What is conjoined twins
Conjoined twins [also known as Siamese twins named after the birth place of the original Siamese twins born in 1811 in Siam (Thailand)] are two babies who are born physically connected to each other. Conjoined twins come from the same egg but the early embryo only partially separates to form two individuals. Although two fetuses will develop from this embryo, they will remain physically connected — most often at the chest, abdomen or pelvis. Conjoined twins may also share one or more internal organs. Historically, the original Siamese twins that were born in Thailand were males and lived for nearly 62 years and fathered 22 children 1.
There are no specific signs or symptoms that indicate a conjoined twin pregnancy. As with other twin pregnancies, the uterus may grow faster than with a single fetus, and there may be more fatigue, nausea and vomiting early in the pregnancy. Conjoined twins can be diagnosed early in the pregnancy using standard ultrasound.
Many conjoined twins die in the womb (stillborn) or die shortly after birth. Some surviving conjoined twins can be surgically separated. The success of surgery depends on where the twins are joined and how many and which organs are shared, as well as the experience and skill of the surgical team.
Conjoined twins are a rare and extreme form of monozygotic twinning. The incidence of conjoined twins falls in the range of 1:50,000 to 1:100,000 live births, with 40–60% being stillborn and about 35% of the live births not surviving beyond 24 hours 2. Most of these conjoined twins are females, with a female to male ratio of 3:1 3. Imaging plays a crucial role in the antenatal and postnatal life of conjoined twins, with the initial modality for screening being ultrasound followed by other modalities such as computed tomography (CT) and/ or magnetic resonance imaging (MRI) 3.
