What is bone marrow transplant
A bone marrow transplant is a blood and bone marrow stem cell transplant from a healthy donor to a recipient whose own bone marrow is affected by disease. Bone marrow transplant replaces a person’s abnormal stem cells with healthy ones from another person (a donor). Bone marrow is the soft, sponge-like material found inside bones. It contains immature cells known as hematopoietic stem cells or blood-forming stem cells. Bone marrow transplant procedure allows the recipient to get new hematopoietic stem cells that work properly. Hematopoietic stem cells are found in bone marrow and hematopoietic stem cells divide to form more blood-forming stem cells, or they mature into one of three types of blood cells that the body needs:
- Red blood cells, which carry oxygen through the body
- White blood cells, which fight infection
- Platelets, which help the blood clot
Most hematopoietic stem cells are found in the bone marrow, but some cells, called peripheral blood stem cells, are found in the bloodstream. Blood in the umbilical cord (the cord that connects a fetus to the mother’s placenta) also contains hematopoietic stem cells. Cells from any of these sources can be used in transplants.
Another type of stem cell, called an embryonic stem cell, can develop into any type of cell in the body. These cells are not found in bone marrow.
Doctors use stem cell transplants to treat people who have:
- Certain cancers, such as leukemia. The high doses of chemotherapy and radiation used to treat some cancers can severely damage or destroy bone marrow. A transplant replaces the stem cells that the treatment destroyed.
- Severe blood diseases, such as thalassemias, aplastic anemia, and sickle cell anemia. The body doesn’t make enough red blood cells, or they don’t work properly.
- Certain immune-deficiency diseases that prevent the body from making some kinds of white blood cells. Without these cells, a person can develop life-threatening infections. A transplant provides stem cells to replace the missing white blood cells.
Hematopoietic stem cell transplants, including peripheral blood, bone marrow, and cord blood transplants, can be used to treat cancer. Bone marrow transplants are most often used for cancers affecting the blood-forming tissues or immune system, such as leukemia, lymphoma, multiple myeloma; certain solid cancers such as neuroblastoma; immune deficiency diseases; and metabolic diseases; aplastic anemia and sickle cell anemia.
Stem cell transplants have serious risks. Some complications are life threatening. For some people, however, stem cell transplants are the best hope for a cure or a longer life.
Is bone marrow transplant painful?
No. The infusion of stem cells will be given through your central venous catheter, much like a blood transfusion, which is painless.
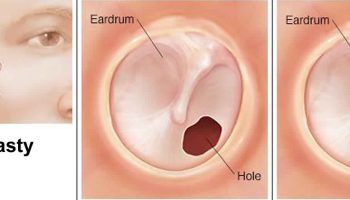
Figure 1. Bone marrow transplant
Figure 2. Bone marrow anatomy
Figure 3. Blood cell development. A blood stem cell goes through several steps to become a red blood cell, platelet, or white blood cell
What makes hematopoietic stem cells so important?
Hematopoietic stem cells make the 3 main types of blood cells: red blood cells, white blood cells, and platelets.
You need all of these types of blood cells to keep you alive. For these blood cells to do their jobs, you need to have enough of each type in your blood.
Red blood cells (RBCs) carry oxygen away from the lungs to all of the cells in the body. They bring carbon dioxide from the cells back to the lungs to be exhaled.
A blood test called a hematocrit shows how much of your blood is made up of RBCs. The normal range is about 35% to 50% for adults. People whose hematocrit is below this level have anemia. This can make them look pale and feel weak, tired, and short of breath.
White blood cells (WBCs) help fight infections caused by bacteria, viruses, and fungi. There are different types of WBCs.
- Neutrophils are the most important type in fighting bacterial infections. The absolute neutrophil count (ANC) is a measure of the neutrophils in your blood. When your absolute neutrophil count drops below 1,000 per cubic millimeter (1,000/mm3) you have neutropenia, and you have a higher risk of infection. The danger is greatest when levels are below 500/mm3.
- Lymphocytes are another type of white blood cell. There are different kinds of lymphocytes, such as T lymphocytes (T cells), B lymphocytes (B cells), and natural killer (NK) cells. Some lymphocytes make antibodies to help fight infections. The body depends on lymphocytes to recognize its own cells and reject cells that don’t belong in the body, such as invading germs or cells that are transplanted from someone else.
Platelets (thrombocytes) are pieces of cells that seal damaged blood vessels and help blood to clot, both of which are important in stopping bleeding. A normal platelet count is usually between 150,000/mm3 and 450,000/mm3, depending on the lab that does the test. A person whose platelet count drops below normal is said to have thrombocytopenia, and may bruise more easily, bleed longer, and have nosebleeds or bleeding gums. Spontaneous bleeding (bleeding with no known injury) can happen if a person’s platelet count drops lower than 20,000/mm3. This can be dangerous if bleeding occurs in the brain, or if blood begins to leak into the intestines or stomach.
Where do stem cells come from?
Depending on the type of transplant that’s done, there are 3 possible sources of stem cells to use for transplants:
- Bone marrow (from you or someone else)
- The bloodstream (peripheral blood – from you or someone else)
- Umbilical cord blood from newborns
Bone marrow
Bone marrow is the spongy liquid tissue in the center of some bones. It has a rich supply of stem cells, and its main job is to make blood cells that circulate in your body. The bones of the pelvis (hip) have the most marrow and contain large numbers of stem cells. For this reason, cells from the pelvic bone are used most often for a bone marrow transplant. Enough marrow must be removed to collect a large number of healthy stem cells.
The bone marrow is harvested (removed) while the donor is under general anesthesia (drugs are used to put the patient into a deep sleep so they don’t feel pain). A large needle is put through the skin on the lower back and into the back of the hip bone. The thick liquid marrow is pulled out through the needle. This is repeated until enough marrow has been taken out.
The harvested marrow is filtered, stored in a special solution in bags, and then frozen. When the marrow is to be used, it’s thawed and then put into the patient’s blood through a vein, just like a blood transfusion. The stem cells travel to the bone marrow, where they engraft or “take” and start to make blood cells. Signs of the new blood cells usually can be measured in the patient’s blood tests in about 2 to 4 weeks.
Peripheral blood
Normally, not many stem cells are found in the blood. But giving shots of hormone-like substances called growth factors to stem cell donors a few days before the harvest causes their stem cells to grow faster and move from the bone marrow into the blood.
For a peripheral blood stem cell transplant, the stem cells are taken from blood. A special thin flexible tube (called a catheter) is put into a large vein in the donor and attached to tubing that carries the blood to a special machine. The machine separates the stem cells from the rest of the blood, which is returned to the donor during the same procedure. This takes several hours, and may need to be repeated for a few days to get enough stem cells. The stem cells are filtered, stored in bags, and frozen until the patient is ready for them.
When they’re given to the patient, the stem cells are put into a vein, much like a blood transfusion. The stem cells travel to the bone marrow, engraft, and then start making new, normal blood cells. The new cells are usually found in the patient’s blood in about 10 to 20 days.
Umbilical cord blood
A large number of stem cells are normally found in the blood of newborn babies. After birth, the blood that’s left behind in the placenta and umbilical cord (known as cord blood) can be taken and stored for later use in a stem cell transplant. The cord blood is frozen until needed. A cord blood transplant uses blood that normally is thrown out after a baby is born.
A possible drawback of cord blood is the smaller number of stem cells in it. But this is partly balanced by the fact that each cord blood stem cell can form more blood cells than a stem cell from adult bone marrow. Still, cord blood transplants can take longer to take hold and start working. Cord blood is given into the patient’s blood just like a blood transfusion.
Evaluation and preparation for a bone marrow transplant
You will first be evaluated to find out if you are eligible for a transplant. A transplant is very hard on your body. For many people, transplants can mean a cure, but for some people, problems can lead to severe complications or even death. You’ll want to weigh the pros and cons before you start.
Transplants can also be hard emotionally. They often require being in the hospital, being isolated, and there’s a high risk of side effects. Many of the effects are short-term, but some problems can go on for years. This can mean changes in the way you live your life. For some people it’s just for a while, but for others, the changes may be lifelong.
Before you have a transplant, you need to discuss the transplant process and all its effects with your doctors. It also helps to talk to others who have already had transplants.
It’s also very hard going through weeks and months of not knowing how your transplant will turn out. This takes a lot of time and emotional energy from the patient, caregivers, and loved ones. It’s very important to have the support of those close to you. For example, you’ll need a responsible adult who will be with you to give you medicines, help watch for problems, and stay in touch with your transplant team after you go home. Your transplant team will help you and your caregiver learn what you need to know. The team can also help you and your loved ones work through the ups and downs as you prepare for and go through the transplant.
