What is Cushing syndrome
Cushing syndrome (also sometimes called Cushing’s syndrome) is a condition where your body is exposed to too much of the hormone cortisol. This can be because your body is making too much cortisol, or because you have taken a lot of oral corticosteroid medicines. If you have Cushing’s syndrome, it is treatable. However Cushing’s syndrome can be serious if it’s not treated. The condition is named after Harvey Cushing, an eminent American neurosurgeon, who described the first patients with this condition in 1912.
Cortisol is a hormone that is made by the adrenal glands. You have two adrenal glands, one sitting on the top of each kidney.
Cortisol is a hormone that it is vital for life.
Cortisol hormone has several important functions including:
- Cortisol helps to regulate blood pressure
- Cortisol helps to regulate the immune system
- Cortisol helps to balance the effect of insulin to keep blood sugar normal by converting fat, carbohydrates, and proteins into energy
- Cortisol helps the body to respond to stress
Cortisol is involved in many different parts of your body. It is produced all day, and especially during times of stress.
- Some people with Cushing’s syndrome have a benign tumor in part of the brain. This tumor tells the adrenal glands to release cortisol. This condition is known as Cushing’s disease.
- Other people develop Cushing’s syndrome from taking steroid medication for a long time. If you have Cushing’s syndrome as a result of taking steroid medication, do not stop taking it suddenly, as you could become very unwell. Talk to your doctor.
- Cushing’s syndrome can also be caused by a tumor of the adrenal gland, overgrowth of the adrenal glands, or occasionally a tumor somewhere else in the body.
Cushing’s syndrome is uncommon. It mostly affects people who have been taking steroid medicine, especially steroid tablets, for a long time. Steroids contain a man-made version of cortisol. For example taking a steroid such as prednisolone for asthma, arthritis or colitis.
Very rarely, it can be caused by the body producing too much cortisol. This is usually due to:
- a growth (tumor) in the pituitary gland in the brain
- a tumor in one of the adrenal glands above the kidneys
The tumors are usually non-cancerous (benign). Far more women than men suffer from Cushing’s syndrome but it isn’t known why; it is most commonly diagnosed between the ages of 30 to 40. Although it is rare in children, some as young as 6 have been diagnosed. There are no environmental triggers known and it’s not hereditary.
Spontaneous Cushing’s syndrome, originating from within the body is rare, but occurs when the adrenal glands are making too much of a hormone called cortisol (the body’s natural glucocorticoid steroid hormone). The quoted incidence of Cushing’s syndrome is 1 in 200,000 but it is now being found more frequently when it is specifically investigated. The difficulty is that the symptoms of Cushing’s syndrome can be very wide ranging and thus the diagnosis may not necessarily be considered; it can be difficult to establish, at the earlier stages and this can cause a delay in diagnosis.