Figure 1. Conjoined twins
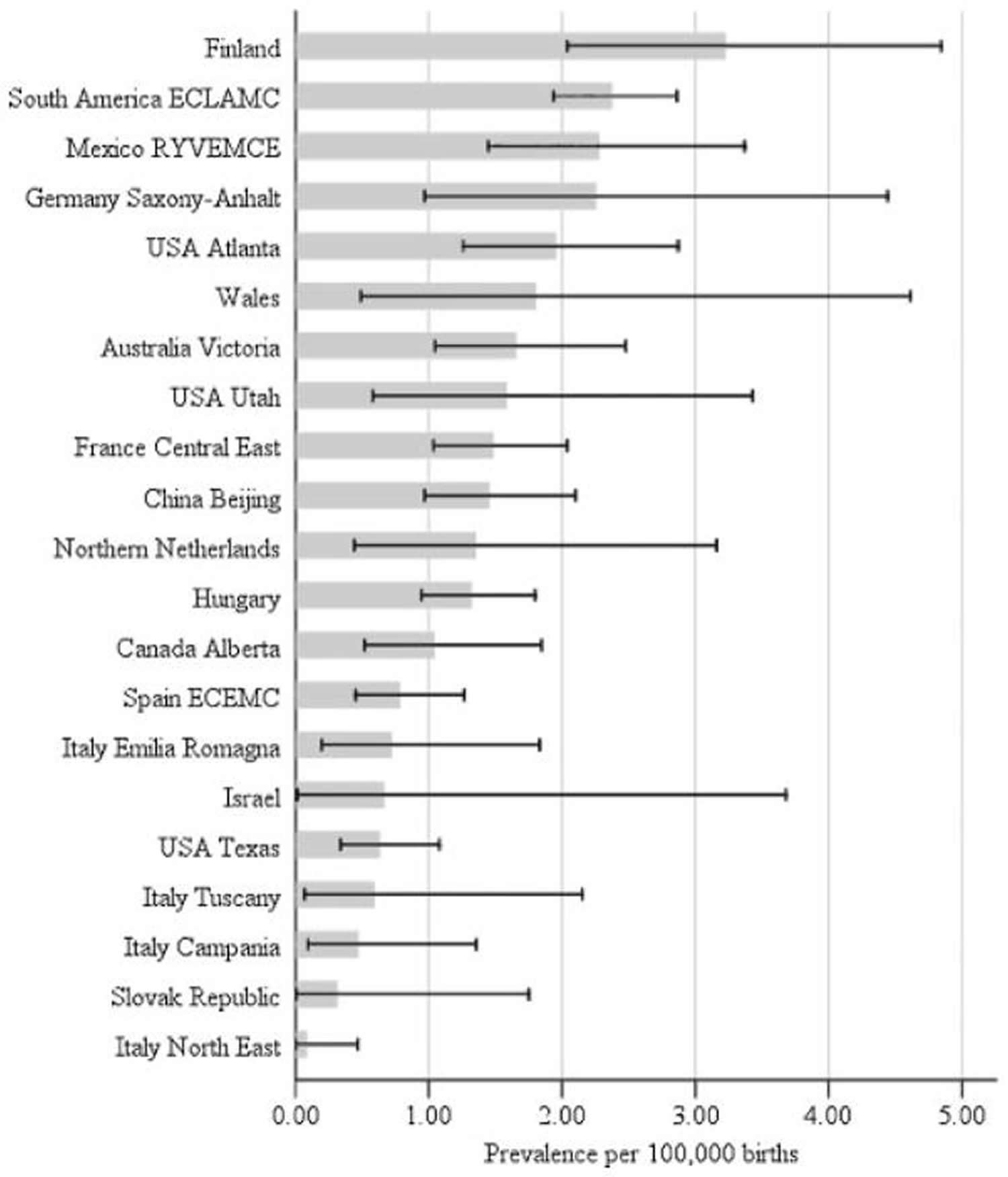
Table 1. Prevalence of Conjoined Twins Observed in Diverse Populations Studied: 1930-2010
| Prevalence | Population studied |
|---|---|
| Higher than 1:20,000 births | 1:2,800 India 4 |
| 1:4,242 Uganda 5 | |
| 1:6,500 Taiwan 6 | |
| 1:14,000 Rhodesia-Africa 7 | |
| Between 1:20,000 and 1:50,000 births | 1:20,000 Sweden 8 |
| 1:20,100 CDC-USA (CDC-Atlanta, 1973) | |
| 1:22,284 Brazil 9 | |
| 1:25,000 Maltese Islands 10 | |
| 1:30,600 China 11 | |
| 1:35,100 China 12 | |
| Between 1:50,000 and 1:100,000 births | 1:50,000 USA-Los Angeles 13 |
| 1:50,000 USA-Chicago 14 | |
| 1:55,865 24 countries WHO project 15 | |
| 1:68,500 Hungary 16 | |
| 1:74,626 South America-ECLAMC 17 | |
| 1:75,000 Sweden 18 | |
| 1:91,131 International Clearinghouse for Birth Defects Monitoring Systems 19 | |
| 1:97,560 USA-Atlanta 20 | |
| Between 1:100,000 and 1:200,000 births | 1:100,000 Japan 21 |
| 1:151,500 Spain 22 | |
| 1:166,000 New York-USA 23 | |
| 1:200,000 USA 24 | |
Figure 2. Conjoined twins prevalence
[Source 25]Recent studies on the epidemiology of conjoined twins are relatively scarce, but the prevalence does not seem to differ significantly (1.02–1.34 per 100,000 births) in Western populations 26. However, increased prevalences of 3.27:100,000 births 11 and 2.85:100,000 births 12 have been reported in two studies in Chinese populations from the same surveillance program at different times.
