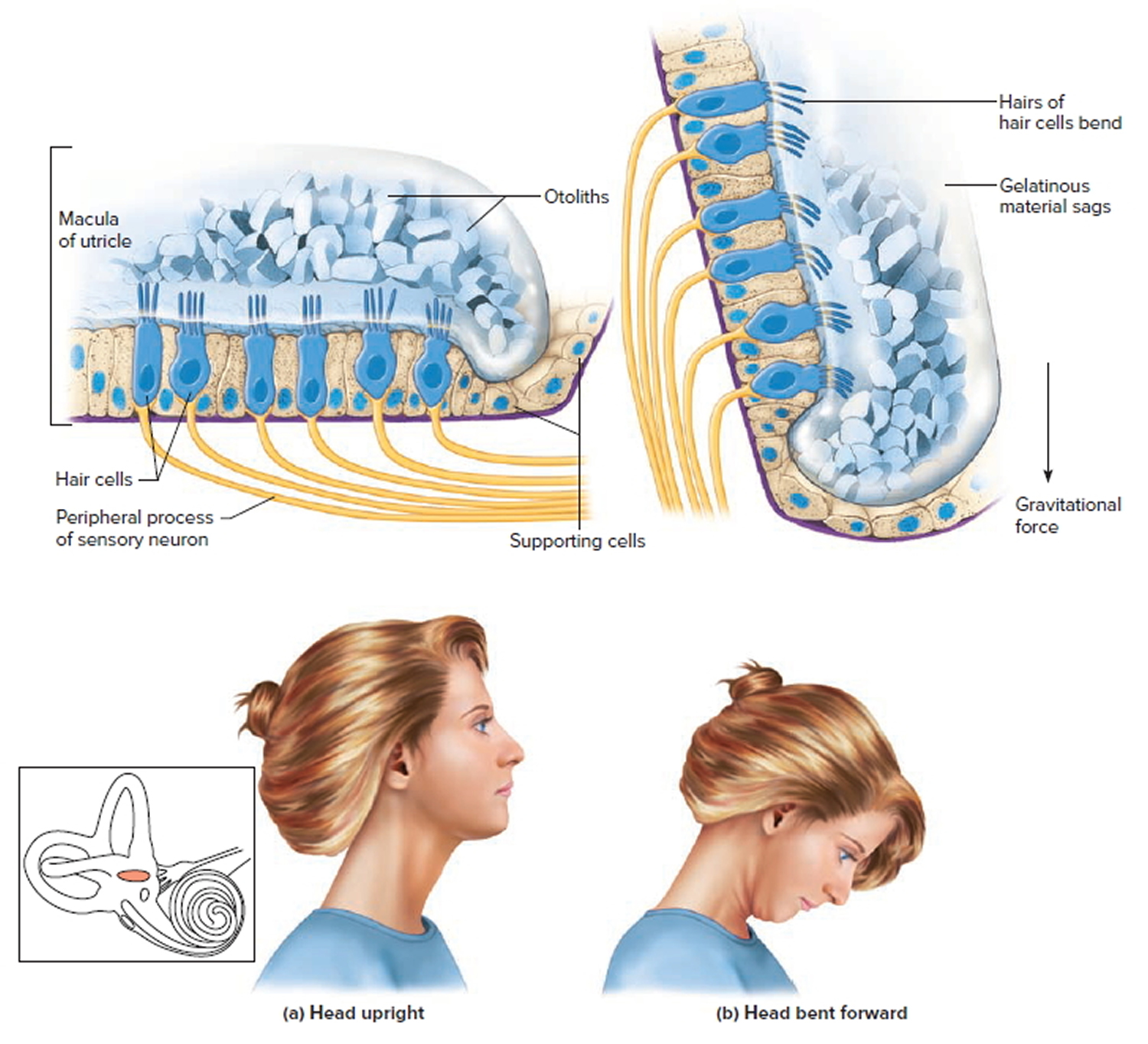
The utricle and the saccule also have sensory hair cells lining the floor or wall of each organ, with stereocilia extending into an overlying gel-like layer. Here, the gel contains tiny, dense grains of calcium carbonate called otoconia. Whatever the position of your head, gravity pulls on these grains, which then move the stereocilia to signal your head’s position to your brain. Any head movement creates a signal that tells your brain about the change in position.
When you move, the vestibular system detects mechanical forces, including gravity, that stimulate the semicircular canals and the otolithic organs. These organs work with other sensory systems in your body, such as your vision and your musculoskeletal sensory system, to control the position of your body at rest or in motion. This helps you maintain stable posture and keep your balance when you’re walking or running. It also helps you keep a stable visual focus on objects when your body changes position.
When the signals from any of these sensory systems malfunction, you can have problems with your sense of balance. If you have additional problems with motor control, such as weakness, slowness, tremor, or rigidity, you can lose your ability to recover properly from imbalance. This raises the risk of falling and injury.
Figure 1. Inner ear anatomy
Figure 2. Parts of the inner ear
Figure 3. Inner ear bones
Note: A closer look at the inner ear. Perilymph separates the bony (osseous) labyrinth of the inner ear from the membranous labyrinth, which contains endolymph. Note that areas of bony labyrinth have been removed to reveal underlying structures.
Sense of Equilibrium
The sense of equilibrium (balance) is really two senses:
- Static equilibrium and
- Dynamic equilibrium—that come from different sensory organs.
The organs of static equilibrium sense the position of the head, maintaining balance, stability and posture when the head and body are still. When the head and body suddenly move or rotate, the organs of dynamic equilibrium detect such motion and aid in maintaining balance.
Static Equilibrium
The organs of static equilibrium are in the vestibule, a bony chamber between the semicircular canals and the cochlea. The membranous labyrinth inside the vestibule consists of two expanded chambers—a utricle and a saccule (see Figures 2 and 3).
The saccule and utricle each have a tiny structure called a macula. Maculae have many hair cells, which serve as sensory receptors. The hairs of the hair cells project into a mass of gelatinous material, which has grains of calcium carbonate (otoliths) embedded in it. These particles add weight to the gelatinous structure.
Bending the head forward, backward, or to either side tilts the gelatinous masses of the maculae, and as they sag in response to gravity, the hairs projecting into them bend. This action causes the hair cells to signal the sensory neurons associated with them in a manner similar to that of hair cells associated with hearing. The resulting action potentials are conducted into the central nervous system on the vestibular branch of the vestibulocochlear nerve, informing the brain of the head’s new position. The brain responds by adjusting the pattern of motor impulses to skeletal muscles, which contract or relax to maintain balance (Figure 4).
