What are polyps in the colon
Colon polyps are small benign growths of tissue inside the colon or large intestine or rectum. Benign colon polyps means they are not a cancer and do not spread. You may have one or many polyps. They become more common with age. Some polyps are mushroom-shaped protrusions on the end of a stalk. Others appear as bumps that lie flat against the intestinal wall.
Colon polyps are very common, affecting around 1 in 4 people at some point in their lives. Certain people are more likely than others. Colon polyps are slightly more common in men than women.
You may have a greater chance of getting polyps if you:
- Are over age 50
- Have had polyps before
- Have a family member with polyps
- Have a family history of colon cancer
Most colon polyps do not cause symptoms. If you have symptoms, they may include blood on your underwear or on toilet paper after a bowel movement, blood in your stool, or constipation or diarrhea lasting more than a week.
Some people develop just one polyp, while others may have a few.
There are several types of polyps. Most colon polyps are noncancerous (benign), but one type, the adenomatous polyp, is associated with changes (called mutations) in the DNA of the lining of the colon. These mutations can progress into colon cancer. The larger the polyp, the greater the chance that it contains cancerous cells, which is why it is important to have them removed.
See your doctor if you experience:
- Cramping or abdominal (belly) pain
- Dark stools, or blood in the stool
- A change in bowel habits, such as diarrhea, constipation, or narrowing of the stool, that lasts for more than a few days
- A feeling that you need to have a bowel movement that is not relieved by doing so
- Rectal bleeding
- Weakness and fatigue
- Unintended weight loss
Many of these symptoms can be caused by conditions other than colon cancer, such as infection, hemorrhoids, or irritable bowel syndrome. Still, if you have any of these problems, it’s important to see your doctor right away so the cause can be found and treated, if needed.
You should be screened regularly for polyps if:
- You’re age 50 or older.
- You have risk factors, such as a family history of colon cancer. Some high-risk individuals should begin regular screening much earlier than age 50.
Colon cancer risk
Colon polyps don’t usually turn into cancer. But if some types of polyps (called adenomas) are not removed, there’s a chance they may eventually become cancerous. Doctors believe that most colon cancers develop from adenoma polyps. However, very few colon polyps will turn into cancer, and it takes many years for this to happen. Because of the risk of colon polyps developing into cancer, your doctor will always recommend getting colon polyps treated.
Polyps bigger than 1 centimeter (cm) have a higher cancer risk than polyps smaller than 1 centimeter.
Risk factors include:
- Age
- Family history of colon cancer or polyps
- A type of polyp called villous adenoma
A small number of people with polyps may also be linked to some inherited disorders, including:
- Familial adenomatous polyposis (FAP)
- Gardner syndrome (a type of FAP)
- Juvenile polyposis (disease that causes many benign growths in the intestine, usually before 20 years old)
- Lynch syndrome (HNPCC, a disease that raises the chance of many types of cancer, including in the intestine)
- Peutz-Jeghers syndrome (disease that causes intestinal polyps, usually in the small intestine and usually benign)
Types of colon polyps
There are two main categories of polyps, non-neoplastic and precancerous colon polyps.
Non-neoplastic polyps include hyperplastic polyps, inflammatory polyps and hamartomatous polyps. Non-neoplastic polyps typically do not become cancerous.
Precancerous colon polyps also called neoplastic polyps include adenomas and serrated types. Most colon polyps are adenomas. Serrated polyps may become cancerous, depending on their size and location in the colon. In general, the larger a polyp, the greater the risk of cancer, especially with neoplastic polyps.
Inflammatory polyps may be seen with ulcerative colitis or Crohn’s disease of the colon. Although the polyps themselves are not a significant threat, having ulcerative colitis or Crohn’s disease of the colon increases your overall risk of colon cancer.
Precancerous colon polyps
Adenomatous polyps are a common type. They are gland-like growths that develop on the mucous membrane that lines your colon, although it is different in several important ways when it is looked at under the microscope. Adenomatous polyps are also called adenomas and are most often one of the following:
- Tubular polyp, which protrudes out in the lumen (open space) of the colon
- Villous adenoma, which is sometimes flat and spreading, and is more likely to become a cancer
Adenomas can have several different growth patterns that can be seen under the microscope by the pathologist. There are 2 major growth patterns: tubular and villous. Many adenomas have a mixture of both growth patterns, and are called tubulovillous adenomas. Most adenomas that are small (less than ½ inch) have a tubular growth pattern. Larger adenomas may have a villous growth pattern. Larger adenomas more often have cancers developing in them. Adenomas with a villous growth pattern are also more likely to have cancers develop in them.
The growth pattern is only important because it helps determine when you will need your next colonoscopy to make sure you don’t develop colon cancer in the future.
When adenomas become cancerous, they are known as adenocarcinomas. Adenocarcinomas are cancers that originate in glandular tissue cells. Adenocarcinoma is the most common type of colorectal cancer.
Sessile serrated adenoma (adenomatous polyp) or traditional serrated adenoma (adenomatous polyp)
Colon polyps that tend to grow as slightly flattened, broad-based polyps are referred to as sessile.
Serrated colon polyps (serrated adenomas) have a saw-tooth appearance under the microscope. There are 2 types, which look a little different under the microscope:
- Sessile serrated adenomas (also called sessile serrated polyps)
- Traditional serrated adenomas
These types of polyps are not cancer, but they are pre-cancerous (meaning that they can turn into cancers). Someone who has had one of these types of polyps has an increased risk of later developing cancer of the colon. Hence, both of these types of colon polyp need to be removed from your colon. However, most patients with these colon polyps, never develop colon cancer.
If your adenoma was biopsied but not completely removed, you will need to talk to your doctor about what other treatment you’ll need. Most of the time, adenomas are removed during a colonoscopy. Sometimes, though, the adenoma may be too large to remove during colonoscopy. In such cases you may need surgery to have the adenoma removed.