Many different medical tests will be done, and questions will be asked to try to find out how well you can handle the transplant process. These might include:
- HLA tissue typing, including high-resolution typing
- A complete health history and physical exam
- Evaluation of your psychological and emotional strengths
- Identifying who will be your primary caregiver throughout the transplant process
- Bone marrow biopsy
- CT (computed tomography) scan or MRI (magnetic resonance imaging)
- Heart tests, such as an EKG (electrocardiogram) or echocardiogram
- Lung studies, such as a chest x-ray and PFTs (pulmonary function tests)
- Consultations with other members of the transplant team, such as a dentist, dietitian, or social worker
- Blood tests, such as a complete blood count, blood chemistries, and screening for viruses like hepatitis B, CMV, and HIV
You will also talk about your health insurance coverage and related costs that you might have to pay.
You may have a central venous catheter (CVC) put into a large vein in your chest. This is most often done as outpatient surgery, and usually only local anesthesia is needed (the place where the catheter goes in is made numb). Nurses will use the catheter to draw blood and give you medicines.
If you’re getting an autologous transplant, a special catheter can be placed that can also be used for apheresis to harvest your stem cells.
The central venous catheter will stay in during your treatment and for some time afterward, usually until your transplanted stem cells have engrafted and your blood counts are on a steady climb to normal.
Bone marrow transplant eligibility
Younger people, those who are in the early stages of disease, or those who have not already had a lot of treatment, often do better with transplants. Some transplant centers set age limits. For instance, they may not allow regular allogeneic transplants for people over 50 or autologous transplants for people over 65. Some people also may not be eligible for transplant if they have other major health problems, such as serious heart, lung, liver, or kidney disease.
Hospital admission or outpatient treatment
The hospital’s transplant team will decide if you need to be in the hospital to have your transplant, if it will be done in an outpatient center, or if you will be in the hospital just for parts of it. If you have to be in the hospital, you will probably go in the day before the transplant procedure is scheduled to start. Before conditioning treatment begins (see section below), the transplant team makes sure you and your family understand the process and want to go forward with it.
If you will be having all or part of your transplant as an outpatient, you’ll need to be very near the transplant center during the early stages. You’ll need a family member or loved one as a caregiver who can stay with you all the time. You and the caregiver will also need reliable transportation to and from the clinic. The transplant team will be watching you closely for complications, so expect to be at the clinic every day for a few weeks. You may still need to be in the hospital if your situation changes or if you start having complications.
To reduce the chance of infection during treatment, patients who are in the hospital are put in private rooms that have special air filters. The room may also have a protective barrier to separate it from other rooms and hallways. Some have an air pressure system that makes sure no unclean outside air gets into the room. If you’re going to be treated as an outpatient, you will get instructions on avoiding infection.
The transplant experience can be overwhelming. Your transplant team will be there to help you physically and emotionally prepare for the process and discuss your needs. Every effort will be made to answer questions so you and your family fully understand what will be happening to you as you go through transplant.
It’s important for you and your family to know what to expect, because once conditioning treatment begins (see the next section), there’s no going back – there can be serious problems if treatment is stopped at any time during transplant.
Types of bone marrow transplants
There are three types of transplants:
- In autologous transplants, patients receive their own stem cells.
- In syngeneic transplants, patients receive stem cells from their identical twin. Because identical twins have the same genes, they have the same set of human leukocyte antigens (HLAs). As a result, the patient’s body will accept a transplant from an identical twin. However, identical twins represent a small number of all births, so syngeneic transplantation is rare.
- In allogeneic transplants (from a donor), patients receive stem cells from their brother, sister, or parent. A person who is not related to the patient (an unrelated donor) also may be used. Allogeneic transplant is most often used to treat certain types of leukemia, lymphomas, multiple myeloma, myelodysplastic syndrome, and other bone marrow disorders such as aplastic anemia.
Today, the two most commonly used bone marrow stem cell transplants are known as autologous (from your own stem cells) and allogeneic (from a donor). Both types of bone marrow stem cell transplants are considered forms of stem cell therapy, since hematopoietic stem cells from the bone marrow are central to the recovery of the patient receiving the graft.
Autologous bone marrow transplant
For an autologous transplant, your own stem cells are collected, frozen and stored for use later. This works best when you still have enough healthy hematopoietic stem cells, even though you’re sick. If you have cancer, the cancer cells are removed or destroyed from the collected cells.
There are 2 options to your hematopoietic stem cells collection. Your doctor will decide which is best for you.
- Peripheral blood stem cell collection: The cells are collected from your bloodstream. This process is called apheresis. Before apheresis, you get shots for a few days to increase the number of blood-forming cells in your bloodstream. During apheresis, blood is removed from your vein through an intravenous (IV) line, passed through a machine, and put back into your vein. The machine takes out the blood-forming cells that will be used for your transplant. Most patients who have an autologous transplant collect their cells this way.
- Bone marrow collection: The cells are collected from the pelvic (hip) bone during surgery. You get anesthesia so you don’t feel pain. A doctor uses a special needle to take out the blood-forming cells from your bone marrow.
In an autologous bone marrow transplant, hematopoietic stem cells are harvested from the blood or bone marrow of a patient before the patient undergoes high doses of chemotherapy or radiation treatment for cancer and storing these cells prior to therapy. In order to remove tumor cells that may have been collected with the stem cells, the sample is incubated with antibodies that bind only to stem cells. The stem cells are then isolated and stored for later use, when they are reinfused into the patient. An autologous transplant is used primarily in the case of cancer patients who are preparing to undergo high doses of chemotherapy or radiation therapy.
A possible disadvantage of an autologous transplant is that cancer cells may be collected along with the stem cells and then later put back into your body. Another disadvantage is that your immune system is the same as it was before your transplant. This means the cancer cells were able to escape attack from your immune system before, and may be able to do so again.
To help prevent this, some centers treat the stem cells before they’re given back to the patient to try to kill any remaining cancer cells. This may be called purging. It isn’t clear that this really helps, as it has not yet been proven to reduce the risk of cancer coming back. A possible downside of purging is that some normal stem cells can be lost during this process. This may cause your body to take longer to start making normal blood cells, and you might have very low and unsafe levels of white blood cells or platelets for a longer time. This could increase the risk of infections or bleeding problems.
Another treatment to help kill cancer cells that might be in the returned stem cells involves giving anti-cancer drugs after transplant. The stem cells are not treated. After transplant, the patient gets anti-cancer drugs to get rid of any cancer cells that may be in the body. This is called in vivo purging. For instance, rituximab (Rituxan®), a monoclonal antibody drug, may be used this way in certain lymphomas and leukemias; lenalidomide (Revlimid®) may be used for multiple myeloma. The need to remove cancer cells from transplanted stem cells or transplant patients and the best way to do it is being researched.
After the patient has undergone therapy to destroy the cancer cells, the hematopoietic stem cells are injected into the bloodstream to speed recovery of the bone marrow. If an individual’s marrow is diseased—from leukemia, for example—a person with a matching tissue type is found to donate stem cells. This type of transplant is called an allogeneic transplant.
What is a “tandem transplant”?
A “tandem transplant” or double autologous transplant, is a type of autologous transplant. This method is being studied in clinical trials for the treatment of several types of cancer, including multiple myeloma and germ cell cancer. During a tandem transplant, a patient receives two sequential courses of high-dose chemotherapy with stem cell transplant. Typically, the two courses are given several weeks to several months apart.
Tandem transplants are most often used to treat multiple myeloma and advanced testicular cancer. But doctors don’t always agree that these are really better than a single transplant for certain cancers. Because this involves 2 transplants, the risk of serious outcomes is higher than for a single transplant. Tandem transplants are still being studied to find out when they might be best used. Researchers hope that this method can prevent the cancer from recurring (coming back) at a later time.
Sometimes an autologous transplant followed by an allogeneic transplant might also be called a tandem transplant.
Allogeneic bone marrow transplant
For an allogenic transplant, you get hematopoietic stem cells from a donor. The donor can be a relative (like a brother or sister) or, sometimes, an unrelated person. You also may get stem cells from umbilical cord blood donated by an unrelated person. This is the blood collected from the umbilical cord and placenta after a baby is born. This small volume of cord blood has a high number of stem cells that tend to multiply quickly. But there are often not enough stem cells in a unit of cord blood for large adults, so most cord blood transplants done so far have been in children and smaller adults. Researchers are now looking for ways to use cord blood for transplants in larger adults. One approach is to find ways to increase the numbers of these cells in the lab before the transplant. Another approach is the use of the cord blood from 2 infants for one adult transplant, called a dual-cord-blood transplant. A third way cord blood is being used is in a “mini-transplant” (see below). Other strategies to better use cord blood transplants are being actively studied.
