Bart Pumphrey syndrome
Bart-Pumphrey syndrome also known as Schwann syndrome, is a rare genetic deafness disease characterized by symmetric or asymmetirc knuckle pads (typically located on the distal and interphalangeal joints), white discoloration of the nails (leukonychia), diffuse palmoplantar keratoderma, and congenital, mild to moderate sensorineural deafness 1. It was described in 1967 by Bart and Pumphrey 2. Bart and Pumphrey 2 reported a six-generation family with leukonychia, knuckle pads and congenital deafness. Some family members also had palmoplantar keratoderma. Before the report of Bart and Pumphrey, Schwann 3 had reported a child who was the only member of his family to manifest all of these findings.
People with Bart-Pumphrey syndrome typically have a white discoloration of the nails (leukonychia); the nails may also be thick and crumbly. Affected individuals often have wart-like (verrucous) skin growths called knuckle pads on the knuckles of the fingers and toes. They may also have thickening of the skin on the palms of the hands and soles of the feet (palmoplantar keratoderma). The skin abnormalities generally become noticeable during childhood. The hearing loss associated with Bart-Pumphrey syndrome ranges from moderate to profound and is typically present from birth (congenital) 4.
The signs and symptoms of Bart-Pumphrey syndrome may vary even within the same family; while almost all affected individuals have hearing loss, they may have different combinations of the other associated features.
Bart-Pumphrey syndrome is a rare disorder; its exact prevalence is unknown. Only a few families with Bart-Pumphrey syndrome have been reported worldwide. To date, the number of case reports or clinical series about Bart Pumphrey syndrome is less than 10 5. Bart-Pumphrey syndrome occurs in patients with pathogenic variants in the gap junction β2 gene (GJB2) encoding connexin 26 6.