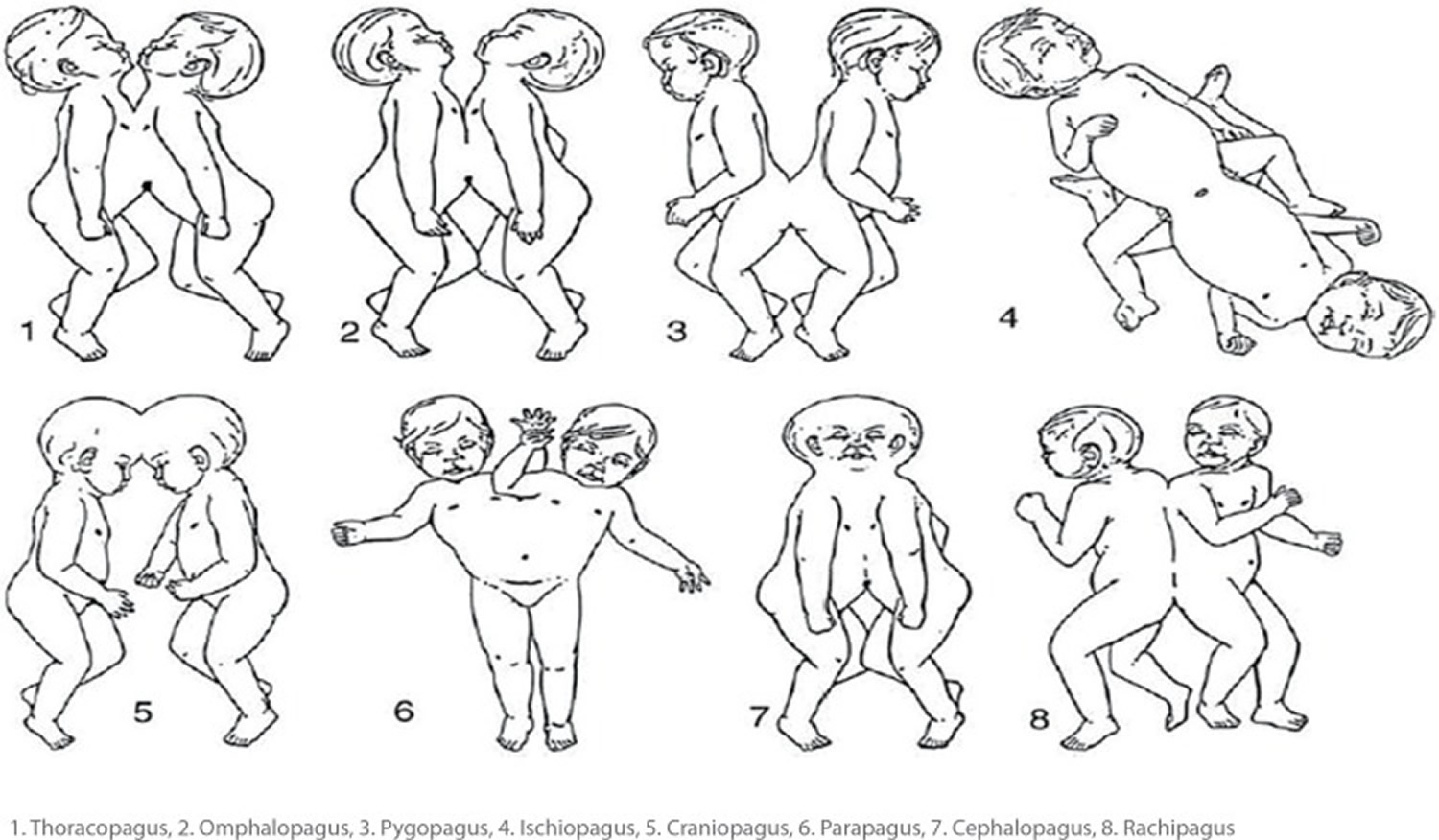
Types of conjoined twins
Conjoined twins are typically classified according to where they’re joined, usually at matching sites, and sometimes at more than one site (Figure 2). They sometimes share organs or other parts of their bodies. The specific anatomy of each pair of conjoined twins is unique.
Conjoined twins may be joined at any of these sites 2:
- Chest. Thoracopagus twins are joined face to face at the chest. They often have a shared heart and may also share one liver and upper intestine. This is one of the most common sites of conjoined twins.
- Abdomen. Omphalopagus twins are joined near the bellybutton. Many omphalopagus twins share the liver, and some share the lower part of the small intestine (ileum) and colon. They generally do not share a heart.
- Base of spine. Pygopagus twins are commonly joined back to back at the base of the spine and the buttocks. Some pygopagus twins share the lower gastrointestinal tract, and a few share the genital and urinary organs.