The commonest cause of spontaneous Cushing’s syndrome (around 70%) is a small benign tumor (growth) of the pituitary gland (a small gland at the base of the brain, behind the bridge of the nose). This produces the hormone called ACTH, (adrenocorticotrophic hormone), that goes through the blood stream to the adrenal glands and causes them to release too much cortisol. In this case there is a good chance that an operation on your pituitary gland will solve the problem. Alternatively, there could be a small growth in another part of your body which is having the same effect (this is called ectopic ACTH). If so, removing this growth will usually solve the problem. Lastly, there may be a small growth in one of the adrenal glands themselves, in which case an operation will be needed to remove that gland. In some circumstances it may be necessary to remove both adrenal glands to solve the problem.
Strictly speaking, if the source of the problem is the pituitary gland, then the correct name is Cushing’s Disease.
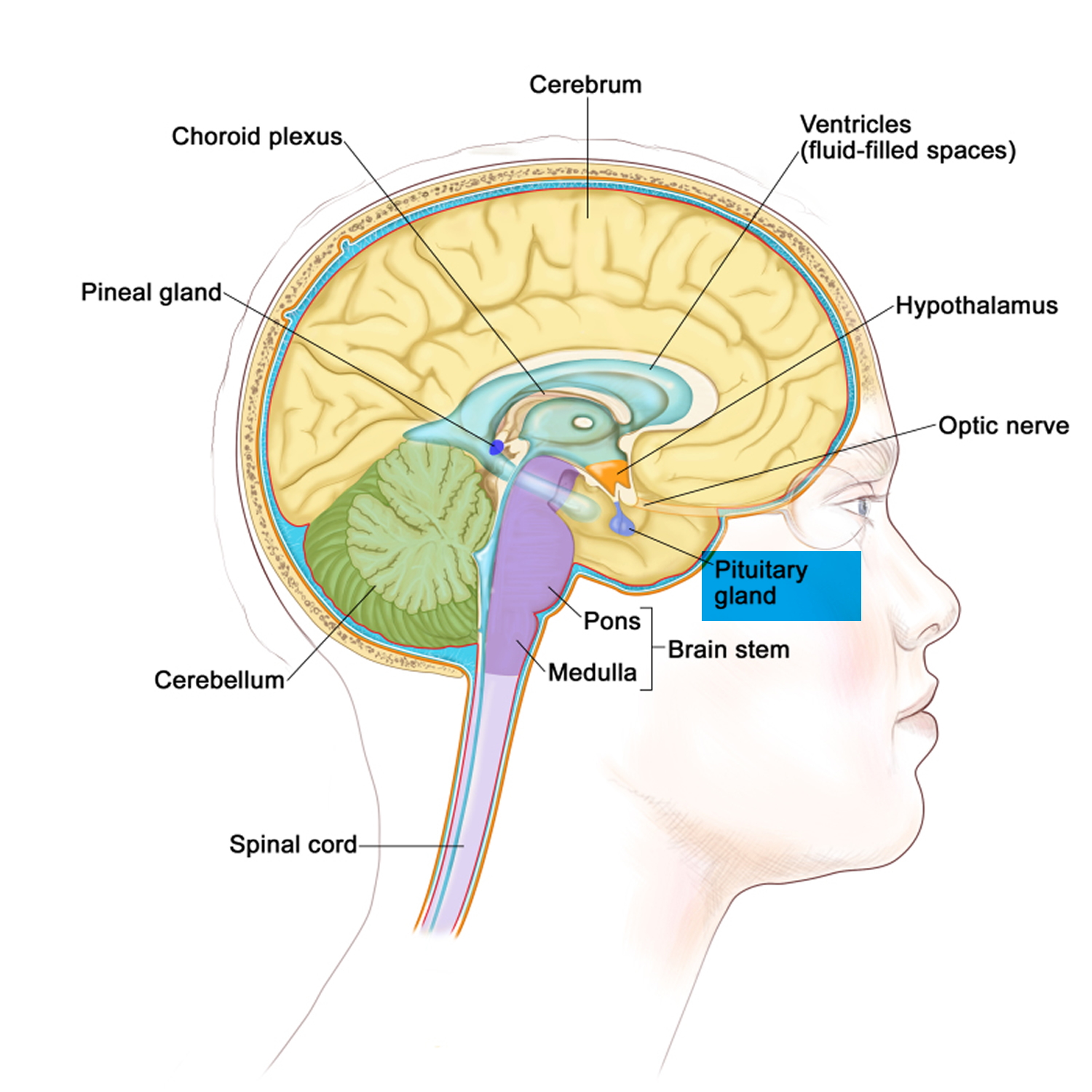
Figure 1. The pituitary gland location
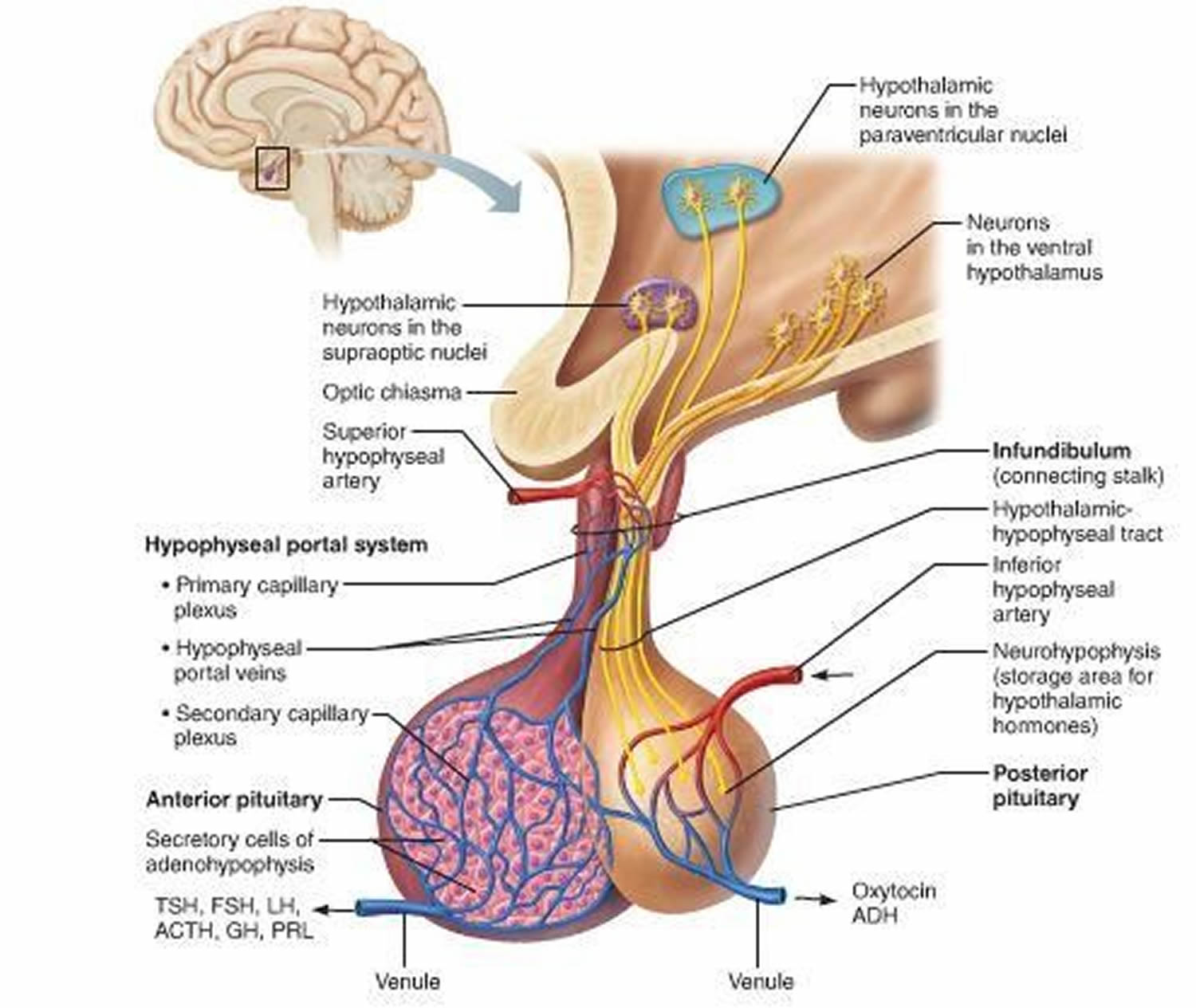
Figure 2. Pituitary gland
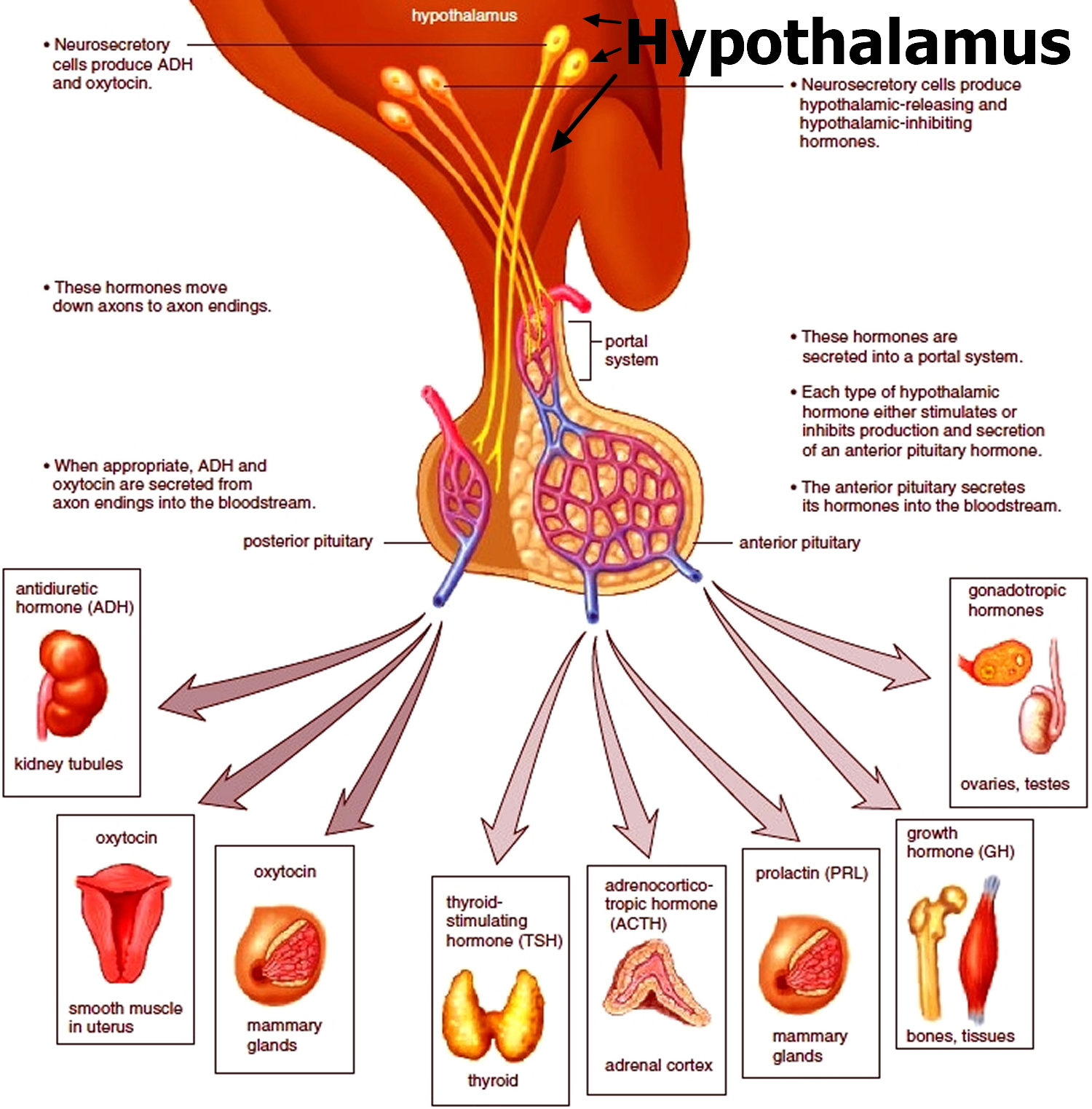
Figure 3. The hypothalamus and pituitary gland (anterior and posterior) endocrine pathways and target organs
See a doctor if you have symptoms of Cushing’s syndrome, especially if you’re taking steroids.
Don’t stop taking your medicine without getting medical advice.
Lots of things can cause similar symptoms to Cushing’s syndrome, so it’s a good idea to get checked to find out what the problem is.
Cushing syndrome vs Cushing disease
Cushing disease is caused by a tumor or excess growth (hyperplasia) of the pituitary gland that produces too much adrenocorticotropic hormone (ACTH). The excess adrenocorticotropic hormone (ACTH) stimulates the excessive production and release of cortisol by your adrenal glands. Too much ACTH causes the adrenal glands to make too much cortisol.
A type of pituitary tumor called an adenoma is the most common cause of Cushing disease. An adenoma is a benign tumor (not a cancer).
Cushing disease can also occur with excess growth of the pituitary gland. The excessive growth, known as hyperplasia, also causes the release of too much ACTH, which then leads to over-production of cortisol.
Cushing syndrome and Cushing disease are both conditions that occur when the body produces too much cortisol. Cortisol is normally released during stressful situations. It controls the body’s use of carbohydrates, fats, and proteins. It also reduces the immune system’s response to swelling (inflammation).