If you’ve had an adenoma, you will need to have another colonoscopy to make sure that you don’t develop any more adenomas. When your next colonoscopy should be scheduled depends on a number of things, like how many adenomas were found, if any were villous, and if any had high-grade dysplasia. The timing of your next colonoscopy should be discussed with your treating doctor, as he or she knows the details of your specific case.
Non-neoplastic colon polyps
Non-neoplastic polyps include hyperplastic colon polyps, inflammatory polyps and hamartomatous polyps. Non-neoplastic polyps typically do not become cancerous and are not a cause for concern.
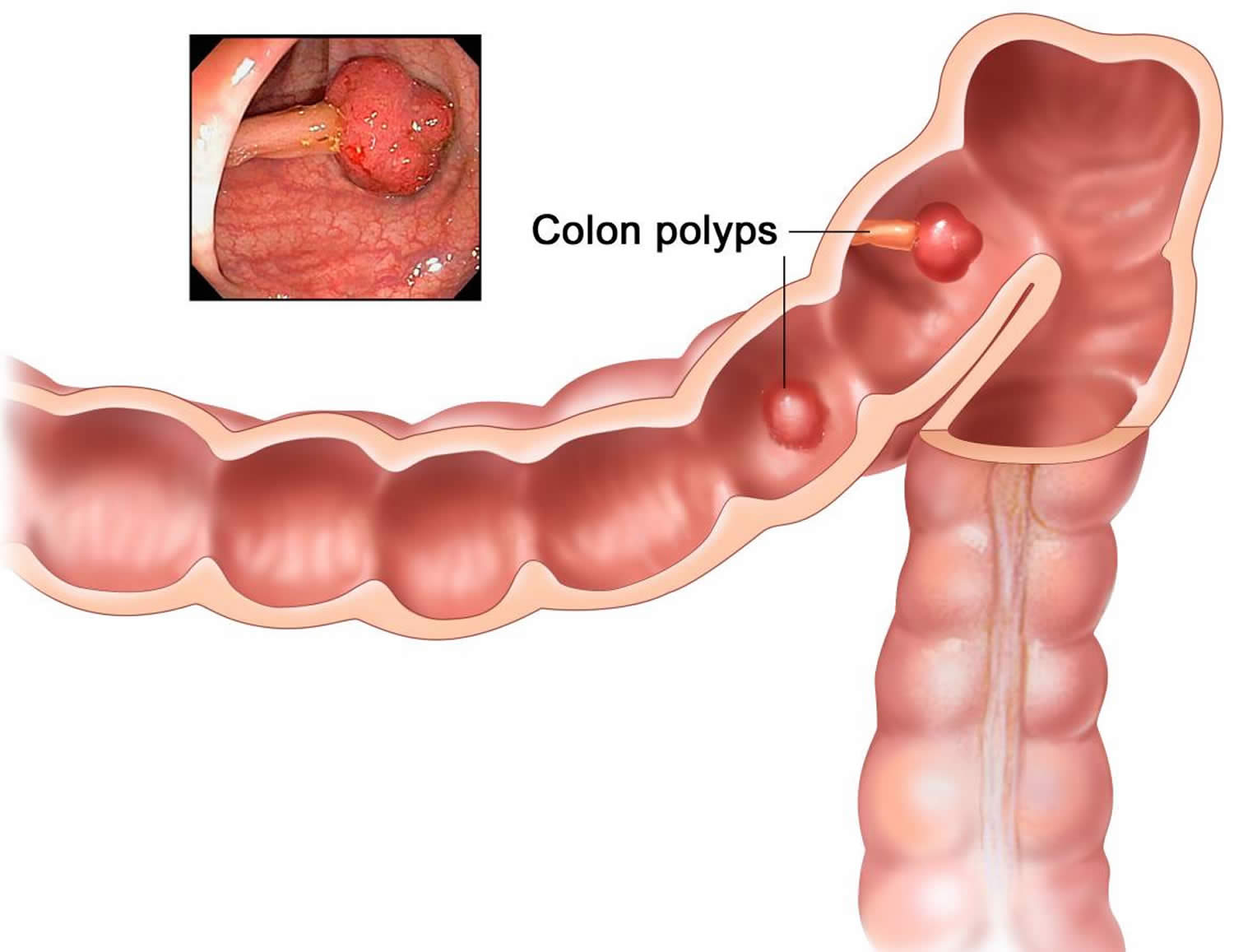
Figure 1. Colon polyps
Figure 2. Colon polyp
Footnotes: Polyps in the colon. Some polyps have a stalk and others do not. Inset shows a photo of a polyp with a stalk.
[Source 1 ]Figure 3. Large colon polyp – large polyps are 10 millimeters (mm) or larger in diameter
Colon polyps outlook (prognosis)
Outlook is excellent if the colon polyps are removed. Polyps that are not removed can develop into cancer over time..
Colorectal Cancer Early Detection
Because colon cancer often doesn’t cause symptoms until it is advanced, the American Cancer Society recommends that people at average risk* of colorectal cancer start regular screening at age 45 2. Screening is the process of looking for cancer in people who have no symptoms. People with a family history of the disease or who have certain other risk factors should talk with their doctor about beginning screening at a younger age. Several different tests can be used to screen for colon cancer. This can be done either with a sensitive test that looks for signs of cancer in a person’s stool (a stool-based test), or with an exam that looks at the colon and rectum (a visual exam). Talk with your doctor to find out which tests might be right for you. The most important thing is to get screened, no matter which test you choose.
*For screening, people are considered to be at AVERAGE risk if they DO NOT have:
- A personal history of colorectal cancer or certain types of polyps
- A family history of colorectal cancer
- A personal history of inflammatory bowel disease (ulcerative colitis or Crohn’s disease)
- A confirmed or suspected hereditary colorectal cancer syndrome, such as familial adenomatous polyposis (FAP) or Lynch syndrome (hereditary non-polyposis colon cancer or HNPCC)
- A personal history of getting radiation to the abdomen (belly) or pelvic area to treat a prior cancer
People who are in good health and with a life expectancy of more than 10 years should continue regular colorectal cancer screening through the age of 75.