To prevent problems, the donor’s stem cells should match yours as closely as possible. Donors and recipients are matched through a blood test called human leukocyte antigen (HLA) tissue typing.
The best bone marrow transplant outcomes (results) happen when a patient’s HLA closely matches the donor’s HLA. A close HLA match also helps lower the risk for problems after transplant. The best donor is a close family member, usually a brother or sister.
Matching HLA markers is much more complex than matching blood types.
A close match is important because it:
- Improves the chances for a successful transplant.
- Helps your donor cells engraft (grow and make new blood cells in your body).
- Reduces the risk of complications like graft-versus-host disease. GVHD (graft-versus-host disease) happens when the immune cells from the donated cells (the graft) attack the recipient’s cells (the host).
There are times when a closely matched donor isn’t the best option. For some patients, a donor who matches exactly half of their HLA is best. This is called a haploidentical (or half-matched) transplant.
Usually, your doctor will first look for a matching donor in your family usually a brother or sister. That’s because you inherit HLA markers from your parents. Each brother and sister has a 25% (1 out of 4) chance of completely matching you, if you have the same mom and dad. Your parents and your children always match exactly half of your HLA markers. For some people a transplant from a half-matched donor, or a haploidentical transplant, is a treatment option.
If you have brothers or sisters that share your same mom and dad, your transplant team may ask to test their HLA. It is very unlikely that extended family members, such as cousins, aunts and uncles, will be a match for you. It is extremely unlikely that a friend or neighbor will match you. Ask your doctor who in your family should be tested. If your friends and family members are willing to help any patient in need, they may be able to help in other ways.
About 70% of patients (7 out of 10) who need a transplant don’t have a close match in their family. If you don’t have a match in your family, your doctor will search the Be The Match Registry (https://bethematch.org/) for an unrelated donor or umbilical cord blood. Finding a donor can take time, so your doctor should start a donor search as soon as possible. Your doctor can look for a donor even if you don’t need a transplant right away.
- Pros of allogeneic stem cell transplant
The donor stem cells make their own immune cells, which could help kill any cancer cells that remain after high-dose treatment. This is called the graft-versus-cancer effect. Other advantages are that the donor can often be asked to donate more stem cells or even white blood cells if needed, and stem cells from healthy donors are free of cancer cells.
- Cons to allogeneic stem cell transplants
The transplant, or graft, might not take – that is, the transplanted donor stem cells could die or be destroyed by the patient’s body before settling in the bone marrow. Another risk is that the immune cells from the donor may not just attack the cancer cells – they could attack healthy cells in the patient’s body. This is called graft-versus-host disease. There is also a very small risk of certain infections from the donor cells, even though donors are tested before they donate. A higher risk comes from infections you had previously, and which your immune system has had under control. These infections may surface after allogeneic transplant because your immune system is held in check (suppressed) by medicines called immunosuppressive drugs. Such infections can cause serious problems and even death.
Rules for HLA matching
There are rules for the minimum, or lowest, HLA match needed between a donor and patient. Research shows that patients have better outcomes (results) with a closely matched donor. Sometimes doctors want to match 8 HLA markers. Other times, doctors want to match 10 markers. These are a few matching rules:
- Be The Match (https://bethematch.org/) requires that patients and donors from the Be The Match Registry® match at least 6 of 8 HLA markers.
- For a haploidentical (half-matched) transplant, donors match exactly half, or 5 of 10, HLA markers. The donor is usually the patient’s parent or child.
- An Umbilical Cord Blood Unit must match at least 4 of 6 markers.
Different transplant centers may have different matching rules. Ask your transplant team what the minimum HLA match is at your center.
Doctors keep learning more about better ways to match donors. Today, fewer tests may be needed for siblings, since their cells vary less than an unrelated donor. But to reduce the risks of mismatched types between unrelated donors, more than the basic 6 HLA antigens may be tested. For example, sometimes doctors to try and get a 10 out of 10 match. Certain transplant centers now require high-resolution matching, which looks more deeply into tissue types and allow more specific HLA matching.
There are thousands of different combinations of possible HLA tissue types. This can make it hard to find an exact match. HLA antigens are inherited from both parents. If possible, the search for a donor usually starts with the patient’s brothers and sisters (siblings), who have the same parents as the patient. The chance that any one sibling would be a perfect match (that is, that you both received the same set of HLA antigens from each of your parents) is 1 out of 4.
If a sibling is not a good match, the search could then move on to relatives who are less likely to be a good match – parents, half siblings, and extended family, such as aunts, uncles, or cousins. (Spouses are no more likely to be good matches than other people who are not related.) If no relatives are found to be a close match, the transplant team will widen the search to the general public.
As unlikely as it seems, it’s possible to find a good match with a stranger. To help with this process, the team will use transplant registries, like those listed here. Registries serve as matchmakers between patients and volunteer donors. They can search for and access millions of possible donors and hundreds of thousands of cord blood units.
- Be the Match (https://bethematch.org/)
- Blood & Marrow Transplant Information Network (https://www.bmtinfonet.org/)
How long does it take to find a donor or cord blood unit for transplant?
Every patient’s search is different. For many patients, the donor search takes as little as 1-2 weeks from the time a donor testing request is made until the lab has the blood sample and HLA typing results. Sometimes it can take longer including some searches that may require multiple rounds of donor selections. It usually takes about 3 months from when a transplant team starts to search for a donor or cord blood unit until the day of transplant.
The chances of finding an unrelated donor match improve each year, as more volunteers sign up. Today, about half of white people who need a stem cell transplant may find a perfect match among unrelated donors. This drops to about 1 out of 10 people in other ethnic groups, mostly because their HLA types are more diverse and in the past they were less likely to take part in donor registries. Depending on a person’s tissue typing, several other international registries also are available. Sometimes the best matches are found in people with a similar racial or ethnic background. Finding an unrelated donor can take months, though cord blood may be a little faster. A single match can require going through millions of records.
Now that transplant centers are more often using high-resolution tests, matching is becoming more complex. Perfect 10 out of 10 matches at that level are much harder to find. But transplant teams are also getting better at figuring out what kinds of mismatches can be tolerated in which particular situations – that is, which mismatched antigens are less likely to affect transplant success and survival.
Keep in mind that there are stages to this process – there may be several matches that look promising but don’t work out as hoped. The team and registry will keep looking for the best possible match for you. If your team finds an adult donor through a transplant registry, the registry will contact the donor to set up the final testing and donation. If your team finds matching cord blood, the registry will have the cord blood sent to your transplant center.
How do I find out how my bone marrow donor search is going?
Contact your transplant team. They will keep you up to date on how your search is going. They have the most accurate and up-to-date information for you.
What if there are no perfectly matched donors or cord blood units for me?
Donors and cord blood units do not have to be perfectly matched for transplant to work well. Many patients have done well after transplant from a partially matched donor or cord blood unit. Ask your transplant team how closely matched your donor must be.
Will I get to meet my bone marrow donor?
If you have an unrelated donor, you won’t know who your donor is on transplant day. There are privacy rules in place to protect you and your donor. But, there are some ways you may be able to contact your donor after transplant.
If you have a cord blood transplant, you will never have any contact with the person who donated the cord blood.
Hematopoietic stem cells collection process
Stem cells used in bone marrow transplants are collected from donors in several ways. A procedure called apheresis may be used. For this procedure, a needle is placed in the donor’s arm to draw blood. Then, his or her blood is passed through a machine that removes the stem cells from the blood. The rest of the blood is returned to the donor.
Stem cells may be collected directly from a donor’s pelvis using a procedure called bone marrow aspiration. This procedure isn’t used very much anymore because it must be done in a hospital using local or general anesthesia. For this procedure, a hollow needle is inserted repeatedly into the pelvis, and marrow is sucked out of the bone.
Blood containing stem cells may be collected from an umbilical cord and placenta after a baby is born. The blood is frozen and stored at a cord blood bank for future use.
What is a haploidentical transplant?
A haploidentical transplant is a type of allogeneic transplant. It uses healthy, blood-forming cells from a half- matched donor to replace the unhealthy ones. The donor is typically a family member.
For allogeneic transplants, your doctor tests your blood to find out your human leukocyte antigen (HLA) type. HLA is a protein — or marker — found on most cells in your body. Doctors look for a donor or umbilical cord blood that closely matches your HLA.
But sometimes they can’t find a close HLA match. Then, a haploidentical transplant may be an option. This is a type of allogeneic transplant where the donor matches exactly half of your HLA.
A haploidentical, or half-matched, donor is usually your mom, your dad or your child. Parents are always a half-match for their children. Siblings (brothers or sisters) have a 50% (1 out of 2) chance of being a half-match for each other. It’s very unlikely that other family members (like cousins, aunts or uncles) would be a half-match.