- Pelvis. Ischiopagus twins are joined at the pelvis, either face to face or end to end. Many ischiopagus twins share the lower gastrointestinal tract, as well as the liver and genital and urinary tract organs. Each twin may have two legs or, less commonly, the twins share two or three legs.
- Head. Craniopagus twins are joined at the back, top or side of the head, but not the face. Craniopagus twins share a portion of the skull. But their brains are usually separate, though they may share some brain tissue.
- Trunk. Parapagus twins are joined side to side at the pelvis and part or all of the abdomen and chest, but with separate heads. The twins can have two, three or four arms and two or three legs.
- Head and chest. Cephalopagus twins are joined at the face and upper body. The faces are on opposite sides of a single shared head, and they share a brain. These twins rarely survive.
- Length of spine. Rachipagus, also called rachiopagus, twins are joined back to back along the length of the spine. The defect may involve the dorsolumbar vertebral column and rarely the cervical vertebrae and the occipital bone. This type is very rare.
In rare cases, twins may be asymmetrically conjoined, with one twin smaller and less fully formed than the other.
Figure 3. Conjoined twins types
Thoracopagus conjoined twins
These types of conjoined twins are fused from the upper thorax to the umbilicus and share a common sternum, diaphragm, and upper abdominal wall. Nearly 90% of them share a common pericardial sac with some degree of cardiac fusion. The overall prognosis and success of separation is determined by the severity of cardiac fusion 27. After echocardiography, the twins are further evaluated by cardiac angiography/ magnetic resonance angiography. Most of the time, the liver is fused with a common biliary system. Better information can be obtained by multiplanar MRI and sagittal CT. The biliary system can be adequately evaluated by 99m- technetium hepatobiliary iminiodiacetic acid (99mTc-HIDA) scan. The visualization of two separate gall bladders along with the excretion of contrast into separate small intestines indicates an independent extrahepatic biliary system for each twin. In indeterminate cases, an intra-operative cholangiography or MR cholangiopancreatography may be useful. These twins have separate large intestines, pelvises and urinary tracts, along with separate sets of limbs 28.
Omphalopagus conjoined twins
These twins are united anteriorly in the umbilical region. The heart is unaffected; however, they may share the common pericardium. The majority (80%) have the common liver. The stomach and proximal small intestines are separate; however, 30% have fusion of the small intestine at the level of Meckel diverticulum in the distal ileum. Distally, the colon separates and each twin has a separate rectum and both the twins have separate sets of limbs, pelvises and urinary systems 29.
Pyopagus conjoined twins
These twins are fused posteriorly, facing away from each other with a common sacrococcyx and perineum. Although the sacral vertebrae are often fused, these twins often have separate spinal cords. They have the common anus with two separate rectums, and separate intestines proximally. These twins have two sets of limbs. If spinal cord fusion is suspected clinically and on electromyography, further assessment by angiography and MRI is needed to assess viability of separation 30.
Ischiopagus conjoined twins
Ischiopagus twins are joined from the level of the umbilicus extending caudally leading to a large fused pelvis. They have separate spinal cords and lie facing each other or end to end with the vertebral column in a straight line 31. Depending on the anatomy of the shared pelvis, these twins may be classified as: tetrapus (four), tripus (three), or bipus (two) depending on the number of legs attached to the fused pelvis. The most common are the tetrapus twins. These conjoined twins require and in-depth evaluation from an orthopedic and urologic point of view 32. These twins have complex and varied genitourinary anomalies. Initial assessment of the genitourinary system is by ultrasound, followed by a detailed study of the urinary tract and bony pelvis by multi-detector computed tomography (MDCT). The detailed ureteral pathways can be studied by using intravenous pyelography (IVP). These twins usually have a single external urethral orifice, which may be studied by cystoscopy or micturating cystouretherogram (MCUG). Renal abnormalities can be adequately assessed using functional isotope renography. MRI and ultrasound can be used to evaluate the genitals 33. When surgical separation is considered in twins with shared genitalia, one of twins will not receive any of the genitalia and will undergo a gender change. The lower digestive tract is often shared up to the anus, with anal atresia and colovesical fistula being frequent 34.
