What is diathermy
Diathermy also called electrodiathermy which means ‘dielectrical heat’, is a medical and surgical technique involving the controlled production of heat in a part of the body by high-frequency electric currents, to stimulate the circulation, relieve pain, destroy abnormal cells, or cause bleeding vessels to clot. The heat may come from electric currents, microwaves, radio waves, or ultrasound.
In principle, diathermy uses the heating effect of passing an electrical current across a resistor. In practice, the “resistor” is the patient’s skin or other tissue being cauterized or cut. Alternating current (AC) is often used in clinical practice. The correct term for resistance with alternating current (AC) as opposed to direct current (DC) is impedance. A potential difference created by the diathermy device produces a current that passes through the patient to complete an electrical circuit. This circuit may be completed in two ways:
- Unipolar diathermy. The cathode (−) is the cautery-diathermy (Bovie) tool tip, and the anode (+) is the ground or return plate. This is usually located on one of the patient’s buttocks or thighs. Unipolar diathermy-cautery configurations have the highest potential for complications with cardiac rhythm management devices, because the current pathway between the cathode and anode may pass near or across the cardiac rhythm management device pulse generator or leads.
- Bipolar diathermy. Both the cathode (−) and the anode (+) are incorporated in a forceps and are therefore very closely spaced. Thus, a grounding plate is not required with bipolar diathermy-cautery, and the current pathway is very small. The risk of cardiac rhythm management device-related complications is much smaller (but not absent) because the current pathway is far less likely to pass near or across the cardiac rhythm management device pulse generator or leads. The exception is if cautery is applied directly to or very near (i.e., within a few centimeters) the pulse generator or leads.
The higher the resistance at a point in an electrical circuit, the higher the heating effect will be with the passage of current. Thus, W = I2R, where W is the power output in watts, which is proportional to the heating effect; I is the current in amps; and R is the resistance in ohms. Resistance and the heating effect are higher where the current passes over a narrow pathway. Thus, current density is very high at the point of the unipolar diathermy-cautery pencil tip and relatively low throughout the patient’s body and across the large surface area of a correctly placed ground electrode pad. In fact, the only significant point of resistance (i.e., heat production) should be at the electrode tip.
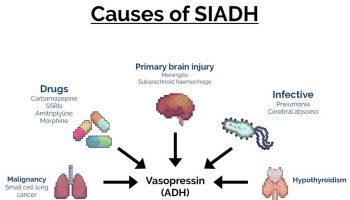
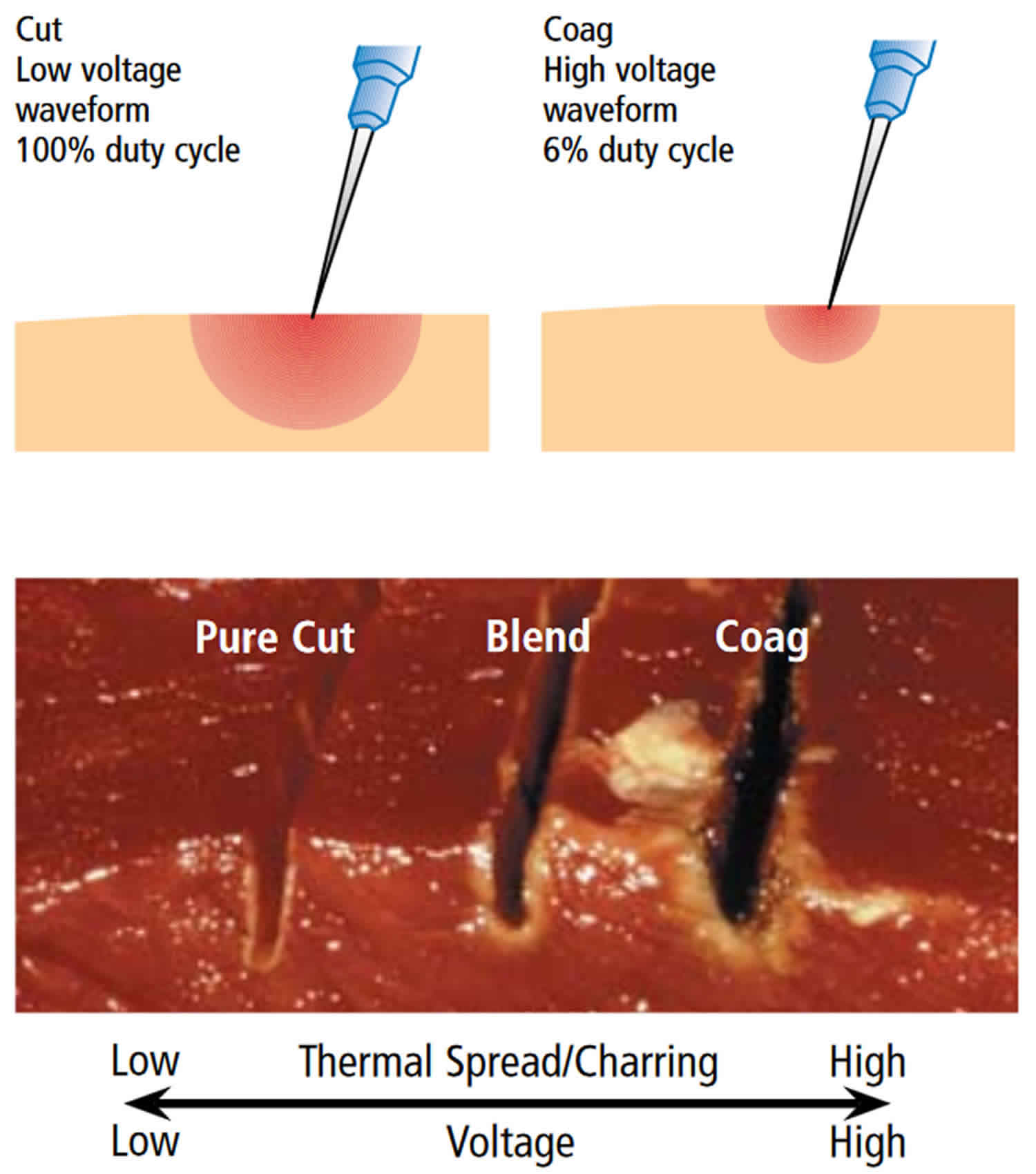
Diathermy units often develop power levels between 50 and 400 watts and radiofrequency AC cycles from 300 kHz to 3 MHz. Current is delivered in varying waveform patterns or modes. Continuous current is used for cutting, and pulses are used for coagulation. Because the pure cutting (diathermy) mode uses continuous current, it produces a series of sparks from the diathermy tool to the tissue. The pencil tip does not have to contact the tissue. The sparks generated cause intense local heating of cellular water, causing cellular explosion and destruction over a narrow band.
In contrast, coagulation (cautery) requires the direct application of the pencil tip; heat is thus dissipated over a wider area, causing the cells to shrink (crenate) and dry out (desiccate) rather than explode. Bipolar diathermy is generally restricted to coagulation modes. In contrast, unipolar diathermy incorporates various coagulation and cutting modes.