For people ages 76 through 85, the decision to be screened should be based on a person’s preferences, life expectancy, overall health, and prior screening history.
People over 85 should no longer get colorectal cancer screening.
When colon cancer is found early, before it has spread, the 5-year relative survival rate is 90%. This means 9 out of 10 people with early-stage cancer survive at least 5 years. But if the cancer has had a chance to spread outside the colon, survival rates are lower.
Table 1. American Cancer Society Guidelines on Screening and Surveillance for the Early Detection of Colorectal Adenomas and Cancer in People at Increased Risk or High Risk
| INCREASED RISK – People who have a history of polyps on prior colonoscopy | |||
| Risk category | When to test | Recommended test(s) | Comment |
| People with small rectal hyperplastic polyps | Same age as those at average risk | Colonoscopy, or other screening options at same intervals as for those at average risk | Those with hyperplastic polyposis syndrome are at increased risk for adenomatous polyps and cancer and should have more intensive follow-up. |
| People with 1 or 2 small (no more than 1 cm) tubular adenomas with low-grade dysplasia | 5 to 10 years after the polyps are removed | Colonoscopy | Time between tests should be based on other factors such as prior colonoscopy findings, family history, and patient and doctor preferences. |
| People with 3 to 10 adenomas, or a large (at least 1 cm) adenoma, or any adenomas with high-grade dysplasia or villous features | 3 years after the polyps are removed | Colonoscopy | Adenomas must have been completely removed. If colonoscopy is normal or shows only 1 or 2 small tubular adenomas with low-grade dysplasia, future colonoscopies can be done every 5 years. |
| People with more than 10 adenomas on a single exam | Within 3 years after the polyps are removed | Colonoscopy | Doctor should consider possible genetic syndrome (such as FAP or Lynch syndrome). |
| People with sessile adenomas that are removed in pieces | 2 to 6 months after adenoma removal | Colonoscopy | If entire adenoma has been removed, further testing should be based on doctor’s judgment. |
| INCREASED RISK – People who have had colorectal cancer | |||
| Risk category | When to test | Recommended test(s) | Comment |
| People diagnosed with colon or rectal cancer | At time of colorectal surgery, or can be 3 to 6 months later if person doesn’t have cancer spread that can’t be removed | Colonoscopy to look at the entire colon and remove all polyps | If the tumor presses on the colon/rectum and prevents colonoscopy, CT colonoscopy (with IV contrast) or double-contrast barium enema may be done to look at the rest of the colon. |
| People who have had colon or rectal cancer removed by surgery | Within 1 year after cancer resection (or 1 year after colonoscopy to make sure the rest of the colon/rectum was clear) | Colonoscopy | If normal, repeat in 3 years. If normal then, repeat test every 5 years. Time between tests may be shorter if polyps are found or there’s reason to suspect Lynch syndrome. After low anterior resection for rectal cancer, exams of the rectum may be done every 3 to 6 months for the first 2 to 3 years to look for signs of recurrence. |
| INCREASED RISK – People with a family history | |||
| Risk category | Age to start testing | Recommended test(s) | Comment |
| Colorectal cancer or adenomatous polyps in any first-degree relative before age 60, or in 2 or more first-degree relatives at any age (if not a hereditary syndrome). | Age 40, or 10 years before the youngest case in the immediate family, whichever is earlier | Colonoscopy | Every 5 years. |
| Colorectal cancer or adenomatous polyps in any first-degree relative aged 60 or older, or in at least 2 second-degree relatives at any age | Age 40 | Same test options as for those at average risk. | Same test intervals as for those at average risk. |
| HIGH RISK | |||
| Risk category | Age to start testing | Recommended test(s) | Comment |
| Familial adenomatous polyposis (FAP) diagnosed by genetic testing, or suspected FAP without genetic testing | Age 10 to 12 | Yearly flexible sigmoidoscopy to look for signs of FAP; counseling to consider genetic testing if it hasn’t been done | If genetic test is positive, removal of colon (colectomy) should be considered. |
| Lynch syndrome (hereditary non-polyposis colon cancer or HNPCC), or at increased risk of Lynch syndrome based on family history without genetic testing | Age 20 to 25 years, or 10 years before the youngest case in the immediate family | Colonoscopy every 1 to 2 years; counseling to consider genetic testing if it hasn’t been done | Genetic testing should be offered to first-degree relatives of people found to have Lynch syndrome mutations by genetic tests. It should also be offered if 1 of the first 3 of the modified Bethesda criteria is met.* |
| Inflammatory bowel disease: -Chronic ulcerative colitis -Crohn’s disease | Cancer risk begins to be significant 8 years after the onset of pancolitis (involvement of entire large intestine), or 12-15 years after the onset of left-sided colitis | Colonoscopy every 1 to 2 years with biopsies for dysplasia | These people are best referred to a center with experience in the surveillance and management of inflammatory bowel disease. |
Table 2. Summary of professional society recommendations on when to start and when to stop colorectal cancer screening
| Colorectal cancer screening start age | Colorectal cancer screening stop age | |
|---|---|---|
| Multi-Society Task Force, 2021 | “We suggest that clinicians offer colorectal cancer screening to all average-risk individuals age 45-49 (weak recommendation; low-quality evidence).” | “We suggest that individuals who are up to date with screening and have negative prior screening tests, particularly high-quality colonoscopy, consider stopping screening at age 75 years or when life expectancy is less than 10 years (weak recommendation, low-quality evidence).” |
| “For average-risk individuals who have not initiated screening before age 50, we recommend that clinicians offer colorectal cancer screening to all average-risk individuals beginning at age 50 (strong recommendation, high-quality evidence).” | “We suggest that persons without prior screening should be considered for screening up to age 85, depending on consideration of their age and comorbidities (weak recommendation, low-quality evidence).” | |
| National Comprehensive Cancer Network, 2021 3 | “Average risk: age ≥45. The panel has reviewed existing data for beginning screening of average-risk individuals at age <50 years. Based on their assessment, the panel agrees that the data are stronger to support beginning screening at 50 years but acknowledges that lower-level evidence supports a benefit for screening earlier. When initiating screening for all eligible individuals, the panel recommends a discussion of potential harms/risks and benefits, and the consideration of all recommended colorectal cancer screening options.” | Not provided |