Figure 4. Inner ear maculae respond to changes in head position
Note: (a) Macula of the utricle with the head in an upright position. (b) Macula of the utricle with the head bent forward.
Dynamic Equilibrium
The organs of dynamic equilibrium are the three semicircular canals in the labyrinth. They detect motion of the head and aid in balancing the head and body during sudden movement. These canals lie at right angles to each other (see Figure 2).
Suspended in the perilymph of the bony portion of each semicircular canal is a membranous semicircular duct that ends in a swelling called an ampulla, which
houses the sensory organs of the semicircular canals. Each of these sensory organs, called a crista ampullaris, contains a number of sensory hair cells and supporting cells. Like the hairs of the maculae, the hair cells of the crista ampullaris extend upward into a dome-shaped, gelatinous mass called the cupula (Figure 5). When the head is stationary, the cupula of the crista ampullaris remains upright. When the head is moving rapidly, the cupula bends opposite the motion of the head, stimulating sensory receptors.
Rapid movement of the head or body stimulates the hair cells of the crista ampullaris (Figure 5). At such times, the semicircular canals move with the head or body, but the fluid inside the membranous ducts remains stationary. Imagine turning rapidly while holding a full glass of water. This action bends the cupula in one or more of the canals in a direction opposite that of the head or body movement, and the hairs embedded in it also bend. The stimulated hair cells signal their associated neurons, which conduct impulses to the brain. The brain interprets these impulses as a movement in a particular direction.
Parts of the cerebellum are particularly important in interpreting impulses from the semicircular canals. Analysis of such information allows the brain to predict the consequences of rapid body movements. By modifying signals to appropriate skeletal muscles, the cerebellum can maintain balance.
Other sensory structures aid in maintaining equilibrium. For example, certain mechanoreceptors (proprioceptors), particularly those associated with the joints of the neck, inform the brain about the position of body parts. In addition, the eyes detect changes in position that result from body movements. Such visual information is so important that even if the organs of equilibrium are damaged, a person may be able to maintain normal balance by keeping the eyes open and moving slowly.
The nausea, vomiting, dizziness, and headache of motion sickness arise from sensations that don’t make sense. The eyes of a person reading in a moving car, for example, signal the brain that the person is stationary, because the print doesn’t move. However, receptors in the skin detect bouncing, swaying, starting, and stopping as the inner ear detects movement. The contradiction triggers the symptoms. Similarly, in a passenger of an airplane flying through heavy turbulence, receptors in the skin and inner ear register the chaos outside, but the eyes focus on the immobile seats and surroundings.
To prevent or lessen the misery of motion sickness, focus on the horizon or an object in the distance ahead. Medications are available by pill (diphenhydramine and dimenhydrinate) and, for longer excursions, in a skin patch (scopolamine).
Figure 5. Dynamic inner ear balance organs (crista ampullaris) within the Semicricular ducts
What are some types of balance problems?
There are more than a dozen different balance disorders. Some of the most common are:
- Benign paroxysmal positional vertigo (BPPV) or positional vertigo: A brief, intense episode of vertigo triggered by a specific change in the position of the head. You might feel as if you’re spinning when you bend down to look under something, tilt your head to look up or over your shoulder, or roll over in bed. Benign paroxysmal positional vertigo occurs when loose otoconia tumble into one of the semicircular canals and weigh on the cupula. The cupula doesn’t flex properly and sends wrong information about your head’s position, causing vertigo. Benign paroxysmal positional vertigo can result from a head injury, or can develop just from getting older.
- Labyrinthitis: An infection or inflammation of the inner ear that causes dizziness and loss of balance. It is often associated with an upper respiratory infection such as the flu.
- Ménière’s disease: Episodes of vertigo, hearing loss, tinnitus (a ringing or buzzing in the ear), and a feeling of fullness in the ear. It may be associated with a change in fluid volume within parts of the labyrinth, but the cause or causes are still unknown.
- Vestibular neuronitis: An inflammation of the vestibular nerve that can be caused by a virus, and primarily causes vertigo.
- Perilymph fistula: A leakage of inner ear fluid into the middle ear. It causes unsteadiness that usually increases with activity, along with dizziness and nausea. Perilymph fistula can occur after a head injury, dramatic changes in air pressure (such as when scuba diving), physical exertion, ear surgery, or chronic ear infections. Some people are born with perilymph fistula.
- Mal de Debarquement syndrome (MdDS): A feeling of continuously rocking or bobbing, typically after an ocean cruise or other sea travel. Usually the symptoms go away a few hours or days after you reach land. Severe cases, however, can last months or even years, and the cause remains unknown.
The important criteria for distinguishing among them are as follows 4:
- The type of dizziness/vertigo: rotatory vertigo resembles the sensation of being on a merry-go-round (in vestibular neuritis and other disorders), while postural vertigo resembles the sensation of riding in a boat (e.g., in bilateral vestibulopathy). Many patients use the term “dizziness” for lightheadedness without any sensation of movement (e.g., in drug intoxication).
- The duration of dizziness/vertigo: attacks may last for seconds or minutes (as in vestibular paroxysm) or hours (as in Menière’s disease or vestibular migraine). Persistent vertigo lasting days or weeks is seen in vestibular neuritis, among other conditions. Attacks of postural vertigo lasting minutes to hours can be produced, for example, by brainstem transient ischemic attacks.
- Precipitating and exacerbating factors of dizziness and vertigo: the symptoms arise at rest in some conditions (e.g., vestibular neuritis); they can also arise when the patient walks (as in bilateral vestibulopathy) or be induced by turning the head to the right or left (as in vestibular paroxysm). Other possible precipitating factors include turning in bed (as in benign paroxysmal positioning vertigo [BPPV]), coughing, pressing, and loud tones of a particular frequency (Tullio’s phenomenon, seen in perilymph fistula), as well as certain social or environmental conditions (e.g., phobic postural vertigo).
- The accompanying symptoms, if present, may arise from the inner ear – e.g., attacks of intense tinnitus, hearing impairment, and a pressure sensation in the ear, which are typical of Menière’s disease. Diplopia (double vision), sensory disturbances, dysphagia, dysarthria, and paralysis of arms and legs are symptoms of central origin that usually arise in the brainstem. Headache or a history of migraine may point to the diagnosis of vestibular migraine but can also be caused by brainstem ischemia or posterior fossa hemorrhage.