Craniopagus conjoined twins
These twins are fused in any location of the skull other than the face or foramen magnum. In more than 60% of the cases, the fusion is vertical and parietal in location. The cranium, meninges and dural venous sinuses are most often shared, with the brains being separate but connected by a neural bridge of tissue. These twins also have separate bodies and limbs 35.
Parapagus conjoined twins
Parapagus twins lie on either side with anterolateral fusion having a common umbilicus, abdomen and pelvis with a single pelvis and one or two sacra. The twins are called dithoracic, if they have separate thoraces and fusion involves only the abdomen and pelvis. The term dicephalic is used when the heads are separate and the trunks are fused. These twins may have between two to four upper limbs, while two or three lower limbs. They share the pelvis and have anal atresia, with colovesical fistula being a common finding. Using a combination of ultrasound, intravenous urography (IVU), cystography and nuclear scans, genitourinary anomalies can be adequately evaluated. For vascular anatomical studies, a combination of aortography with selective arteriography may be helpful. An adequate assessment of the musculoskeletal system may be carried out by MRI and/or CT 36.
Cephalopagus conjoined twins
These twins are rare and are fused from the vertex to the umbilicus. They usually have two faces on either side of the fused head, with one face being rudimentary. They have the common heart and liver with separate lower abdomen and pelvis. Each twin has two pairs of limbs. Separation of these twins is usually not possible.
Rachipagus conjoined twins
Rachipagus twins are very rare, and are fused posteriorly face away from each other, with the fusion terminating above the sacrum. The occiput and vertebral column are variably involved 36.
Table 2. Anomalies associated with conjoined twins
| Thoracic anomalies | Dextrocardia (in thoracopagus and dicephalic parapagus twins) Congenital diaphragmatic hernia Anomalous pulmonary venous drainage |
| Gastrointestinal anomalies | Meckel’s diverticulum Bowel atresia Anomalous hepatic venous drainage |
| Genitourinary anomalies | Duplex system Renal dysplasia Pelviureteric junction obstruction Vesicoureteric junction obstruction |
| Musculoskeletal anomalies | Congenital dislocation of hip Clubfeet Vertical tali Scoliosis |
Conjoined twins complications
Conjoined twins must be delivered by cesarean section. Many conjoined twins are stillborn or die shortly after birth. Not all surviving twins are candidates for separation surgery. The success of surgery depends on where the twins are joined and how many and which organs are shared, as well as the experience and skill of the surgical team.
The proportion of associated malformations unrelated to the site of union of conjoined twins has been reported in other studies 26 and was similar to the 63% observed in the present study. However, only two studies 26, 37 stratified the associated malformations according to the conjoined twins type. Neural tube defects were observed in more than 15% of parapagus dicephalus and diprosopus types. Genitourinary anomalies were recorded in more than 15% of thoracopagus, omphalopagus, ischiopagus, and pygo-pagus types, and musculoskeletal defects in more than 15% of thoracopagus, parapagus dicephalus, craniopagus, and ischiopagus types. Oral clefts and gastrointestinal atresias were evenly distributed. The reported proportion of associated anomalies does not differ significantly from those reported by Métneki and Czeizel 37 and the International Clearinghouse for Birth Defects Monitoring Systems 26. Although, some anomalies occurred more frequently with certain conjoined twins types, numbers are still too small to suggest specific associations and could merely represent spurious associations.
What causes conjoined twins
Identical twins (monozygotic twins) occur when a single fertilized egg splits and develops into two individuals. Eight to 12 days after conception, the embryonic layers that will split to form monozygotic twins begin to develop into specific organs and structures.
The two most common theories behind the origin of conjoined twins are the “fission theory” and “fusion theory”, with the latter gaining more acceptance. According to the fission theory, it’s believed that when the embryo splits later than this — usually between 13 and 15 days after fertilization — separation stops before the process is complete, and the resulting twins are conjoined.
While according to the fusion theory, two separate mono-ovulatary embryonic discs undergo a secondary association, somehow fuse together in early development.