| American College of Gastroenterology, 2021 4 | “We recommend colorectal cancer screening in average-risk individuals between ages 50 and 75 years to reduce incidence of advanced adenoma, colorectal cancer, and mortality from colorectal cancer.” Strong recommendation; moderate-quality evidence “We suggest colorectal cancer screening in average-risk individuals between ages 45 and 49 years to reduce incidence of advanced adenoma, colorectal cancer, and mortality from colorectal cancer.” Conditional recommendation; very low-quality evidence | “We suggest that a decision to continue screening beyond age 75 years be individualized (conditional recommendation strength, very low-Grading of Recommendations Assessment, Development and Evaluation quality of evidence).” |
| U.S. Preventative Services Task Force, 2021 5 | Grade A: “The U.S. Preventative Services Task Force recommends screening for colorectal cancer in all adults ages 50 to 75 years.” Grade B: “The U.S. Preventative Services Task Force recommends screening for colorectal cancer in adults aged 45 to 49 years.” | Grade C: “The U.S. Preventative Services Task Force recommends that clinicians selectively offer screening for colorectal cancer in adults aged 76 to 85 years. Evidence indicates that the net benefit of screening all persons in this age group is small. In determining whether this service is appropriate in individual cases, patients and clinicians should consider the patient’s overall health, prior screening history, and preferences.” |
| American College of Physicians, 2019 6 | “Clinicians should screen for colorectal cancer in average-risk adults between the ages of 50 and 75 years.” | “Clinicians should discontinue screening for colorectal cancer in average-risk adults older than 75 years or in adults with a life expectancy of 10 years or less.” |
| American Cancer Society, 2018 7 | “The American Cancer Society recommends that adults aged 45 and older with an average risk of colorectal cancer undergo regular screening with either a high-sensitivity stool-based test or a structural (visual) examination, depending on patient preference and test availability. As a part of the screening process, all positive results on non-colonoscopy screening tests should be followed up with timely colonoscopy.” | “Average-risk adults in good health with a life expectancy of greater than 10 years continue colorectal cancer screening through the age of 75 years (qualified recommendation).” |
| “The recommendation to begin screening at age 45 is a qualified recommendation.” | Clinicians should “individualize colorectal cancer screening decisions for individuals aged 76 through 85 years based on patient preferences, life expectancy, health status, and prior screening history (qualified recommendation).” | |
| “The recommendation for regular screening in adults aged 50 y and older is a strong recommendation.” | Clinicians should “discourage individuals over age 85 years from continuing colorectal cancer screening (qualified recommendation).” |
Table 3. Benefits and limitations of colorectal cancer screening tests
| Test | Benefits | Limits |
|---|---|---|
| Fecal immunochemical test (FIT) | No direct risk to the colon No bowel prep No pre-test diet or medication changes needed Sampling done at home Fairly inexpensive | Can miss many polyps and some cancers Can have false-positive test results Needs to be done every year Colonoscopy will be needed if abnormal |
| Guaiac-based fecal occult blood test (gFOBT) | No direct risk to the colon No bowel prep Sampling done at home Inexpensive | Can miss many polyps and some cancers Can have false-positive test results Pre-test diet changes (and possibly medication changes) are needed Needs to be done every year Colonoscopy will be needed if abnormal |
| Stool DNA test | No direct risk to the colon No bowel prep No pre-test diet or medication changes needed Sampling done at home | Can miss many polyps and some cancers Can have false-positive test results Should be done every 3 years Colonoscopy will be needed if abnormal Still fairly new – may have insurance coverage issues |
| Colonoscopy | Can usually look at the entire colon Can biopsy and remove polyps Done every 10 years Can help find some other diseases | Can miss small polyps Full bowel prep needed Costs more on a one-time basis than other forms of testing Sedation is usually needed, in which case you will need someone to drive you home You may miss a day of work Small risk of bleeding, bowel tears, or infection |
| CT colonography (virtual colonoscopy) | Fairly quick and safe Can usually see the entire colon Done every 5 years No sedation needed | Can miss small polyps Full bowel prep needed Some false-positive test results Exposure to a small amount of radiation Can’t remove polyps during testing Colonoscopy will be needed if abnormal Still fairly new – may have insurance coverage issues |
| Flexible sigmoidoscopy | Fairly quick and safe Usually doesn’t require full bowel prep Sedation usually not used Does not require a specialist Done every 5 years | Not widely used as a screening test Looks at only about a third of the colon Can miss small polyps Can’t remove all polyps May be some discomfort Very small risk of bleeding, infection, or bowel tear Colonoscopy will be needed if abnormal |
People at average risk
The American Cancer Society believes that preventing colorectal cancer (and not just finding it early) should be a major reason for getting tested. Having colon polyps found and removed keeps some people from getting colorectal cancer. You are encouraged to have tests that have the best chance of finding both colon polyps and colon cancer if these tests are available to you and you are willing to have them. But the most important thing is to get tested, no matter which test you choose.
Starting at age 45, men and women at average risk for developing colorectal cancer should use one of the screening tests below:
Stool-based tests
- Highly sensitive fecal immunochemical test (FIT) every year
- Highly sensitive guaiac-based fecal occult blood test (gFOBT) every year
- Multi-targeted stool DNA test (mt-sDNA) every 3 years
Visual (structural) exams of the colon and rectum
- Colonoscopy every 10 years
- CT colonography (virtual colonoscopy) every 5 years
- Flexible sigmoidoscopy (FSIG) every 5 years
There are some differences between these tests to consider, but the most important thing is to get screened, no matter which test you choose. Talk to your health care provider about which tests might be good options for you, and to your insurance provider about your coverage.