Although there is currently no cure for Bart Pumphrey syndrome, treatment with oral retinoids can improve the skin symptoms. Leukonychia may improve with age. Patients with hearing loss may get benefit from hearing aids, cochlear implants, educational programs, speech therapy, and language training.
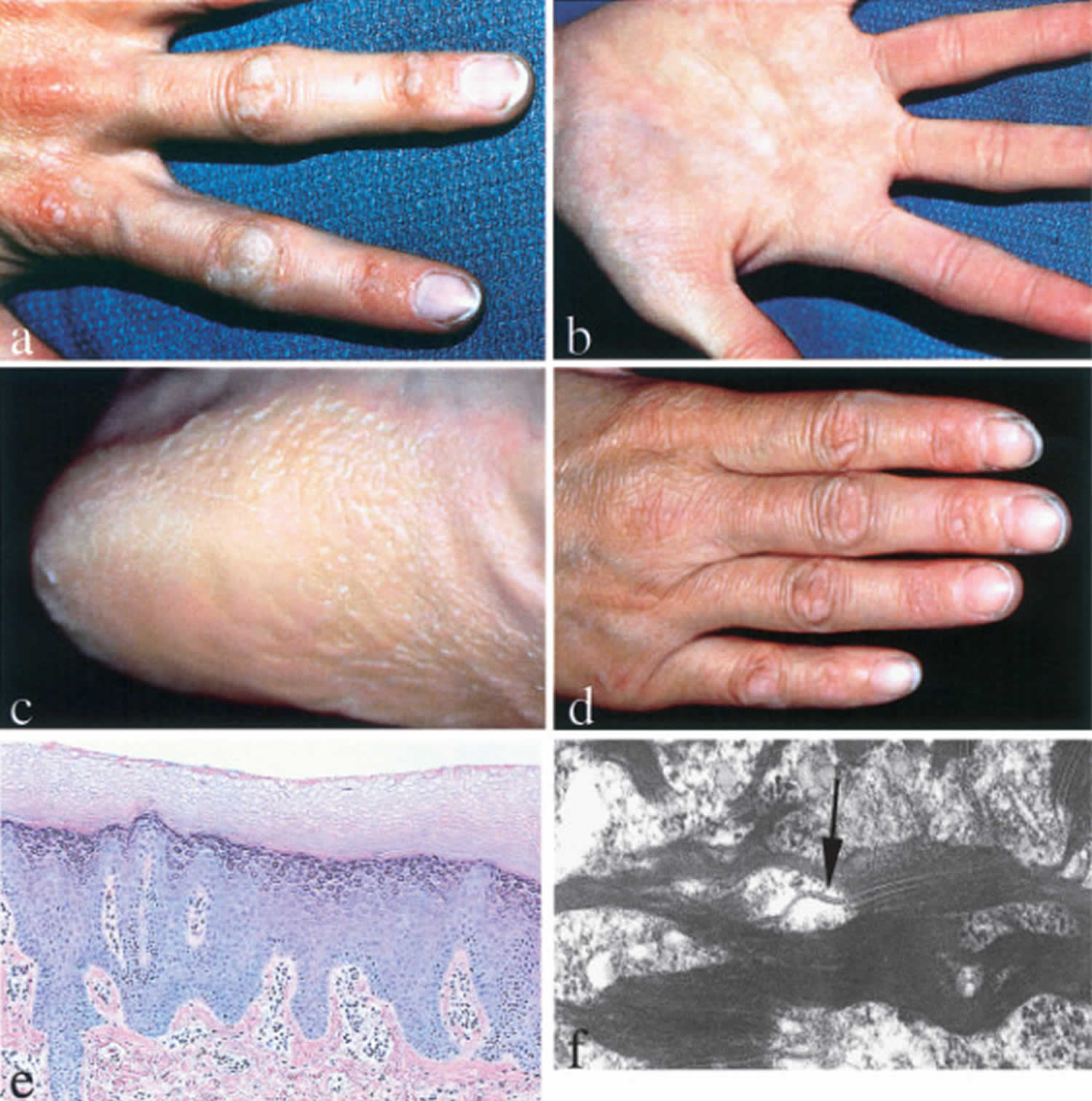
Figure 1. Bart Pumphrey syndrome
Footnote: Knuckle pads and leukonychia are seen on the hands and feet.
[Source 5 ]Bart Pumphrey syndrome causes
Bart-Pumphrey syndrome is caused by mutations in the gap junction β2 (GJB2) gene. This gene provides instructions for making a protein called gap junction beta 2, more commonly known as connexin 26. Connexin 26 is a member of the connexin protein family. Connexin proteins form channels called gap junctions that permit the transport of nutrients, charged atoms (ions), and signaling molecules between neighboring cells that are in contact with each other. Gap junctions made with connexin 26 transport potassium ions and certain small molecules.
Connexin 26 is found in cells throughout the body, including the inner ear and the skin. In the inner ear, channels made from connexin 26 are found in a snail-shaped structure called the cochlea. These channels may help to maintain the proper level of potassium ions required for the conversion of sound waves to electrical nerve impulses. This conversion is essential for normal hearing. In addition, connexin 26 may be involved in the maturation of certain cells in the cochlea. Connexin 26 also plays a role in the growth, maturation, and stability of the outermost layer of skin (the epidermis).
The GJB2 gene mutations that cause Bart-Pumphrey syndrome change single protein building blocks (amino acids) in the connexin 26 protein. The altered protein probably disrupts the function of normal connexin 26 in cells, and may interfere with the function of other connexin proteins. This disruption could affect skin growth and also impair hearing by disturbing the conversion of sound waves to nerve impulses.
