Byssinosis
Byssinosis also known as cotton worker’s lung, brown lung disease, Monday fever or mill fever 1, that is caused by exposure to cotton dust and is sometimes included among the pneumoconioses. Pneumoconioses are a group of interstitial lung diseases caused by the inhalation of certain dusts and the lung tissue’s reaction to the dust. The principal cause of the pneumoconioses is work-place exposure; environmental exposures have rarely given rise to these diseases.
Byssinosis is a type of hypersensitivity pneumonitis which can result from exposure to cotton fibers 2. Other similiar textiles fibers such as jute, hemp and flax are also thought to cause similar lung pathology 3.
Byssinosis is more common in people who work in the textile industry where cotton fabrics are made. In the United States, the disease is most common in Georgia, North and South Carolina, and Maryland 4.
In 1978, the Occupational Safety and Health Administration (OSHA) published a mandatory standard regarding exposure to cotton dust in the workplace which both improved both the detection and prevention of byssinosis.
Data published by the Center for Disease Control and Prevention (CDC) confirms a significant decline in the number of reported deaths from byssinosis between 1979 to 2010; however, comprehensive epidemiological data are lacking. Based on some older data, the quoted prevalence of byssinosis in the United Kingdom about 4%.
Outside of North America, byssinosis is not rare at all. In countries where cotton industries flourish, such as India, Pakistan, Nepal, Sri Lanka, and Bangladesh, byssinosis is common. In addition to the cotton industry, exposure to jute, hemp, and flex also cause byssinosis. The general population in these countries also smokes heavily which tends to exacerbate the symptoms. Despite modernization and introducing better working environments, byssinosis still is common in many parts of Pakistan, India, Indonesia, Ethiopia, Turkey, and Sudan 5.