Argon gas, applied as a jet around the tip of the cathode, has been used to improve the safety and effectiveness of diathermy. This gas is heavier than air, inert, and noncombustible, and it displaces nitrogen and oxygen. It is also readily ionized by the current and provides a medium for the passage of current, so that the pencil tip does not have to be in direct contact with tissue.
There are basically two types of diathermy devices on the market today:
- Radio or high frequency and
- Microwave.
Ultrasonic or ultrasound therapy is also a form of diathermy, and is sometimes combined with electrical stimulation. Radio frequency diathermy is assigned an operating frequency of 27.12MH Z (short wave) by the Federal Communications Commission. Older radio frequency units were assigned an operating frequency of 13.56MH Z. Microwave diathermy is assigned 915MH Z and 2450MH Z as operating frequencies (these are also Microwave oven frequencies).
The present informal position of the Food and Drug Administration (FDA) is that a diathermy device should be capable of producing heat in tissue from a minimum of 104 °F (40 °C) to a maximum of 114 °F (45.6 °C) at a depth of two inches in not more than 20 minutes. When diathermy equipment is utilized, the power output is maintained below the pain threshold of the patient.
There are basically two methods of applying high or radio frequency diathermy – Dielectric and Inductive.
- Dielectric – When dielectric coupled diathermy is used, a rapidly alternating voltage differential is created between two electrodes producing a rapidly alternating electric field between the electrodes. The electrodes are placed either one on each side or both on the same side of the part of the body to be treated so that the electric field penetrates the tissues of the concerned area of the body. Because of the electrical charges within the tissue molecules, the tissue molecules will try to align themselves with the rapidly changing electric field. This rapid movement, or alternation, of the molecules, causing friction or collisions with other molecules, produces heat in the tissues. The electric field strength is determined by the degree of difference in potential between the electrodes set by the unit power control. Since frequency is not varied, the average power output determines the intensity of heating. The electrodes are usually small metal plates mounted in cushion like enclosures, but may be made of a flexible material such as wire mesh so that they may be contoured to fit a particular portion of the body.
- Inductive – In Inductive coupled radio frequency diathermy, high frequency current is generated through a coil to produce a rapidly reversing magnetic field. The coil is normally wound inside an applicator attached to the diathermy unit by an adjustable arm. The applicator is made in various forms for ease of application to the concerned area and is positioned directly over or next to the area to be treated. The rapidly reversing magnetic field induces circulating currents and electric fields into the body tissues, producing heat in the tissues. Induction coupling is generally employed at the lower radio frequency diathermy region. Intensity of heating is again determined by average power output.
It is the opinion of FDA and the consensus of experts that pulsing the output of radio frequency diathermy (as opposed to continuous wave) produces no extra beneficial therapeutic effects. Any physiological responses produced by pulsed radio frequency diathermy are attributable to heat produced by the average power output.