Balance problems in elderly
Each year, more than 2 million older Americans go to the emergency room because of fall-related injuries. A simple fall can cause a serious fracture of the arm, hand, ankle, or hip.
Gait and balance disorders are among the most common causes of falls in older adults 5 and often lead to injury, disability, loss of independence, and limited quality of life 6. Gait and balance problems are usually multifactorial in origin and require a comprehensive assessment to determine contributing factors and targeted interventions 7. Most changes in gait that occur in older adults are related to underlying medical conditions, particularly as conditions increase in severity, and should not be viewed as merely an inevitable consequence of aging 7. Early identification of gait and balance disorders and appropriate intervention may prevent dysfunction and loss of independence.
At least 30 percent of persons 65 and older report difficulty walking three city blocks or climbing one flight of stairs, and approximately 20 percent require the use of a mobility aid to ambulate 8. In a sample of non-institutionalized older adults, 35 percent were found to have an abnormal gait 9. The prevalence of abnormal gait increases with age and is higher in persons in the acute hospital setting and in those living in long-term care facilities 10. In one study, gait disorders were detected in approximately 25 percent of persons 70 to 74 years of age, and nearly 60 percent of those 80 to 84 years of age 9.
Changes of Gait with Aging in the Elderly
Determining that a gait is abnormal can be challenging, because there are no clearly accepted standards to define a normal gait in an older adult 11. Studies comparing healthy persons in their 70s with healthy persons in their 20s demonstrate a 10 to 20 percent reduction in gait velocity and stride length in the older population 12. Other characteristics of gait that commonly change with aging include an increased stance width, increased time spent in the double support phase (i.e., with both feet on the ground), bent posture, and less vigorous force development at the moment of push off. These changes may represent adaptations to alterations in sensory or motor systems to produce a safer and more stable gait pattern.
The term “senile gait disorder” has been used to describe disturbances in gait in older persons when an underlying disease cannot be identified. It is characterized by a slow, broad-based, shuffling, and cautious walking pattern 13. However, current understandings of gait disorders challenge this term because most major changes in gait and balance are attributable to one or more underlying conditions. Up to 20 percent of older adults maintain normal gait patterns into very old age, reinforcing that aging is not inevitably accompanied by disordered gait 14. Senile gait patterns may actually represent an early manifestation of subclinical disease, because their occurrence correlates with increased risk of cardiovascular disease, dementia, institutionalization, and death 15.
Causes of balance and gait problems in the elderly
Medical conditions associated with gait and balance disorders are listed in Table 1. They may contribute to gait and balance disorders for a variety of reasons, such as causing pain, dyspnea (shortness of breath), imbalance, diminished strength, limited range of motion, poor posture, decreased sensory perception, fatigue, deformity, and decreased awareness of and ability to adapt to and traverse through possibly hazardous surroundings. In addition, recent surgery or hospitalization and other acute medical illnesses may lead to gait and balance disorders. The use of multiple medications (four or more), as well as specific classes of medications, can lead to gait disorders and an increased rate of falls 16.
Table 1. Medical Conditions and Risk Factors Associated with Gait and Balance Disorders
Affective disorders and psychiatric conditions |
|
|
|
|
Cardiovascular diseases |
|
|
|
|
|
|
| Infectious and metabolic diseases |
|
|
|
|
|
|
|
|
Musculoskeletal disorders |
|
|
|
|
|
|
|
Neurologic disorders |
|
|
|
|
|
|
|
|
|
|
Sensory abnormalities |
|
|
|
Other |
|
|
|
|
In one study performed in a family medicine setting, gait and balance disorders were multifactorial in origin in 75 percent of older patients 18. In this study of patients with self-reported difficulty in walking, the most common problems identified included arthritis (37 percent) and orthostatic hypotension (9 percent) 18. In a group of community-dwelling adults older than 88, joint pain was reported as the most common contributor to gait problems (32 percent), followed by several other causes, including stroke (1 percent), visual impairment (1 percent), and back or neck pain (0.5 percent) 14. Older patients referred to a neurology clinic for evaluation of a gait disorder of unknown cause were diagnosed with various neurologic conditions, including myelopathy (commonly related to cervical spondylosis), sensory abnormalities (either visual, vestibular, or proprioceptive dysfunction), multiple strokes, normal-pressure hydrocephalus, parkinsonism, and cerebellar disorders 7.
Table 2. Common Gait Patterns in Elderly
| Type of gait | Description | Associated signs | Causes |
|---|---|---|---|
Antalgic | Limited range of motion; limping; slow and short steps; unable to bear full weight | Pain worsening with movement and weight bearing | Degenerative joint disease; trauma |
Cautious | Arms and legs abducted; careful; en bloc turns; like walking on ice; slow; wide-based | Associated with anxiety, fear of falling, or open spaces | Deconditioning; post-fall syndrome; visual impairment |
Cerebellar ataxia | Staggering; wide-based | Dysarthria; dysdiadochokinesia; dysmetria; impaired check; intention tremor; nystagmus; postural instability; rebound; Romberg sign present; titubation | Cerebellar degeneration; drug or alcohol intoxication; multiple sclerosis; stroke; thiamine deficiency and vitamin B12 deficiency |
Choreic | Dance-like; irregular; slow; spontaneous knee flexion and leg rising; wide-based | Choreoathetotic movements of upper extremities | Huntington disease; levodopa-induced dyskinesia |
Dystonic | Abnormal posture of foot or leg; distorted gait; foot dragging; hyperflexion of hips | Worse with the action of walking; may improve when walking backward | — |
Frontal gait disorder (gait apraxia) | Magnetic; start and turn hesitation; freezing; marche à petits pas | Dementia; frontal lobe signs; incontinence | Frontal lobe degeneration; multi-infarct state; normal-pressure hydrocephalus |
Hemiparetic | Extension and circumduction of weak and spastic limb; flexed arm | Extensor plantar response; face, arm, and leg weakness; hyperreflexia | Hemispheric or brainstem lesion |
Paraparetic | Adduction; extension; scissoring of both legs; stiffness | Bilateral leg weakness; extensor plantar response; hyperreflexia; spasticity | Spinal cord or bilateral cerebral lesions |
Parkinsonian | Short-stepped; shuffling; hips, knees, and spine flexed; festination; en bloc turns | Bradykinesia; muscular rigidity; postural instability; reduced arm swing; rest tremor | Parkinson disease; atypical or secondary forms of parkinsonism |
Psychogenic | Astasia-abasia; bizarre and nonphysiologic gait; lurching; rare fall or injury | Absence of objective neurologic signs; give-way weakness | Factitious, somatoform disorders or malingering |
Sensory ataxia | Unsteady; worse without visual input, particularly at night | Distal sensory loss; impaired position and vibratory sensation; Romberg sign present | Dorsal column dysfunction; neuronopathy; sensory neuropathy |
Steppage | Resulting from footdrop; excessive flexion of hips and knees when walking; short strides; slapping quality; tripping | Atrophy of distal leg muscles; distal sensory loss and weakness footdrop; loss of ankle jerk | Motor neuropathy |
Vestibular ataxia | Unsteady; falling to one side; postural instability | Nausea; normal sensation, reflexes, and strength; nystagmus; vertigo | Acute labyrinthitis; Meniere disease |
Waddling | Lumbar lordosis; swaying; symmetric; toe walk; wide-based | Hip dislocation; proximal muscle weakness of lower extremities; use arms to get up from chair | Muscular dystrophy; myopathy |
Interventions
A multifactorial evaluation followed by targeted interventions for identified contributing factors can reduce falls by 30 to 40 percent 20 and is the most effective strategy for falls prevention. However, evidence on the effectiveness of interventions for gait and balance disorders is limited because of the lack of standardized outcome measures determining gait and balance abilities.