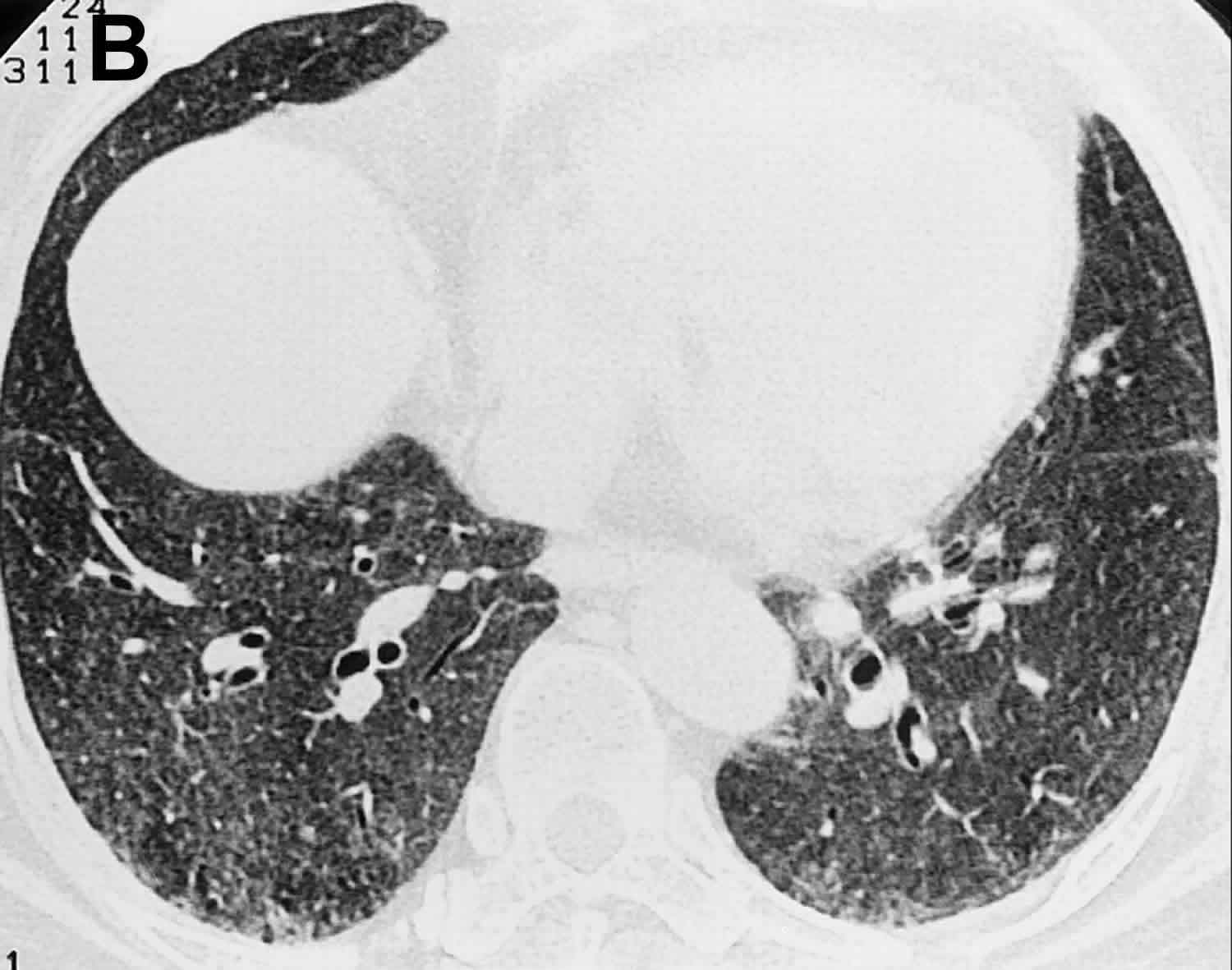
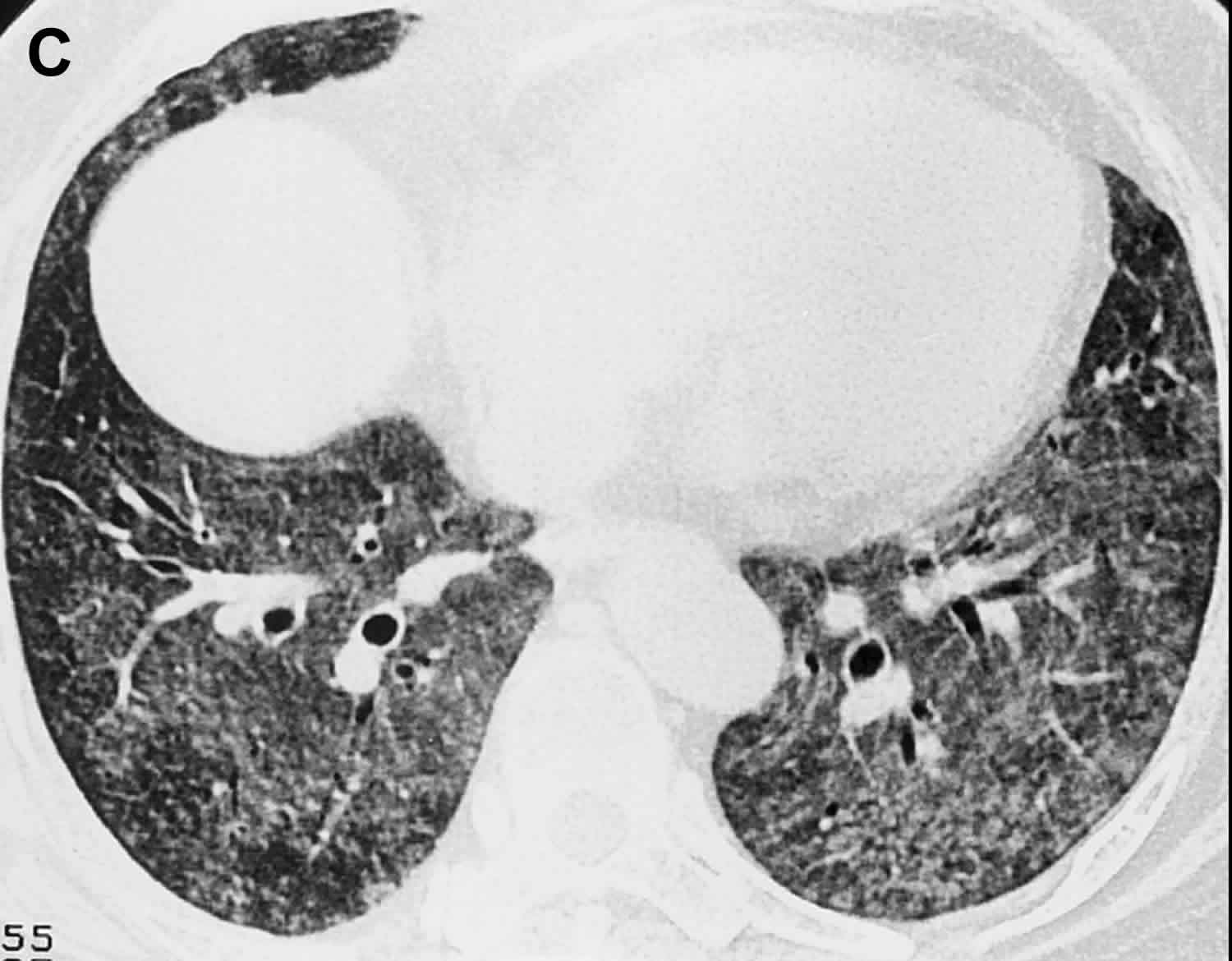
Figure 1. Byssinosis
Footnote: Byssinosis in a 56-year-old woman who had had frequent episodes of “Monday fever” and dyspnea while working in a cotton quilt factory over a 7-year period. (a) Chest radiograph shows diffuse, ill-defined haziness, predominantly in the lower lung zones. (b) High-resolution CT scan shows numerous ill-defined small nodules with ground-glass attenuation in both lungs. (c) High-resolution CT scan obtained 23 days later shows resolution of the ground-glass attenuation with fewer residual small nodules than were previously noted. No abnormality was seen at high-resolution CT performed 1 year after the patient quit her job. In spite of prolonged exposure, the patient’s respiratory symptoms and pulmonary functional impairment resolved completely.
[Source 3 ]Byssinosis causes
Byssinosis is caused by inhalation of cotton dust during the spinning and manufacturing process 1. However, exposure to jute, flax, and hemp fibers have been implicated in its development. Recent studies identified that endotoxin released from the cell wall of bacteria within textile fibers contributes to byssinosis symptoms 1. This endotoxin is a lipopolysaccharide found in the outer membrane of gram-negative bacteria which reside within the cotton dust. Exposure has been implicated as the key mediator of respiratory disease among these workers with studies showing a decline in FEV1 with endotoxin exposure. However, this is not uniform, and there seems to be a variable response – with an even greater decline in FEV1 in those with polymorphisms in the tumor necrosis factor (TNF) gene 6.