Microwave diathermy produces heat in the body tissues through application of microwave energy to the concerned area. The microwave energy stimulates tissue molecules, as radio frequency diathermy does, converting electrical energy to heat. Microwave energy is beamed from a director or applicator to the treatment area with intensity of heating controlled by the average power output of the microwave source and the spacing of the applicator from the concerned area. Microwave diathermy applicator size and shape is normally determined by the desired directivity and amount of tissue area to be treated.
When ultrasonic diathermy is used, a coupling oil or cream is applied to the concerned area. The ultrasonic applicator is then brought in contact with the cream which acts as a coupling medium for the ultrasonic energy between the transducer and the body. For an irregular surface such as a hand or foot, the limb and the applicator are immersed in water which readily transmits the energy to the tissues. Ultrasonic diathermy must operate at a frequency within the 800 to 1,000KH Z range. Power output must be plane wave (unfocused) and not exceed 3 watts per square centimeter (3 W/cm²). This does not apply to the experimental focused ultrasound surgery devices or new ultrasound diagnostic devices.
Diathermy electromagnetic energy can propagate by radiation or other coupling through air, tissue or current conductors to effect the operation of sensitive electronic equipment. Diathermy electromagnetic fields may induce currents that cause excessive heating of metal devices in the body, e.g., bone pins, implanted electrodes, dental fillings and metal sutures, producing burns in the adjacent tissues 1. A patient under treatment with r.f. diathermy is in a strong electrical field and is a conductor at some voltage above electrical ground. If this patient touches a bare metal part of the diathermy cabinet or any other electrically grounded part, he can receive a shock or burn 1.
Diathermy treatment
All types of diathermy produce changes in temperature through resistance to the passage of electromagnetic energy through the tissue being treated.
The three diathermy agents are ultrasound, short-wave diathermy, and microwave diathermy.
Ultrasound
Ultrasound is commonly used in the treatment of decreased range of motion, contractures, subacute trauma, and chronic degenerative osteoarthritis. Ultrasound is often used as an adjunct to stretching exercises prior to aggressive joint manipulation. Ultrasound is defined as an acoustic vibration with an audible range of 20,000 Hz. The heat is produced as a result of the conversion of electrical current into ultrasound energy through the use of a quartz crystal, which is subsequently converted into heat. Depth of heating may be up to 5 cm below the skin surface, providing a therapeutic benefit to superficial bone, joint capsule, ligament, and scar tissue. The ultrasound dosage is measured in Watts per square centimeter. Intensities of 0.8 to 3.0 W/cm² are commonly used. The dosage is varied depending on the condition. In subacute painful conditions such as tendinitis and adhesive capsulitis, lower intensities and higher frequencies are used. In more chronic conditions, such as contractures due to scar formations, intensities as high as 3.0 W/cm² are utilized. Ultrasound may decrease pain and improve range of motion in acute pain disorders and osteoarthritis compared with chronic pain conditions. Other studies have found any benefit to be based on empirical experience, lacking support from controlled studies.
Short-wave diathermy
Short-wave diathermy uses an oscillating electromagnetic field of high frequency to heat body surface areas. It heats to a tissue depth of 2 to 3 cm. Despite gradual decline in its use, short-wave diathermy still finds its place in treatment of large-surface body areas, such as lower extremities, upper extremities, and back. A study by Garrett and colleagues 2 concluded that pulsed short-wave diathermy was more effective than 1-MHz ultrasound in heating a large muscle mass and resulted in the muscles’ retaining heat longer.
This 2012 meta-analysis 3 found small, significant effects on pain and muscle performance only when short wave diathermy evoked a local thermal sensation. However, the variability in the treatment protocols makes it difficult to draw definitive conclusions about the factors determining the effectiveness of short wave diathermy treatment. More research (using comparable protocols and outcome measurements) is needed to evaluate possible long-term effects of thermal short wave diathermy treatment and its cost effectiveness in patients with knee osteoarthritis. Short wave diathermy treatment appears to be effective for decreasing pain and increasing muscle strength in patients with knee osteoarthritis. However, this effect is noticed primarily immediately post-treatment and is lost by 12 weeks following treatment. No definitive answers can be provided regarding the effects of short wave diathermy treatment on other impairments (e.g., joint inflammation) or on functional ability. The results indicate that a thermal treatment is probably not beneficial. Since the more modern short wave diathermy equipment is menu driven, clinicians are encouraged to determine that the dose provided by the menu is sufficient to induce at least some thermal sensation. More research, especially research using comparable samples,protocols and outcome measurements, is needed to evaluate the long-term effects of treatment and its cost effectiveness in patients with osteoarthritis of the knee as well as osteoarthritis of other joints.
A 2014 Cochcrane Review4 of electrotherapy modalities for adhesive capsulitis (frozen shoulder) concluded that therapeutic ultrasound, pulsed electromagnetic field therapy, Iodex phonophoresis, continuous short wave diathermy, a combination of Iodex iontophoresis with continuous short wave diathermy, or a combination of therapeutic ultrasound with transcutaneous electrical nerve stimulation (TENS) are ineffective as adjuncts to exercise for frozen shoulder therapy.