If a person chooses to be screened with a test other than colonoscopy, any abnormal test result should be followed up with a timely colonoscopy.
Stool-based tests
These tests look at the stool (feces) for possible signs of colorectal cancer or polyps. These tests are typically done at home, so many people find them easier than tests like a colonoscopy. But these tests need to be done more often. And if the result from one of these stool tests is positive (abnormal), you will still need a colonoscopy to see if you have cancer.
Fecal immunochemical test (FIT)
One way to test for colorectal cancer is to look for occult (hidden) blood in the stool. The idea behind this type of test is that blood vessels in larger colorectal polyps or cancers are often fragile and easily damaged by the passage of stool. The damaged vessels usually bleed into the colon or rectum, but only rarely is there enough bleeding for blood to be seen by the naked eye in the stool.
The fecal immunochemical test (FIT) checks for hidden blood in the stool from the lower intestines. This test must be done every year, unlike some other tests (like the visual tests described below). It can be done in the privacy of your own home.
Unlike the guaiac-based fecal occult blood test (gFOBT), there are no drug or dietary restrictions before the fecal immunochemical test (FIT) test (because vitamins and foods do not affect the test), and collecting the samples may be easier. This test is also less likely to react to bleeding from the upper parts of the digestive tract, such as the stomach.
Collecting the samples: Your health care provider will give you the supplies you need for testing. Have all of your supplies ready and in one place. Supplies typically include a test kit, test cards or tubes, long brushes or other collecting devices, waste bags, and a mailing envelope. The kit will give you detailed instructions on how to collect the samples. Be sure to follow the instructions that come with your kit, as different kits might have different instructions. If you have any questions about how to use your kit, contact your health care provider’s office or clinic. Once you have collected the samples, return them as instructed in the kit.
If the test result is positive (that is, if hidden blood is found), a colonoscopy will need to be done to investigate further. Although blood in the stool can be from cancer or polyps, it can also be from other causes, such as ulcers, hemorrhoids, or other conditions.
Guaiac-based fecal occult blood test (gFOBT)
The guaiac-based fecal occult blood test (gFOBT) finds occult (hidden) blood in the stool through a chemical reaction. It works differently from the FIT, but like the FIT, the gFOBT can’t tell if the blood is from the colon or from other parts of the digestive tract (such as the stomach).
This test must be done every year, unlike some other tests (like the visual tests described below). This test can be done in the privacy of your own home. It checks more than one stool sample.
If guaiac-based fecal occult blood test (gFOBT) is chosen for colorectal screening, the American Cancer Society recommends the highly sensitive versions of this test be used.
Before the test: Some foods or drugs can affect the results of this test, so you may be instructed to avoid the following before this test:
- Non-steroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen (Advil), naproxen (Aleve), or aspirin, for 7 days before testing. (They can cause bleeding, which can lead to a false-positive result.) Note: People should try to avoid taking NSAIDs for minor aches prior to the test. But if you take these medicines daily for heart problems or other conditions, don’t stop them for this test without talking to your health care provider first.
- Vitamin C more than 250 mg a day from either supplements or citrus fruits and juices for 3 to 7 days before testing. This can affect the chemicals in the test and make the result negative, even if blood is present.
- Red meats (beef, lamb, or liver) for 3 days before testing. Components of blood in the meat may cause a positive test result.
Some people who are given the test never do it or don’t return it because they worry that something they ate may affect the test. Even if you are concerned that something you ate may alter the test, the most important thing is to get the test done.
Collecting the samples: You will get a kit with instructions from your health care provider’s office or clinic. The kit will explain how to take stool samples at home (usually samples from 3 separate bowel movements are smeared onto small paper cards). The kit is then returned to the doctor’s office or medical lab for testing.
When doing this test, have all of your supplies ready and in one place. Supplies typically include a test kit, test cards, either a brush or wooden applicator, and a mailing envelope. The kit will give you detailed instructions on how to collect the stool samples. Be sure to follow the instructions that come with your kit, as different kits might have different instructions. If you have any questions about how to use your kit, contact your health care provider’s office or clinic. Once you have collected the samples, return them as instructed in the kit.
If the test result is positive (if hidden blood is found), a colonoscopy will be needed to find the reason for the bleeding.
A fecal occult blood test (FOBT) done during a digital rectal exam in the doctor’s office (which only checks one stool sample) is not enough for proper screening, because it is likely to miss most colorectal cancers.
Stool DNA test
A stool DNA test also known as a multitargeted stool DNA test (MT-sDNA) or FIT-DNA, looks for certain abnormal sections of DNA from cancer or polyp cells and also for occult (hidden) blood. Colorectal cancer or polyp cells often have DNA mutations (changes) in certain genes. Cells with these mutations often get into the stool, where tests may be able to find them. Cologuard, the only test currently available in the US, tests for both DNA changes and blood in the stool (FIT).
This test should be done every 3 years and can be done in the privacy of your own home. It tests a full stool sample. There are no drug or dietary restrictions before taking the test.
Collecting the samples: You’ll get a kit in the mail to use to collect your entire stool sample at home. The kit will have a sample container, a bracket for holding the container in the toilet, a bottle of liquid preservative, a tube, labels, and a shipping box. The kit has detailed instructions on how to collect the sample. Be sure to follow the instructions that come with your kit. If you have any questions about how to use your kit, contact your doctor’s office or clinic. Once you have collected the sample, return it as instructed in the kit.
If the test is positive (if it finds DNA changes or blood), a colonoscopy will be need to be done.
Visual (structural) exams
These tests look at the inside of the colon and rectum for any abnormal areas that might be cancer or polyps. These tests can be done less often than stool-based tests, but they require more preparation ahead of time, and can have some risks not seen with stool-based tests.
Colonoscopy
For this test, the doctor looks at the entire length of the colon and rectum with a colonoscope, a flexible tube about the width of a finger with a light and small video camera on the end. It’s put in through the anus and into the rectum and colon. Special instruments can be passed through the colonoscope to biopsy (take a sample) or remove any suspicious-looking areas such as polyps, if needed.