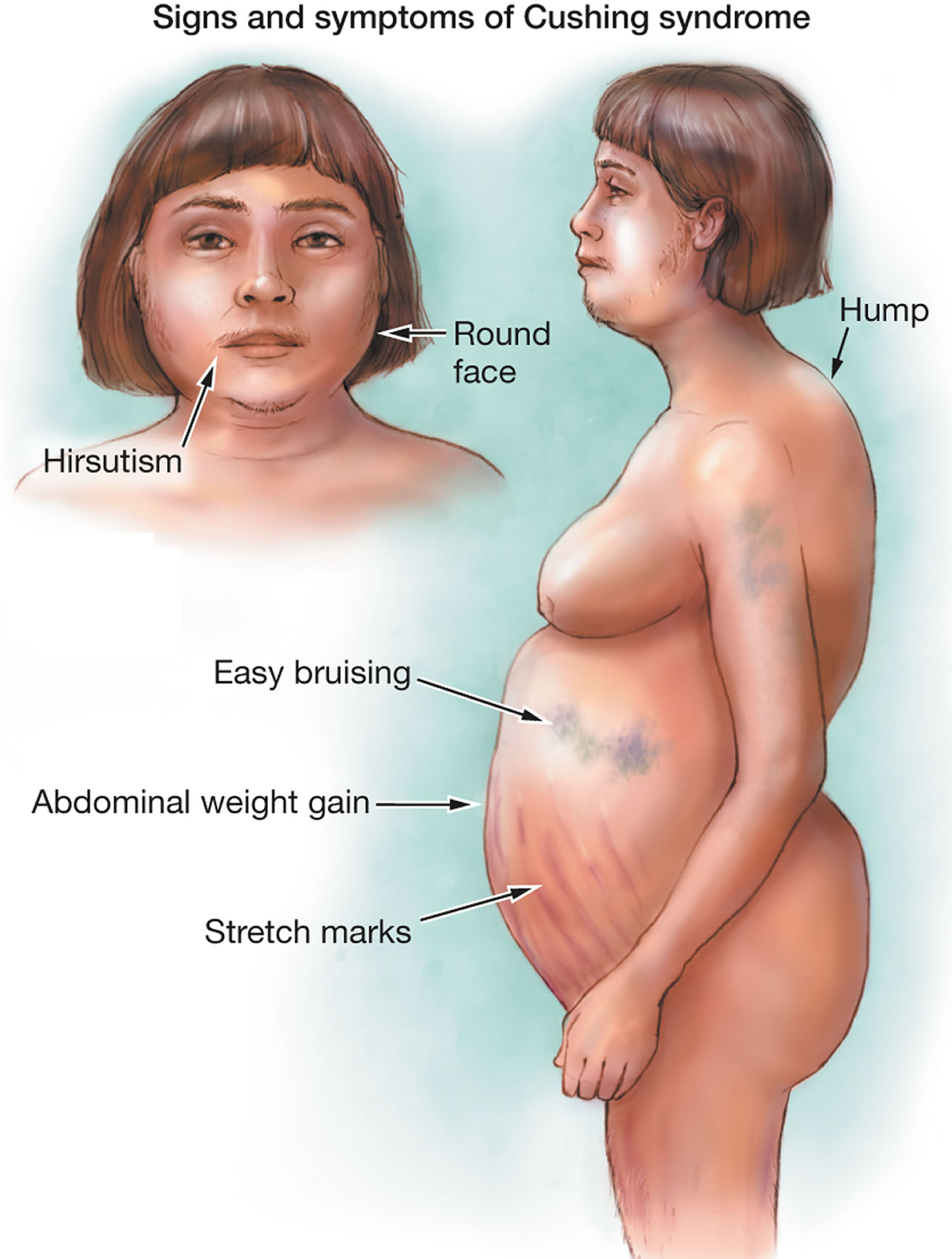
Both Cushing syndrome and Cushing disease cause the same symptoms, including red lines on the abdomen, abdominal weight gain, and roundness to the face.
What causes Cushing disease?
Cushing disease is a relatively rare condition, only affecting 10 to 15 people per million every year. It is more common in women and occurs most often in people between the ages of 20 and 50. Adenoma is the most common cause of Cushing disease. Adenoma is a pituitary tumor that is almost always benign. The tumors can be hard to diagnose, because they are quite small, so many people who have Cushing disease have a delayed diagnosis. Having an endocrinologist help with the diagnostic process can improve the chances of a prompt, successful diagnosis for patients who have symptoms of Cushing syndrome and Cushing disease.
Signs and symptoms of Cushing disease (except for the cause, both Cushing syndrome and Cushing disease cause the same signs and symptoms)
Symptoms of Cushing disease include:
- Upper body obesity (above the waist) and thin arms and legs
- Round, red, full face (moon face)
- Slow growth rate in children
Skin changes that are often seen include:
- Acne or skin infections
- Purple stretch marks (1/2 inch or 1 centimeter or more wide), called striae, on the skin of the abdomen, thighs, upper arms, and breasts
- Thin skin with easy bruising, most commonly on the arms and hands
Muscle and bone changes include:
- Backache, which occurs with routine activities
- Bone pain or tenderness
- Collection of fat between the shoulders (buffalo hump)
- Weakening of the bones, which leads to rib and spine fractures
- Weak muscles
Women may have:
- Excess hair growth on the face, neck, chest, abdomen, and thighs
- Menstrual cycle that becomes irregular or stops
Men may have:
- Decreased or no desire for sex (low libido)
- Erection problems
Other symptoms or problems may include:
- Mental changes, such as depression, anxiety, or changes in behavior
- Fatigue
- Frequent infections
- Headache
- Increased thirst and urination
- High blood pressure
- Diabetes
Cushing disease possible complications
Health problems that may result from Cushing disease include:
- Compression fractures in the spine
- Diabetes
- High blood pressure
- Infections
- Kidney stones
- Mood or other psychiatric problems
How is Cushing disease treated?
Untreated, Cushing disease can cause severe illness, even death. Removal of the tumor may lead to full recovery, but the tumor can grow back.
The first line therapy is surgical removal of the tumor. Cure rates with an experienced pituitary surgeon are about 90% in people with small tumors. A patient will typically have trans-sphenoidal microsurgery through the nasal sinuses. During the recovery process from surgery, you may need cortisol replacement treatments because the pituitary needs time to start making ACTH again.
People who are not cured usually have repeat surgery. When surgery does not work, radiation therapy may treat any remaining tumor mass. Several medications to block the adrenal glands (such as ketoconazole, metyrapone or mitotane) are often used while waiting for radiation to have an effect. In some cases, a type of drug called a dopamine agonist can reduce ACTH levels and cortisol production. Pasireotide (given by injection under the skin) can also reduce ACTH levels and cortisol production. Mifepristone is another medication that stops cortisol from working on the body. The adrenal glands are rarely removed.
If all of the above treatments are not successful, the adrenal glands may need to be removed to stop the high levels of cortisol from being produced. Removal of the adrenal glands can cause the pituitary tumor to get much bigger (Nelson syndrome).
Cushing syndrome causes
There are two types of Cushing syndrome:
- Exogenous (caused by factors outside the body) and
- Endogenous (caused by factors within the body).
The symptoms for both are the same. The only difference is how they are caused.
The most common is exogenous Cushing syndrome and is found in people taking cortisol-like medications such as prednisone. These drugs are used to treat inflammatory disorders such as asthma and rheumatoid arthritis. They also suppress the immune system after an organ transplant. This type of Cushing is temporary and goes away after the patient has finished taking the cortisol-like medications.
Endogenous Cushing syndrome, in which the adrenal glands produce too much cortisol, is uncommon. It usually comes on slowly and can be difficult to diagnose. This type of Cushing syndrome is most often caused by hormone-secreting tumors of the adrenal glands or the pituitary, a gland located at the base of the brain. In the adrenal glands, the tumor (usually non-cancerous) produces too much cortisol. In the pituitary, the tumor produces too much ACTH—the hormone that tells the adrenal glands to make cortisol. When the tumors form in the pituitary, the condition is often called Cushing disease.
Most tumors that produce ACTH originate in the pituitary but sometimes non-pituitary tumors, usually in the lungs, can also produce too much ACTH and cause Cushing syndrome.
Cushing syndrome signs and symptoms
Symptoms of Cushing’s syndrome can start suddenly or gradually. They tend to get slowly worse if not treated.
One of the main signs is weight gain and more body fat, such as:
- increased fat on your chest, shoulders and neck and tummy, but slim arms and legs
- a build-up of fat on the back of your neck and shoulders – known as a “buffalo hump”
- a red, puffy, rounded face
Other symptoms include:
- skin that bruises easily
- skin problems like slow healing of wounds
- large purple stretch marks on the tummy, hips and thighs
- weakness in your upper arms and thighs due to muscle loss
- a low libido and fertility problems
- irregular periods
- feeling tired or emotional
- depression and mood swings
- brittle bones or thin bones (osteoporosis)
- too much facial hair in women
Cushing’s syndrome can also cause high blood pressure (hypertension) and high blood sugar or diabetes, which can be serious if not treated.
Other symptoms include more hair on the face and body and a change in menstrual periods for women, and lower libido or erectile dysfunction for men.
Women with Cushing syndrome may experience:
- Thicker or more visible body and facial hair (hirsutism)
- Irregular or absent menstrual periods
Men with Cushing syndrome may experience:
- Decreased libido
- Decreased fertility
- Erectile dysfunction
Other signs and symptoms include:
- Severe fatigue
- Depression, anxiety and irritability
- Loss of emotional control
- Cognitive difficulties
- New or worsened high blood pressure
- Headache
- Bone loss, leading to fractures over time
- In children, impaired growth
Cushing syndrome diagnosis
Cushing’s syndrome can be hard to diagnose because it can look like other things. Your doctor may suspect Cushing’s syndrome if you have typical symptoms and are taking steroid medicine.
If you’re not taking steroids, it can be difficult to diagnose because the symptoms can be similar to other conditions.
Your doctor will talk to you, examine you and may arrange a number of tests of your blood, urine and saliva.