Because most gait and balance disorders in older persons are multifactorial in origin, they usually require several modes of treatment to restore, maintain, or improve functional capacity 21. In most cases, it is unlikely that gait disorders are reversible; however, modest improvements in gait and balance may be achievable, and interventions may impact important functional outcomes, such as reduction in rates of falls, fear of falling, weight-bearing pain, and overall limitations in mobility.
Many gait disorders are caused by chronic medical conditions that may be alleviated to some extent through targeted medical or surgical interventions. Gait disorders secondary to conditions such as arthritis, orthostatic hypotension, Parkinson disease, vitamin B12 deficiency, hypothyroidism, heart rate or rhythm abnormalities, or depression may respond to medical therapies 8.
What are the symptoms of a balance problem?
If you have a balance problem, you may stagger when you try to walk, or teeter or fall when you try to stand up. You might experience other symptoms such as:
- Dizziness or vertigo (a spinning sensation)
- Falling or feeling as if you are going to fall
- Lightheadedness, faintness, or a floating sensation
- Blurred vision
- Confusion or disorientation.
Other symptoms might include nausea and vomiting, diarrhea, changes in heart rate and blood pressure, and fear, anxiety, or panic. Symptoms may come and go over short time periods or last for a long time, and can lead to fatigue and depression.
What causes balance and gait problems
There are many causes of balance problems, such as medications, ear infections, a head injury, or anything else that affects the inner ear or brain. Low blood pressure can lead to dizziness when you stand up too quickly. Problems that affect the skeletal or visual systems, such as arthritis or eye muscle imbalance, can also cause balance disorders. Your risk of having balance problems increases as you get older.
Unfortunately, many balance disorders start suddenly and with no obvious cause.
Balance problems causes
The cause of balance problems is usually related to the specific sign or symptom.
Sense of motion or spinning (vertigo)
Vertigo can be associated with many conditions, including:
- Benign paroxysmal positional vertigo (BPPV). Benign paroxysmal positional vertigo occurs when calcium crystals in your inner ear — which help control your balance — are dislodged from their normal position and move elsewhere in the inner ear. Benign paroxysmal positional vertigo is the most common cause of vertigo. You might experience a spinning sensation when turning in bed or tilting your head back to look up.
- Meniere’s disease. In addition to sudden and severe vertigo, Meniere’s disease can cause fluctuating hearing loss and buzzing, ringing or a feeling of fullness in your ear. The cause of Meniere’s disease isn’t fully known. Meniere’s disease is rare and typically develops in people who are between the ages of 20 and 60.
- Migraine. Dizziness and sensitivity to motion (vestibular migraine) can occur due to migraine headache. Migraine is a common cause of dizziness.
- Acoustic neuroma. This noncancerous (benign), slow-growing tumor develops on a nerve that affects your hearing and balance. You might experience dizziness or loss of balance, but the most common symptoms are hearing loss and ringing in your ear. Acoustic neuroma is a rare condition.
- Vestibular neuritis. This inflammatory disorder, probably caused by a virus, can affect the nerves in the balance portion of your inner ear. Symptoms are often severe and persistent, and include nausea and difficulty walking. Symptoms can last several days and gradually improve on their own.
- Ramsay Hunt syndrome. Also known as herpes zoster otitis, this condition occurs when a shingles infection affects the facial nerve near one of your ears. You might experience vertigo, ear pain and hearing loss.
- Head injury. You might experience vertigo due to a concussion or other head injury.
- Motion sickness. You might experience dizziness in boats, cars and airplanes, or on amusement park rides.
- Persistent postural-perceptual dizziness. This disorder occurs frequently with other types of vertigo. Symptoms include unsteadiness or a sensation of motion in your head. Symptoms often worsen when you watch objects move, when you read, or when you are in a visually complex environment such as a shopping mall.
Feeling of faintness (presyncope)
Presyncope can be associated with:
- Orthostatic hypotension (postural hypotension). Standing or sitting up too quickly can cause some people to experience a significant drop in their blood pressure, resulting in presyncope.
- Cardiovascular disease. Abnormal heart rhythms (heart arrhythmia), narrowed or blocked blood vessels, a thickened heart muscle (hypertrophic cardiomyopathy), or a decrease in blood volume can reduce blood flow and cause presyncope.
Loss of balance (disequilibrium)
Losing your balance while walking, or feeling imbalanced, can result from:
- Vestibular problems. Abnormalities in your inner ear can cause a sensation of a floating or heavy head, and unsteadiness in the dark.
- Nerve damage to your legs (peripheral neuropathy). The damage can lead to difficulties with walking.
- Joint, muscle or vision problems. Muscle weakness and unstable joints can contribute to your loss of balance. Difficulties with eyesight also can lead to disequilibrium.
- Medications. Disequilibrium can be a side effect of medications.
- Certain neurologic conditions. These include cervical spondylosis and Parkinson’s disease.