Microwave diathermy
Microwave diathermy uses electromagnetic radiation by microwaves and heats to a lesser tissue depth than short-wave diathermy. It is primarily used to heat superficial muscles and joints such as the shoulder. Besides its use in musculoskeletal conditions, this modality has been employed to reduce the potential effects of cancer chemotherapy and radiation treatment.
Surgical diathermy
Surgical diathermy is usually better known as “electrosurgery”. Electrosurgery and surgical diathermy involve the use of high-frequency A.C. electric current in surgery as either a cutting modality, or else to cauterize small blood vessels to stop bleeding. This technique induces localized tissue burning and damage, the zone of which is controlled by the frequency and power of the device.
Electrosurgery has three effects on body tissue:
- Cutting – generation of heat destroys tissue cell. Electrosurgical cutting divides tissue with electric sparks that focus intense heat at the surgical site. By sparking to tissue, the surgeon produces maximum current concentration. To create this spark the surgeon should hold the electrode slightly away from the tissue. This will produce the greatest amount of heat over a very short period of time, which results in vaporization of tissue.
- Fulguration and Coagulation– cell walls destroyed through dehydration. Electrosurgical fulguration (sparking with the coagulation waveform) coagulates and chars the tissue over a wide area. Since the duty cycle (on time) is only about 6 percent, less heat is produced. The result is the creation of a coagulum rather than cellular vaporization. In order to overcome the high impedance of air, the coagulation waveform has significantly higher voltage than the cutting current. Use of high voltage coagulation current has implications during minimally invasive surgery.
- Desiccation. Electrosurgical desiccation occurs when the electrode is in direct contact with the tissue. Desiccation is achieved most efficiently with the “cutting” current. By touching the tissue with the electrode, the current concentration is reduced. Less heat is generated and no cutting action occurs. The cells dry out and form a coagulum rather than vaporize and explode. Many surgeons routinely “cut” with the coagulation current. Likewise, you can coagulate with the cutting current by holding the electrode in direct contact with tissue. It may be necessary to adjust power settings and electrode size to achieve the desired surgical effect. The benefit of coagulating with the cutting current is that you will be using far less voltage. Likewise, cutting with the cut current will also accomplish the task with less voltage. This is an important consideration during minimally invasive procedures.
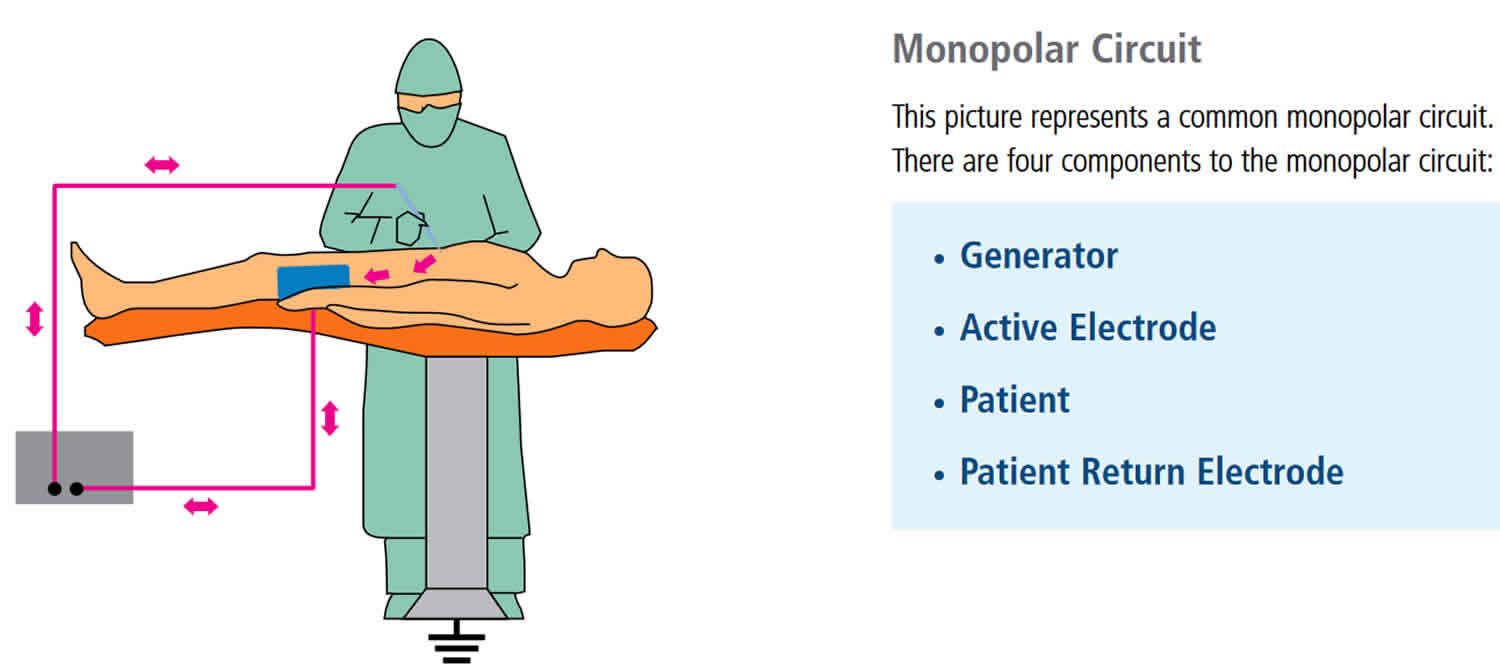
Figure 1. Surgical diathermy
Each of these processes generates smoke plume which contains:
- chemical by-products (eg acrylonitrile and hydrogen cyanide) which can be absorbed by the skin and lungs
- carbonised tissue, blood particles and viral DNA particles
- infectious viruses and bacteria have also been noted 5
Surgical diathermy or electrosurgery may be monoterminal, monopolar or bipolar:
Monoterminal electrosurgery
- Handpiece has single electrode.