People who smoke are at a high risk for acquiring byssinosis 7.
Byssinosis symptoms
The beginning steps in yarn preparation produce the most dust. Therefore, the closer to the beginning of the process the person is, the higher the level of dust exposure and the greater risk of experiencing a pulmonary reaction or response.
In the initial stages, symptoms manifest as frequent coughing, chest tightness, dyspnea, and at times, wheezing, particularly within a few hours of exposure (or reexposure) to the workplace. Hence, patients usually report symptoms towards the beginning of their work week and thus the term Monday fever. This is in contrast to patients with occupational asthma who experience symptoms towards the end of their work week. Once exposure and lung irritation becomes persistent, patients will no longer have cyclical symptoms and progress to the chronic byssinosis state.
In conjunction with the above symptoms, cough with sputum production may also manifest, which can lead to a misdiagnosis of chronic obstructive pulmonary disease (COPD) or bronchitis.
Byssinosis complications
Byssinosis complications include:
- Lung fibrosis
- Oxygen dependency
- Disability
- Reduced exercise tolerance
- Premature death
Byssinosis diagnosis
There are no known diagnostic tests for byssinosis. However, acute exposure to cotton dust can result in a serological increase in leukocyte count. The diagnosis is often difficult because the condition can mimic asthma and many other pneumoconioses. Besides the physical exam, which is nonspecific, a chest x-ray is required to rule out other pathologies. The biggest clue to the disease is that the patient will usually complain that the symptoms get worse when he or she comes to work on Monday (hence the name Monday disease) and gets better when off work.