If Cushing’s syndrome is suspected, the amount of cortisol in your body can be measured in your:
- 24-hour urine cortisol
- Dexamethasone suppression test (low dose)
- Salivary cortisol levels (early morning and late at night).
Three tests are commonly used to diagnose Cushing syndrome. One of the most sensitive tests measures cortisol levels in the saliva between 11:00 p.m. and midnight. A sample of saliva is collected in a small plastic container and sent to the laboratory for analysis. In healthy people, cortisol levels are very low during this period of time. In contrast, people with Cushing syndrome have high levels.
Cortisol levels can also be measured in urine that has been collected over a 24-hour period.
In another screening test, people with suspected Cushing syndrome have their cortisol levels measured the morning after taking a late-night dose of dexamethasone, a laboratory-made steroid. Normally, dexamethasone causes cortisol to drop to a very low level, but in people with Cushing syndrome, this doesn’t happen.
If these tests show a high level of cortisol, you may be referred to a specialist in hormone conditions (endocrinologist) to confirm or rule out Cushing’s syndrome.
You may also need other tests or scans to find out the cause.
Other tests that may be done include any of the following:
- Fasting blood glucose and A1C to test for diabetes
- Lipid and cholesterol testing
- Bone mineral density scan to check for osteoporosis
- Blood ACTH level
- Brain MRI
- Corticotropin-releasing hormone test, which acts on the pituitary gland to cause the release of ACTH
- Dexamethasone suppression test (high dose)
- Inferior petrosal sinus sampling (IPSS) — measures ACTH levels in the veins that drain the pituitary gland compared to the veins in the chest. This test can help determine whether the cause of endogenous Cushing syndrome is rooted in the pituitary or somewhere else. For the test, blood samples are taken from the petrosal sinuses — veins that drain the pituitary glands.A thin tube is inserted into your upper thigh or groin area while you’re sedated, and threaded to the petrosal sinuses. Levels of ACTH are measured from the petrosal sinuses, and from a blood sample taken from the forearm.If ACTH is higher in the sinus sample, the problem stems from the pituitary. If the ACTH levels are similar between the sinus and forearm, the root of the problem lies outside of the pituitary gland.
Cushing syndrome test
Dexamethasone suppression test (also called ACTH suppression test or Cortisol suppression test) measures whether adrenocorticotrophic hormone (ACTH) secretion by the pituitary can be suppressed.
How the Test is Performed
During this test, you will receive dexamethasone. This is a strong man-made (synthetic) glucocorticoid medicine. Afterward, your blood is drawn so that the cortisol level in your blood can be measured.
There are two different types of dexamethasone suppression tests: low dose and high dose. Each type can either be done in an overnight (common) or standard (3-day) method (rare). There are different processes that may be used for either test. Examples of these are described below.
Common:
- Low-dose overnight — You will get 1 milligram (mg) of dexamethasone at 11 p.m., and a health care provider will draw your blood the next morning at 8 a.m. for a cortisol measurement.
- High-dose overnight — The provider will measure your cortisol on the morning of the test. Then you will receive 8 mg of dexamethasone at 11 p.m. Your blood is drawn the next morning at 8 a.m. for a cortisol measurement.
Rare:
- Standard low-dose — Urine is collected over 3 days (stored in 24-hour collection containers) to measure cortisol. On day 2, you will get a low dose (0.5 mg) of dexamethasone by mouth every 6 hours for 48 hours.
- Standard high-dose — Urine is collected over 3 days (stored in 24-hour collection containers) for measurement of cortisol. On day 2, you will receive a high dose (2 mg) of dexamethasone by mouth every 6 hours for 48 hours.
Read and follow the instructions carefully. The most common cause of an abnormal test result is when instructions are not followed.
How to Prepare for the Test
The provider may tell you to stop taking certain medicines that can affect the test, including:
- Antibiotics
- Anti-seizure drugs
- Medicines that contain corticosteroids, such as hydrocortisone, prednisone
- Estrogen
- Oral birth control (contraceptives)
- Water pills (diuretics)
How the Test will Feel
When the needle is inserted to draw blood, some people feel moderate pain. Others feel only a prick or stinging. Afterward, there may be some throbbing or slight bruising. This soon goes away.
Why the Test is Performed
This test is done when the provider suspects that your body is producing too much cortisol. It is done to help diagnose Cushing syndrome and identify the cause.
The low-dose test can help tell whether your body is producing too much ACTH. The high-dose test can help determine whether the problem is in the pituitary gland (Cushing disease).
Dexamethasone is a man-made (synthetic) steroid that is similar to cortisol. It reduces ACTH release in normal people. Therefore, taking dexamethasone should reduce ACTH level and lead to a decreased cortisol level.
If your pituitary gland produces too much ACTH, you will have an abnormal response to the low-dose test. But you can have a normal response to the high-dose test.
Normal Results
Cortisol level should decrease after you receive dexamethasone.
Low dose:
- Overnight — 8 a.m. plasma cortisol lower than 1.8 micrograms per deciliter (mcg/dL) or 50 nanomoles per liter (nmol/L)
- Standard — Urinary free cortisol on day 3 lower than 10 micrograms per day (mcg/day) or 280 nmol/L
High dose:
- Overnight — greater than 50% reduction in plasma cortisol
- Standard — greater than 90% reduction in urinary free cortisol
Normal value ranges may vary slightly among different laboratories. Some labs use different measurements or may test different specimens. Talk to your doctor about the meaning of your specific test results.
What Abnormal Results Mean
An abnormal response to the low-dose test may mean that you have abnormal release of cortisol (Cushing syndrome). This could be due to:
- Adrenal tumor that produces cortisol
- Pituitary tumor that produces ACTH
- Tumor in the body that produces ACTH (ectopic Cushing syndrome)
The high-dose test can help tell a pituitary cause (Cushing disease) from other causes. An ACTH blood test may also help identify the cause of high cortisol.
Abnormal results vary based on the condition causing the problem.
Cushing syndrome caused by an adrenal tumor:
- Low-dose test — no decrease in blood cortisol
- ACTH level — low
- In most cases, the high-dose test is not needed
Ectopic Cushing syndrome:
- Low-dose test — no decrease in blood cortisol
- ACTH level — high
- High-dose test — no decrease in blood cortisol
Cushing syndrome caused by a pituitary tumor (Cushing disease)
- Low-dose test — no decrease in blood cortisol
- High-dose test — expected decrease in blood cortisol
False test results can occur due to many reasons, including different medicines, obesity, depression, and stress.
Risks of Dexamethasone suppression test
Veins and arteries vary in size from one patient to another, and from one side of the body to the other. Obtaining a blood sample from some people may be more difficult than from others.
Other risks associated with having blood drawn are slight, but may include:
- Excessive bleeding
- Fainting or feeling lightheaded
- Hematoma (blood accumulating under the skin)
- Infection (a slight risk any time the skin is broken).
Cushing syndrome treatment
The treatment depends on the cause. Cushing’s syndrome usually gets better with treatment, although it might take a long time to recover completely. Remember to be patient. You didn’t develop Cushing syndrome overnight, and your symptoms won’t disappear overnight, either. In the meantime, these tips may help you on your journey back to health.
Treatment depends on what’s causing it.
If Cushing syndrome is caused by taking steroids:
- If you are taking steroids, then you and your doctor will need to talk about whether it is possible to reduce the dose or not. Your steroid dose will probably be gradually reduced or stopped
Exogenous Cushing syndrome goes away after a patient stops taking the cortisol-like medications they were using to treat another condition. Your doctor will determine when it is appropriate for you to slowly decrease and eventually stop using the medication.
If Cushing syndrome is caused by a tumor, treatment may include:
- surgery to remove the tumor
- radiotherapy to destroy the tumor
- medicines to reduce the effect of cortisol on your body
For endogenous Cushing syndrome, the initial approach is almost always surgery to remove the tumor that is causing high cortisol levels. Although surgery is usually successful, some people may also need medications that lower cortisol or radiation therapy to destroy remaining tumor cells. Some people must have both adrenal glands removed to control Cushing syndrome.
If there are other reasons as to why you have Cushing’s syndrome, then you may be advised to have treatment such as surgery, radiotherapy, chemotherapy or other medication to stop your body taking too much cortisol.
Speak to your doctor about the benefits and risks of the different treatment options.
Medical therapy of Cushing syndrome
The role of medical treatment of Cushing syndrome is an important one. It is the routine practice of many groups to pre-treat Cushing syndrome patients prior to surgical treatment to reverse the hypercortisolaemia and its metabolic sequelae, and to hopefully reduce the complications of the definitive procedure. Similarly, medical treatment is desirable in patients with Cushing’s disease whilst awaiting for pituitary radiotherapy to take effect. In patients where surgery and/or radiotherapy have failed, medical management is often essential prior to (or long-term as an alternative to) bilateral adrenalectomy. Sometimes, in the occult ectopic ACTH syndrome, it may not always be possible to identify the source of secretion, and therefore medical management is desirable pending re-investigation. Finally, medical therapy is helpful as a palliative modality in patients with metastatic disease causing Cushing’s syndrome.