A haploidentical transplant is a newer type of transplant. This means:
- You may have the option to join a clinical trial (research study).
- Not all transplant centers will do this type of transplant.
What is a “mini-transplant”?
A “mini-transplant” (also called a non-myeloablative or reduced-intensity transplant) is a type of allogeneic transplant. This approach is being studied in clinical trials for the treatment of several types of cancer, including leukemia, lymphoma, multiple myeloma, and other cancers of the blood.
A mini-transplant uses lower, less toxic doses of chemotherapy and/or radiation to prepare the patient for an allogeneic transplant. The use of lower doses of anticancer drugs and radiation eliminates some, but not all, of the patient’s bone marrow. It also reduces the number of cancer cells and suppresses the patient’s immune system to prevent rejection of the transplant.
Unlike traditional bone marrow transplantation or peripheral blood stem cell transplantation, cells from both the donor and the patient may exist in the patient’s body for some time after a mini-transplant. Once the cells from the donor begin to engraft, they may cause the graft-versus-tumor effect and work to destroy the cancer cells that were not eliminated by the anticancer drugs and/or radiation. To boost the graft-versus-tumor effect, the patient may be given an injection of the donor’s white blood cells. This procedure is called a “donor lymphocyte infusion.”
Syngeneic stem cell transplants – for those with an identical sibling
This is a special kind of allogeneic transplant that can only be used when the patient has an identical sibling (twin or triplet) – someone who has the exact same tissue type. An advantage of syngeneic stem cell transplant is that graft-versus-host disease will not be a problem. Also, there are no cancer cells in the transplanted stem cells, as there might be in an autologous transplant.
A disadvantage is that because the new immune system is so much like the recipient’s immune system, there’s no graft-versus-cancer effect. Every effort must be made to destroy all the cancer cells before the transplant is done to help keep the cancer from coming back.
Diseases treated by bone marrow transplant
A bone marrow transplant, also called a blood stem cell transplant, can treat many diseases. For some diseases, bone marrow transplant is the only potential cure. There are over 70 diseases that can be treated by bone marrow transplant. Some of them are listed here:
- Acute lymphoblastic leukemia (ALL)
- Acute myeloid leukemia (AML)
- Adrenoleukodystrophy
- Chronic lymphocytic leukemia (CLL)
- Chronic myelogenous leukemia (CML)
- Hodgkin lymphoma
- Hurler syndrome
- Krabbe disease (Globoid-Cell Leukodystrophy)
- Metachromatic Leukodystrophy
- Multiple myeloma
- Myelodysplastic syndromes (MDS)
- Non-Hodgkin lymphoma (NHL)
- Severe aplastic anemia
- Severe Combined Immunodeficiency
- Sickle cell disease
- Wiskott-Aldrich syndrome
- Other diseases
How do patients cover the cost of bone marrow transplantation?
Stem cell transplants cost a lot – some estimates say $350,000 to $800,000. Advances in treatment methods, including the use of peripheral blood stem cell transplantation, have reduced the amount of time many patients must spend in the hospital by speeding recovery. This shorter recovery time has brought about a reduction in cost. However, because bone marrow transplantation and peripheral blood stem cell transplantation are complicated technical procedures, they are very expensive. Many health insurance companies cover some of the costs of transplantation for certain types of cancer. Insurers may also cover a portion of the costs if special care is required when the patient returns home.
There are options for relieving the financial burden associated with bone marrow transplantation and peripheral blood stem cell transplantation. A hospital social worker is a valuable resource in planning for these financial needs. Federal government programs and local service organizations may also be able to help.
- National Cancer Institute’s Cancer Information Service can provide patients and their families with additional information about sources of financial assistance at 1–800–422–6237 (https://www.cancer.gov/contact).
These organizations can also help you plan your fundraising campaign:
- The Bone Marrow Foundation (http://bonemarrow.org/)
- Children’s Organ Transplant Association (https://cota.org/)
- HelpHOPELive (https://helphopelive.org)
- National Foundation for Transplants (https://transplants.org/)
You may find other online tools to help fundraise, too. This is called crowdfunding and may be helpful for those who use social media.
How much money will it cost me to find bone marrow donor?
The search costs are different for each patient. The costs depend on health insurance coverage, how many donors need to be tested, and where the donors live. Transplant centers may charge for the search differently too. Ask your transplant center’s financial coordinator what your costs might be.
Financial grants are available to help cover some of your transplant costs. Learn more about financial grants and how to apply at Be The Match® (https://bethematch.org/).
What are the costs of donating bone marrow, peripheral blood stem cells, or umbilical cord blood?
All medical costs for the donation procedure are covered by Be The Match® (https://bethematch.org/), or by the patient’s medical insurance, as are travel expenses and other non-medical costs. The only costs to the donor might be time taken off from work.
A woman can donate her baby’s umbilical cord blood to public cord blood banks at no charge. However, commercial blood banks do charge varying fees to store umbilical cord blood for the private use of the patient or his or her family.
Where can people get more information about potential donors and transplant centers?
The National Marrow Donor Program® (https://bethematch.org/), a nonprofit organization, manages the world’s largest registry of more than 11 million potential donors and cord blood units. The National Marrow Donor Program® (https://bethematch.org/) operates Be The Match®, which helps connect patients with matching donors.
A list of U.S. transplant centers that perform allogeneic transplants can be found at Be The Match® (https://bethematch.org/). The list includes descriptions of the centers, their transplant experience, and survival statistics, as well as financial and contact information.
How does a bone marrow transplant work
Bone marrow transplantation and peripheral blood stem cell transplantation are procedures that restore hematopoietic stem cells that have been destroyed by high doses of chemotherapy and/or radiation therapy. Before a bone marrow transplant, you get chemotherapy (chemo) with or without radiation to destroy the diseased blood-forming cells and marrow. Then, healthy cells are given to you (similar to blood transfusion). The new hematopoietic stem cells go into your bloodstream through an intravenous (IV) line, or tube. It’s just like getting blood or medicine through an IV. The hematopoietic stem cells find their way into your marrow, where they grow and start to make healthy red blood cells, white blood cells and platelets.
One reason bone marrow transplantation and peripheral blood stem cell transplantation are used in cancer treatment is to make it possible for patients to receive very high doses of chemotherapy and/or radiation therapy. To understand more about why bone marrow transplantation and peripheral blood stem cell transplantation are used, it is helpful to understand how chemotherapy and radiation therapy work.
Chemotherapy and radiation therapy generally affect cells that divide rapidly. They are used to treat cancer because cancer cells divide more often than most healthy cells. However, because bone marrow cells also divide frequently, high-dose treatments can severely damage or destroy the patient’s bone marrow. Without healthy bone marrow, the patient is no longer able to make the blood cells needed to carry oxygen, fight infection, and prevent bleeding. Bone marrow transplantation and peripheral blood stem cell transplantation replace stem cells destroyed by treatment. The healthy, transplanted hematopoietic stem cells can restore the bone marrow’s ability to produce the blood cells the patient needs.
In some types of leukemia, the graft-versus-tumor effect that occurs after allogeneic bone marrow transplantation and peripheral blood stem cell transplantation is crucial to the effectiveness of the treatment. Graft-versus-tumor occurs when white blood cells from the donor (the graft) identify the cancer cells that remain in the patient’s body after the chemotherapy and/or radiation therapy (the tumor) as foreign and attack them.
What types of cancer are treated with bone marrow transplantation and peripheral blood stem cell transplantation?
Bone marrow transplantation and peripheral blood stem cell transplantation are most commonly used in the treatment of leukemia and lymphoma. They are most effective when the leukemia or lymphoma is in remission (the signs and symptoms of cancer have disappeared). Bone marrow transplantation and peripheral blood stem cell transplantation are also used to treat other cancers such as neuroblastoma (cancer that arises in immature nerve cells and affects mostly infants and children) and multiple myeloma. Researchers are evaluating bone marrow transplantation and peripheral blood stem cell transplantation in clinical trials (research studies) for the treatment of various types of cancer.
How are the donor’s stem cells matched to the patient’s stem cells in allogeneic or syngeneic transplantation?
To minimize potential side effects, doctors most often use transplanted hematopoietic stem cells that match the patient’s own stem cells as closely as possible. People have different sets of proteins, called human leukocyte antigens (HLA), on the surface of their cells. The set of proteins, called the HLA type, is identified by a special blood test.
In most cases, the success of allogeneic transplantation depends in part on how well the HLA antigens of the donor’s stem cells match those of the recipient’s stem cells. The higher the number of matching HLA antigens, the greater the chance that the patient’s body will accept the donor’s stem cells. In general, patients are less likely to develop a complication known as graft-versus-host disease if the stem cells of the donor and patient are closely matched.