- Indifferent electrode is not required.
Monopolar electrosurgery
- Uses single pointed probe to carry electrical current from power generator to surgical site.
- Requires indifferent electrode, typically large metal plate or flexible metalised plastic pad placed on skin distant from surgical site.
- Current passes from tip of probe through patient to indifferent electrode and completes circuit by returning to electrosurgical generator.
Monopolar electrosurgery is the most commonly used electrosurgical modality. This is due to its versatility and clinical effectiveness. In monopolar electrosurgery, the active electrode is in the surgical site. The patient return electrode is somewhere else on the patient’s body. The current passes through the patient as it completes the circuit from the active electrode to the patient return electrode.
Figure 2. Monopolar electrosurgery
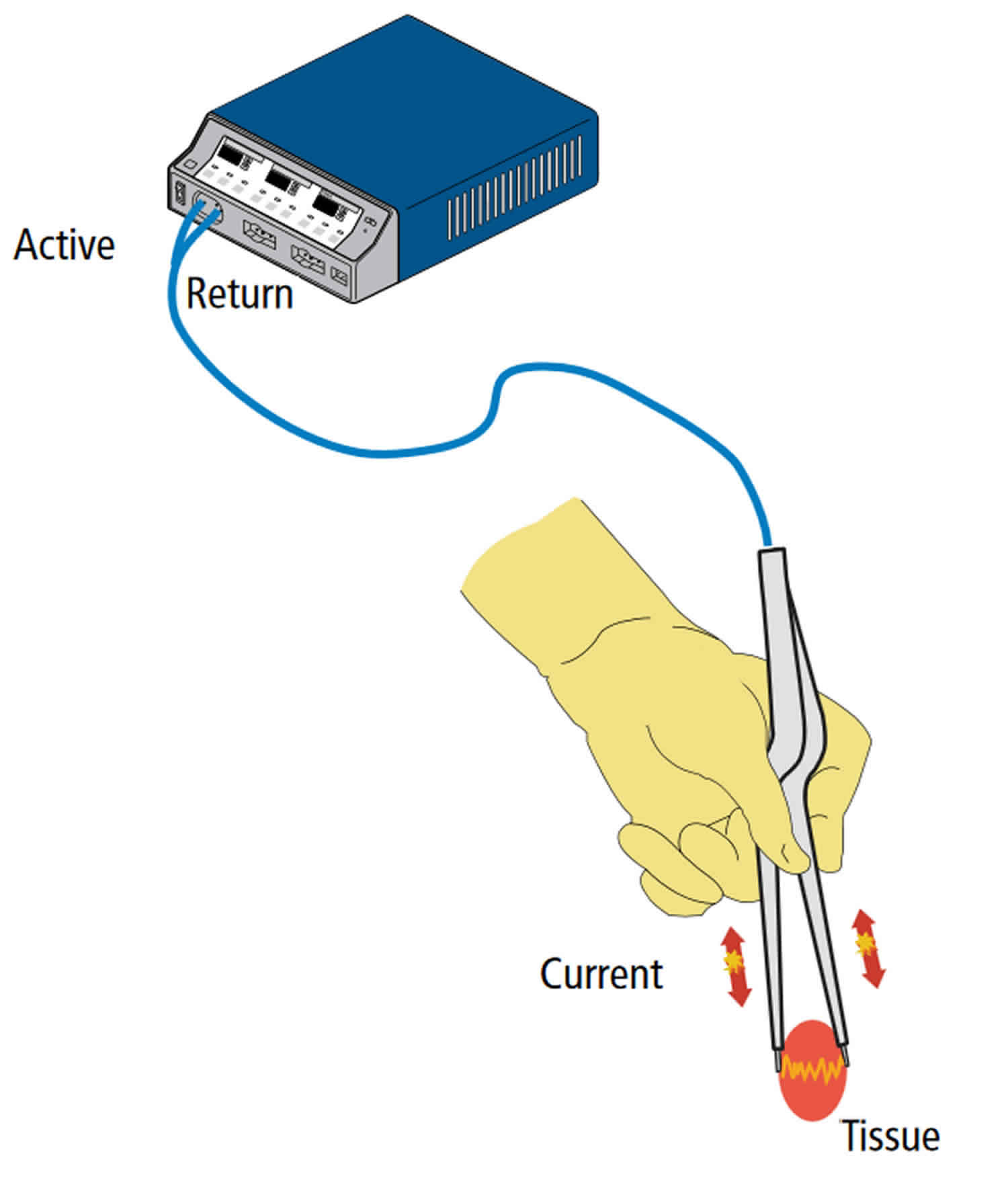
Bipolar electrosurgery
- Uses forceps with both tines connected to power generator: one is active and other is indifferent electrode.