Dizziness
A sense of dizziness or lightheadedness can result from:
- Inner ear problems. Abnormalities of the vestibular system can lead to a sensation of floating or other false sensation of motion.
- Psychiatric disorders. Depression (major depressive disorder), anxiety and other psychiatric disorders can cause dizziness.
- Abnormally rapid breathing (hyperventilation). This condition often accompanies anxiety disorders and may cause lightheadedness.
- Medications. Lightheadedness can be a side effect of medications.
How are balance problems diagnosed?
Diagnosis of a balance problem is difficult. To find out if you have a balance problem, your doctor may suggest that you see an otolaryngologist. An otolaryngologist is a physician and surgeon who specializes in diseases and disorders of the ear, nose, neck, and throat.
The otolaryngologist may ask you to have a hearing examination, blood tests, an electronystagmogram (a test that measures eye movements and the muscles that control them), or imaging studies of your head and brain. Another possible test is called posturography. For this test, you stand on a special movable platform in front of a patterned screen. The doctor measures how your body responds to movement of the platform, the patterned screen, or both.
Medical History
- Acute and chronic medical problems
- Complete review of systems
- Falls history (previous falls, injuries from falls, circumstances of fall, and associated symptoms)
- Nature of difficulty with walking (e.g., pain, imbalance) and associated symptoms
- Surgical history
- Usual activity, mobility status, and level of function
Medication review
- New medications or dosing changes
- Number and types of medications
Physical examination
- Affective/cognitive (delirium, dementia, depression, fear of falling)
- Cardiovascular (heart murmurs, arrhythmias, carotid bruits, pedal pulse)
- Musculoskeletal (joint swelling, deformity, or instability; limitations in range of motion involving the knees, hips, back, neck, arms, ankles, and feet; kyphosis; footwear)
- Neurologic (muscle strength and tone; reflexes; coordination; sensation; presence of tremor; cerebellar, vestibular, and sensory function; proprioception)
- Sensory (vision, hearing)
- Vitals (weight, height, orthostatic blood pressure and pulse)
Gait and balance performance testing
- Direct observation of gait and balance
- Functional reach test
- Timed Up and Go test
Because gait and balance disorders are major causes of falls, and predict future falls more consistently than other identified risk factors, evaluation of gait and balance is an essential step in identifying persons at increased risk of falling 22. In addition, patients who have fallen in the past year are significantly more likely to fall again 22.
Guidelines on fall prevention recommend that physicians ask older persons (especially those who are frail or vulnerable) at least annually about falls, and ask about or examine for difficulties with gait and balance at least once 23. Older persons who report a fall should be asked about difficulties with gait and balance, and should be observed for any gait or balance dysfunctions. Patients who present to their physician after a fall, report recurrent falls, demonstrate gait and balance abnormalities, or report difficulties in walking or balance should undergo a comprehensive assessment.
To determine if your symptoms are caused by problems in the balance function in your inner ear, your doctor is likely to recommend tests. They might include:
- Hearing tests. Difficulties with hearing are frequently associated with balance problems.
- Posturography test. Wearing a safety harness, you try to remain standing on a moving platform. A posturography test indicates which parts of your balance system you rely on most.
- Electronystagmography and video nystagmography. Both tests record your eye movements, which play a role in vestibular function and balance. Electronystagmography uses electrodes and video nystagmography uses small cameras to record eye movements.
- Rotary chair test. Your eye movements are analyzed while you sit in a computer-controlled chair that moves slowly in one place in a circle.
- Dix-Hallpike maneuver. Your doctor carefully turns your head in different positions while watching your eye movements to determine if you have a false sense of motion or spinning.
- Vestibular evoked myogenic potentials test. Sensor pads attached to your neck and forehead and under your eyes measure tiny changes in muscle contractions in reaction to sounds.
- Imaging tests. MRI and CT scans can determine if underlying medical conditions might be causing your balance problem.
- Blood pressure and heart rate tests. Your blood pressure might be checked when sitting and then after standing for 2 to 3 minutes to determine if you have significant drops in blood pressure. Your heart rate might be checked when standing to help determine if a heart condition is causing your symptoms.
Figure 6. Rotary chair test
Dix-Hallpike maneuver
How are balance problems treated?
The first thing a doctor will do if you have a balance problem is determine if another health condition or a medication is to blame. If so, your doctor will treat the condition, suggest a different medication, or refer you to a specialist if the condition is outside his or her expertise.
Your treatment may include:
- Balance retraining exercises (vestibular rehabilitation). Therapists trained in balance problems design a customized program of balance retraining and exercises. Therapy can help you compensate for imbalance, adapt to less balance and maintain physical activity. To prevent falls, your therapist might recommend a balance aid, such as a cane, and ways to reduce your risk of falls in your home.
- Positioning procedures. If you have benign paroxysmal positional vertigo, a therapist might conduct a procedure (canalith repositioning) that clears particles out of your inner ear and deposits them into a different area of your ear. The procedure involves maneuvering the position of your head.
- Diet and lifestyle changes. If you have Meniere’s disease or migraine headaches, dietary changes are often suggested that can ease symptoms. If you experience orthostatic hypotension, you might need to drink more fluids or wear compressive stockings.
- Medications. If you have severe vertigo that lasts hours or days, you might be prescribed medications that can control dizziness and vomiting.
- Surgery. If you have Meniere’s disease or acoustic neuroma, your treatment team may recommend surgery. Stereotactic radiosurgery might be an option for some people with acoustic neuroma. This procedure delivers radiation precisely to your tumor and doesn’t require an incision. Although data are limited, surgery may improve gait for patients with cervical spondylotic myelopathy 24, lumbar spinal stenosis 25, normal-pressure hydrocephalus 26, or arthritis of the knee or hip 27. Insertion of pacemakers in patients with carotid sinus hypersensitivity and first eye cataract surgery have been shown to reduce the rate of falls.48,49,56,57 Improving sensory input, with visual correction or hearing aids, may augment gait and function.
- The use of mobility aids, such as canes or walkers (properly fitted to the person), can reduce load on a painful joint and increase stability. Although evidence supporting the use of home environment assessment and intervention alone as a strategy to reduce falls in the general older population is mixed, evidence strongly supports home environment assessment and intervention as part of a multifactorial fall prevention program 28. In particular, home safety programs provided by a trained health care professional appear to be effective for persons at high risk of falls, such as those with a history of falls or other fall risk factors 29.