Close relatives, especially brothers and sisters, are more likely than unrelated people to be HLA-matched. However, only 25 to 35 percent of patients have an HLA-matched sibling. The chances of obtaining HLA-matched stem cells from an unrelated donor are slightly better, approximately 50 percent. Among unrelated donors, HLA-matching is greatly improved when the donor and recipient have the same ethnic and racial background. Although the number of donors is increasing overall, individuals from certain ethnic and racial groups still have a lower chance of finding a matching donor. Large volunteer donor registries can assist in finding an appropriate unrelated donor.
Because identical twins have the same genes, they have the same set of HLA antigens. As a result, the patient’s body will accept a transplant from an identical twin. However, identical twins represent a small number of all births, so syngeneic transplantation is rare.
How is bone marrow obtained for transplantation?
The stem cells used in bone marrow transplantation come from the liquid center of the bone, called the marrow. In general, the procedure for obtaining bone marrow, which is called “harvesting,” is similar for all three types of bone marrow transplantations (autologous, syngeneic, and allogeneic). The donor is given either general anesthesia, which puts the person to sleep during the procedure, or regional anesthesia, which causes loss of feeling below the waist. Needles are inserted through the skin over the pelvic (hip) bone or, in rare cases, the sternum (breastbone), and into the bone marrow to draw the marrow out of the bone. Harvesting the marrow takes about an hour.
The harvested bone marrow is then processed to remove blood and bone fragments. Harvested bone marrow can be combined with a preservative and frozen to keep the stem cells alive until they are needed. This technique is known as cryopreservation. Stem cells can be cryopreserved for many years.
Are there any risks associated with bone marrow transplant donor?
Because only a small amount of bone marrow is removed, donating usually does not pose any significant problems for the donor. The most serious risk associated with donating bone marrow involves the use of anesthesia during the procedure.
The area where the bone marrow was taken out may feel stiff or sore for a few days, and the donor may feel tired. Within a few weeks, the donor’s body replaces the donated marrow; however, the time required for a donor to recover varies. Some people are back to their usual routine within 2 or 3 days, while others may take up to 3 to 4 weeks to fully recover their strength.
How are peripheral blood stem cells obtained for transplantation?
The stem cells used in peripheral blood stem cell transplantation come from the bloodstream. A process called apheresis or leukapheresis is used to obtain peripheral blood stem cells for transplantation. For 4 or 5 days before apheresis, the donor may be given a medication to increase the number of stem cells released into the bloodstream. In apheresis, blood is removed through a large vein in the arm or a central venous catheter (a flexible tube that is placed in a large vein in the neck, chest, or groin area). The blood goes through a machine that removes the stem cells. The blood is then returned to the donor and the collected cells are stored. Apheresis typically takes 4 to 6 hours. The stem cells are then frozen until they are given to the recipient.
Are there any risks associated with donating peripheral blood stem cells?
Apheresis usually causes minimal discomfort. During apheresis, the person may feel lightheadedness, chills, numbness around the lips, and cramping in the hands. Unlike bone marrow donation, peripheral blood stem cell donation does not require anesthesia. The medication that is given to stimulate the mobilization (release) of stem cells from the marrow into the bloodstream may cause bone and muscle aches, headaches, fatigue, nausea, vomiting, and/or difficulty sleeping. These side effects generally stop within 2 to 3 days of the last dose of the medication.
How are umbilical cord stem cells obtained for transplantation?
Stem cells also may be retrieved from umbilical cord blood. For this to occur, the mother must contact a cord blood bank before the baby’s birth. The cord blood bank may request that she complete a questionnaire and give a small blood sample.
Cord blood banks may be public or commercial. Public cord blood banks accept donations of cord blood and may provide the donated stem cells to another matched individual in their network. In contrast, commercial cord blood banks will store the cord blood for the family, in case it is needed later for the child or another family member.
After the baby is born and the umbilical cord has been cut, blood is retrieved from the umbilical cord and placenta. This process poses minimal health risk to the mother or the child. If the mother agrees, the umbilical cord blood is processed and frozen for storage by the cord blood bank. Only a small amount of blood can be retrieved from the umbilical cord and placenta, so the collected stem cells are typically used for children or small adults.
Bone marrow transplant procedure
The blood and marrow transplant process is different for everyone. Your path will depend on many things such as the type of transplant, your overall health and your disease. Your transplant team will always be there to guide and support you. The entire transplant process, from the start of chemo and sometimes radiation, until hospital discharge, can last weeks to months. This is followed by many months of recovery near the transplant center and at home. The transplant team will closely care for you to prevent and treat any complications.
Blood or bone marrow transplants are usually performed in a hospital. Often, you must stay in the hospital for one to two weeks before the bone marrow transplant to prepare. During this time, you will have a narrow tube placed in one of your large veins in your chest or neck. You may be given medicine to make you sleepy for this procedure. You also will receive special medicines (high-dose anticancer drugs) and possibly radiation to destroy your abnormal stem cells and to weaken your immune system so that it won’t reject the donor cells after the transplant.
Figure 4. Bone marrow transplant process
Before bone marrow transplant
Many things happen in the days and weeks before transplant. You will:
- Have a checkup to make sure your body is healthy enough for transplant.
- Get a central line if you don’t already have one.
- Receive chemotherapy (chemo), and possibly radiation, to prepare your body for transplant. This is also called the preparative or conditioning regimen.
Schedule
The number of days you receive the preparative regiment will depend on the type of regimen. The days you receive the preparative regimen are called “minus” days (or –days). Some patients may receive the regimen for an entire week while others may only receive it for a few days. This part of the transplant process is the “countdown” to “Day Zero” — the day you receive the new cells from your donor.
The cells for your transplant are collected before transplant day.
- Autologous transplant – You get your own cells. The cells are collected from your bloodstream or your bone marrow.
- Allogeneic transplant – You get cells from a family member or unrelated donor. The cells are collected from the person’s bloodstream or bone marrow. They can also be from an umbilical cord blood collected from the umbilical cord after a baby is born.
Conditioning regimen (chemo and/or radiation therapy)
Conditioning, also known as bone marrow preparation or myeloablation, is treatment with high-dose chemo and/or radiation therapy. It’s the first step in the transplant process and typically takes a week or two. It’s done for one or more of these reasons:
- To make room in the bone marrow for the transplanted stem cells
- To suppress the patient’s immune system to lessen the chance of graft rejection
- To destroy any remaining cancer cells in the patient’s body
The conditioning treatment is different for every transplant. Your treatment will be planned based on the type of cancer you have, the type of transplant, and any chemo or radiation therapy you’ve had in the past.
If chemo is part of your treatment plan, it will be given in your central venous catheter and/or as pills. If radiation therapy is planned, it’s given to the entire body (called total body irradiation or TBI). Total body irradiation may be given in a single treatment session or in divided doses over a few days.
This phase of the transplant can be very uncomfortable because very high treatment doses are used. Chemo and radiation side effects can make you sick, and it may take you months to fully recover. A very common problem is mouth sores that will need to be treated with strong pain medicines. You may also have nausea, vomiting, be unable to eat, lose your hair, and have lung or breathing problems.
Conditioning can also cause premature menopause in women and often makes both men and women sterile (unable to have children).
Allogeneic preparative regimens
There are 2 main types of preparative regimens:
- Standard-intensity regimen: Uses high doses of chemo, with or without high doses of radiation. Also called a myeloablative regimen.
- Reduced-intensity regimen: Uses a lower dose of chemo, with or without lower doses of radiation. Also called a non-myeloablative regimen.
Your doctor will choose the type of preparative regimen for you based on your disease and overall health.
Autologous preparative regimens
For this type of transplant, you get higher doses of chemo (with or without radiation) than you would get if you weren’t getting a transplant. The higher doses may cause more severe side effects, but they also destroy more diseased cells.
How is a bone marrow transplant done
On the day of the transplant (transplant day 0 or “Day Zero”) usually comes 1 or 2 days after you finish the preparative regimen (see above), you will be awake and may get medicine to relax you during the procedure. The stem cells will be given to you through an intravenous (IV) line through your central line that was placed into a large vein in your chest or neck, just like a blood transfusion. The hematopoietic stem cells come in blood bags, similar to the ones used for blood transfusions. This part of the transplant takes 1 to 5 hours. The hematopoietic stem cells will travel through your blood to your bone marrow, where they will begin making new healthy blood cells.
You will be awake for this process, and it doesn’t hurt. This is a big step and often has great meaning for recipients and their families. Many people consider this their rebirth or chance at a second life. They may celebrate this day as they would their actual birthday.