CT colonography (virtual colonoscopy)
This test is an advanced type of computed tomography (CT) scan of the colon and rectum that can show abnormal areas, like polyps or cancer. Special computer programs use both x-rays and a CT scan to make 3-dimensional pictures of the inside of the colon and rectum. It does not require sedation (medicine to sleep) or any type of instrument or scope being put into the rectum or colon.
This test may be useful for some people who can’t have or don’t want to have a more invasive test such as a colonoscopy. It can be done fairly quickly, but it requires the same type of bowel prep as for a colonoscopy.
If polyps or other suspicious areas are seen on this test, a colonoscopy will still be needed to remove them or to explore the area fully.
Before the test: It’s important that the colon and rectum are emptied before this test to get the best images. You’ll probably be told to follow the same instructions to clean out the intestines as someone getting a colonoscopy.
During the test: This test is done in a special room with a CT scanner. It takes about 10 minutes. You may be asked to drink a contrast solution before the test to help identify any stool left in the colon or rectum, which helps the doctor when looking at the images. You’ll be asked to lie on a narrow table that’s part of the CT scanner, and will have a small, flexible tube put into your rectum. Air is pumped through the tube into the colon and rectum to expand them to provide better pictures. The table then slides into the CT scanner, and you’ll be asked to hold your breath for about 15 seconds while the scan is done. You’ll likely have 2 scans: one while you’re lying on your back and one while you’re on your stomach or side.
Possible side effects and complications: There are usually few side effects after this test. You may feel bloated or have cramps because of the air in the colon and rectum, but this should go away once the air passes from the body. There’s a very small risk that inflating the colon with air could injure or puncture it, but this risk is thought to be much less than with colonoscopy. Like other types of CT scans, this test also exposes you to a small amount of radiation.
Flexible sigmoidoscopy
A flexible sigmoidoscopy is similar to a colonoscopy except it doesn’t examine the entire colon. A sigmoidoscope (a flexible, lighted tube about the thickness of a finger with a small video camera on the end) is put in through the anus, into the rectum and then moved into the lower part of the colon. But the sigmoidoscope is only about 2 feet (60cm) long, so the doctor can only see less than half of the colon and the entire rectum. Images from the scope are seen on a video screen so the doctor can find and possibly remove any abnormal areas.
This test is not widely used as a screening tool for colorectal cancer in the United States.
Before the test: The colon and rectum should be emptied before this test to get the best pictures. You’ll probably be told to follow similar instructions to clean out the intestines as someone getting a colonoscopy.
During the test: A sigmoidoscopy usually takes about 10 to 20 minutes. Most people don’t need to be sedated for this test, but this might be an option you can discuss with your doctor. Sedation may make the test less uncomfortable, but you’ll need some time to recover from it and you’ll need someone with you to take you home after the test.
You’ll probably be asked to lie on a table on your left side with your knees pulled up near your chest. Before the test, your doctor may put a gloved, lubricated finger into your rectum to examine it. The sigmoidoscope is first lubricated to make it easier to put into the rectum. Air is then pumped into the colon and rectum through the sigmoidoscope so the doctor can see the inner lining better. This may cause some discomfort, but it should not be painful. Be sure to let your doctor know if you feel pain during the procedure.
If you are not sedated during the procedure, you might feel pressure and slight cramping in your lower belly. To ease discomfort and the urge to have a bowel movement, it may help to breathe deeply and slowly through your mouth. You’ll feel better after the test once the air leaves your bowels.
If any polyps are found during the test, the doctor may remove them with a small instrument passed through the scope. The polyps will be looked at in the lab. If a pre-cancerous polyp (an adenoma) or colorectal cancer is found, you’ll need to have a colonoscopy later to look for polyps or cancer in the rest of the colon.
Possible complications and side effects: You might see a small amount of blood in your bowel movements for a day or 2 after the test. More serious bleeding and puncture of the colon or rectum are possible, but they are not common.
People at increased or high risk
If you are at an increased or high risk of colorectal cancer, you might need to start colorectal cancer screening before age 45 and/or be screened more often. The following conditions make your risk higher than average:
- A personal history of colorectal cancer or adenomatous polyps
- A personal history of inflammatory bowel disease (ulcerative colitis or Crohn’s disease)
- A personal history of radiation to the abdomen (belly) or pelvic area to treat a prior cancer
- A strong family history of colorectal cancer or polyps
- A known family history of a hereditary colorectal cancer syndrome such as familial adenomatous polyposis (FAP) or Lynch syndrome (hereditary non-polyposis colon cancer or HNPCC)
The American Cancer Society does not have screening guidelines specifically for people at increased or high risk of colorectal cancer. However, some other professional medical organizations, such as the U.S. Multi-Society Task Force on Colorectal Cancer (MSTF), comprised of representatives from the American College of Gastroenterology, the American Gastroenterological Association, and the American Society for Gastrointestinal Endoscopy, do put out such guidelines 8. These guidelines are complex and are best looked at along with your health care provider. In general, these guidelines put people into several groups (although the details depend on each person’s specific risk factors).
People at increased risk for colorectal cancer
- People with one or more family members who have had colon or rectal cancer. Screening recommendations for these people depend on who in the family had cancer and how old they were when it was diagnosed. Some people with a family history will be able to follow the recommendations for average risk adults, but others might need to get a colonoscopy (and not any other type of test) more often, and possibly starting before age 45.
- People who have had certain types of polyps removed during a colonoscopy. Most of these people will need to get a colonoscopy again after 3 years, but some people might need to get one earlier (or later) than 3 years, depending on the type, size, and number of polyps.
- People who have had colon or rectal cancer. Most of these people will need to start having colonoscopies regularly about one year after surgery to remove the cancer. Other procedures like MRI or proctoscopy with ultrasound might also be recommended for some people with rectal cancer, depending on the type of surgery they had.