- Physical therapists can play an important role in the evaluation and treatment of persons with gait and balance disorders. They can help determine the impairments produced by a gait abnormality and develop individualized plans aimed at identified functional limitations 30.
- Other generally effective options for patients with gait and balance disorders include exercise and physical therapy 31. Exercise programs may target strength, balance, flexibility, or endurance. A Cochrane review found that programs containing two or more of these components reduce the rate of falls and number of persons falling 32. Exercising in supervised groups, particularly tai chi, and carrying out individually prescribed exercise programs at home are effective 31. A variety of exercise interventions, including walking, functional exercises, muscle strengthening, and multiple exercise types, have also been found to significantly improve balance 33.
If you have benign paroxysmal positional vertigo, your doctor might recommend a series of simple movements, such as the Epley maneuver, which can help dislodge the otoconia from the semicircular canal. In many cases, one session works; other people need the procedure several times to relieve their dizziness.
Epley maneuver to treat BPPV Vertigo
Deep Head Hanging Maneuver to Treat BPPV Vertigo
Lempert (BBQ) Maneuver to Treat BPPV Vertigo
Half Somersault Maneuver to Treat BPPV Vertigo
If you are diagnosed with Ménière’s disease, your doctor may recommend that you make some changes to your diet and, if you are a smoker, that you stop smoking. Anti-vertigo or anti-nausea medications may relieve your symptoms, but they can also make you drowsy. Other medications, such as gentamicin (an antibiotic) or corticosteroids may be used. Although gentamicin may reduce dizziness better than corticosteroids, it occasionally causes permanent hearing loss. In some severe cases of Ménière’s disease, surgery on the vestibular organs may be needed.
Some people with a balance disorder may not be able to fully relieve their dizziness and will need to find ways to cope with it. A vestibular rehabilitation therapist can help you develop an individualized treatment plan.
Talk to your doctor about whether it’s safe to drive, as well as ways to lower your risk of falling and getting hurt during daily activities, such as when you walk up or down stairs, use the bathroom, or exercise. To reduce your risk of injury from dizziness, avoid walking in the dark. You should also wear low-heeled shoes or walking shoes outdoors. If necessary, use a cane or walker and modify conditions at your home and workplace, such as by adding handrails.
Exercise for balance problems
Balance exercises can help prevent falls and avoid the disability that may result from falling. A simple fall can cause a serious fracture of the arm, hand, ankle, or hip. Each year, more than 2 million older Americans go to the emergency room because of fall-related injuries.
You can do balance exercises almost anytime, anywhere, and as often as you like as long as you have something sturdy nearby to hold on to for support.
Note: As you progress in your exercise routine, try adding the following challenges to help your balance even more:
- Start by holding on to a sturdy chair with both hands for support.
- When you are able, try holding on to the chair with only one hand.
- With time, hold on with only one finger, then with no hands at all.
- If you are really steady on your feet, try doing the balance exercises with your eyes closed
- You can do balance exercises almost anytime, anywhere, and as often as you like.
Also try lower-body strength exercises because they can help improve your balance. Do the lower-body strength exercises 2 or more days a week but not on any 2 days in a row.
Try these balance exercises:
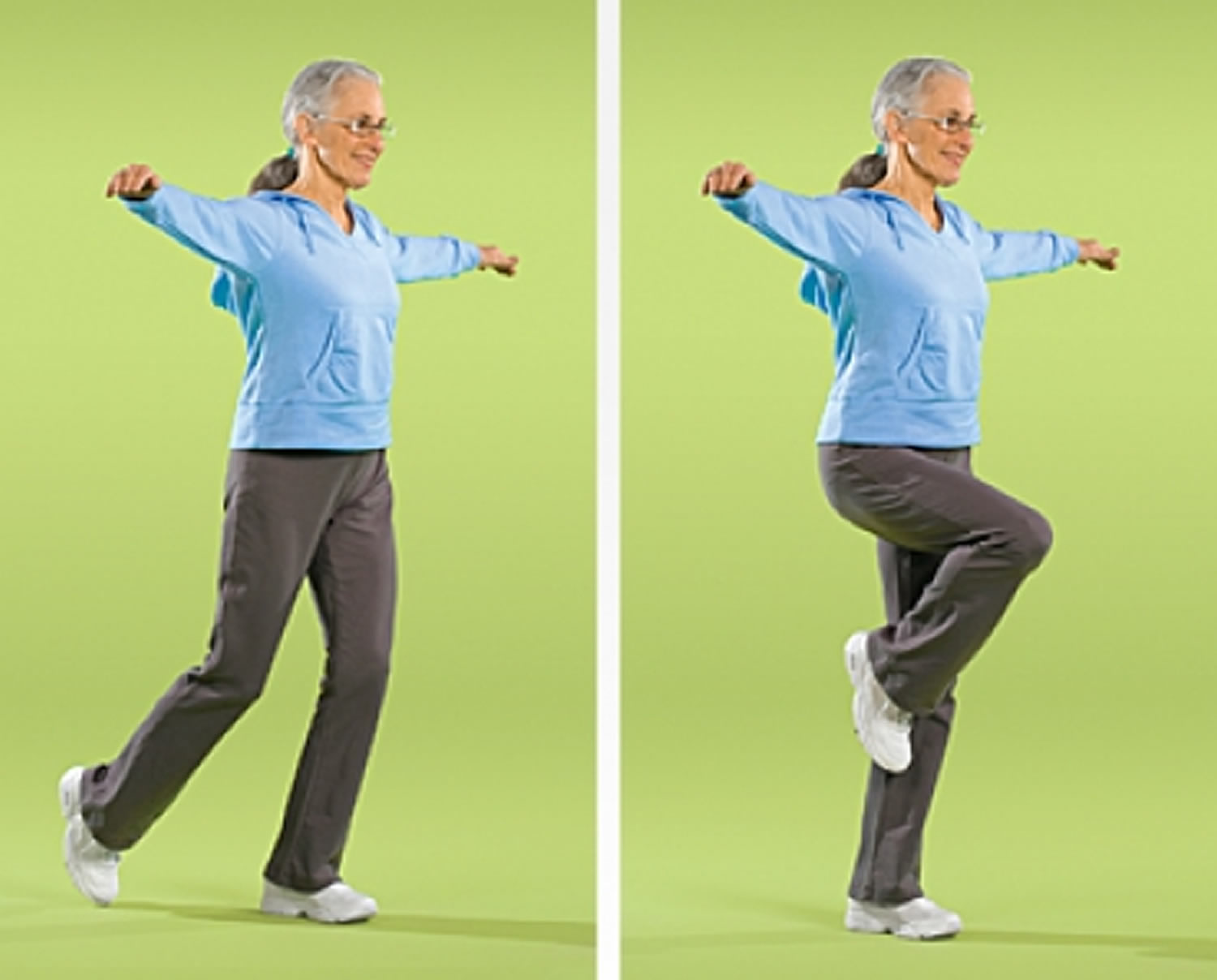
Stand on One Foot
You can do this exercise while waiting for the bus or standing in line at the grocery. For an added challenge, you can modify the exercise to improve your balance.