After the bone marrow transplant, your doctor will check your blood counts every day to see if new blood cells have started to grow in your bone marrow. Depending on the type of transplant, you may be able to leave, but stay near the hospital, or you may need to remain in the hospital for weeks or months. The length of time will depend on how your immune system is recovering and whether or not the transplanted cells stay in your body. Before you leave the hospital, the doctors will give you detailed instructions that you must follow to prevent infection and other complications. Your doctor will keep monitoring your recovery, possibly for up to one year.
Although blood or bone marrow transplant is an effective treatment for some conditions, the procedure can cause early or late complications. The required medicines and radiation can cause nausea, vomiting, diarrhea, tiredness, mouth sores, skin rashes, hair loss, or liver damage. These treatments also can weaken your immune system and increase your risk for infection. Some people may experience a serious complication called graft-versus-host disease if the donated stem cells attack the body. Other people may reject the donor stem cells after the transplant, which can be an extremely serious complication.
Are any special measures taken when the cancer patient is also the donor (autologous transplant)?
The stem cells used for autologous transplantation must be relatively free of cancer cells. The harvested cells can sometimes be treated before transplantation in a process known as “purging” to get rid of cancer cells. This process can remove some cancer cells from the harvested cells and minimize the chance that cancer will come back. Because purging may damage some healthy stem cells, more cells are obtained from the patient before the transplant so that enough healthy stem cells will remain after purging.
What happens after the stem cells have been transplanted to the patient?
After entering the bloodstream, the stem cells travel to the bone marrow, where they begin to produce new white blood cells, red blood cells, and platelets in a process known as “engraftment.” Engraftment usually occurs within about 2 to 4 weeks after transplantation. Doctors monitor it by checking blood counts on a frequent basis. Complete recovery of immune function takes much longer, however—up to several months for autologous transplant recipients and 1 to 2 years for patients receiving allogeneic or syngeneic transplants. Doctors evaluate the results of various blood tests to confirm that new blood cells are being produced and that the cancer has not returned. Bone marrow aspiration (the removal of a small sample of bone marrow through a needle for examination under a microscope) can also help doctors determine how well the new marrow is working.
Bone marrow transplant infusion side effects
Side effects from the infusion are rare and usually mild. The preserving agent used when freezing the stem cells (called dimethylsulfoxide or DMSO) causes many of the side effects. For instance, you might have a strong taste of garlic or creamed corn in your mouth. Sucking on candy or sipping flavored drinks during and after the infusion can help with the taste. Your body will also smell like this. The smell may bother those around you, but you might not even notice it. The smell, along with the taste, may last for a few days, but slowly fades away. Often having cut up oranges in the room will offset the odor. Patients who have transplants from cells that were not frozen do not have this problem because the cells are not mixed with the preserving agent.
Other side effects you might have during and right after the stem cell infusion include:
- Fever or chills
- Shortness of breath
- Hives
- Tightness in the chest
- Low blood pressure
- Coughing
- Chest pain
- Less urine output
- Feeling weak
Again, side effects are rare and usually mild. If they do happen, they are treated as needed. The stem cell infusion must always be completed.
Recovery after bone marrow transplant infusion
The recovery stage begins after the stem cell infusion. During this time, you and your family wait for the cells to engraft, or “take,” after which they start to multiply and make new blood cells. The time it takes to start seeing a steady return to normal blood counts varies depending on the patient and the transplant type, but it’s usually about 2 to 6 weeks. You’ll be in the hospital or visit the transplant center daily for at least a few weeks.
During the first couple of weeks you’ll have low numbers of red and white blood cells and platelets. Right after transplant, when your counts are the lowest, you may be given antibiotics to help keep you from getting infections. (This is called prophylactic antibiotics.) You may get a combination of anti-bacterial, anti-fungal, and anti-viral drugs. These are usually given until your white blood cell count reaches a certain level. Still, you can have problems, such as infection from too few white blood cells (neutropenia), or bleeding from too few platelets (thrombocytopenia). Many patients have high fevers and need IV antibiotics to treat serious infections. Transfusions of red blood cells and platelets are often needed until the bone marrow starts working and new blood cells are being made by the infused stem cells.
Except for graft-versus-host disease, which only happens with allogeneic transplants, the side effects from autologous, allogeneic, and syngeneic stem cell transplants are much the same. Problems may include stomach, heart, lung, liver, or kidney problems. You might also go through feelings of distress, anxiety, depression, joy, or anger. Adjusting emotionally after the stem cells can be hard because of the length of time you feel ill and isolated from others.
You might feel as if you are on an emotional roller coaster during this time. Support and encouragement from family, friends, and the transplant team are very important to get you through the challenges after transplant.
Discharge from the hospital
Planning to go home
The discharge process actually begins weeks before your transplant. It starts with the transplant team teaching you and your primary (main) caregiver about:
- The precautions you’ll need to take
- Who will be your primary caregiver and what the job will be like, and who will be the back-up caregiver in case your main caregiver gets sick and can’t be near you
- How to prepare your home
- How to care for your central venous catheter
- How to take good care of your mouth and teeth
- What foods you should and shouldn’t eat
- Activities you can and can’t do
- When to call the transplant team or other health care providers
What has to happen before you can go home?
For the most part, transplant centers don’t send patients home until they meet the following criteria (neutrophils, platelets, and hematocrit):
- No fever for 48 hours
- Able to take and keep down pills or other drugs for 48 hours
- Nausea, vomiting, and diarrhea are controlled with medicine
- Neutrophil count (absolute neutrophil count or ANC) is at least 500 to 1,000/mm3
- Hematocrit is at least 25% to 30%
- Platelet count is at least 15,000 to 20,000/mm3
- They have someone to help them at home and a safe and supportive home environment
If you do not meet all of these requirements, but still don’t need the intensive care of the transplant unit, you might be moved to another oncology unit. When you do go home, you might need to stay near the transplant center for some time, depending on your condition.
Rehabilitation
The process of stem cell transplant doesn’t end when you go home. You’ll feel tired, and some people have physical or mental health problems in the rehabilitation period. You might still be taking a lot of medicines. These ongoing needs must now be managed at home, so caregiver and friend/family support is very important.
Transplant patients are still followed closely during rehab. You might need daily or weekly exams along with things like blood tests, and maybe other tests, too. During early rehab, you also might need blood and platelet transfusions, antibiotics, or other treatments. At first you’ll need to see your transplant team often, maybe even every day, but you’ll progress to less frequent visits if things are going well. It can take 6 to 12 months, or even longer, for blood counts to get close to normal and your immune system to work well. During this time, your team will still be closely watching you.
Some problems might show up as much as a year or more after the stem cells were infused. They can include:
- Graft-versus-host disease (in allogeneic transplants)
- Infections
- Lung problems, such as pneumonia or inflammation that makes it hard to breathe
- Kidney, liver, or heart problems
- Low thyroid function
- Overwhelming tiredness (fatigue)
- Limited ability to exercise
- Slowed growth and development (in children)
- Cataracts
- Reproductive or sexual problems, like infertility, early menopause, pain or discomfort during sex, or loss of interest in sex
- New cancers caused by the transplant
Other problems can also come up, such as:
- Memory loss, trouble concentrating
- Emotional distress, depression, body image changes, anxiety
- Social isolation
- Changes in relationships
- Changes in how you view the meaning of life
- Feeling indebted to others
- Job and insurance discrimination
Your transplant team is still there to help you. It’s important that you talk to them about any problems you are having – they can help you get the support you need to manage the changes that you are going through. They can also help you know if problems are serious, or a normal part of recovery. The National Bone Marrow Transplant Link helps patients, caregivers, and families by providing information and support services before, during, and after transplant. They can be reached at 1-800-546-5268 or online at http://www.nbmtlink.org/
Bone marrow transplant risks
The likelihood and severity of complications are specific to the patient’s treatment and should be discussed with the patient’s doctor. The major risk of both bone marrow transplantation and peripheral blood stem cell transplantation treatments is an increased susceptibility to infection and bleeding as a result of the high-dose cancer treatment. Doctors may give the patient antibiotics to prevent or treat infection. They may also give the patient transfusions of platelets to prevent bleeding and red blood cells to treat anemia. Patients who undergo bone marrow transplantation and peripheral blood stem cell transplantation may experience short-term side effects such as nausea, vomiting, fatigue, loss of appetite, mouth sores, hair loss, and skin reactions.
Side effects of the pretransplant chemotherapy and radiation therapy
Many of the problems that can happen shortly after the transplant come from having the bone marrow wiped out by medicines or radiation just before the transplant from your preparative regimen. Others may be side effects of the conditioning treatments themselves.
Some may last a few days. Others can last longer. Your transplant team will treat your side effects and help keep you comfortable.