- People who have had radiation to the abdomen (belly) or pelvic area to treat a prior cancer. Most of these people will need to start having colorectal screening (colonoscopy or stool based testing) at an earlier age (depending on how old they were when they got the radiation). Screening often begins 5 years after the radiation was given or at age 30, whichever comes last. These people might also need to be screened more often than normal (such as at least every 3 to 5 years).
People at high risk for colorectal cancer
- People with inflammatory bowel disease (Crohn’s disease or ulcerative colitis). These people generally need to get colonoscopies (not any other type of test) starting at least 8 years after they are diagnosed with inflammatory bowel disease. Follow-up colonoscopies should be done every 1 to 3 years, depending on the person’s risk factors for colorectal cancer and the findings on the previous colonoscopy.
- People known or suspected to have certain genetic syndromes. These people generally need to have colonoscopy (not any of the other tests). Screening is often recommended to begin at a young age, possibly as early as the teenage years for some syndromes – and needs to be done much more frequently. Specifics depend on which genetic syndrome you have, and other factors. If you’re at increased or high risk of colorectal cancer (or think you might be), talk to your health care provider to learn more. Your provider can suggest the best screening option for you, as well as determine what type of screening schedule you should follow, based on your individual risk.
Colon polyps causes
Doctors don’t know the exact cause of colon polyps. Mutations in certain genes can cause cells to continue dividing even when new cells aren’t needed. These extra cells then form into a bump, which is the polyp. In the colon and rectum, this unregulated growth can cause polyps to form. Polyps can develop anywhere in your large intestine.
Risk factors for developing colon polyps
Factors that may contribute to the formation of colon polyps or cancer include:
- Age. Most people with colon polyps are 50 or older.
- Inflammatory intestinal conditions, such as ulcerative colitis and Crohn’s disease.
- Family history. You’re more likely to develop colon polyps or cancer if you have a parent, sibling or child with them. If many family members have them, your risk is even greater. In some people, this connection isn’t hereditary.
- Tobacco and alcohol use.
- Obesity and lack of exercise.
- Race. African-Americans are at higher risk of developing colon cancer.
- Type 2 diabetes that isn’t well-controlled.
Hereditary polyp disorders
Rarely, people inherit genetic mutations that cause colon polyps to form. If you have one of these genetic mutations, you are at much higher risk of developing colorectal cancer. Screening and early detection can help prevent the development or spread of these cancers.
Hereditary disorders that cause colon polyps include:
- Lynch syndrome, also called hereditary nonpolyposis colorectal cancer. People with Lynch syndrome tend to develop relatively few colon polyps, but those polyps can quickly become malignant. Lynch syndrome is the most common form of inherited colon cancer and is also associated with tumors in the breast, stomach, small intestine, urinary tract and ovaries.
- Familial adenomatous polyposis (FAP), a rare disorder that causes hundreds or even thousands of polyps to develop in the lining of your colon beginning during your teenage years. If the polyps aren’t treated, your risk of developing colon cancer is nearly 100 percent, usually before age 40. Genetic testing can help determine your risk of FAP.
- Gardner’s syndrome, a variant of FAP that causes polyps to develop throughout your colon and small intestine. You may also develop noncancerous tumors in other parts of your body, including your skin, bones and abdomen.
- MYH-associated polyposis (MAP), a condition similar to FAP that is caused by mutations in the MYH gene. People with MAP often develop multiple adenomatous polyps and colon cancer at a young age. Genetic testing can help determine your risk of MAP.
- Peutz-Jeghers syndrome, a condition that usually begins with freckles developing all over the body, including the lips, gums and feet. Then noncancerous polyps develop throughout the intestines. These polyps may become malignant, so people with this condition have an increased risk of colon cancer.
- Serrated polyposis syndrome, a condition that leads to multiple serrated adenomatous polyps in the upper part of the colon. These polyps may become malignant.
How to prevent colon polyps
You can greatly reduce your risk of colon polyps and colorectal cancer by having regular screenings. Certain lifestyle changes also can help:
- Adopt healthy habits. Include plenty of fruits, vegetables and whole grains in your diet and reduce your fat intake. Limit alcohol consumption and quit tobacco. Stay physically active and maintain a healthy body weight.
- Talk to your doctor about calcium and vitamin D. Studies have shown that increasing your consumption of calcium may help prevent recurrence of colon adenomas. But it isn’t clear whether calcium has any protective benefits against colon cancer. Other studies have shown that vitamin D may have a protective effect against colorectal cancer.
- Consider your options if you’re at high risk. If you have a family history of colon polyps, consider having genetic counseling. If you’ve been diagnosed with a hereditary disorder that causes colon polyps, you’ll need regular colonoscopies starting in young adulthood.
Your provider can order a colonoscopy or other screening tests (see the American Cancer Society Guidelines on Screening and Surveillance for the Early Detection of Colorectal Adenomas and Cancer above) :
- These tests help prevent colon cancer by finding and removing polyps before they become cancer. This may reduce the chance of developing colon cancer, or at least help catch it in its most treatable stage.
- Most people should begin these tests at age 50. Those with a family history of colon cancer or colon polyps may need to be screened at an earlier age or more often.
Taking aspirin, naproxen, ibuprofen, or similar medicines may help reduce the risk for new polyps. Be aware that these medicines can have serious side effects if taken for a long time. Side effects include bleeding in the stomach or colon and heart disease. Talk with your provider before taking these medicines.
Colon polyps signs and symptoms
Colon polyps don’t usually cause any symptoms, so most people with polyps won’t know they have them. They are often picked up during screening for colon cancer.
But some people with colon polyps experience:
- Rectal bleeding. This can be a sign of colon polyps or cancer or other conditions, such as hemorrhoids or minor tears in your anus.
- Change in stool color. Blood can show up as red streaks in your stool or make stool appear black. A change in color may also be caused by foods, medications and supplements.
- Change in bowel habits. Constipation or diarrhea that lasts longer than a week may indicate the presence of a large colon polyp. But a number of other conditions can also cause changes in bowel habits.