Bart Pumphrey syndrome inheritance pattern
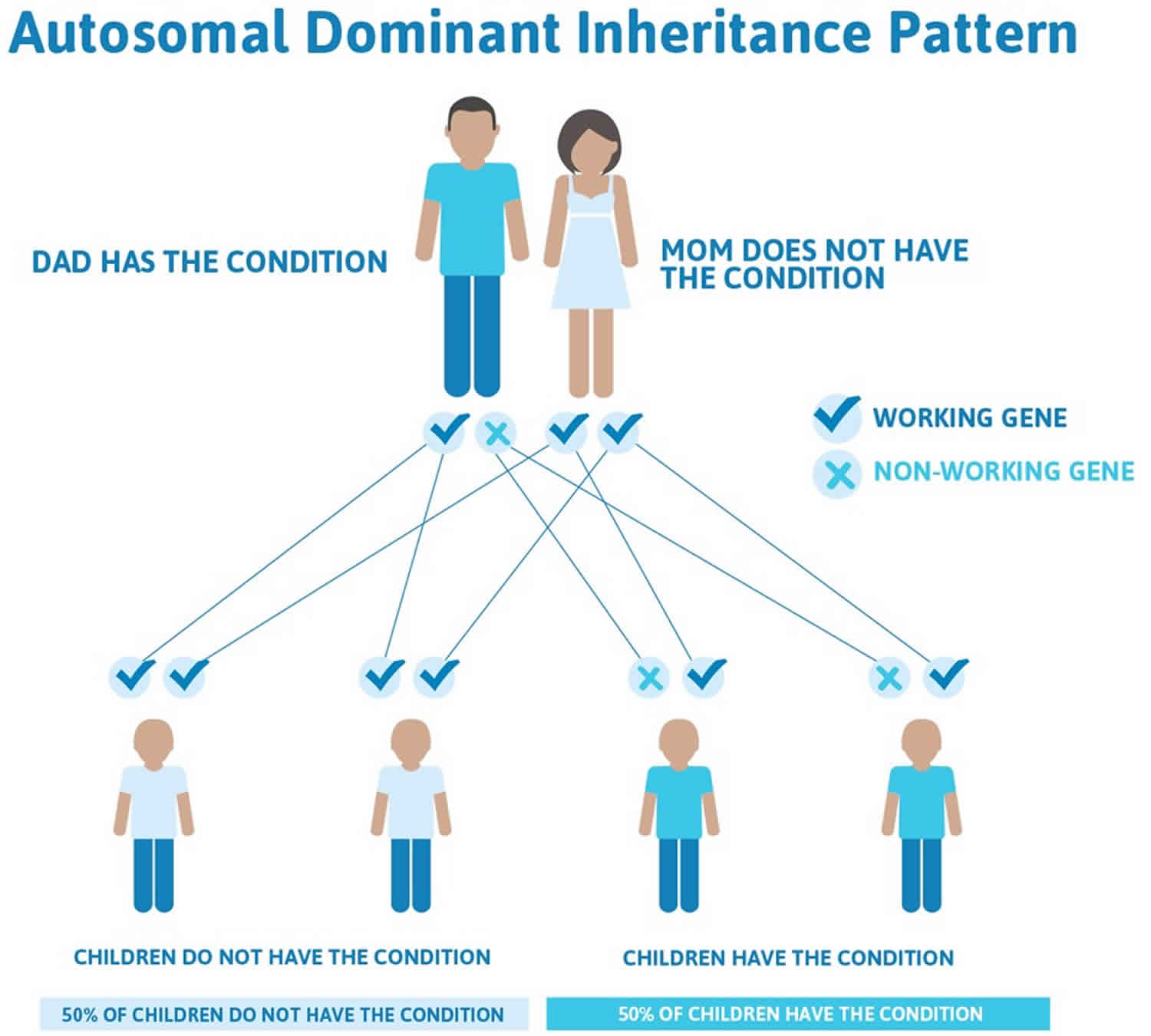
Bart Pumphrey syndrome is inherited in an autosomal dominant pattern, which means one copy of the altered gene in each cell is sufficient to cause the disorder. In most cases, an affected person has one parent with the condition. Other cases result from new mutations in the gene and occur in people with no history of the disorder in their family. This is called a de novo mutation.
Often autosomal dominant conditions can be seen in multiple generations within the family. If one looks back through their family history they notice their mother, grandfather, aunt/uncle, etc., all had the same condition. In cases where the autosomal dominant condition does run in the family, the chance for an affected person to have a child with the same condition is 50% regardless of whether it is a boy or a girl. These possible outcomes occur randomly. The chance remains the same in every pregnancy and is the same for boys and girls.
- When one parent has the abnormal gene, they will pass on either their normal gene or their abnormal gene to their child. Each of their children therefore has a 50% (1 in 2) chance of inheriting the changed gene and being affected by the condition.
- There is also a 50% (1 in 2) chance that a child will inherit the normal copy of the gene. If this happens the child will not be affected by the disorder and cannot pass it on to any of his or her children.
Figure 2 illustrates autosomal dominant inheritance. The example below shows what happens when dad has the condition, but the chances of having a child with the condition would be the same if mom had the condition.
Figure 2. Bart Pumphrey syndrome autosomal dominant inheritance pattern
People with specific questions about genetic risks or genetic testing for themselves or family members should speak with a genetics professional.
Resources for locating a genetics professional in your community are available online:
- The National Society of Genetic Counselors (https://www.findageneticcounselor.com/) offers a searchable directory of genetic counselors in the United States and Canada. You can search by location, name, area of practice/specialization, and/or ZIP Code.