What might cause either scenario to occur is unknown. Further work in epidemiology and molecular research is needed to elucidate the etiologic processes involved and associated risk factors for the development of conjoined twins.
Risk factors for conjoined twins
Because conjoined twins are so rare, and the cause isn’t clear, it’s unknown what might make some couples more likely to have conjoined twins.
Conjoined twins diagnosis
Conjoined twins can be diagnosed using standard ultrasound as early as the end of the first trimester. More-detailed ultrasounds and echocardiograms can be used about halfway through pregnancy to better determine the extent of the twins’ connection and the functioning of their organs.
If an ultrasound detects conjoined twins, a magnetic resonance imaging (MRI) scan may be done. The MRI may provide greater detail about where the conjoined twins are connected and which organs they share.
Antenatal assessment
An antenatal diagnosis of conjoined twins can be made on ultrasound in the 1st trimester. Features favoring a diagnosis of conjoined twins on antenatal ultrasound include – fetuses lying in the same constant position with heads and body parts at the same level persistently; inseparable body and skin contours; fetuses facing each other with hyperflexion of cervical spines; fewer limbs than expected; sharing of organs; and a single umbilical cord with more than 3 vessels 38.
Conjoined twins treatment
Treatment of conjoined twins depends on their unique circumstances — their health, where they’re joined, and whether they share organs or other vital structures.
Monitoring during pregnancy
If you’re carrying conjoined twins, you should be closely monitored throughout your pregnancy. You’ll likely be referred to a maternal and fetal medicine doctor who specializes in high-risk pregnancy. You may also be referred to other specialists such as pediatric surgeons, pediatric cardiologists and neonatologists.
Your doctors and others on your health care team learn as much as possible about your twins’ anatomy, functional capabilities and prognosis to form a treatment plan for your twins.
Delivery
A surgical delivery (C-section) is planned ahead of time, often two to four weeks before your due date.
After your conjoined twins are born, they’re fully evaluated. With this information, you and your health care team members can make decisions regarding their care and whether separation surgery is appropriate.
Conjoined twins separation surgery
Separation surgery is an elective procedure done two to four months after birth. Sometimes an emergency separation may be needed if one of the twins dies, develops a life-threatening condition or threatens the survival of the other twin.
Many complex factors must be considered as part of the decision to pursue separation surgery. Each set of conjoined twins presents a unique set of considerations due to variations in anatomy.
Questions may include:
- Do the twins share vital organs, such as the heart?
- Are the twins healthy enough to withstand separation surgery?
- What are the odds of successful separation?
- What type of reconstructive surgery might be needed for each twin after successful separation?
- What functional support will be needed after separation?
- What issues would the twins face if left conjoined?
Recent advances in prenatal imaging, critical care and anesthetic care have improved outcomes in separation surgery.
If surgery isn’t an option
If separation surgery isn’t possible or if you decide not to pursue the surgery, your team can help you meet the medical care needs of your twins.
If the circumstances are grave, medical comfort care — such as nutrition, fluids, human touch and pain relief — is provided.
Coping and support
Learning that your unborn twins have a major medical issue or life-threatening condition can be devastating. As a parent, you struggle with difficult decisions for your conjoined twins and the uncertain future. Outcomes can be difficult to determine, and conjoined twins who survive sometimes face tremendous obstacles.
Because conjoined twins are rare, it may be difficult to find supportive resources. Ask your health care team if medical social workers or counselors are available to help. Depending on your needs, ask for information on organizations that support parents who have children with significant physical conditions or who have lost children.
References- Sultan OM, Tawfeek AS. Conjoined twins – thoraco-omphalopagus (type A) BJR Case Rep. 2016;2:20150016.
- Mathew RP, Francis S, Basti RS, et al. Conjoined twins – role of imaging and recent advances. Journal of Ultrasonography. 2017;17(71):259-266. doi:10.15557/JoU.2017.0038. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5769666/
- Wen X, Parajuly SS, Lu Q, Xiang B, Jiang X, Tang H, et al. Thoraco-omphalopagus conjoined twins: impact of ultrasound assessment on successful surgical separation. Clin Imaging. 2013;37:138–142. https://www.ncbi.nlm.nih.gov/pubmed/23206620
- Mudaliar AL. Double monsters: A study of their circulatory system and some other anatomical abnormalities and the complications in labor. BJOG. 1930;37(4):753–768.