The most commonly used agents are adrenal enzyme inhibitors, but adrenolytic agents, pituitary-targeted therapies or glucocorticoid-receptor antagonists are also used. Drugs can be used in combinations in lower doses, aiming for side effect reduction with synergistic effects.
When determining the approach to treatment, the first step is to determine whether the final goal is reducing the level of serum cortisol within normal values or complete cortisol secretion blockade. The latter approach is convenient for patients with more variable secretion, while patients showing less variability can benefit more from lowering the values to the normal range and therefore avoiding the necessity of steroid replacement therapy, as well as a possibility of side effects connected to the higher dosages required with that strategy.
Adrenal Enzyme Inhibitors
These agents are primarily used as inhibitors of steroid biosynthesis in the adrenal cortex, and thus can be utilized in all cases of hypercortisolaemia regardless of cause, but most commonly in ACTH-dependent forms, often with rapid improvement in the clinical features of Cushing’s syndrome. The most commonly used agents are metyrapone, ketoconazole, and in certain circumstances etomidate. In the UK ketoconazole and metyrapone are licenced for treatment of Cushing syndrome, while mitotene is licensed for the treatment of hypercortisolaemia due to adrenocortical carcinoma. The use of etomidate or mifepristone in Cushing syndrome is off-licence. However, the regulations are very nation-specific. When used in combinations, they have a synergistic therapeutic effect, lowering the rate of side effects.
Metyrapone
Metyrapone acts primarily to inhibit the enzyme 11β-hydroxylase, thus blocking the production of cortisol from 11-deoxycortisol in the adrenal gland 1. As a consequence to blockade of cortisol synthesis, levels of adrenal androgens and deoxycorticosterone rise. The subsequent elevation of 11-deoxycortisol can be monitored in the serum of patients treated with metyrapone. It should be noted that there may be some cross-reactivity from 11-deoxycortisol with some cortisol radioimmunoassays: this may result in an unnecessary increase in the metyrapone dose and subsequent clinical hypoadrenalism 2. It is preferable to measure the serum cortisol via liquid chromatography-tandem mass spectrometry in patients treated with metyrapone 3. The fall in cortisol is rapid, with trough levels at 2 hours post-dose, and sometimes administration of a test dose of 750 mg with hourly cortisol estimation for 4 hours is performed, although not strictly necessary in our opinion 4. Maintenance therapy is usually in the range 500-6000 mg/day in 3-4 divided doses daily.
Metyrapone has been used to good effect to reduce the hypercortisolaemia in patients with Cushing’s syndrome from adrenal tumours, the ectopic ACTH syndrome, and Cushing’s disease. In the former, patients can be very sensitive to low doses of this agent, whilst in Cushing’s disease higher doses are often required. In Cushing’s disease this can be due to the compensatory rise in ACTH in patients not having received pituitary radiotherapy. There have not been serious maternal or perinatal complications connected with the use of metyrapone in pregnant women, but the question of safety remains open 5.
The principal side effects with metyrapone are hirsutism and acne (as predicted by the rise in adrenal androgens), dizziness and gastrointestinal upset. Because of the androgen effect the drug is not considered appropriate for the first- line therapy of long-term treatment in women 6. However, it is hypoadrenalism that remains the most important potential problem, and careful monitoring of treatment and education of the patient is required. If there is uncertainty as to whether the measured cortisol is valid, and not over-estimated by cross-reactivity, it may be appropriate to consider a block-and-replace regimen.
Hypokalaemia, oedema and hypertension due to salt retention because of mineralocorticoid activity of raised levels of 11-deoxycorticosterone are infrequent 4, but may require cessation of therapy 7.
An new 11-hydroxylase inhibitor, osilodrostat is currently under trial.
Ketoconazole
Ketoconazole is an imidazole derivative originally developed as an oral anti-fungal agent. It is a potent inhibitor of sex steroids (androstendione and testosterone) production by its action on C17-20 lyase, and cortisol secretion by 11β-hydroxylase inhibition 8. It also inhibits 17-hydroxylase and 18-hydroxylase activity, amongst other enzymes 9. It has also been reported to have a direct effect on ectopic ACTH secretion from a thymic carcinoid tumour 10, and possibly corticotroph ACTH release.
The treatment for Cushing’s syndrome is usually started at a dose of 200 mg twice daily, with an onset of action that is slower than metyrapone. The usual maximum dose is 400mg three times a day.
It has been used successfully to lower cortisol levels in patients with Cushing’s syndrome of various aetiologies including adrenal carcinoma, the ectopic ACTH syndrome, and invasive ACTH-producing pituitary carcinoma, with doses required between 200-1200mg/day in up to 4 divided daily doses 11, although 2-3 times daily is more usual. Although there has not been consequences on human fetuses, considering animal teratogenity and toxicity the drug is not recommend for use during pregnancy 12.
The principal side effect of ketoconazole is hepatotoxicity 13. A reversible elevation of hepatic serum transaminases occurs in approximately 5%-10% of patients, with the incidence of serious hepatic injury at around 1 in 15,000 patients 14. The hepatotoxicity appears to be idiosyncratic, but has been reported within 7 days of the initiation of treatment in a patient with Cushing’s syndrome 15. Prior to the start of therapy liver function tests should be performed. The alanine aminotransferase (ALT) level should be monitored weekly within first month of therapy, then once a month in the following trimester and afterwards sporadically or when the dose is changed. If levels reach 3-times above the upper normal range, therapy should be discontinued. Other adverse reactions of ketoconazole include skin rashes and gastrointestinal upset 16, and one must always be wary of causing adrenal insufficiency 17. Ketoconazole is a mixture of laevo- and dextro- enantiomeric forms. Currently, the laevo-enantiomer of ketoconazole is under clinical trial as it may be less likely to be hepatotoxic than the racemic mixture.
Due to its C17-20 lyase inhibition and consequent anti-androgenic properties, ketoconazole is particularly useful in female patients where hirsutism is an issue, which may be worsened with metyrapone. Conversely, gynaecomastia and reduced libido in male patients may be unacceptable as a first-line long-term treatment and require alternative agents. However, replacement therapy is an option. On the other hand, women having lower levels of oestradiol and testosterone do not experience clinically manifest disorder because of the usually present menstrual irregularity. It requires gastric acid for absorption, so should never be given with proton-pump inhibitors. One further advantage of ketoconazole is its inhibition of cholesterol synthesis, particularly LDL cholesterol 18, and in 34 patients with Cushing’s syndrome the mean total cholesterol was reduced from 6.1 to 5.0 mmol/l on ketoconazole 16.
The triazole antifungal fluconazole can also be effective, but experience is limited 19.
Etomidate
Etomidate is an imidazole-derived anaesthetic agent which was reported to have an adverse effect on adrenocortical function in 1983 20. Compared to the other imidazole derivative ketoconazole, etomidate more potently inhibits adrenocortical 11β-hydroxylase, has a similar inhibition of 17-hydroxylase, but has less of an effect on C17-20 lyase 21. At higher concentrations it also appears to have an effect on cholesterol side-chain cleavage 22.
Following their initial report in 1983 23, Allolio and colleagues have shown that low-dose intravenous non-hypnotic etomidate (2.5mg/hour) normalized cortisol levels in 5 patients with Cushing’s syndrome of various aetiologies 24. Since then, there have been a number of case reports on the use of etomidate in successfully reducing hypercortisolaemia in seriously-ill patients with either Cushing’s disease or the ectopic ACTH syndrome 25.
It is usually given at a dose of 2.5 – 3.0 mg/hour, which is adjusted based on the serum cortisol levels. It usually takes several hours for cortisol to be lowered to within the normal range 26. Etomidate is an effective agent that acts rapidly, but is limited in its use by the fact it has to be given parenterally and requires intensive care settings to safely manage and monitor cortisol and potassium levels 4-6 hourly to adjust the infusion rate 26. A simultaneous infusion of hydrocortisone of 0.5-2mg/h may be required to maintain normal cortisol levels. However, in this situation it may be life saving. The preparation available in the USA contains the vehicle propylene glycol with the potential for nephrotoxicity, as opposed to the preparation available in Europe, which contains alcohol.
Adrenolytic therapy
Mitotane (o’p’DDD), an isomer of the insecticide DDD (belonging to the same family of chemicals as the insecticide DDT), was developed following the observation of adrenal atrophy in dogs administered DDD. Mitotane inhibits steroidogenesis by reducing cortisol and aldosterone production by blocking cholesterol side-chain cleavage and 11β-hydroxylase in the adrenal gland 27. It also acts as an adrenolytic drug, causing medical adrenalectomy, after being metabolised into an acyl chloride that binds in mitochondria and causes necrosis of adrenocortical cells 28.