- The American Board of Genetic Counseling (https://www.abgc.net/about-genetic-counseling/find-a-certified-counselor/) provides a searchable directory of certified genetic counselors worldwide. You can search by practice area, name, organization, or location.
- The Canadian Association of Genetic Counselors (https://www.cagc-accg.ca/index.php?page=225) has a searchable directory of genetic counselors in Canada. You can search by name, distance from an address, province, or services.
- The American College of Medical Genetics and Genomics (http://www.acmg.net/ACMG/Genetic_Services_Directory_Search.aspx) has a searchable database of medical genetics clinic services in the United States.
Bart Pumphrey syndrome signs and symptoms
Hearing loss and knuckle pads (typically located on the distal and interphalangeal joints) are the most common findings of Bart Pumphrey syndrome. Leukonychia (white discoloration of the nails) and palmoplantar hyperkeratosis (thickening of the skin on the palms of the hands and soles of the feet) are seen less frequently in Bart Pumphrey syndrome.
Knuckle pads are circumscribed, hyperkeratotic or fibrous thickenings over the dorsal aspects of the small joints of hands or feet 7. Most of the lesions are localized on the proximal interphalangeal joints, and two lesions presented over the inner surface of the wrist of the right hand. Location of knuckle pads over the wrist was reported by Ramer et al. 8. These lesions should be differentiated from “pseudo knuckle pads,” which are associated with occupational trauma and tend to disappear when traumatic stimulus is removed. Rheumatoid nodules and erythema elevatum diutinum should also be excluded.
Leukonychia that may be seen in Bart Pumphrey syndrome is defined as whiteness of nails that can occur either in patches or involving the total nail. Large keratohyaline granules are found in the keratinocytes, and the keratohyaline-containing cells reflected light, resulting in a white nail appearence 9. Leukonychia is usually autosomal dominantly inherited in syndromes including Bart Pumphrey syndrome 8.
Palmoplantar hyperkeratosis of Bart Pumphrey syndrome may be diffuse and striate, with accentuation of crease patterns and with grainy surface 10. Moreover, the severity and pattern of palmoplantar hyperkeratosis may be variable in members of the same family, such as in the present family. Mild hyperkeratosis may be ignored by the patients.
In Bart Pumphrey syndrome, hearing loss is generally of the sensorineural type. But, mixed sensorineural and conductive loss may also be seen 8.
Bart Pumphrey syndrome diagnosis
Bart Pumphrey syndrome need to be differentiated from other clinically similar lesions that may require specific treatments or are related to important underlying pathology. The presence of leukonychia and the absence of digital constrictions appear to distinguish Bart Pumphrey syndrome from Vohwinkel syndrome 11. Vohwinkel syndrome is an inherited condition that affects the skin. People with the “classic form of Vohwinkel syndrome” generally have honeycomb-patterned calluses on the palms of the hands and the soles of the feet (palmoplantar keratoses); constricting bands of tissue on the fingers and toes which can cause amputation; starfish-shaped, thickened skin on the tops of the fingers and knees; and hearing loss. A “variant form” of Vohwinkel syndrome has also been identified which is characterized by ichthyosis in addition to the classic skin abnormalities and is not associated with hearing loss 12. Classic Vohwinkel syndrome is caused by changes (mutations) in the GJB2 gene and the variant form is caused by mutations in the LOR gene. Both are inherited in an autosomal dominant manner 13.
A biopsy is indicated if the diagnosis is in doubt. Light microscopic evaluation of skin biopsies revealed massive orthokeratotic hyperkeratosis without evidence for retained nuclei, hypergranulosis, acanthosis, and papillomatosis. Epidermal gap junctions appeared normal on electron microscopic evaluation.
