Cervix dilation
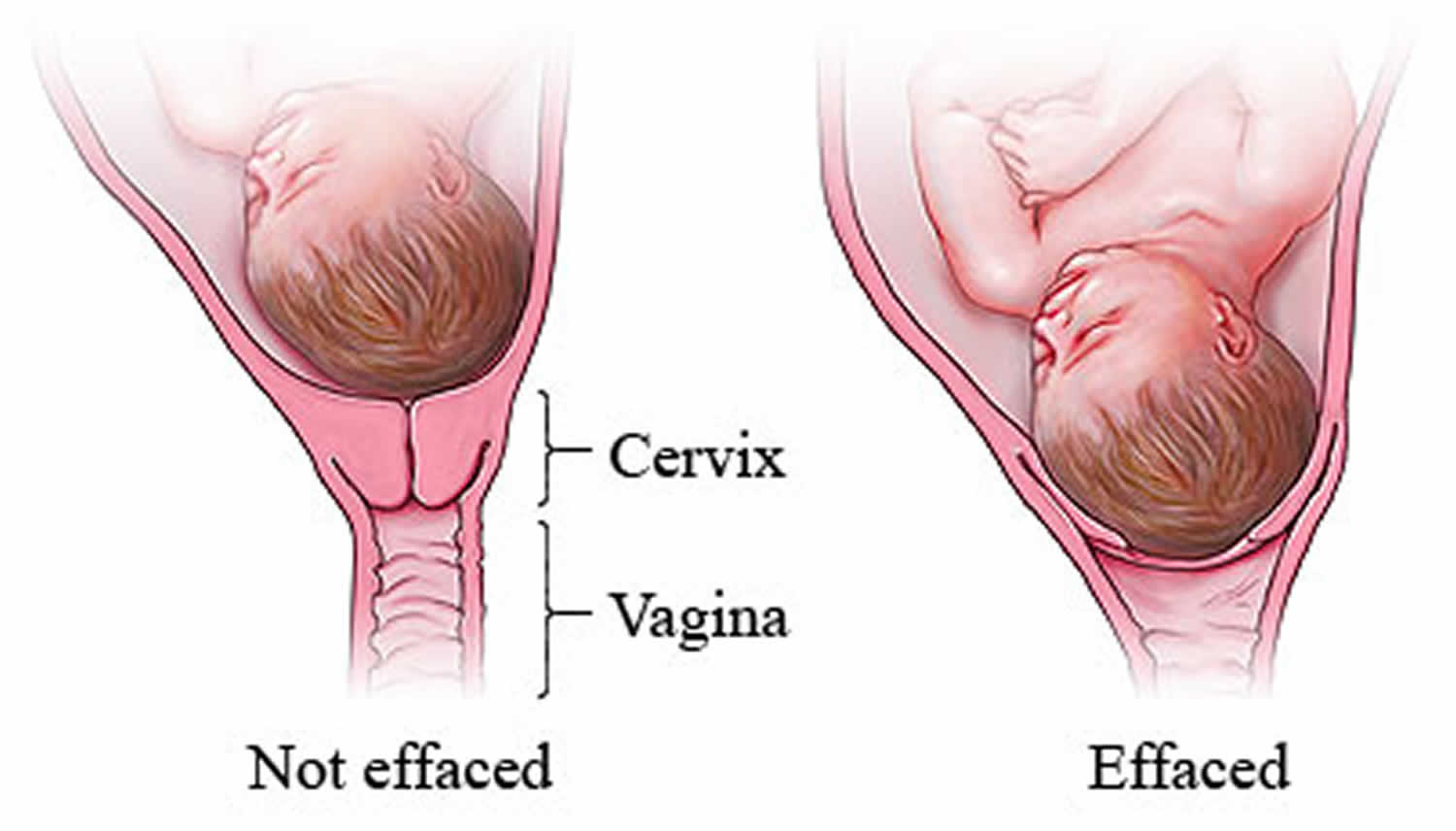
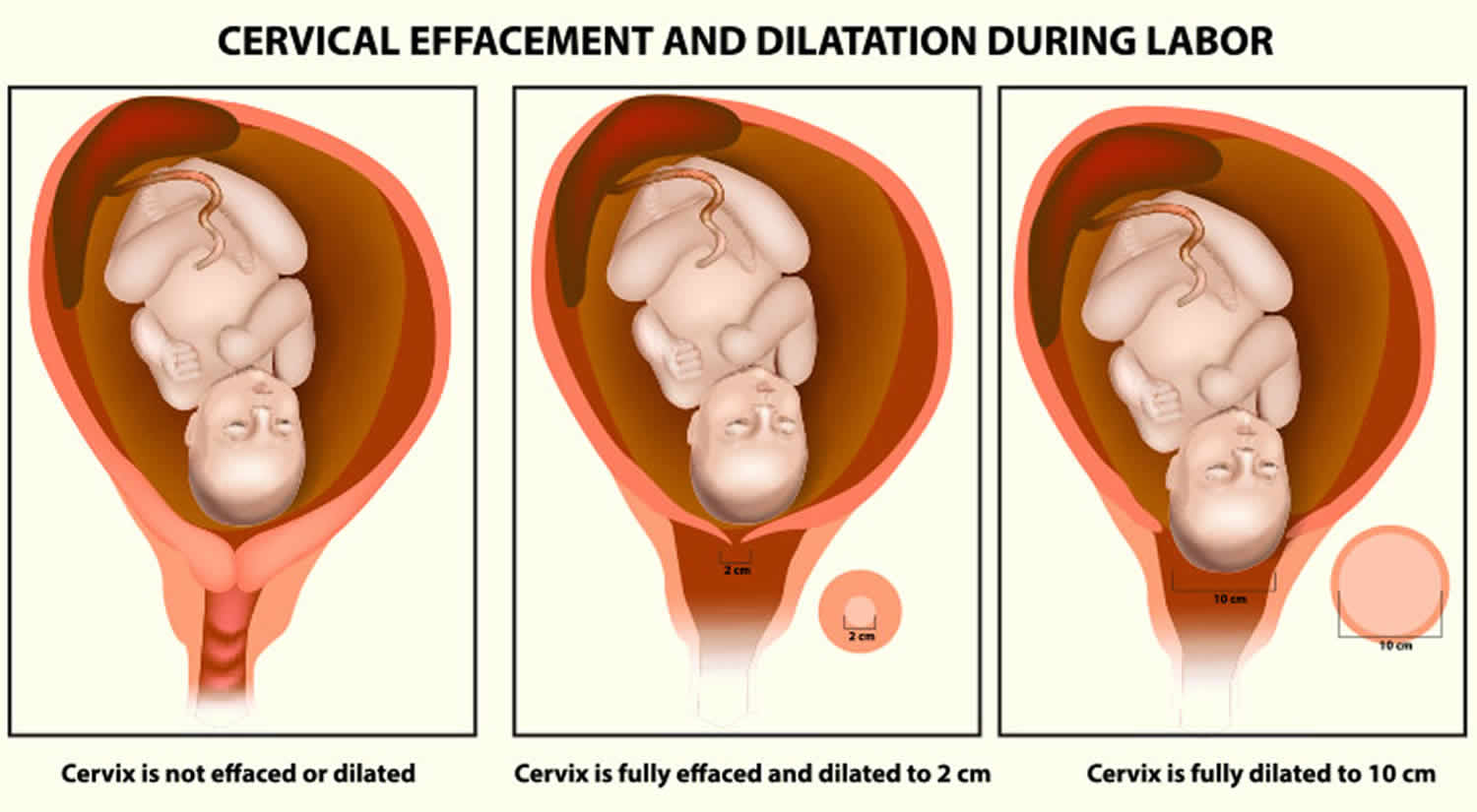
Cervix dilation also called cervical dilation is the opening of the cervix or the neck of the uterus, which happens in the first stage of labor 1. The cervix dilates (uterus opens) due to uterine contractions, and is a vital part of labor and delivery. Cervix dilation is measured in centimeters (cm) from 0 to 10 cm. At 0 cm, the cervix is closed. At 10 cm, it’s completely dilated 1. Your cervix must be completely dilated (10 cm dilated) before you can start the pushing stage. Labor and delivery generally follows a pattern — the cervix softening and opening; the amniotic sac rupturing; the contractions getting stronger and closer together. During the first stage of labor, the cervix opens (dilates) and thins out (effaces) to allow the baby to move into the birth canal. The cervix must be 100 percent effaced and 10 centimeters dilated before a vaginal delivery. Sometimes, however, labor and delivery takes surprising twists and turns. You might need an unexpected C-section.