Some common side effects are:
- Fatigue (feeling tired)
- Nausea
- Vomiting (throwing up)
- Diarrhea
- Lack of appetite
- Mouth sores
- Hair loss
- Skin rash
Mouth and throat pain
Mucositis (inflammation or sores in the mouth) is a short-term side effect that can happen with chemo and radiation. It usually gets better within a few weeks after treatment, but it can make it very painful to eat and drink.
Good nutrition is important for people with cancer. If mouth pain or sores make it hard to eat or swallow, your transplant team will help you develop a plan to manage your symptoms.
Nausea and vomiting
Because chemotherapy drugs can cause severe nausea and vomiting, doctors often give anti-nausea medicines at the same time as chemo to try and prevent it. As much as possible, the goal is to prevent nausea and vomiting, because it’s easier to prevent it than it is to stop it once it starts. Preventive treatment should start before the chemotherapy is given and should continue for as long as the chemo is likely to cause vomiting, which can be up to 7 to 10 days after the last dose.
No one drug can prevent or control chemo-related nausea and vomiting 100% of the time. In many cases, two or more medicines are used. You’ll need to tell your transplant team how well the medicines are controlling your nausea and vomiting. If they aren’t working, they will need to be changed.
Infection
During about the first 6 weeks after transplant, until the new stem cells start making white blood cells (engraftment), you can easily get serious infections. Bacterial infections are most common during this time, but viral infections that were controlled by your immune system can become active again. Fungal infections can also be an issue. And even infections that cause only mild symptoms in people with normal immune systems can be quite dangerous for you.
You may be given antibiotics to try to prevent infections until your blood counts reach a certain level. For instance, pneumocystis pneumonia (often called PCP) is a common infection that’s easy to catch. Even though the germ doesn’t harm people with normal immune systems, for others it can cause fever, cough, and serious breathing problems. Antibiotics are often used to keep transplant patients from getting this.
Your doctor may check you before the transplant for signs of certain infections that may become active after transplant, and give you special medicines to keep those germs under control. For example, the virus called CMV (cytomegalovirus) is a common cause of pneumonia in people who have had transplants. It mainly happens to people who were already infected with cytomegalovirus, or whose donor had the virus. If neither you nor your donor had cytomegalovirus, the transplant team might follow special precautions to prevent infection while you are in the hospital.
After engraftment, the risk of infection is lower, but it still can happen. It takes 6 months to a year after transplant for the immune systems of most patients to work as well as they should. It can take even longer for patients with graft-versus-host disease (GVHD, see below).
Because of the increased risk, you will be watched closely for signs of infection, such as fever, cough, shortness of breath, or diarrhea. Your doctor may check your blood often, and extra precautions will be needed to avoid exposure to germs. While in the hospital, everyone who enters your room must wash their hands well. They may also wear gowns, shoe coverings, gloves, and masks.
Since flowers and plants can carry bacteria and fungi, they’re not allowed in your room. For the same reason, you may be told not to eat certain fresh fruits and vegetables. All your food must be well cooked and handled very carefully by you and family members. Certain foods may need to be avoided for a while.
You may also be told to avoid contact with soil, feces (stool, both human and animal), aquariums, reptiles, and exotic pets. Your team may tell you to avoid being near disturbed soil, bird droppings, or mold. You will need to wash your hands after touching pets. Your family may need to move the cat’s litter box away from places you eat or spend your time.
Your transplant team will tell you and your family in detail about the precautions you need to follow. There are many viruses, bacteria, and fungi that can cause infection after your transplant.
Despite all these precautions, patients often develop fevers, one of the first signs of infection. If you do get a fever or other signs of infection, contact your doctor right away. Tests will be done to look for the cause of the infection (chest x-rays, urine tests, and blood cultures) and antibiotics will be started.
Bleeding and transfusions
After transplant, you’re at risk for bleeding because the conditioning treatment destroys your body’s ability to make platelets. (Platelets are the blood cells that help blood to clot.) While you wait for your transplanted stem cells to start working, your transplant team may have you follow special precautions to avoid injury and bleeding.
Platelet counts are low for at least 3 weeks after transplant. In the meantime, you might notice easy bruising and bleeding, such as nosebleeds and bleeding gums. If your platelet count drops below a certain level, a platelet transfusion may be needed. You’ll need to follow precautions until your platelet counts stay at safe levels.
It also takes time for your bone marrow to start making red blood cells, and you might need red blood cell transfusions from time to time as you recover.
Interstitial pneumonitis and other lung problems
Pneumonitis is a type of lung inflammation that’s most common in the first 100 days after transplant. But some lung problems can happen much later – even 2 or more years after transplant.
Pneumonia caused by infection happens more often, but pneumonitis may be caused by radiation, graft-versus-host disease, or chemo rather than germs. It’s caused by damage to the areas between the cells of the lungs (called interstitial spaces).
Pneumonitis can be severe, especially if total body irradiation was given with chemo as part of the conditioning treatment. Chest x-rays will be taken in the hospital to watch for pneumonitis as well as pneumonia. Some doctors will do breathing tests every few months if you have graft-versus-host disease (see next section).
You should report any shortness of breath or changes in your breathing to your doctor or transplant team right away. There are many other types of lung and breathing problems that also need to be handled quickly.
Graft-versus-host disease
With allogeneic transplants, graft-versus-host disease sometimes develops when white blood cells from the donor (the graft) identify cells in the patient’s body (the host) as foreign and attack them. Graft-versus-host disease reactions are very common and can range from barely noticeable to life-threatening. Doctors think of graft-versus-host disease as acute or chronic. Acute graft-versus-host disease starts soon after transplant and lasts a short time. Chronic graft-versus-host disease starts later and lasts a long time. A person could have one, both, or neither type of graft-versus-host disease. The most commonly damaged organs are the skin, liver, and intestines. This complication can develop within a few weeks of the transplant (acute graft-versus-host disease) or much later (chronic graft-versus-host disease). To prevent this complication, the patient may receive medications that suppress the immune system. Additionally, the donated stem cells can be treated to remove the white blood cells that cause graft-versus-host disease in a process called “T-cell depletion.” If graft-versus-host disease develops, it can be very serious and is treated with steroids or other immunosuppressive agents. Graft-versus-host disease can be difficult to treat, but some studies suggest that patients with leukemia who develop graft-versus-host disease are less likely to have the cancer come back. Clinical trials are being conducted to find ways to prevent and treat graft-versus-host disease.
Acute graft-versus-host disease
Acute graft-versus-host disease can happen 10 to 90 days after a transplant, though the average time is around 25 days.
About one-third to one-half of allogeneic transplant recipients will develop acute graft-versus-host disease. It’s less common in younger patients and in those with closer HLA matches between donor and recipient.
The first signs are usually a rash, burning, and redness of the skin on the palms and soles. This can spread over the entire body. Other symptoms include:
- Nausea
- Vomiting
- Stomach cramps
- Diarrhea (watery and sometimes bloody)
- Loss of appetite
- Yellowing of the skin and eyes (jaundice)
- Abdominal (belly) pain
- Weight loss
Most cases are mild and can be treated. How well a person does depends on how bad the graft-versus-host disease is. Some cases of graft-versus-host disease can lead to death.
Doctors try to prevent acute graft-versus-host disease by giving drugs, such as steroids, certain monoclonal antibodies, methotrexate, cyclosporine, and tacrolimus to lessen the immune response. These drugs are given before acute graft-versus-host disease starts and can help prevent serious graft-versus-host disease. Still, mild graft-versus-host disease will almost always happen in allogeneic transplant patients. Other drugs in different combinations are being tested for graft-versus-host disease prevention.
The risk of acute graft-versus-host disease can also be lowered by removing a certain kind of immune cells, called T-cells, from the donor stem cells before the transplant. But this can also increase the risk of viral infection, leukemia relapse, and graft failure (which is discussed later). Researchers are looking at new ways to remove only certain cells, called alloactivated T-cells, from donor grafts. This would reduce the severity of graft-versus-host disease and still let the donor T-cells destroy any cancer cells left. Preventing and managing graft-versus-host disease are major priorities for research.
Chronic graft-versus-host disease
Chronic graft-versus-host disease can start anywhere from about 90 to 600 days after the stem cell transplant. A rash on the palms of the hands or the soles of the feet is often the earliest sign. The rash can spread and is usually itchy and dry. In severe cases, the skin may blister and peel, like a bad sunburn. A fever may also develop. Other symptoms of chronic graft-versus-host disease can include:
- Decreased appetite
- Diarrhea
- Abdominal (belly) cramps
- Weight loss
- Yellowing of the skin and eyes (jaundice)
- Enlarged liver
- Bloated abdomen (belly)
- Pain in the upper right part of the abdomen (belly)
- Increased levels of liver enzymes in the blood (seen on blood tests)
- The skin feels tight
- Dry, burning eyes
- Dryness or painful sores in the mouth
- Burning sensations when eating acidic foods
- Bacterial infections
- Blockages in the smaller airways of the lungs
Chronic graft-versus-host disease is treated with medicines that suppress the immune system, much like those used for acute graft-versus-host disease. These drugs can increase your risk of infection for as long as you are treated for graft-versus-host disease. Most patients with chronic graft-versus-host disease can stop the immunosuppressive drugs after their symptoms improve.