Molecular genetics
To date, there have been two observed mutated residues, N54K and G59S, which are responsible for Bart Pumphrey syndrome 5. Both mutations are in the extracellular domain of GBJ2, the gene encoding connexin-26 (C×26). Mutations in Connexin 26 may be the cause of both non-syndromic and syndromic deafness associated with skin disorder, such as Vohwinkel syndrome and keratitis-ichthyosis deafness syndrome, besides Bart Pumphrey syndrome. Connexin 26 is in gap junctions and plays a role in exchange of ions and small molecules between adjacent cells by forming intercellular channels 14. In a multigeneration Polish family with Bart-Pumphrey syndrome, Richard et al. 15 investigated GJB2 mutations and reported that immunostaining of C×26 was weak or absent in lesional palmar and knuckle skin, although its adnexal expression and other epidermal connexins were not altered. They found Cx30 (GJB6) compensatory overexpression throughout the spinous cell layers in their investigation. The authors emphasized that GJB2 mutations were responsible for dermatological disorders associated with syndromic hearing loss 16.
In a 26-year-old male with Bart-Pumphrey syndrome, Alexandrino et al. 17 identified heterozygosity for a missense mutation in the GJB2 gene.
Bart Pumphrey syndrome treatment
Although there is currently no cure for Bart Pumphrey syndrome, treatment with oral retinoids can improve the skin symptoms. Leukonychia may improve with age. Patients with hearing loss may get benefit from hearing aids, cochlear implants, educational programs, speech therapy, and language training.
References- Al-Hamdi KI, Qais Saadoon A, Abduljabbar NH. Bart-Pumphrey Syndrome. JAMA Dermatol. 2020;156(10):1126. doi:10.1001/jamadermatol.2020.2555
- Bart RS, Pumphrey RE. Knuckle pads, leukonychia and deafness. A dominantly inherited syndrome. N Engl J Med. 1967 Jan 26;276(4):202-7. doi: 10.1056/NEJM196701262760403
- Schwann, J. Keratosis palmaris et plantaris cum surditate congenita et leuconychia totali unguium. Dermatologica 126: 335-353.
- Bart-Pumphrey syndrome. https://medlineplus.gov/genetics/condition/bart-pumphrey-syndrome
- Gönül M, Gül Ü, Hizli P, Hizli Ö. A family of Bart-Pumphrey syndrome. Indian J Dermatol Venereol Leprol 2012;78:178-81. https://www.ijdvl.com/text.asp?2012/78/2/178/93636
- Alexandrino F, Sartorato EL, Marques-de-Faria AP, Steiner CE . G59S Mutation in the GJB2 (Connexin 26) Gene in patient with Bart-Pumphrey syndrome. Am J Med Genet Am 2005;136:282-4.
- Burrows NP, Lowell CR. Disorders of connective tissue. In. Burns T, Breathnach S, Cox N, Griffiths C. Rook’s Textbook of Dermatology; 8th ed, Vol. 3. Chichester: Wiley-Blackwell; 2010. p. 45-8.
- Ramer JC, Vasily DB, Ladda RL. Familial leukonychia, knuckle pads, hearing loss, and palmoplantar hyperkeratosis: An additional family with Bart-Pumphrey syndrome. J Med Genet 1994;31:68-71.
- de D, Handa S. Hereditary leukonychia totalis. Indian J Dermatol Venereol Leprol 2007;73:355-7.
- Leonard NJ, Krol AL, Bleoo S, Somerville MJ. Sensorineural hearing loss, striate palmoplantar hyperkeratosis, and knuckle pads in a patients with a novel connexin 26 (GJB2) mutation. J Med Genet 2005;42: e2.
- Bart Pumphrey syndrome. https://www.omim.org/entry/149200
- Vohwinkel Syndrome. https://emedicine.medscape.com/article/1108458-overview
- Vohwinkel syndrome. https://medlineplus.gov/genetics/condition/vohwinkel-syndrome
- Lee JR, White TW. Connexin-26 mutations in deafness and skin disease. Expert Rev Mol Med 2009;11: e35.
- Richard G, Brown N, Ishida-Yamamoto A, Krol A. Expanding the phenotypic spectrum of Cx26 disorders: Bart-Pumphrey syndrome is caused by a novel missense mutation in GJB2. J Invest Dermatol. 2004 Nov;123(5):856-63. doi: 10.1111/j.0022-202X.2004.23470.x
- Kose O, Baloglu H. Knuckle pads, leukonychia and deafness. Int J Dermatol 1996;35:728-9.
- Alexandrino F, Sartorato EL, Marques-de-Faria AP, Steiner CE. G59S mutation in the GJB2 (connexin 26) gene in a patient with Bart-Pumphrey syndrome. Am J Med Genet A. 2005 Jul 30;136(3):282-4. doi: 10.1002/ajmg.a.30822