In pregnancy, the uterine cervix serves 2 major functions. First, it retains its physical integrity by remaining firm during pregnancy as the uterus dramatically enlarges. This physical integrity is critical so that the developing fetus can remain in the uterus until the appropriate time for delivery. Second, in preparation for labor and delivery, the cervix softens and becomes more distensible, a process called cervical ripening. These chemical and physical changes are required for cervical dilation, labor and delivery of a fetus.
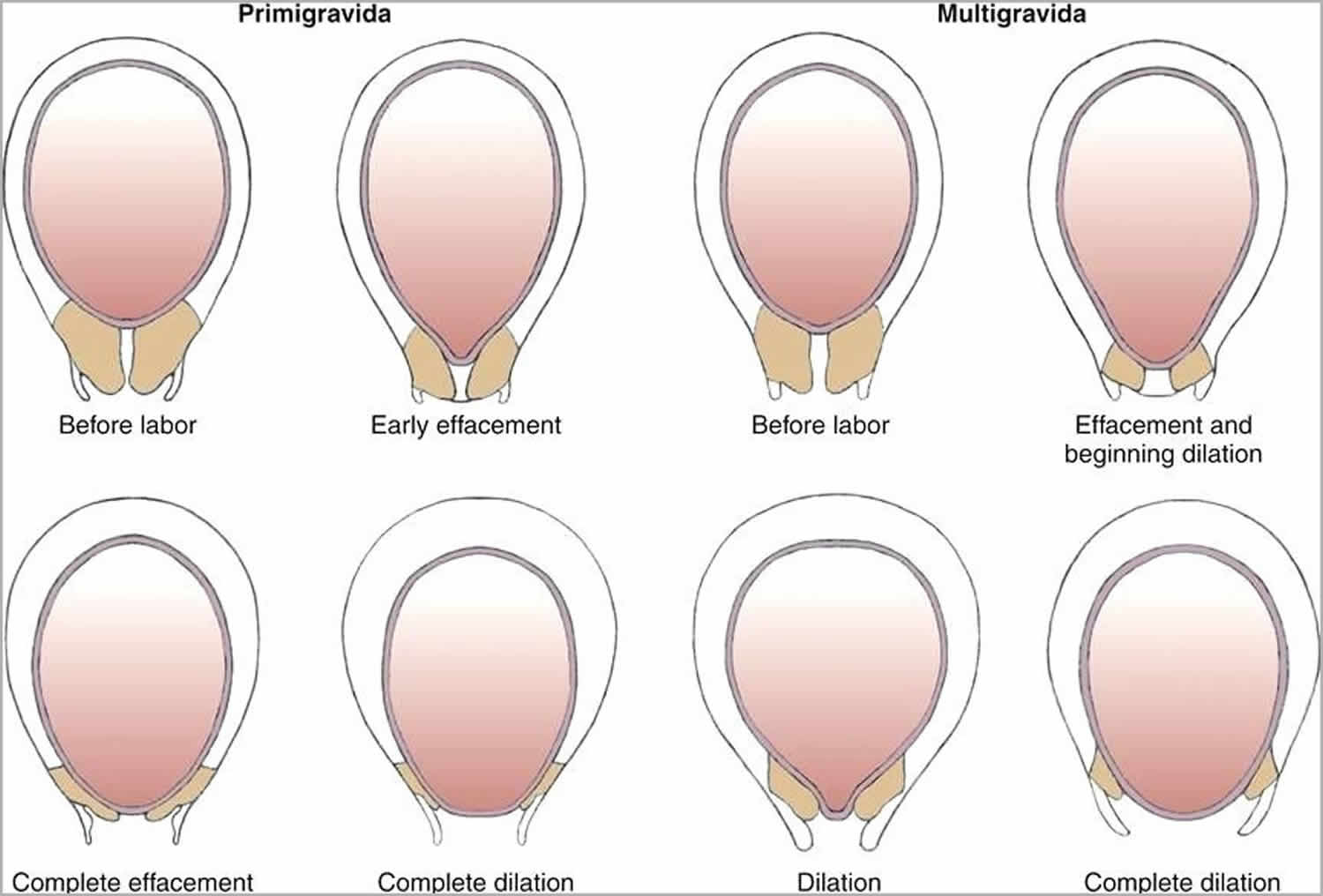
The stretching and thinning of the cervix is called effacement. Cervical effacement is measured in percentage and mostly happens before cervical dilation. The cervix thins and softens at first, and then opens. This happens when labor begins, which is usually around week 37. However, in some women, it could happen during week 38 or later.