In a small proportion of the patients, physical examination was notable for the presence of fine basilar rales 8. X-ray examination demonstrated the presence of hyperlucency, diaphragm flattening, and emphysema 5. Diffuse, ill-defined haziness, mainly in the lower lung fields was also seen. A chest CT scan is usually done when the diagnosis is uncertain or when one wants to rule out other disorders. The available literature on radiological findings is limited, however, ground-glass opacities distributed largely in a basal fashion with centrilobular nodules, on high-resolution computed tomography (HRCT), have been reported 9.
Pulmonary function testing (PFT) can support suspected byssinosis by revealing a decline in forced expiratory volume over 1 second (FEV1) below 80% of their predicted values or a greater than 5% decline in their intrashift FEV1. The normal, physiologic 20 mL to 30mL annual decline in FEV1 seems to be accelerated to a value closer to 50 mL/year in cotton workers.
Byssinosis treatment
Once the condition is diagnosed, the patient must be told to avoid all exposure to cotton and other fabrics. One may require a change in career to avoid further exposure to cotton. Removing themselves from the work environment seems to be a beneficial approach for these patients. However, the available data on an annual FEV1 decline is conflicting.
After that symptomatic management with short- and long-acting, inhaled beta-agonists and perhaps corticosteroid inhalers may be necessary. Bronchodilators may be required for many months to improve symptoms. A short course of steroids does help those with severe symptoms.
It is vital that the patient stop smoking 10.
Byssinosis prognosis
The majority of people recover uneventfully with treatment, but at the same time, one needs to avoid exposure to cotton. For those individuals who are misdiagnosed or untreated, the chronic exposure to cotton can lead to lung fibrosis and impaired lung function. Most of these individuals will require oxygen and have impaired exercise function. Deaths from chronic exposure are not uncommon in Pakistan and India where textile industries still flourish, without preventive measures for workers.
References- Patel PH, Yarrarapu SNS, Anjum F. Byssinosis. [Updated 2020 Jul 2]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2020 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK519549
- Miller WT Jr, Shah RM. Isolated diffuse ground-glass opacity in thoracic CT: causes and clinical presentations. AJR Am J Roentgenol. 2005;184(2):613-622. doi:10.2214/ajr.184.2.01840613
- Kim KI, Kim CW, Lee MK, et al. Imaging of occupational lung disease. Radiographics. 2001;21(6):1371-1391. doi:10.1148/radiographics.21.6.g01nv011371
- Ali NA, Nafees AA, Fatmi Z, Azam SI. Dose-response of Cotton Dust Exposure with Lung Function among Textile Workers: MultiTex Study in Karachi, Pakistan. Int J Occup Environ Med. 2018 Jul;9(3):120-128.
- Er M, Emri SA, Demir AU, Thorne PS, Karakoca Y, Bilir N, Baris IY. Byssinosis and COPD rates among factory workers manufacturing hemp and jute. Int J Occup Med Environ Health. 2016;29(1):55-68.
- Hinson AV, Schlünssen V, Agodokpessi G, Sigsgaards T, Fayomi B. The prevalence of byssinosis among cotton workers in the north of Benin. Int J Occup Environ Med. 2014 Oct;5(4):194-200.
- Dangi BM, Bhise AR. Cotton dust exposure: Analysis of pulmonary function and respiratory symptoms. Lung India. 2017 Mar-Apr;34(2):144-149.
- Ozesmi M, Aslan H, Hillerdal G, Rylander R, Ozesmi C, Baris YI. Byssinosis in carpet weavers exposed to wool contaminated with endotoxin. Br J Ind Med. 1987 Jul;44(7):479-83.
- Satija B, Kumar S, Ojha UC, Gothi D. Spectrum of high-resolution computed tomography imaging in occupational lung disease. Indian J Radiol Imaging. 2013 Oct;23(4):287-96.
- Boubopoulos NJ, Constandinidis TC, Froudarakis ME, Bouros D. Reduction in cotton dust concentration does not totally eliminate respiratory health hazards: the Greek study. Toxicol Ind Health. 2010 Nov;26(10):701-7.