- Stand on one foot behind a sturdy chair, holding on for balance.
- Hold position for up to 10 seconds.
- Repeat 10-15 times.
- Repeat 10-15 times with other leg.
- Repeat 10-15 more times with each leg.
Figure 7. Stand on One Foot

Heel-to-Toe Walk
Having good balance is important for many everyday activities, such as going up and down stairs.
- Position the heel of one foot just in front of the toes of the other foot. Your heel and toes should touch or almost touch.
- Choose a spot ahead of you and focus on it to keep you steady as you walk.
- Take a step. Put your heel just in front of the toe of your other foot.
- Repeat for 20 steps.
Note: If you are unsteady on your feet, try doing this exercise near a wall so you can steady yourself if you need to.
Figure 8. Heel-to-Toe Walk

Balance Walk
Good balance helps you walk safely and avoid tripping and falling over objects in your way.
- Raise arms to sides, shoulder height.
- Choose a spot ahead of you and focus on it to keep you steady as you walk.
- Walk in a straight line with one foot in front of the other.
- As you walk, lift your back leg. Pause for 1 second before stepping forward.
- Repeat for 20 steps, alternating legs.
Note: As you progress, try looking from side to side as you walk, but skip this step if you have inner ear problems.
Figure 9. Balance Walk
Tai Chi
Balance is important to help you perform many of your daily activities and prevent falls. Research has shown that tai chi can significantly reduce the risk of falls among older people. In tai chi, which is sometimes called “moving meditation,” you work to improve your balance by moving your body slowly, gently, and precisely, while breathing deeply.
Other benefits from practicing tai chi include:
- improvements in bone and heart health
- easing of pain and stiffness from osteoarthritis
- better sleep
- improvements in overall wellness
Note: Try to put aside distracting thoughts and focus on being aware of your movements.
Figure 10. Tai Chi

Lower-body strength exercises
A number of lower-body exercises – especially those that strengthen your legs and ankles – also can help improve your balance.
These include:
Back Leg Raise
This exercise strengthens your buttocks and lower back. For an added challenge, you can modify the exercise to improve your balance.
- Stand behind a sturdy chair, holding on for balance. Breathe in slowly.
- Breathe out and slowly lift one leg straight back without bending your knee or pointing your toes. Try not to lean forward. The leg you are standing on should be slightly bent.
- Hold position for 1 second.
- Breathe in as you slowly lower your leg.
- Repeat 10-15 times.
- Repeat 10-15 times with other leg.
- Repeat 10-15 more times with each leg.
Figure 11. Back Leg Raise Strength Exercise for Seniors (you’ll need a sturdy chair)

Side Leg Raise
This exercise strengthens hips, thighs, and buttocks. For an added challenge, you can modify the exercise to improve your balance.
- Stand behind a sturdy chair with feet slightly apart, holding on for balance. Breathe in slowly.
- Breathe out and slowly lift one leg out to the side. Keep your back straight and your toes facing forward. The leg you are standing on should be slightly bent.
- Hold position for 1 second.
- Breathe in as you slowly lower your leg.
- Repeat 10-15 times.
- Repeat 10-15 times with other leg.
- Repeat 10-15 more times with each leg.
Figure 12. Side Leg Raise Strength Exercise for Seniors (you’ll need a sturdy chair)

Knee Curl
Walking and climbing stairs are easier when you do both the Knee Curl and Leg Straightening exercises. For an added challenge, you can modify the exercise to improve your balance.
- Stand behind a sturdy chair, holding on for balance. Lift one leg straight back without bending your knee or pointing your toes. Breathe in slowly.
- Breathe out as you slowly bring your heel up toward your buttocks as far as possible. Bend only from your knee, and keep your hips still. The leg you are standing on should be slightly bent.
- Hold position for 1 second.
- Breathe in as you slowly lower your foot to the floor.
- Repeat 10-15 times.
- Repeat 10-15 times with other leg.
- Repeat 10-15 more times with each leg.
Figure 13. Knee Curl Strength Exercise for Seniors (you’ll need a sturdy chair)

Leg Straightening
This exercise strengthens your thighs and may reduce symptoms of arthritis of the knee.
- Sit in a sturdy chair with your back supported by the chair. Only the balls of your feet and your toes should rest on the floor. Put a rolled bath towel at the edge of the chair under thighs for support. Breathe in slowly.
- Breathe out and slowly extend one leg in front of you as straight as possible, but don’t lock your knee.
- Flex foot to point toes toward the ceiling. Hold position for 1 second.
- Breathe in as you slowly lower leg back down.
- Repeat 10-15 times.
- Repeat 10-15 times with other leg.
- Repeat 10-15 more times with each leg.
Figure 14. Leg Straightening

Toe Stand
This exercise will help make walking easier by strengthening your calves and ankles. For an added challenge, you can modify the exercise to improve your balance.
- Stand behind a sturdy chair, feet shoulder-width apart, holding on for balance. Breathe in slowly.
- Breathe out and slowly stand on tiptoes, as high as possible.
- Hold position for 1 second.
- Breathe in as you slowly lower heels to the floor.
- Repeat 10-15 times.
- Rest; then repeat 10-15 more times.
Figure 15. Toe Stand Strength Exercise for Seniors (you’ll need a sturdy chair)

- Strupp M, Brandt T. Diagnosis and Treatment of Vertigo and Dizziness. Deutsches Ärzteblatt International. 2008;105(10):173-180. doi:10.3238/arztebl.2008.0173. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2696792/
- Epidemiology of vertigo. Neuhauser HK. Curr Opin Neurol. 2007 Feb; 20(1):40-6. https://www.ncbi.nlm.nih.gov/pubmed/17215687/
- Dizziness in primary care. Results from the National Ambulatory Medical Care Survey. Sloane PD. J Fam Pract. 1989 Jul; 29(1):33-8. https://www.ncbi.nlm.nih.gov/pubmed/2738548/
- Brandt T, Dieterich M, Strupp M. Vertigo – Leitsymptom Schwindel. Darmstadt: Steinkopff; 2003.