Usually, in the first pregnancy, the cervix dilates during labor or after the contractions start. And in some cases, cervical effacement and dilation might happen just before the labor 2. As every pregnancy is different, the occurrence of effacement and dilation can differ.
You will know when dilation happens. All you need to do is pay attention to your bodily changes.
Although cervical dilation is most commonly reserved for childbirth, its use has expanded to a large number of diagnostic procedures (dilation and curettage for diagnosing endometrial cancer, endometrial biopsies, evaluating the causes of infertility and hysteroscopy) and therapeutic procedures (cervical stenosis, dysfunctional uterine bleeding and dysmenorrhea, inserting intrauterine devices and draining the uterine cavity) 3. Mechanical instruments, such as the Hern, Hegar, Pratt, Hanks and Denniston dilators, are used to sequentially dilate the cervix 4 by incrementally increasing the diameter of the inserted dilator until the dilation procedure is complete. However, these mechanical dilators require the use of appropriate force, which could permanently damage the cervical tissue and have adverse long-term effects on fertility 5. Their use is associated with various potential complications, such as uterine perforation, cervical laceration, infections and intraperitoneal hemorrhages 4.
Figure 1. Cervical effacement
Figure 2. Cervical dilation
Footnote: As labor nears, the fetus’s head drops down into the pelvis and pushes against the cervix. The cervix begins to thin (efface) and open (dilate), sometimes over a few weeks.
Ripening of the cervix
Cervical ripening refers to the softening of the cervix that typically begins prior to the onset of labor contractions and is necessary for cervical dilation and the passage of the fetus. Cervical ripening results from a series of complex biochemical processes that ends with rearrangement and realignment of the collagen molecules. The cervix thins, softens, relaxes and dilates in response to uterine contractions, allowing the cervix to easily pass over the presenting fetal part during labor.
In late pregnancy, hyaluronic acid content increases in the cervix. This leads to an increase in water molecules that intercalate among the collagen fibers. The amount of dermatan sulfate decreases, leading to reduced bridging among the collagen fibers and a corresponding decrease in cervical firmness. Chondroitin sulfate also decreases.
Cervical ripening is associated with decreased collagen fiber alignment, decreased collagen fiber strength and diminished tensile strength of the extracellular cervical matrix. An associated change with the cervical ripening process is an increase in cervical decorin (dermatan sulfate proteoglycan 2), leading to collagen fiber separation. Together, these changes lead to softening of the cervix (ie, ripening).
With uterine contractions, the ripened cervix dilates as the presenting fetal part descends, leading to reorientation of the tissue fibers in the cervix in the direction of the stress. Under the effect of myometrial contractions, the cervix passively dilates and is pulled over the presenting fetal part. Evidence also indicates that the elastin component of the cervix behaves in a ratchetlike manner so that dilation is maintained following the contraction.
In summary, cervical ripening is the result of realignment of collagen, degradation of collagen cross-linking due to proteolytic enzymes. Cervical dilation results from these processes plus uterine contractions. This is a complicated series of events in which many changes occur both simultaneously and sequentially. Research in this area is challenging due to both the difficulties inherent in human subjects research and the many differences existing between species.
Evaluation of cervical ripening
A variety of techniques have been developed to quantify cervical ripening in order to predict the timing of labor and delivery. This quantification is useful for patients at risk for preterm labor and for helping predict which patients will respond to induction of labor for medical reasons or for postdate pregnancy.
The most commonly used methodology to evaluate cervical ripening is the Bishop score because it is simple and has the most predictive value. This score uses cervical dilation, effacement, consistency, position, and the station of the presenting part. Other methods that have been described in the literature, generally for gauging the risk of preterm labor, include ultrasound assessment of the cervix and detection of fetal fibronectin in cervicovaginal secretions.
The total Bishop score is achieved by assessing the following five components on vaginal examination:
- Cervical dilatation: Cervical dilation is the measure of how dilated the cervix is in centimeters. This is performed by estimating the average diameter of the open cervix.