- Current runs through tissue grasped by forceps.
- Used in patients with implanted cardiac devices such as a pacemaker or defibrillator, to prevent electrical current passing through the device, which might short-circuit or fire inappropriately.
In bipolar electrosurgery, both the active electrode and return electrode functions are performed at the site of surgery. The two tines of the forceps perform the active and return electrode functions. Only the tissue grasped is included in the electrical circuit. Because the return function is performed by one tine of the forceps, no patient return electrode is needed.
Figure 3. Bipolar electrosurgery
Frequency Spectrum
Standard electrical current alternates at a frequency of 60 cycles per second (Hz). Electrosurgical systems could function at this frequency, but because current would be transmitted through body tissue at 60 cycles, excessive neuromuscular stimulation and perhaps electrocution would result. Because nerve and muscle stimulation cease at 100,000 cycles/second (100 kHz), electrosurgery can be performed safely at “radio” frequencies above 100 kHz. An electrosurgical generator
takes 60 cycle current and increases the frequency to over 200,000 cycles per second. At this frequency electrosurgical energy can pass through the patient with minimal neuromuscular stimulation and no risk of electrocution.
Waveforms in electrosurgery
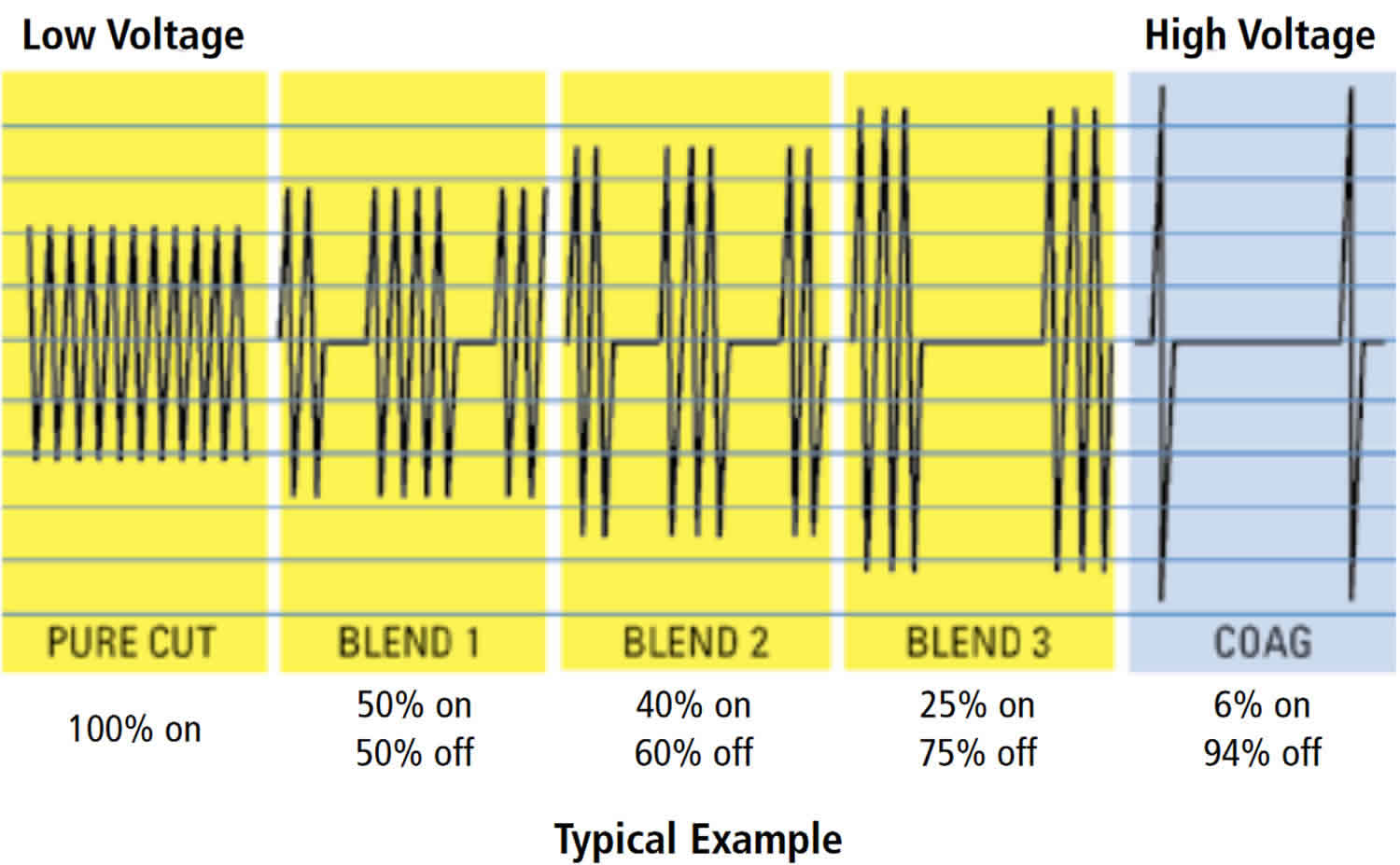
Different waveforms may be generated by the electrosurgery machine for different procedures.