- Bland KG, Hammar B. Xiphopagus twins. Report of obstetric and surgical management of a case. Cent Afr J Med. 1962;8:371–375.
- Emanuel I, Huang SW, Gutman LT, Yu FC, Lin CC. The incidence of congenital malformations in a Chinese population: The Taipei Collaborative Study. Teratology. 1972;5(2):159–169.
- Zake EZ. Case reports of 16 sets of conjoined twins from a Uganda hospital. Acta Genet Med Gemellol (Roma) 1984;33(1):75–80.
- Ryden AL. Kasuistischur beitrog zur kenntris der gerburtron thoracapagen. Zbl Gynak. 1934;58:972–975.
- Berezowski AT, Duarte G, Rodrigues R, de Carvalho Cavalli R, de Olivera Cardoso dos Santos R, de Moraes Villela de Andrade Vicente YA, Galli Sorita Tazima M, de F. Conjoined twins: An experience of a tertiary hospital in Southeast Brazil. Rev Bras Ginecol Obstet. 2010;32(2):61–65.
- Savona-Ventura C, Grima S, Buttigieg GG. Conjoint twinning in the Maltese Islands. J Obstet Gynaecol. 2009;29(7):599–604.
- [Epidemiological survey of conjoined twins in China]. Liang J, Xu CI, Wang Y. Hua Xi Yi Ke Da Xue Xue Bao. 1999 Mar; 30(1):56-8. https://www.ncbi.nlm.nih.gov/pubmed/12205925/
- [An epidemiological study on conjoined twins in China, from 1996 to 2004]. Tang Y, Zhu J, Zhou GX, Dai L, Wang YP, Liang J. Zhonghua Yu Fang Yi Xue Za Zhi. 2007 Jun; 41 Suppl():146-9. https://www.ncbi.nlm.nih.gov/pubmed/17767883/
- Robertson EG. Craniopagus parietalia. Arch Neurol Psychiatry. 1953;70:189–205.
- Potter EL. Pathology of the fetus and infant. Chicago: Chicago Year Book Medical Publishers; 1961. p. 217.
- Stevenson AD, Johnston HA, Stewart MIP, et al. Congenital malformations. Bull World Health Org. 1966;34(Suppl):9–127.
- Métneki J, Czeizel A. Conjoined twins in Hungary, 1970–1986. Acta Genet Med Gemellol (Roma) 1989;38(3–4):285–299.
- The epidemiology of conjoined twins in Latin America. Castilla EE, Lopez-Camelo JS, Orioli IM, Sánchez O, Paz JE. Acta Genet Med Gemellol (Roma). 1988; 37(2):111-8.
- Conjoined twinning in Sweden. Källén B, Rybo G. Acta Obstet Gynecol Scand. 1978; 57(3):257-9.
- Conjoined twins–an epidemiological study based on 312 cases. The International Clearinghouse for Birth Defects Monitoring Systems. Acta Genet Med Gemellol (Roma). 1991; 40(3-4):325-35.