- Cervical effacement: Cervical effacement is the thinning or shortening of the cervix expressed as a percentage of the whole cervix. Zero percent effacement means the cervix is a normal, pre-labor length. Fifty percent effaced means the cervix is at half of the expected length. If the cervix is 100% effaced, it is paper thin.
- Cervical consistency: Cervical consistency of the cervix refers to the feel of the cervix on the exam. A firm cervix has a consistency similar to the tip of the nose, while a soft cervix has a consistency similar to the lips of the oral cavity.
- Cervical position: Cervical position refers to the position of the cervix relative to the fetal head and maternal pelvis.
- Fetal station: Fetal station is the position of the fetal head relative to the ischial spines of the maternal pelvis. The ischial spines are halfway between the pelvic inlet and outlet. At zero station, the fetal head is at the level of the ischial spines. Above and below this level are divided into thirds, by which station is denoted with negative numbers above and positive numbers below the zero station. As a fetal head makes its descent, the station changes from -3, -2, -1, 0, +1, +2, +3. In 1989, the American College of Obstetrics and Gynecology redefined fetal station from -5 to +5, using centimeters instead of thirds as a measurement from the ischial spines. The Bishop score, however, uses the -3 to +3 system.
Each components is given a Bishop score of 0-2 or 0-3. The highest possible total Bishop score is 13. A Bishop score of 5 or more is considered significant for cervical ripening and favorable for induction of labor, while a score of 9 or greater suggests ripening is completed.
Table 1. Bishop score for induction of labor
| Parameter\Score | 0 | 1 | 2 | 3 |
|---|---|---|---|---|
| Position of cervix | Posterior | Mid position | Anterior | – |
| Cervical Consistency | Firm | Medium | Soft | – |
| Cervical Effacement (%) | 0-30% | 40-50% | 60-70% | 80% |
| Cervical Dilation (cm) | Closed | 1-2 cm | 3-4 cm | 5-6 cm |
| Fetal station (-3 to +3) | -3 | -2 | -1, 0 | +1, +2 |
A recent study examining over 5,600 nulliparous women undergoing induction of labor found that a simplified Bishop score, including only cervical dilation, effacement, and station, was equally as predictive as the traditional Bishop score in predicting vaginal delivery 7.
Emerging evidence suggests that ultrasound assessment of the cervix helps distinguish patients at increased risk of preterm labor. In an meta analysis, Crane and Hutchens evaluated more than 300 studies, including 14 articles involving more than 2200 women in their final analysis. They found that ultrasound is a strong predictor of preterm birth among asymptomatic women at less than 35 weeks’ gestation 8.
Detection of fetal fibronectin in cervicovaginal secretions has also been used. Fetal fibronectin is a glycoprotein found in amniotic fluid and at the chorionic decidual interface. The absence of this protein in cervicovaginal secretions predicts prolongation of pregnancy. Fetal fibronectin is also predictive of response to prostaglandin application to the cervix at term in order to induce cervical ripening and labor. Currently, evaluation of fetal fibronectin is used predominantly in the assessment and triage of patients for preterm labor.
How do you know if your cervix is dilating?
You will be able to notice even the slightest of changes in the body if you are observant as you near the due date. The following signs indicate that the cervix is dilating:
- Lightning crotch: It is the sudden and intense pain experienced in your vagina when your baby descends. Some pregnant women say that the pain feels like a punch in the crotch. When you experience such pain near your due date, it could be an indication of cervix dilation.
- Frequent uterine contractions: When you experience frequent contractions, say six or more in 60 minutes, it might lead to cervix dilation. Such frequency of contractions usually happens before the due date 9.
- Ruptured membranes or breaking of water: This generally happens during the active phase of stage one labor. When a gush of water is released, the pressure might open the cervix.
- The purple or red line: When the labor progresses, some women get a purple line (discoloration) extending from buttocks to down. This line has proved to have a correlation with the cervical dilation 10.
- Mucus plug discharge: Mucus plug works as a seal to your cervix, and protects your little one from bacteria. So when your cervix opens, the mucus plug comes out 11.
- Bloody show: Brown or pink colored discharge could be a result of dilation. If you start noticing some stains, then it might mean your cervix has dilated 11.
- Others: There are other evident signs such as breathing or moaning due to contractions, a difference in your sense of smell, or curling of your toes. All these could be the result of cervix dilation.