- Nevitt MC, Cummings SR, Kidd S, Black D. Risk factors for recurrent nonsyncopal falls. A prospective study. JAMA. 1989;261(18):2663–2668.
- Chu LW, Chi I, Chiu AY. Incidence and predictors of falls in the Chinese elderly [published correction appears in Ann Acad Med Singapore. 2005;34(7):469]. Ann Acad Med Singapore. 2005;34(1):60–72.
- Sudarsky L. Gait disorders: prevalence, morbidity, and etiology. Adv Neurol. 2001;87111–117.
- Centers for Disease Control and Prevention. Prevalence and most common causes of disability among adults—United States, 2005. MMWR Morb Mortal Wkly Rep. 2009;58(16):421–426.
- Verghese J, LeValley A, Hall CB, Katz MJ, Ambrose AF, Lipton RB. Epidemiology of gait disorders in community-residing older adults. J Am Geriatr Soc. 2006;54(2):255–261.
- Bloem BR, Gussekloo J, Lagaay AM, Remarque EJ, Haan J, Westendorp RG. Idiopathic senile gait disorders are signs of subclinical disease. J Am Geriatr Soc. 2000;48(9):1098–1101.
- Alexander NB. Gait disorders in older adults. J Am Geriatr Soc. 1996;44(4):434–451.
- Winter DA, Patla AE, Frank JS, Walt SE. Biomechanical walking pattern changes in the fit and healthy elderly. Phys Ther. 1990;70(6):340–347.
- Snijders AH, van de Warrenburg BP, Giladi N, Bloem BR. Neurological gait disorders in elderly people: clinical approach and classification. Lancet Neurol. 2007;6(1):63–74.
- Bloem BR, Haan J, Lagaay AM, van Beek W, Wintzen AR, Roos RA. Investigation of gait in elderly subjects over 88 years of age. J Geriatr Psychiatry Neurol. 1992;5(2):78–84.
- Verghese J, Lipton RB, Hall CB, Kuslansky G, Katz MJ, Buschke H. Abnormality of gait as a predictor of non-Alzheimer’s dementia. N Engl J Med. 2002;347(22):1761–1768.
- Kelly KD, Pickett W, Yiannakoulias N, et al. Medication use and falls in community-dwelling older persons [published correction appears in Age Ageing. 2004;33(1):91]. Age Ageing. 2003;32(5):503–509.
- Gait and Balance Disorders in Older Adults. Am Fam Physician. 2010 Jul 1;82(1):61-68. https://www.aafp.org/afp/2010/0701/p61.html
- Hough JC, McHenry MP, Kammer LM. Gait disorders in the elderly. Am Fam Physician. 1987;35(6):191–196.
- Zawora M, Liang TW, Jarra H. Neurological problems in the elderly. In: Arenson C, Busby-Whitehead J, Brummel-Smith K, O’Brien JG, Palmer MH, Reichel W, eds. Reichel’s Care of the Elderly: Clinical Aspects of Aging . 6th ed. New York, NY: Cambridge University Press; 2009:143.
- Chang JT, Morton SC, Rubenstein LZ, et al. Interventions for the prevention of falls in older adults: systematic review and meta-analysis of randomised clinical trials. BMJ. 2004;328(7441):680.
- Hausdorff JM, Nelson ME, Kaliton D, et al. Etiology and modification of gait instability in older adults: a randomized controlled trial of exercise. J Appl Physiol. 2001;90(6):2117–2129.
- Ganz DA, Bao Y, Shekelle PG, Rubenstein LZ. Will my patient fall? JAMA. 2007;297(1):77–86.
- Rubenstein LZ, Powers CM, MacLean CH. Quality indicators for the management and prevention of falls and mobility problems in vulnerable elders. Ann Intern Med. 2001;135(8 pt 2):686–693.
- Engsberg JR, Lauryssen C, Ross SA, Hollman JH, Walker D, Wippold FJ II. Spasticity, strength, and gait changes after surgery for cervical spondylotic myelopathy: a case report. Spine (Phila Pa 1976). 2003;28(7):E136–E139.
- Girardi FP, Cammisa FP Jr, Huang RC, Parvataneni HK, Tsairis P. Improvement of preoperative foot drop after lumbar surgery. J Spinal Disord Tech. 2002;15(6):490–494.
- Krauss JK, Faist M, Schubert M, et al. Evaluation of gait in normalpressure hydrocephalus before and after shunting. In: Ruzicka E, Hallet M, Jankovic J, eds. Gait Disorders. Philadelphia, Pa.: Lippincott Williams & Wilkins; 2001.
- Miki H, Sugano N, Hagio K, et al. Recovery of walking speed and symmetrical movement of the pelvis and lower extremity joints after unilateral THA. J Biomech. 2004;37(4):443–455.
- American Geriatrics Society, British Geriatrics Society, and American Academy of Orthopaedic Surgeons Panel on Falls Prevention Guideline for the prevention of falls in older persons. J Am Geriatr Soc. 2001;49(5):664–672.
- Campbell AJ, Robertson MC, La Grow SJ, et al. Randomised controlled trial of prevention of falls in people aged > or = 75 with severe visual impairment: the VIP trial. BMJ. 2005;331(7520):817.
- Harris MH, Holden MK, Cahalin LP, Fitzpatrick D, Lowe S, Canavan PK. Gait in older adults: a review of the literature with an emphasis toward achieving favorable clinical outcomes, part II. Clin Geriatrics. 2008;16(8):37–45.
- Gillespie LD, Gillespie WJ, Robertson MC, Lamb SE, Cumming RG, Rowe BH. Interventions for preventing falls in elderly people. Cochrane Database Syst Rev. 2009;(2):CD000340.
- Gillespie LD, Robertson MC, Gillespie WJ, et al. Interventions for preventing falls in older people living in the community. Cochrane Database Syst Rev. 2009;(2):CD007146.
- Schenkman M, Riegger-Krugh C. Physical intervention for elderly patients with gait disorders. In: Masdeu JC, Sudarsky L, Wolfson L, eds. Gait Disorders of Aging: Falls and Therapeutic Strategies. Philadelphia, Pa.: Lippincott-Raven; 1997:327–353.