- Continuous single, high frequency (>400 V) sine wave used at high heat for cutting / vaporisation leaves a zone of thermal damage. A high pitched sound is heard.
- Pulsed or modulated waveforms allow tissue to cool between bursts so that the zone of thermal damage is minimal.
- A sine wave turned on and off in a rapid succession (rectified) produces the slower heating process that results in coagulation. A rougher, lower tone is heard due to lower power.
- Variable waveforms can be produced to blend cut and coagulation, as power is adjusted in real time depending on tissue impedance.
Electrosurgical generators are able to produce a variety of electrical waveforms. As waveforms change, so will the corresponding tissue effects. Using a constant waveform, like “cut,” the surgeon is able to vaporize or cut tissue. This waveform produces heat very rapidly.
Using an intermittent waveform, like “coagulation,” causes the generator to modify the waveform so that the duty cycle (“on” time) is reduced. This interrupted waveform will produce less heat. Instead of tissue vaporization, a coagulum is produced.
A “blended current” is not a mixture of both cutting and coagulation current but rather a modification of the duty cycle. As you go from Blend 1 to Blend 3 the duty cycle is progressively reduced. A lower duty cycle produces less heat. Consequently, Blend 1 is able to vaporize tissue with minimal hemostasis whereas Blend 3 is less effective at cutting but has maximum hemostasis.
The only variable that determines whether one waveform vaporizes tissue and another produces a coagulum is the rate at which heat is produced. High heat produced rapidly causes vaporization. Low heat produced more slowly creates a coagulum. Any one of the five waveforms can accomplish both tasks by modifying the variables that impact tissue effect.
Figure 4. Waveforms in electrosurgery
Variables impacting tissue effect
In addition to waveform and power setting, other variables impact tissue effect. They include:
- Size of the electrode: The smaller the electrode, the higher the current concentration. Consequently, the same tissue effect can be achieved with a smaller electrode, even though the power setting is reduced.
- Time: At any given setting, the longer the generator is activated, the more heat is produced. And the greater the heat, the farther it will travel to adjacent tissue (thermal spread).
- Manipulation of the electrode: This can determine whether vaporization or coagulation occurs. This is a function of current density and the resultant heat produced while sparking to tissue versus holding the electrode in direct contact with tissue.
- Type of Tissue: Tissues vary widely in resistance.
- Eschar: Eschar is relatively high in resistance to current. Keeping electrodes clean and free of eschar will enhance performance by maintaining lower resistance within the surgical circuit.
Diathermy therapy
Ultrasonic diathermy products used in physical therapy equipment produce high-frequency sound waves that travel deep into tissue and create gentle therapeutic heat. Ultrasonic diathermy is intended to generate deep heat within body tissues for the treatment of selected medical conditions such as pain, muscle spasms and joint contractures, but not for the treatment of malignancies.
The sound waves are transmitted through a round-headed wand that the therapist applies to the skin with gentle, circular movements. A hypo-allergenic gel aids in the transmission of the ultrasonic energy and prevents overheating at the surface of the applicator.
Treatments usually last between five and 10 minutes.
Ultrasonic therapy does not hurt (there may be a bit of a tingling sensation and/or a sensation of warmth) if the therapist keeps the wand moving continuously. If, however, the wand is held in place for more than a few seconds, it can become uncomfortable at higher energies.
Ultrasonic diathermy is used to treat the following conditions:
- arthritis
- back pain
- fibromyalgia
- muscle spasms
- myositis
- neuralgia
- sprains and strains
- tenosynovitis
- tendonitis
- bursitis
However, there is still not a lot of evidence to prove that ultrasonic diathermy is the most effective treatment for these conditions.
You should also be aware that commercial ultrasonic diathermy devices may exist that have not been formally evaluated by FDA. Typically, these devices will claim to treat a range of diseases, disorders, and have other uses that are not covered in the description above (for example, to reduce wrinkles on the face).