- Pain. A large colon polyp can partially obstruct your bowel, leading to crampy abdominal pain.
- Iron deficiency anemia. Bleeding from polyps can occur slowly over time, without visible blood in your stool. Chronic bleeding robs your body of the iron needed to produce the substance that allows red blood cells to carry oxygen to your body (hemoglobin). The result is iron deficiency anemia, which can make you feel tired and short of breath.
Colon polyps diagnosis
Colon polyps are usually found when your colon is being looked at for another reason or during screening for colon cancer.
Screening tests play a key role in detecting polyps before they become cancerous. These tests can also help find colorectal cancer in its early stages, when you have a good chance of recovery.
Screening methods include:
- Colonoscopy, the most sensitive test for colorectal polyps and cancer. If polyps are found, your doctor may remove them immediately or take tissue samples (biopsies) for analysis.
- Virtual colonoscopy (CT colonography), a minimally invasive test that uses a CT scan to view your colon. Virtual colonoscopy requires the same bowel preparation as a colonoscopy. If a polyp is found, you’ll need a colonoscopy to have it removed.
- Flexible sigmoidoscopy, in which a slender, lighted tube is inserted in your rectum to examine it and the last third of your colon (sigmoid) and rectum. If a polyp is found, you’ll need a colonoscopy to have it removed.
- Stool-based tests. This type of test works by checking for the presence of blood in the stool or assessing your stool DNA. If your stool test is positive you will need a colonoscopy.
Monitoring colon polyps
Some people with a certain type of colon polyp may be at risk of it coming back in the future (recurring).
This is uncommon, but means you’ll need examining (by colonoscopy) at regular intervals of around three to five years. This is to catch any further polyps that may develop and potentially turn into colon cancer.
Colon polyps treatment
Colorectal polyps should be removed because some can develop into cancer.
There are several methods for treating colon polyps, but the most common procedure involves physically removing the colon polyp using a wire loop. This happens during a procedure called a colonoscopy.
The colonoscopy involves passing a flexible tube called a colonoscope through your bottom and up into your colon. The colonoscope has a wire attached to it with an electric current through it. This wire is used to either burn off (cauterize) or cut off (snare) the polyp. Both of these methods are painless.
In rare cases, colon polyps may need to be treated by surgically removing part of the colon (a colectomy). This is usually only done when the colon polyp has some cell changes, if it is particularly large, or if there are a lot of colon polyps. This is surgery to remove part of the colon that has the polyps.
After the polyp or polyps have been removed, they are sent to specialists in a laboratory, who will inform your consultant if:
- the polyp has been completely removed
- there is any risk of it regrowing
- there is any cancerous change in the polyp
If there is a cancerous change in the colon polyp, you may need further treatment (depending on the degree and extent of change). Your specialist will be able to advise you on this.
Follow-up care
If you have had an adenomatous polyp or a serrated polyp, you are at increased risk of colon cancer. The level of risk depends on the size, number and characteristics of the adenomatous polyps that were removed.
You’ll need follow-up screenings for polyps. Your doctor is likely to recommend a colonoscopy:
- In five to 10 years if you had only one or two small adenomas
- In three years if you had more than two adenomas, adenomas measuring 0.4 inches (about 1 centimeter) or larger, or certain adenomas
- Within three years if you had more than 10 adenomas
- Within six months if you had a very large adenoma or an adenoma that had to be removed in pieces
It’s important to fully prepare your colon before a colonoscopy. If stool remains in the colon and obstructs your doctor’s view of the colon wall, you will likely need a follow-up colonoscopy sooner than the guidelines specify.
References- PDQ Adult Treatment Editorial Board. Colon Cancer Treatment (PDQ®): Patient Version. 2022 Apr 6. In: PDQ Cancer Information Summaries [Internet]. Bethesda (MD): National Cancer Institute (US); 2002-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK65880
- American Cancer Society Guideline for Colorectal Cancer Screening. https://www.cancer.org/cancer/colon-rectal-cancer/detection-diagnosis-staging/acs-recommendations.html
- NCCN. Colorectal cancer screening guidelines. https://www.nccn.org/professionals/physician_gls/pdf/colorectal_screening.pdf
- Shaukat A, Kahi CJ, Burke CA, Rabeneck L, Sauer BG, Rex DK. ACG Clinical Guidelines: Colorectal Cancer Screening 2021. Am J Gastroenterol. 2021 Mar 1;116(3):458-479. doi: 10.14309/ajg.0000000000001122
- US Preventive Services Task Force. Screening for Colorectal Cancer: US Preventive Services Task Force Recommendation Statement. JAMA. 2021;325(19):1965–1977. doi:10.1001/jama.2021.6238
- Qaseem, A., Crandall, C. J., Mustafa, R. A., Hicks, L. A., Wilt, T. J., Clinical Guidelines Committee of the American College of Physicians, Forciea, M. A., Fitterman, N., Horwitch, C. A., Kansagara, D., Maroto, M., McLean, R. M., Roa, J., & Tufte, J. (2019). Screening for Colorectal Cancer in Asymptomatic Average-Risk Adults: A Guidance Statement From the American College of Physicians. Annals of internal medicine, 171(9), 643–654. https://doi.org/10.7326/M19-0642
- Wolf, A.M., et al. Colorectal cancer screening for average-risk adults: 2018 guideline update from the American Cancer Society. CA: A Cancer Journal for Clinicians, 68: 250-281. https://doi.org/10.3322/caac.21457
- Updates on age to start and stop colorectal cancer screening: recommendations from the U.S. Multi-Society Task Force on Colorectal Cancer. Patel, Swati G. et al. Gastrointestinal Endoscopy, Volume 95, Issue 1, 1-15, November 15, 2021. https://doi.org/10.1016/j.gie.2021.06.012
- Colorectal Cancer Screening Tests. https://www.cancer.org/cancer/colon-rectal-cancer/detection-diagnosis-staging/screening-tests-used.html