Hepatic veno-occlusive disease
Hepatic veno-occlusive disease is a serious problem in which tiny veins and other blood vessels inside the liver become blocked. It’s not common, and it only happens in people with allogeneic transplants, and mainly in those who got the drugs busulfan or melphalan as part of conditioning.
Veno-occlusive disease usually happens within about 3 weeks of conditioning. It’s more common in older people who had liver problems before the transplant, and in those with acute graft-versus-host disease. It starts with yellowing skin and eyes, dark urine, tenderness below the right ribs (this is where the liver is), and quick weight gain (mostly from fluid that bloats the belly). Sometimes it can result in liver failure and death.
Doctors have found that giving busulfan in the vein (IV) rather than by mouth may reduce the risk of VOD. New ways to prevent and treat this problem are being tested.
Graft failure
Grafts fail when the body does not accept the new stem cells (the graft). The stem cells that were given do not go into the bone marrow and multiply like they should. Graft failure is more common when the patient and donor are not well matched and when patients get stem cells that have had the T-cells removed. It can also happen in patients who get a low number of stem cells, such as a single umbilical cord unit. Still, it’s not very common.
Graft failure can lead to serious bleeding and/or infection. It’s suspected in patients whose counts do not start going up within 3 to 4 weeks of a bone marrow or peripheral blood transplant, or within 7 weeks of a cord blood transplant.
It may be treated by a second dose of stem cells, if available. Grafts rarely fail, but if they do it can result in death.
Problems that may show up later
You may have other side effects in the first month after the preparative regimen. Your transplant team will watch you closely and care for you throughout your recovery after transplant.
Potential long-term risks include complications of the pretransplant chemotherapy and radiation therapy, such as infertility (the inability to produce children); cataracts (clouding of the lens of the eye, which causes loss of vision); secondary (new) cancers; and damage to the liver, kidneys, lungs, and/or heart.
Possible long-term risks of bone marrow transplant include:
- Organ damage
- Relapse (the cancer comes back)
- Secondary (new) cancers
- Abnormal growth of lymph tissues
- Infertility (the inability to produce children)
- Hormone changes, such as changes in the thyroid or pituitary gland
- Cataracts (clouding of the lens of the eye, which causes vision loss)
The medicines used in transplants can harm the body’s organs, such as the heart, lungs, kidneys, liver, bones/joints, and nervous system. You may need careful follow-up with close monitoring and treatment of the long-term organ problems that the transplant can cause. Some of these, like infertility, should be discussed before the transplant, so you can prepare for them.
It’s important to find and quickly treat any long-term problems. Tell your doctor right away if you notice any changes or problems. Physical exams by your doctor, blood work, imaging tests, lung/breathing studies, and other tests will help look for and keep tabs on organ problems.
As transplant methods have improved, more people are living longer and doctors are learning more about the long-term results of stem cell transplant. Researchers continue to look for better ways to care for these survivors to give them the best possible quality of life.
Cancer relapse
The goal of a stem cell transplant in cancer is to prolong life and even cure the cancer. But in some cases, the cancer comes back (relapses). Relapse can happen a few months to a few years after transplant. It happens much more rarely 5 or more years after transplant.
After relapse, treatment options are often quite limited. A lot depends on your overall health at that point, and whether the type of cancer you have responds well to drug treatment. Treatment for those who are otherwise healthy and strong may include chemotherapy or targeted therapy. Some patients who have had allogeneic transplants may be helped by getting white blood cells from the same donor (this is called donor lymphocyte infusion) to boost the graft-versus-cancer effect. Sometimes a second transplant is possible. But most of these treatments pose serious risks even to healthier patients, so those who are frail, older, or have chronic health problems are often unable to get them.
Other options may include palliative (comfort) care, or a clinical trial of an investigational treatment. It’s important to know what the expected outcome of any further treatment might be, so talk with your doctor about the purpose of the treatment. Be sure you understand the pros and cons before you decide.
Secondary cancers (new cancers caused by treatment)
Along with the possibility of the original cancer coming back (relapse) after it was treated with a stem cell transplant, there is also a chance of having a second cancer after transplant. Studies have shown that people who have had allogeneic transplants have a higher risk of second cancer than people who got a different type of stem cell transplant.
Cancers that happen a few months after transplant are mainly lymphomas, especially the B-cell types. These seem to be caused by a common virus known as Epstein-Barr virus, or EBV. The immune system can normally keep the virus under control, but EBV can cause cancer — especially when the immune system is being suppressed with drugs, as it is after allogeneic transplant.
Acute leukemia is a type of cancer that can develop a few years after stem cell transplant. Another disorder of the bone marrow called myelodysplasia or myelodysplastic syndrome, in which the bone marrow makes defective blood cells, can also happen a few years after transplant. Myelodysplasia is generally a mild form of cancer, but it can become more aggressive in some people.
Secondary cancers that happen many years later may include solid tumor cancers, often of the skin, mouth, brain, liver, cervix, thyroid, breast, and bone.
Risk factors for developing a second cancer are being studied and may include:
- Radiation (such as total body irradiation) and high-dose chemo as part of the conditioning treatment
- Previous chemo or radiation treatment that was not part of the transplant process
- Immune system problems (such as graft-versus-host disease, HLA-mismatched allogeneic transplant, and immunosuppressant therapy)
- Being older than age 40 at the time of transplant
- Infection with viruses such as Epstein-Barr (EBV), cytomegalovirus (CMV), hepatitis B (HBV), or hepatitis C (HCV)
Some second cancers can show up a few months or a few years after transplant. But second cancers can take many years to develop, so the best studies are in those who have lived a long time after treatment.
Successfully treating a first cancer gives a second cancer time (and the chance) to develop. No matter what type of cancer is treated, and even without the high doses used for transplant, treatments like radiation and chemo can lead to a second cancer in the future.
Post-transplant lymphoproliferative disorder
Post-transplant lymphoproliferative disorder is an out-of-control growth of lymph cells, actually a type of lymphoma, that can develop after an allogeneic stem cell transplant. It’s linked to a malfunction of T-cells (a type of white blood cell that is part of the immune system) and the presence of Epstein-Barr virus (EBV). T-cells normally help rid the body of cells that contain viruses. When the T-cells aren’t working well, EBV-infected B-lymphocytes (a type of white blood cell) can grow and multiply. Most people are infected with EBV at some time during their lives, but the infection is controlled by a healthy immune system. The conditioning treatment given before transplant weakens the immune system, allowing the EBV infection to get out of control, which can lead to a post-transplant lymphoproliferative disorder.
Still, post-transplant lymphoproliferative disorder after allogeneic stem cell transplant is fairly rare. It most often happens within 1 to 6 months after allogeneic stem cell transplant, when the immune system is still very weak.
Post-transplant lymphoproliferative disorder is life-threatening. It may show up as lymph node swelling, fever, and chills. There’s no one standard treatment, but it’s often treated by cutting back on immunosuppressant drugs to let the patient’s immune system fight back. Other treatments include white blood cell (lymphocyte) transfusions to boost the immune response, using drugs like rituximab to kill the B cells, and giving anti-viral drugs to treat the EBV.
Even though post-transplant lymphoproliferative disorder doesn’t often happen after transplant, it’s more likely to occur with less well-matched donors and when strong suppression of the immune system is needed. Studies are being done to identify risk factors for post-transplant lymphoproliferative disorder and look for ways to prevent it in transplant patients who are at risk.
Stem cell transplant and having children
Most people who have stem cell transplants become infertile (unable to have children). This is not caused by the cells that are transplanted, but rather by the high doses of chemo and/or radiation therapy used. These treatments affect both normal and abnormal cells, and often damage reproductive organs.
If having children is important to you, or if you think it might be important in the future, talk to your doctor before treatment about ways to protect your fertility. Your doctor may be able to tell you if a particular treatment will be likely to cause infertility.
After chemo or radiation, women may find their menstrual periods become irregular or stop completely. This doesn’t always mean they cannot get pregnant, so birth control should be used before and after a transplant. The drugs used in transplants can harm a growing fetus.
The drugs used during transplant can also damage sperm, so men should use birth control to avoid starting a pregnancy during and for some time after the transplant process. Transplants may cause temporary or permanent infertility for men as well. Men might consider storing their sperm before having a transplant. This process can take several days. Fertility returns in some men, but the timing is unpredictable.