If you do not notice any of the above signs, then you can manually check your cervix for dilation. Checking cervical dilation helps you to know how close you are to labor and the effective management of labor. It is always good to get this done by a medical professional. In case you are doing it on your own, seek medical advice. When your due date is nearing or has passed, your doctor may check the cervix to see if it is dilated.
Checking cervix dilation
The person performing the procedure should make sure that the fingernails are cut and clean, use sterilized gloves for hands. Otherwise, there could be chances of infections and cuts. Using sterile gloves and lubricant, perform a vaginal exam and determine the dilatation and effacement of the cervix. Squatting is the preferred position. However, you can choose any other position that is comfortable for you. A small amount of bleeding during the days or hours leading up to the onset of labor is common and called “bloody show.”
Steps to check cervix dilation: Follow these steps to check if the cervix is dilated.
- Use two fingers: Index and middle fingers are inserted into the vagina and against the cervix to gauge the opening. Avoid the anal area.
- Assess the dilation: The two fingers should feel the cervix and the opening to assess the length.
Dispose of the gloves: Once the examination is done, the gloves have to be disposed of.
You can use the cervix dilation chart below to compare your cervical dilation 12.
Cervix dilation is expressed in centimeters.
- 1.5 cm: One finger fits tightly through the cervix and touches the fetal head.
- 2.0 cm: One finger fits loosely inside the cervix, but I can’t fit two fingers in.
- 3.0 cm: Two fingers fit tightly inside the cervix.
- 4.0 cm: Two fingers fit loosely inside the cervix.
- 6.0 cm: There is still 2 cm of cervix still palpable on both sides of the cervix.
- 8.0 cm: There is only 1 cm of cervix still palpable on both sides of the cervix.
- 9.0 cm: Not even 1 cm of cervix is left laterally, or there is only an anterior lip of cervix.
- 10.0 cm: You can’t feel any cervix anywhere around the fetal head.
Effacement is easiest to measure in terms of centimeters of thickness, ie., 1 cm thick, 1.5 cm thick, etc. Alternatively, you may express the thickness in percent of an uneffaced cervix i.e., 50%, 90%, etc. This expression presumes a good knowledge of what an uneffaced cervix should feel like.
When not to check your cervix during pregnancy?
The cervix should not be checked either by you or by a healthcare professional in these cases.
- In case you have had bad experiences with checking the cervix for dilation, you should avoid trying it again.
- If it causes too much pain, then stop doing it.
- When the placenta is covering the cervix (placenta previa), it is not recommended to check the cervix.
- If you have any sutures, you shouldn’t check your cervix.
If your doctor finds it risky to check cervical dilation, then do not attempt it. Cervical dilation should only be done when your medical professional has recommended it. Otherwise, do not attempt it.
Are there ways to dilate the cervix?
Yes, there are natural and medical ways to dilate the cervix. To dilate the cervix, it has to be softened (cervical ripening) first. Usually, medical experts prefer waiting for it to happen naturally. But in some cases, it becomes necessary to dilate the cervix and induce labor. Labor is induced to start contractions of the uterus for a vaginal birth. Labor induction may be recommended when there are concerns about the health of the woman or the fetus. It also may be recommended when labor has not started on its own. In addition to some conditions for which labor induction is recommended, new research suggests that induction for healthy women at 39 weeks in their first full-term pregnancies may reduce the risk of cesarean birth.
You and your obstetrician–gynecologist (ob-gyn) or other health care professional may talk about induction at 39 weeks if:
- this is your first full-term pregnancy
- you are carrying only one fetus
- you and your fetus are healthy
When a woman and her fetus are healthy, induction should not be done before 39 weeks. Babies born at or after 39 weeks have the best chance at healthy outcomes compared with babies born before 39 weeks. When the health of a woman or her fetus is at risk, induction before 39 weeks may be recommended.
There are several methods to start labor if it has not started naturally. The ways to start labor may include the following:
- Ripening the cervix
- Stripping the membranes
- Oxytocin
- Rupturing the amniotic sac
Ripening the cervix
Ripening the cervix is a procedure that helps the cervix soften and thin out so that it will dilate (open) during labor. Before inducing labor, your obstetrician–gynecologist (ob-gyn) or other health care professional may check to see if your cervix is ready using the Bishop score. With this scoring system, a number ranging from 0 to 13 is given to rate the condition of the cervix. A score of 6 or less means that your cervix is not yet ready for labor. If the cervix is not ready, ripening may be done.