- Conjoined twins in the united states, 1970-1977. Edmonds LD, Layde PM. Teratology. 1982 Jun; 25(3):301-8. https://www.ncbi.nlm.nih.gov/pubmed/7112433/
- Imaizumi Y. Conjoined twins in Japan, 1979–1985. Acta Genet Med Gemellol (Roma) 1988;37(3–4):339–345. https://www.ncbi.nlm.nih.gov/pubmed/3254024
- Epidemiological and clinical analysis of a consecutive series of conjoined twins in Spain. Martínez-Frías ML, Bermejo E, Mendioroz J, Rodríguez-Pinilla E, Blanco M, Egüés J, Félix V, García A, Huertas H, Nieto C, López JA, López S, Paisán L, Rosa A, Vázquez MS. J Pediatr Surg. 2009 Apr; 44(4):811-20. https://www.ncbi.nlm.nih.gov/pubmed/19361646/
- Milham S. Symmetrical conjoined twins: An analysis of the birth records of twenty-two sets. J Pediatr. 1966;69(4):643–647. https://www.ncbi.nlm.nih.gov/pubmed/5921342
- Studies on symmetrically conjoined twins. Bender C. J Pediatr. 1967 Jun; 70(6):1010-1. https://www.ncbi.nlm.nih.gov/pubmed/6027285/
- MUTCHINICK OM, LUNA-MUÑOZ L, AMAR E, et al. Conjoined Twins: A Worldwide Collaborative Epidemiological Study of the International Clearinghouse for Birth Defects Surveillance and Research. American journal of medical genetics Part C, Seminars in medical genetics. 2011;0(4):274-287. doi:10.1002/ajmg.c.30321. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4457318/
- Conjoined twins–an epidemiological study based on 312 cases. The International Clearinghouse for Birth Defects Monitoring Systems. Acta Genet Med Gemellol (Roma). 1991; 40(3-4):325-35. https://www.ncbi.nlm.nih.gov/pubmed/1821509/
- Spencer R. Anatomic description of conjoined twins: a plea for standardized terminology. J Pediatr Surg. 1996;31:941–944. https://www.ncbi.nlm.nih.gov/pubmed/8811563
- Spitz L, Crabbe DCG, Kiely EM. Separation of thoraco-omphalopagus conjoined twins with complex hepato-biliary anatomy. J Pediatr Surg. 1997;32:787–789. https://www.ncbi.nlm.nih.gov/pubmed/9165482
- Aneja A, Rajanna DK, Reddy VN, Mayilvavaganan KR, Pujar P. Conjoined twins: a rare case of thoraco-omphalopagus. J Clin Diagn Res. 2013;7:1471–1472. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3749668/
- Spitz L. Conjoined twins. Br J Surg. 1996;83:1028–1030. https://www.ncbi.nlm.nih.gov/pubmed/8869298
- Spencer R. Minimally united ischiopagus twins: infraumbilical union with cloacal anomalies. J Pediatr Surg. 1996;31:1538–1545. https://www.ncbi.nlm.nih.gov/pubmed/8943118
- Albert MC, Drummond DS, O’Neill J, Watts H. The orthopedic management of conjoined twins: a review of 13 cases and report of 4 cases. J Pediatr Orthop. 1992;12:300–307. https://www.ncbi.nlm.nih.gov/pubmed/1572992
- Wilcox DT, Quinn FM, Spitz L, Kiely EM, Ransley PG. Urological problems in conjoined twins. Br J Urol. 1998;81:905–910. https://www.ncbi.nlm.nih.gov/pubmed/9666780
- Spitz L, Capps SN, Kiely EM. Xiphoomphaloischiopagus tripus conjoined twins: successful separation following abdominal wall expansion. J Pediatr Surg. 1991;26:26–29. https://www.ncbi.nlm.nih.gov/pubmed/1826029
- Jansen O, Mehrabi VA, Sartor K. Neuroradiological findings in adult cranially conjoined twins. Case report. J Neurosurg. 1998;89:635–639. https://www.ncbi.nlm.nih.gov/pubmed/9761059
- Spitz L, Stringer MD, Kiely EM, Ransley PG, Smith P. Separation of brachio-thoraco-omphaloischiopagus bipus conjoined twins. J Pediatr Surg. 1994;29:477–481. https://www.ncbi.nlm.nih.gov/pubmed/8014797
- Métneki J, Czeizel A. Conjoined twins in Hungary, 1970–1986. Acta Genet Med Gemellol (Roma) 1989;38(3–4):285–299. https://www.ncbi.nlm.nih.gov/pubmed/2631499
- Barth RA, Filly RA, Goldberg JD, Moore P, Silverman NH. Conjoined twins: prenatal diagnosis and assessment of associated malformations. Radiology. 1990;177:201–207. https://www.ncbi.nlm.nih.gov/pubmed/2204966