Mitotane is used as a treatment for adrenal carcinoma and causes tumour regression and improved survival in some patients 29, and has a beneficial effect on endocrine hypersecretion in approximately 75% of patients 30. It is also utilised in Cushing’s syndrome of non-malignant origin, and in this regard lower doses can be utilised (up to 4 g/day), thus reducing the incidence of side effects, particularly gastrointestinal 31. At these lower doses the onset of the cortisol lowering effect takes longer (6-8 weeks) than with higher doses. Mitotane should not be used in pregnant women, and reproductively active women must use reliable contraception while on therapy 32.
One problem even with low-dose mitotane is the hypercholesterolemia (principally an increase in LDL-cholesterol), which appears to be due to the impairment of hepatic production of oxysterolds, normally a brake on the enzyme HMG Co A reductase 33. However, simvastatin, an HMG Co A reductase inhibitor, can reverse the hypercholesterolemia, and it or a similar agent should be used if necessary in patients treated with mitotane 33. Other side effects of mitotane include neurological disturbance; elevation of hepatic enzymes; hypouricaemia; gynaecomastia in men; and a prolonged bleeding time 34. Most importantly, it elevates cortisol-binding globulin, such that levels of total serum cortisol are misleading. Control should be titrated on urinary free cortisol or salivary cortisol. A monitoring of serum levels of mitotane should be undertaken due to narrow therapeutic window and the risk of toxicity.
In the long-term, measurement of blood levels can allow dose titration and reduction as appropriate. A therapeutic level of 14-20 mg/L has been recommended for adrenocortical carcinoma, but lower levels can be sought for simple control of elevated cortisol levels. Mitotane is taken up by fatty tissues, sometimes being released gradually several months after discontinuing therapy, therefore requiring adjustments in glucocorticoid therapy dosage 35.
Mitotane shows cytotoxic activity on both normal and tumorous tissue causing primary adrenal insufficiency and therefore requiring glucocorticoid replacement therapy. It tends to spare the zona glomerulosa, but in a long-term use mineralocorticoid replacement is also needed 36.
In general, despite effective in other forms of Cushing syndrome, its use has been limited outside of adrenal carcinoma, in which cases it has recently been shown to prolong life 29.
Modulators of ACTH release
Pasireotide
Somatostatin receptors have been demonstrated on both corticotroph adenomas, and some ectopic ACTH-secreting tumours. However, although octreotide has been helpful in reducing ACTH and cortisol levels in selected case reports of ectopic ACTH-secreting tumours there has been much more limited success in patients with Cushing’s syndrome probably through down-regulation of receptor sub-type 2 in these tumours by hypercortisolaemia 37.
Recently, there has been renewed interest with the introduction of pasireotide (SOM230), a somatostatin analogue with a broader spectrum of activity for somatostatin receptor sub-types, including type 5, which is not downregulated during hypercortisolaemia. Ever since this agent was shown in vitro to reduce human corticotroph proliferation and ACTH secretion 38, there have now been a number of clinical trials published. In an initial phase II trial, pasireotide 600µg injected twice daily for 15 days reduced urinary free cortisol levels in 76% of 29 patients and normalised levels in 17% 39. A multicentre phase III dose-randomised trial in 162 patients with either new, persistent, or recurrent Cushing’s disease has presented 12 month results. At six months there was a reduction in urinary free cortisol levels in 91 of 103 evaluable patients, with a median urinary free cortisol reduction of 48%. Normalisation of urinary free cortisol levels was achieved in 14.6% of patients on the 600µg dose twice daily, and 26% of patients on the 900µg twice-daily dose. Patients who showed <50% reduction in urinary free cortisol levels from baseline by month two were unlikely to show improvement by month 6 or 12. The most clinically relevant adverse events were hyperglycaemia (73%), with 46% developing frank diabetes mellitus related to decreases in both insulin and incretin secretion, and hypocortisolaemia (8%) 40. Other side effects included elevated liver enzymes, cholelithiasis, nausea and diarrhoea in the rate expected from experience with other somatostatin analogues 41. There is now also experience with pasireotide long-acting repeatable (pasireotide LAR), a monthly injection, with preliminary results suggesting around 30% control, although mostly in those patients with mild disease.
Pasireotide should be given in a dose 600µg subcutaneously twice daily, with a possibility of increasing the dosage to 900µg twice daily after couple of months of therapy. Pasireotide is not recommended as a first line treatment but can be considered as add-on therapy or second line treatment if other medications are not tolerated. In cases where there is no clinical response, it should be discontinued.
Pasireotide at a lower dose of 250µg three times daily has also been used in stepwise combination therapy with the dopamine agonist cabergoline (previously been demonstrated to have modest but variable efficacy as monotherapy in Cushing’s disease 42, and ketoconazole. Pasireotide monotherapy induced normalisation of urinary free cortisol levels in 5 of 17 patients (29%). The addition of cabergoline normalised urinary free cortisol levels in an additional 4 patients (24%). The further addition of ketoconazole in the remaining 8 patients induced normalisation of urinary free cortisol levels in 6 of these. Thus in total, remission was achieved in 88% of patients using combination therapy out to 80 days treatment 43. Therefore pasireotide represents a potential new treatment for Cushing’s disease, although the frequency of hyperglycaemia is of major concern.
Cabergoline
The presence of dopamine receptors (D2) on around 80% of corticotroph adenomas supported use of cabergoline in patients with Cushing’s disease 44. Cabergoline at the dose of 1-7mg weekly was reported to control hypercortisolaemia due to CD in 25-40% of patients in small case series 45. It is usually well tolerated and the most common side effects include nausea and dizziness. At the doses used for the treatment of pituitary tumors, the incidence of cardiac valve sclerosis and subsequent regurgitation was not increased in one large study, and therefore echocardiograms are not routinely needed unless high, long-term dose is required 46. However, escape is seen in some patients, so the precentage of patients with long-term control is low.
TemozolamideTemozolomide is an oral alkylating prodrug that is converted in vivo to the DNA repair inhibitor dacarbazine. Traditionally, this chemotherapy agent has been used in the treatment of malignant gliomas, but recent evidence suggests it is also useful in selected aggressive pituitary tumours including corticotroph pituitary carcinomas 47. Although, some reports suggested that the response to temozolomide in pituitary tumours can be predicted by low expression of the DNA repair enzyme O6-methylguanine-DNA-methyltransferase (MGMT), possibly related to MGMT gene promotor methylation 48, not all studies have confirmed this 49. However, the therapeutic response can usually be determined after 3 cycles of chemotherapy.
Other Agents
Retinoic acid has been found to inhibit ACTH-secretion and cell proliferation both in vitro in ACTH-producing tumour cell lines, and cultured human corticotroph adenomas, and in vivo in nude mice 50. However, clinical trials in man are limited, and it is unlikely to be a major contributor to control.
The thiazolidinedione rosiglitazone, a PPAR-γ agonist, has been shown in supra-pharmacological doses to suppress ACTH secretion in human and murine corticotroph tumour cells. In addition, the development of murine corticotroph tumours, generated by subcutaneous injection of ACTH-secreting AtT20 cells, were prevented 51. It appears this is not specific to corticotroph adenomas, but also applies to other forms of pituitary tumour 52. However, the results in human subjects with Cushing’s disease have been disappointing 53. This may be because doses used in the animal studies were much higher than the equivalent licensed dose in humans. Its use cannot be recommended, and indeed for other reasons it has now been withdrawn from the market.
In the rare causes of Cushing’s syndrome due to bilateral macronodular adrenal hyperplasia (BMAH) and aberrant receptor expression of GIP, β-adrenergic and LH/hCG receptors, specific receptor antagonists may prove to be useful 54. Although octreotide has been shown to have cause a therapeutic response in GIP-related ACTH-independent bilateral macronodular adrenal hyperplasia 55, others have found neither this somatostatin analogue or pasireotide to be helpful in inducing a sustained response 56.
Glucocorticoid receptor antagonist(s)
Mifepristone (RU 486), as a potent antagonist of glucocorticoid and progesterone receptors, blocks the peripheral actions of glucocorticoids and progestogens 57. As a consequence it also blocks glucocorticoid-induced negative feedback at the hypothalamo-pituitary level, inducing a rise in ACTH, arginine-vasopressin (AVP) and hence cortisol 58. It has occasionally been given to patients with all forms of Cushing’s syndrome 59, showing effectiveness in rapid reducing symptoms of cortisol-induced psychosis 60, and the metabolic benefit of glycaemic control and hypertension have been established 59. Although, it has proven to be effective in the treatment of hypercortisolaemia symptoms and signs 61, the major drawback is the lack of biochemical markers to asses either therapeutical effectiveness or possible hypoadrenalism. Adrenal insufficiency is challenging to treat, because the drug, besides blocking endogenous cortisol, also blocks the action of synthetic steroids as replacement therapy. Hypokalaemia is a frequent problem due to the saturation of 11β-HSD type 2 and cortisol action on mineralocorticoid receptor, although it responds well to spironolactone.