Ripening of the cervix may be done in the following ways:
- Using medications that contain prostaglandins. These drugs can be inserted into the vagina or taken by mouth.
- Using a thin tube that has an inflatable balloon on the end. The tube is inserted into the cervix and then expanded. This helps widen the cervix.
Stripping the membranes
To “strip the membranes,” your obstetrician–gynecologist (ob-gyn) or other health care professional sweeps a gloved finger over the thin membranes that connect the amniotic sac to the wall of your uterus. This also is called “sweeping the membranes.” This action is done when the cervix is partially dilated. It may cause your body to release natural prostaglandins, which soften the cervix further and may cause contractions.
Oxytocin
Oxytocin is a hormone that causes contractions of the uterus. It can be used to start labor or to speed up labor that began on its own. Contractions usually start about 30 minutes after oxytocin is given.
Rupturing the amniotic sac
To rupture the amniotic sac, an ob-gyn or other health care professional makes a small hole in the sac with a special tool. This procedure, called an amniotomy, may be done after a woman has been given oxytocin. Amniotomy is done to start labor when the cervix is dilated and thinned and the fetus’s head has moved down into the pelvis. Most women go into labor within hours after the amniotic sac breaks (their “water breaks”).
What are the risks of labor induction?
With some induction methods, the uterus can be overstimulated, causing it to contract too often. Too many contractions may lead to changes in the fetal heart rate. Other risks of cervical ripening and labor induction can include infection in the woman or her fetus.
Is labor induction always effective?
Sometimes labor induction does not work. Early labor is the time when a woman’s contractions start and her cervix begins to open. Women who have induction at 39 weeks should be allowed up to 24 hours or longer for the early phase of labor. They also should be given oxytocin at least 12–18 hours after stripping of the membranes. If a woman’s labor does not progress, it may be considered a failed attempt at induction.
What happens if induction does not work?
If your labor does not progress, and if you and your fetus are doing well after attempting induction, you may be sent home. You can schedule another appointment to try induction again. If your labor starts, you should go back to the hospital. If you or your fetus are not doing well after attempting induction, a cesarean delivery may be needed.
References- What Happens During Labor. https://www.bidmc.org/centers-and-departments/obstetrics-and-gynecology/pregnancy/labor-and-delivery/stages-of-labor
- Cervical Effacement and Dilatation. https://www.uofmhealth.org/health-library/zx3441
- Newmann S, Dalve-Endres A, Drey EA. Cervical preparation for surgical abortion from 20 to 24 weeks’ gestation. Contraception. 2008;77:308–314. doi: 10.1016/j.contraception.2008.01.004
- Gelber S, Sciscione A. Mechanical methods of cervical ripening and labor induction. Clin Obstet Gynecol. 2006;49:642–657. doi: 10.1097/00003081-200609000-00022
- Gupta JK, Johnson N. Should we use prostaglandins, tents or progesterone antagonists for cervical ripening before first trimester abortion? Contraception. 1992;46:489–497. doi: 10.1016/0010-7824(92)90152-J
- Wormer KC, Williford AE. Bishop Score. [Updated 2019 Jan 7]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK470368
- Laughon SK, Zhang J, Troendle J, Sun L, Reddy UM. Using a simplified Bishop score to predict vaginal delivery. Obstet Gynecol. 2011 Apr. 117(4):805-11.
- Crane JM, Hutchens D. Transvaginal sonographic measurement of cervical length to predict preterm birth in asymptomatic women at increased risk: a systematic review. Ultrasound Obstet Gynecol. 2008 May. 31(5):579-87.
- Recognizing Premature Labor. https://www.ucsfhealth.org/education/recognizing-premature-labor
- A. Shepherd and et al.; The purple line as a measure of labour progress: a longitudinal study; BMC Pregnancy & Childbirth (2010). https://www.academia.edu/12842275/The_purple_line_as_a_measure_of_labour_progress_a_longitudinal_study
- How to Tell When Labor Begins. https://www.acog.org/Patients/FAQs/How-to-Tell-When-Labor-Begins?IsMobileSet=false
- Operational Obstetrics & Gynecology. Labor and Delivery. http://www.operationalmedicine.org/ed2/Enhanced/LandD/DilatationandEffacement.htm