Ultrasonic diathermy contraindications
While ultrasonic therapy can be used to treat the conditions described above, it is important to know that there are situations and areas of the body where it cannot safely be used. You should notify the practitioner administering the ultrasound if any of the following applies to you:
- You have a cardiac pacemaker
- You have a malignancy in the area to be treated
- You have a healing fracture in the area to be treated
- You are pregnant
- You have an implanted medical device other than a pacemaker such as implanted deep brain stimulation device
Diathermy complications
Two types of complications associated with surgical diathermy or cautery are electrocution and electromagnetic interference. Electrocution may occur if the patient circuit becomes a route for the passage of electrical current from other sources to the diathermy or cautery ground plate. These are termed leakage currents. Current passing through the body at the AC outlet frequency (60 Hz) can cause serious problems in excitable tissue (e.g., arrhythmias and large muscle group contractions, which may be perceived by awake patients). However, the same current applied in the radiofrequency range allows diathermy-cautery to work without producing these untoward effects. Thus, diathermy-cautery units incorporate an isolating capacitor in their circuits. This allows the passage of relatively harmless (for excitable tissue) radiofrequency current but impairs the passage of more dangerous low-frequency leakage currents to the ground plate.
The duration of the applied diathermy or cautery may also increase the probability of certain complications. For example, cardiac arrhythmias can be avoided if leakage current is prevented altogether or terminated rapidly (within a few microseconds) by line isolation circuitry. Major complications (e.g., ventricular fibrillation due to the passage of very small frequency currents across the heart) can also be minimized by line isolation monitors and ground fault circuit indicators.
Diathermy risks
Burns from electrocautery generally arise from a faulty grounding pad or from an outbreak of a fire 6. Monopolar electrocautery works because radio frequency energy is concentrated by the surgical instrument’s small surface area. The electrical circuit is completed by passing current through the patient’s body to a conductive pad that is connected to the radio frequency generator. Because the pad’s surface area is large relative to the instrument’s tip, energy density across the pad is reliably low enough that no tissue injury occurs at the pad site 7. Electrical shocks and burns are possible, however, if the circuit is interrupted or energy is concentrated in some way. This can happen if the pad surface in contact is small, e.g. if the pad’s electrolytic gel is dry, if the pad becomes disconnected from the radio frequency generator, or via a metal implant 8. Modern electrocautery systems are equipped with sensors to detect high resistance in the circuit that can prevent some injuries.
As with all forms of heat applications, care must be taken to avoid burns during diathermy treatments, especially in patients with decreased sensitivity to heat and cold. With electrocautery there have been reported cases of flash fires in the operating theatre related to heat generation meeting chemical flash points, especially in the presence of increased oxygen concentrations associated with anaesthetic.
Concerns have also been raised regarding the toxicity of surgical smoke produced by electrocautery. This has been shown to contain chemicals which may cause harm to patients, surgeons and/or operating theater staff 9.
For patients that have a surgically implanted Spinal Cord Stimulator system, diathermy can cause tissue damage through energy that is transferred into the implanted Spinal Cord Stimulator components resulting in severe injury or death 10.
References- High – Frequency Electrical Equipment in Hospitals; 1970, NFPA No. 76CM, Part III, Section 31, National Fire Protection Association, Boston, Massachusetts
- Garrett CL, Draper DO, Knight KL. Heat distribution in the lower leg from pulsed short-wave diathermy and ultrasound treatments. J Athl Train. 2000;35(1):50-5. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1323438/pdf/jathtrain00001-0052.pdf
- Effectiveness of thermal and athermal short-wave diathermy for the management of knee osteoarthritis: a systematic review and meta-analysis. Osteoarthritis and Cartilage. Volume 20, Issue 9, September 2012, Pages 957-966. https://doi.org/10.1016/j.joca.2012.05.005
- Page MJ, Green S, Kramer S, Johnston RV, McBain B, Buchbinder R. Electrotherapy modalities for adhesive capsulitis (frozen shoulder). Cochrane Database of Systematic Reviews 2014, Issue 10. Art. No.: CD011324. DOI: 10.1002/14651858.CD011324
- Woolhead K, Wicker P (2005) A Textbook of Perioperative Care. Edinburgh, Elsevier Churchill Livingstone
- Kressin KA; Posner KL; Lee LA; Cheney FW; Domino KB (2004). “Burn injury in the OR: a closed claims analysis”. Anesthesiology. 101: A1282.
- Principles of Electrosurgery. http://www.asit.org/assets/documents/Prinicpals_in_electrosurgery.pdf
- Mundlinger, Gerhard; Rosen, Shai; Carson, Benjamin (208). “Case Report Full-Thickness Forehead Burn Over Indwelling Titanium Hardware Resulting From an Aberrant Intraoperative Electrocautery Circuit”. ePlasty. 8: e1
- Fitzgerald, J. Edward F.; Malik, Momin; Ahmed, Irfan (2011). “A single-blind controlled study of electrocautery and ultrasonic scalpel smoke plumes in laparoscopic surgery”. Surgical Endoscopy. 26 (2): 337–42. doi:10.1007/s00464-011-1872-1
- Spinal Cord Stimulation Periprocedural Care. https://emedicine.medscape.com/article/1980819-periprocedure#aw2aab6b3b2