The daily dose of mifepristone ranges between 300 and 1200mg. It showed a significant improvement of glucose and HbA1c in 60% of patients with impaired glucose tolerance or diabetes 62. Mifepristone could be used as add-on therapy for Cushing’s syndrome with associated hyperglycemia. Endometrial thickening and vaginal bleeding secondary to the antiprogestin effect are likely to be seen in women. However, a new derivative of mifepristone with less anti-progestone blocking activity is currently under trial.
Cushing syndrome diet
Nutritious, wholesome foods provide a good source of fuel for your recovering body and can help you lose the extra pounds that you gained from Cushing syndrome. Make sure you’re getting enough calcium and vitamin D. Taken together, they help your body absorb calcium, which can help strengthen your bones, counteracting the bone density loss that often occurs with Cushing syndrome.
Home remedies
- Increase activities slowly. You may be in such a hurry to get your old self back that you push yourself too hard too fast, but your weakened muscles need a slower approach. Work up to a reasonable level of exercise or activity that feels comfortable without overdoing it. You’ll improve little by little, and your persistence will be rewarded.
- Monitor your mental health. Depression can be a side effect of Cushing syndrome, but it can also persist or develop after treatment begins. Don’t ignore your depression or wait it out. Seek help promptly from your doctor or a therapist if you’re depressed, overwhelmed or having difficulty coping during your recovery.
- Gently soothe aches and pains. Hot baths, massages and low-impact exercises, such as water aerobics and tai chi, can help alleviate some of the muscle and joint pain that accompanies Cushing syndrome recovery.
Coping and support
Support groups can be valuable in dealing with Cushing syndrome and recovery. They bring you together with other people who are coping with the same kinds of challenges, along with their families and friends, and offer a setting in which you can share common problems.
Ask your doctor about support groups in your community. Your local health department, public library and telephone book as well as the Internet also may be good sources to find a support group in your area.
Cushing syndrome prognosis
Although the earliest studies of Cushing syndrome reported a median survival of 4.6 years and five-year survival of only 50%, with recent advances in treatment, the standard mortality ratio is similar to the age-matched population. The morbidity and mortality of Cushing syndrome are primarily due to the effects of related conditions such as diabetes, hypertension, heart disease, obesity, and osteoporosis with fractures. The prognosis is worsened in the setting of an unresectable hormone-secreting tumor.
References- Carballeira A, Fishman LM, Jacobi JD. Dual sites of inhibition by metyrapone of human adrenal steroidogenesis: correlation of in vivo and in vitro studies. J Clin Endocrinol Metab 1976; 42:687-695.
- Trainer PJ, Besser M. Cushing’s syndrome. Therapy directed at the adrenal glands. Endocrinol Metab Clin North Am 1994; 23:571-584.
- Owen LJ, Halsall DJ, Keevil BG. Cortisol measurement in patients receiving metyrapone therapy. Ann Clin Biochem 2010; 47:573-575.
- Verhelst JA, Trainer PJ, Howlett TA, Perry L, Rees LH, Grossman AB, Wass JA, Besser GM. Short and long-term responses to metyrapone in the medical management of 91 patients with Cushing’s syndrome. Clin Endocrinol (Oxf) 1991; 35:169-178
- Buescher MA, McClamrock HD, Adashi EY. Cushing syndrome in pregnancy. Obstet Gynecol 1992; 79:130
- Feelders RA, Hofland LJ, de Herder WW. Medical treatment of Cushing’s syndrome: adrenal-blocking drugs and ketaconazole. Neuroendocrinology 2010; 92 Suppl 1:111
- Connell JM, Cordiner J, Davies DL, Fraser R, Frier BM, McPherson SG. Pregnancy complicated by Cushing’s syndrome: potential hazard of metyrapone therapy. Case report. Br J Obstet Gynaecol 1985; 92:1192-1195
- Engelhardt D, Dorr G, Jaspers C, Knorr D. Ketoconazole blocks cortisol secretion in man by inhibition of adrenal 11 beta-hydroxylase. Klin Wochenschr 1985; 63:607-612
- Engelhardt D, Weber MM, Miksch T, Abedinpour F, Jaspers C. The influence of ketoconazole on human adrenal steroidogenesis: incubation studies with tissue slices. Clin Endocrinol (Oxf) 1991; 35:163-168
- Steen RE, Kapelrud H, Haug E, Frey H. In vivo and in vitro inhibition by ketoconazole of ACTH secretion from a human thymic carcinoid tumour. Acta Endocrinol (Copenh) 1991; 125:331-334
- Rickman T, Garmany R, Doherty T, Benson D, Okusa MD. Hypokalemia, metabolic alkalosis, and hypertension: Cushing’s syndrome in a patient with metastatic prostate adenocarcinoma. Am J Kidney Dis 2001; 37:838-846
- Berwaerts J, Verhelst J, Mahler C, Abs R. Cushing’s syndrome in pregnancy treated by ketoconazole: case report and review of the literature. Gynecol Endocrinol 1999; 13:175.
- Castinetti F, Guignat L, Giraud P, et al. Ketoconazole in Cushing’s disease: is it worth a try? J Clin Endocrinol Metab 2014; 99:1623.
- Lewis JH, Zimmerman HJ, Benson GD, Ishak KG. Hepatic injury associated with ketoconazole therapy. Analysis of 33 cases. Gastroenterology 1984; 86:503-513
- McCance DR, Ritchie CM, Sheridan B, Atkinson AB. Acute hypoadrenalism and hepatotoxicity after treatment with ketoconazole. Lancet 1987; 1:573
- Sonino N, Boscaro M, Paoletta A, Mantero F, Ziliotto D. Ketoconazole treatment in Cushing’s syndrome: experience in 34 patients. Clin Endocrinol (Oxf) 1991; 35:347-352
- Tucker WS, Jr., Snell BB, Island DP, Gregg CR. Reversible adrenal insufficiency induced by ketoconazole. JAMA 1985; 253:2413-2414
- Miettinen TA. Cholesterol metabolism during ketoconazole treatment in man. J Lipid Res 1988; 29:43-51
- Van der Pas R, Hofland LJ, Hofland J, et al. Fluconazole inhibits human adrenocortical steroidogenesis in vitro. J Endocrinol 2012; 215:403.
- Ledingham IM, Watt I. Influence of sedation on mortality in critically ill multiple trauma patients. Lancet 1983; 1:1270
- Weber MM, Lang J, Abedinpour F, Zeilberger K, Adelmann B, Engelhardt D. Different inhibitory effect of etomidate and ketoconazole on the human adrenal steroid biosynthesis. Clin Investig 1993; 71:933-938
- Lamberts SW, Bons EG, Bruining HA, de Jong FH. Differential effects of the imidazole derivatives etomidate, ketoconazole and miconazole and of metyrapone on the secretion of cortisol and its precursors by human adrenocortical cells. J Pharmacol Exp Ther 1987; 240:259-264
- Allolio B, Stuttmann R, Fischer H, Leonhard W, Winkelmann W. Long-term etomidate and adrenocortical suppression. Lancet 1983; 2:626
- Allolio B, Schulte HM, Kaulen D, Reincke M, Jaursch-Hancke C, Winkelmann W. Nonhypnotic low-dose etomidate for rapid correction of hypercortisolaemia in Cushing’s syndrome. Klin Wochenschr 1988; 66:361-364
- Preda VA, Sen J, Karavitaki N, Grossman AB. Etomidate in the menagement of hypercortisolemia in Cushing’s syndrome: a review. Eur J Endocrinolo. 2012; 167(2):137-43
- Schulte HM, Benker G, Reinwein D, et al. Infusion of low dose etomidate: correction of hypercortisolemia in patients with Cushing’s syndrome and dose-response relationship in normal subjects. J Clin Endocrinol Metab 1990; 70:1426
- Young RB, Bryson MJ, Sweat ML, Street JC. Complexing of DDT and o,p’DDD with adrenal cytochrome P-450 hydroxylating systems. J Steroid Biochem 1973; 4:585-591
- Cueto C, Brown JH, Richardson AP Jr. Biological studies on an adrenocorticolytic agent and the isolation of the active components. Endocrinology 1958; 62:334.
- Terzolo M, Angeli A, Fassnacht M, Daffara F, Tauchmanova L, Conton PA, Rossetto R, Buci L, Sperone P, Grossrubatscher E, Reimondo G, Bollito E, Papotti M, Saeger W, Hahner S, Koschker AC, Arvat E, Ambrosi B, Loli P, Lombardi G, Mannelli M, Bruzzi P, Mantero F, Allolio B, Dogliotti L, Berruti A. Adjuvant mitotane treatment for adrenocortical carcinoma. N Engl J Med 2007; 356:2372-2380
- Luton JP, Cerdas S, Billaud L, Thomas G, Guilhaume B, Bertagna X, Laudat MH, Louvel A, Chapuis Y, Blondeau P. Clinical features of adrenocortical carcinoma, prognostic factors, and the effect of mitotane therapy. N Engl J Med 1990; 322:1195-1201
- Trainer PJ, Besser M. Cushing’s syndrome. Therapy directed at the adrenal glands. Endocrinol Metab Clin North Am 1994; 23:571-584
- Leiba S, Weinstein R, Shindel B, et al. The protracted effect of o,p’-DDD in Cushing’s disease and its impact on adrenal morphogenesis of young human embryo. Ann Endocrinol (Paris) 1989; 50:49
- Maher VM, Trainer PJ, Scoppola A, Anderson JV, Thompson GR, Besser GM. Possible mechanism and treatment of o,p’DDD-induced hypercholesterolaemia. Q J Med 1992; 84:671-679
- Haak HR, Caekebeke-Peerlinck KM, van Seters AP, Briet E. Prolonged bleeding time due to mitotane therapy. Eur J Cancer 1991; 27:638-641
- Hogan TF, Citrin DL, Johnson BM, et al. o,p’-DDD (mitotane) therapy of adrenal cortical carcinoma: observations on drug dosage, toxicity, and steroid replacement. Cancer 1978; 42:2177.
- Vilar O, Tullner Ww. Effects of o,p’ DDD on histology and 17-hydroxycorticosteroid output of the dog adrenal cortex. Endocrinology 1959; 65:80.
- Lamberts SW, de Herder WW, Krenning EP, Reubi JC. A role of (labeled) somatostatin analogs in the differential diagnosis and treatment of Cushing’s syndrome. J Clin Endocrinol Metab 1994; 78:17-19
- Batista DL, Zhang X, Gejman R, Ansell PJ, Zhou Y, Johnson SA, Swearingen B, Hedley-Whyte ET, Stratakis CA, Klibanski A. The effects of SOM230 on cell proliferation and adrenocorticotropin secretion in human corticotroph pituitary adenomas. J Clin Endocrinol Metab 2006; 91:4482-4488
- Boscaro M, Ludlam WH, Atkinson B, Glusman JE, Petersenn S, Reincke M, Snyder P, Tabarin A, Biller BM, Findling J, Melmed S, Darby CH, Hu K, Wang Y, Freda PU, Grossman AB, Frohman LA, Bertherat J. Treatment of pituitary-dependent Cushing’s disease with the multireceptor ligand somatostatin analog pasireotide (SOM230): a multicenter, phase II trial. J Clin Endocrinol Metab 2009; 94:115-122
- Henry RR, Ciaraldi TP, Armstrong D, et al. Hyperglycemia associated with pasireotide: results from a mechanistic study in healthy volunteers. J Clin Endocrinol Metab 2013; 98:3446
- Colao A, Petersenn S, Newell-Price J, et al: A 12-month phase 3 study of pasireotide in Cushing’s disease. N Engl J Med. 2012; 366(10):914-924.
- Godbout A, Manavela M, Danilowicz K, Beauregard H, Bruno OD, Lacroix A. Cabergoline monotherapy in the long-term treatment of Cushing’s disease. Eur J Endocrinol 2010; 163:709-716
- Feelders RA, de Bruin C, Pereira AM, Romijn JA, Netea-Maier RT, Hermus AR, Zelissen PM, van Heerebeek R, de Jong FH, van der Lely AJ, de Herder WW, Hofland LJ, Lamberts SW. Pasireotide alone or with cabergoline and ketoconazole in Cushing’s disease. N Engl J Med 2010; 362:1846-1848
- Pivonello R, Ferone D, de Herder WW, et al. Dopamine receptor expression and function in corticotroph pituitary tumors. J Clin Endocrinol Metab 2004; 89(5):2452-2462
- Godbout A, Manavela M, Danilowicz K, et al. Cabergoline monotherapy in the long-term treatment of Cushing’s disease. Eur J Endocrinol 2010; 163(5):709-716
- Trifiro G, Mokhles MM, Dieleman JP et al. Risk of cardiac valve regurgitation with dopamine agonist use in Parkinson’s disease and hyperprolactinaemia: a multi-country, nested case-control study. Drug Saf 2012; 35(2),159-171
- Curto L, Torre ML, Ferrau F, Pitini V, Altavilla G, Granata F, Longo M, Hofland LJ, Trimarchi F, Cannavo S. Temozolomide-induced shrinkage of a pituitary carcinoma causing Cushing’s disease–report of a case and literature review. ScientificWorldJournal 2010; 10:2132-2138
- McCormack AI, McDonald KL, Gill AJ, Clark SJ, Burt MG, Campbell KA, Braund WJ, Little NS, Cook RJ, Grossman AB, Robinson BG, Clifton-Bligh RJ. Low O6-methylguanine-DNA methyltransferase (MGMT) expression and response to temozolomide in aggressive pituitary tumours. Clin Endocrinol (Oxf) 2009; 71:226-233
- Bush ZM, Longtine JA, Cunningham T, Schiff D, Jane JA, Jr., Vance ML, Thorner MO, Laws ER, Jr., Lopes MB. Temozolomide treatment for aggressive pituitary tumors: correlation of clinical outcome with O(6)-methylguanine methyltransferase (MGMT) promoter methylation and expression. J Clin Endocrinol Metab 2010; 95:E280-E290
- Paez-Pereda M, Kovalovsky D, Hopfner U, Theodoropoulou M, Pagotto U, Uhl E, Losa M, Stalla J, Grubler Y, Missale C, Arzt E, Stalla GK. Retinoic acid prevents experimental Cushing syndrome. J Clin Invest 2001; 108:1123-1131
- Heaney AP, Fernando M, Yong WH, Melmed S. Functional PPAR-gamma receptor is a novel therapeutic target for ACTH-secreting pituitary adenomas. Nat Med 2002; 8:1281-1287
- Heaney AP, Fernando M, Melmed S. PPAR-gamma receptor ligands: novel therapy for pituitary adenomas. J Clin Invest 2003; 111:1381-1388
- Munir A, Song F, Ince P, Walters SJ, Ross R, Newell-Price J. Ineffectiveness of rosiglitazone therapy in Nelson’s syndrome. J Clin Endocrinol Metab 2007; 92:1758-1763
- Lacroix A, N’Diaye N, Mircescu H, Tremblay J, Hamet P. The diversity of abnormal hormone receptors in adrenal Cushing’s syndrome allows novel pharmacological therapies. Braz J Med Biol Res 2000; 33: 1201-1209
- Reznik Y, Allali-Zerah V, Chayvialle JA, Leroyer R, Leymarie P, Travert G, Lebrethon MC, Budi I, Balliere AM, Mahoudeau J. Food-dependent Cushing’s syndrome mediated by aberrant adrenal sensitivity to gastric inhibitory polypeptide. N Engl J Med 1992; 327:981-986
- Preumont V, Mermejo LM, Damoiseaux P, Lacroix A, Maiter D. Transient Efficacy of Octreotide and Pasireotide (SOM230) treatment in GIP-dependent Cushing’s syndrome. Horm Metab Res. 2011 Apr;43(4):287-91
- Baulieu EE. The steroid hormone antagonist RU486. Mechanism at the cellular level and clinical applications. Endocrinol Metab Clin North Am 1991; 20:873-891
- Healy DL, Chrousos GP, Schulte HM, Gold PW, Hodgen GD. Increased adrenocorticotropin, cortisol, and arginine vasopressin secretion in primates after the antiglucocorticoid steroid RU 486: dose response relationships. J Clin Endocrinol Metab 1985; 60:1-4
- Fleseriu M, Biller BM, Findling JW, et al. Mifepristone, a glucocorticoid receptor antagonist, produces clinical and metabolic benefits in patients with Cushing’s syndrome. J Clin Endocrinol Metab 2012; 97:2039
- Castinetti F, Fassnacht M, Johanssen S, et al. Merits and pitfalls of mifepristone in Cushing’s syndrome. Eur J Endocrinol 2009; 160:1003.
- Bertagna X, Bertagna C, Laudat MH, Husson JM, Girard F, Luton JP. Pituitary-adrenal response to the antiglucocorticoid action of RU 486 in Cushing’s syndrome. J Clin Endocrinol Metab 1986; 63:639-643
- Fleseriu M, Biller BM, Findling JW, et al. Mifepristone, a Glucocorticoid Receptor Antagonist, Produces Clinical and Metabolic Benefits in Patients with Cushing’s Syndrome. J Clin Endocrinol Metab 2012; 97(6):2039-2049.